Abstract
The fusion of human serum albumin (HSA) with human lactoferrin (hLF) (designated as hLF-HSA) has improved the pharmacokinetic properties and anti-proliferative activities of hLF against cancer cells. In this study, we evaluated the anti-migratory activities of hLF and hLF-HSA against the human lung adenocarcinoma PC-14 cell line using wound healing and Boyden chamber assays. Despite the unexpected hLF-induced migration, hLF-HSA clearly demonstrated the complete inhibition of PC-14 cell migration. To examine the mechanism underlying the enhanced PC-14 cell migration by hLF alone but suppressed migration by hLF-HSA, we focused on the matrix metalloproteinase (MMP) family of endopeptidases because MMPs are often reported to play important roles in facilitating the migration and metastasis of cancer cells. Furthermore, hLF is a transactivator of MMP1 transcription. As expected, treatment of cells with hLF and hLF-HSA led to the upregulation and downregulation of MMP1, respectively. In contrast, MMP9 expression levels, which are often associated with cancer migration, were unchanged in the presence of either protein. An MMP inhibitor attenuated hLF-induced migration of PC-14 cells. Therefore, specific enhancement and suppression of MMP1 expression by hLF and hLF-HSA have been implicated as causes of a marked increase and decrease in PC-14 cell migration, respectively. In conclusion, the fusion of HSA with hLF (hLF-HSA) promoted its anti-migratory effects against cancer cells. Therefore, hLF-HSA is a promising anti-cancer drug candidate based on its improved anti-migratory activity towards cancer cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer cells that develop in primary tumors acquire the ability to migrate as they become cancerous, which allows them to move from the original site of the primary tumor to other distant organs through lymphatic and blood vessels to form secondary tumors (Guan 2015). This process is called cancer metastasis, which represents the leading cause of cancer-related deaths (Dillekås et al. 2019). Cancer migration is a critical process during cancer metastasis; thus, it is a suitable target pathway for the development of anti-metastatic agents (Hulkower and Herber 2011).
Lactoferrin (LF) is an innate immune protein that exhibits anti-cancer effects, such as inhibition of cancer growth and metastasis (Cutone et al. 2020). Oral (Iigo et al. 1999) and subcutaneous (Yoo et al. 1997) administration of bovine LF (bLF) or intraperitoneal (Bezault et al. 1994) administration of human LF (hLF) has been reported to exert anti-metastatic effects in experimental mouse models of tumor metastasis. As expected, the migration of cancer cells treated with bLF or hLF was inhibited, as revealed by in vitro wound healing (Grada et al. 2017) or Boyden chamber assays (Katt et al. 2016). These previous publications strongly suggest the potential anti-migratory activities of LF as an anti-cancer protein candidate (Cutone et al. 2020).
Recently, we developed human serum albumin (HSA)-fused hLF (hLF-HSA) as a potential therapeutic protein (Ueda et al. 2020). hLF-HSA demonstrates not only an extended half-life but also enhanced anti-proliferative effects against cancer cells (Ueda et al. 2020). In the present study, we evaluated the effects of hLF and hLF-HSA on cancer migration with a focus on the possible application of hLF-HSA as an anti-metastatic protein in two widely available assays, namely, a wound healing assay (Grada et al. 2017) and Boyden chamber assay (Katt et al. 2016). Although hLF unexpectedly promoted cancer cell migration, hLF-HSA exerted robust anti-migratory activity against cancer cells. The molecular mechanisms of action are also discussed in this report.
Materials and methods
Preparation of iron-saturated recombinant hLF (holo-hLF)
Recombinant human lactoferrin (hLF) produced in Aspergillus niger (> 95% purity, NRL Pharma Inc., Kawasaki, Japan) was dissolved in 0.1 M citric acid solution (pH 2.1) containing 3 mM ethylenediaminetetraacetic acid. After incubation for 24 h at room temperature, hLF was dialyzed against distilled water for 24 h at 10 °C to remove ferric ions (apo-hLF). Iron-saturated recombinant hLF (holo-hLF) was prepared by dialyzing apo-hLF to 50 mM phosphate buffer (pH 7.5) containing 0.001% (w/v) ferric ammonium citrate and 50 mM bicarbonate for 24 h at 10 °C, followed by dialysis against 50 mM phosphate buffer (pH 6.6) containing 50 mM NaCl for 24 h to remove excess iron. The iron content in holo-hLF was measured by using the Fe-C test kit (Wako Pure Chemicals, Osaka, Japan). The holo form of hLF (1588 ng Fe3+/mg protein) was used in this study because of the consistency with the use of holo-hLF-HSA (see below, 1302 ng Fe3+/ mg hLF equivalent) produced in CHO DG44 cells.
Preparation of recombinant hLF-HSA produced in CHO DG44 cells
Production of HSA fusion to the C-terminal hLF (hLF-HSA) in CHO DG44 cells was described in previous work (Ueda et al. 2020). hLF-HSA has an Asp-Pro linker derived from restriction sites between hLF and HSA in cloning. hLF-HSA expressed with the native hLF signal peptide was secreted into the culture medium and purified by cation-exchange chromatography (> 95% pure). hLF-HSA was usually produced as the holo form (1302 ng iron per mg hLF equivalent) in CHO DG44 cells. hLF-HSA was reported to show an approximately 3.3-fold longer half-life (64.0 min) than the holo form of hLF (19.5 min) (Ueda et al. 2020).
Reagents and chemicals
Commercially available HSA (> 95% purity) was purchased from the Fujifilm Wako Pure Chemical Corporation (Osaka, Japan). The reagents for cell culture were purchased from Fujifilm Wako Pure Chemical Corporation unless otherwise indicated.
Cell culture
The human lung adenocarcinoma cell line PC-14 (Noro et al. 2006) was acquired from Immuno-Biological Laboratories Co. Ltd. (Gunma, Japan). PC-14 cells were maintained in RPMI 1640 medium supplemented with 10% (v/v) fetal bovine serum (FBS). The cells were then incubated at 37 °C in an atmosphere containing 5% CO2.
Wound healing assay
A wound healing assay was performed to compare the migratory abilities of PC-14 cells in the presence of each sample. The cells were seeded at 2 × 105 cells/well in a 24-well plate and cultured until they reached 90% confluence. Prior to scratching, the cells were pretreated with 5 µg/ml mitomycin C (a cell proliferation inhibitor) in serum-free RPMI 1640 medium for 2 h. A mechanical wound (approximately 2.5 mm wide) was made across the cells, and then the cells were treated with 5 µM of each protein (hLF, HSA, hLF-HSA, or concurrent addition of hLF and HSA [hLF + HSA]) in a serum-free medium for 48 h. The capacity of the proteins to suppress the migration of PC-14 cells was evaluated using two methods: measuring the wound width and counting the number of migrating cells in a mechanical wound. To measure the wound width, the mechanical wound was photographed and the wound width was measured in five random fields. To count the number of migrating cells in a mechanical wound, the mechanical wound was photographed and the migrating cell numbers were counted in five random fields. When an matrix metalloproteinase (MMP) inhibitor (IIomastat, MedChemExpress, Monmouth Junction, NJ, USA) was used, 20 µM IIomastat was simultaneously added to the sample proteins tested. All results were analyzed using ImageJ software (National Institutes of Health, Bethesda, MD, USA).
Boyden chamber assay
The Boyden chamber assay (No. 140,629, Nunc, Thermo Fisher Scientific, Denmark) was designed according to the principle that cancer cells can migrate into the bottom chambers containing medium with 10% FBS through polycarbonate microporous membranes with an 8 μm pore diameter. Two × 105 cells of PC-14 in 400 µL serum-free RPMI 1640 containing 5 µM of each protein (hLF, HSA, hLF-HSA, or the concurrent addition of hLF and HSA [hLF + HSA]) were seeded in the top chamber of a 24-well plate. The bottom chamber was filled with 750 µL RPMI-1640 supplemented with 10% FBS. The cells were cultured for 48 h, and cotton swabs were used to scrub the non-migrating cells on the top surfaces. Migrating cells on the undersurface were fixed with ice-cold methanol for 15 min and stained with 0.2% crystal violet. The membrane was washed three times with ice-cold PBS. The stained cells on the undersurfaces were photographed, and the ratio of the stained area was calculated in five random fields. All results were analyzed using ImageJ software.
Immunoblotting
PC-14 cells (2 × 105 cells/well) were seeded in a 12-well plate and treated with 5 µM of each protein (hLF, hLF-HSA, HSA, or concurrent addition of hLF and HSA [hLF + HSA]) in serum-free RPMI 1640 for 48 h. The cells were suspended in 300 µL of lysis buffer (PBS containing 1% Triton X-100 and a mixture of protease inhibitors) and then incubated at 4 °C for 1 h. After centrifugation, the protein concentration in the cell lysate was measured using a Bradford assay. Heat-treated cell lysates (30 µg) were separated by 15% SDS-PAGE under reducing conditions and transferred onto a nitrocellulose membrane (Amersham Protran 0.45 μm NC [GE Healthcare]). The membranes were blocked in blocking buffer (5% skim milk in TBS-0.05% Tween 20 [TBS-T]) for 1 h at 25 °C and then incubated overnight at 4 °C with primary antibodies diluted to 1:1000 in blocking buffer (MMP1[10371-2-AP] and MMP9 [10375-2-AP], Proteintech, Rosemont, IL, USA). Then, the membranes were incubated with HRP-conjugated anti-rabbit IgG (1:5000, Zymed) for 1 h at 25 °C. Chemiluminescence was detected using a chemiluminescence reagent (Immunostar Zeta; Fujifilm Wako Pure Chemical Corporation). After immunoblotting with MMP antibodies, the antibodies were removed from the membranes using stripping buffer (Fujifilm Wako Pure Chemical Corporation) and the blots were reprobed with γ1 actin antibodies (Fujifilm Wako Pure Chemical Corporation) as described previously (Matsuzaki et al. 2019). Band intensities were quantified using ImageJ software.
Statistical analysis
Tukey’s test was conducted to compare cell migration in a wound healing assay (Figs. 1 and 2) or a Boyden chamber assay (Fig. 3), and the expression levels of MMP1 and MMP9 in the treated PC-14 cells (Fig. 4). Student’s t-test was performed to evaluate cell migration with or without an MMP inhibitor in a wound healing assay (Fig. 5). Statistical significance was set at p < 0.05. Statistical analyses were performed using the online statistical software EZR (Kanda 2013) (See https://www.jichi.ac.jp/saitama-sct/SaitamaHP.files/statmedEN.html).
Results
Human lactoferrin (hLF) and human serum albumin-fused hLF (hLF-HSA) suppress PC-14 lung cancer cell migration as revealed by the wound width in a wound healing assay
The human lung adenocarcinoma PC-14 cell line was used to evaluate the inhibitory effects of hLF and hLF-HSA on cancer cell migration based on an in vitro wound healing assay. First, the anti-migratory effects on PC-14 cells were evaluated by measuring the mechanical wound width, which is a frequently used method (Fig. 1). To reduce the contribution of cell proliferation in this assay, cells were pretreated with the proliferation inhibitor mitomycin C and subsequently treated with each protein sample in serum-free medium. hLF inhibited PC-14 cell migration after 48 h of incubation time. HSA also showed similar inhibitory effects. hLF-HSA exerted superior anti-migratory effects on PC-14 cells compared with hLF and HSA. However, the concurrent addition of hLF and HSA (hLF + HSA) did not show any significant effects.
hLF and hLF-HSA show anti-migratory activities against human lung cancer PC-14 cells, as revealed by measuring the wound width in a wound healing assay. A PC-14 cells were treated with 5 µM of each protein (hLF, HSA, hLF-HSA or concurrent addition of hLF and HSA [hLF + HSA]) to serum-free medium for 48 h. Representative light microscopy images of mechanical wounds are shown. B Wound width between the edges of the scratch is represented graphically. All data are presented as mean ± SD (n = 3); non-significant (ns), *p < 0.05, and ***p < 0.001 compared with the control; ##p < 0.01 hLF vs. hLF-HSA
Migration of PC-14 cells was unexpectedly enhanced by hLF but suppressed by hLF-HSA based on migrating cell counts in a mechanical wound in a wound healing assay
Next, we evaluated the anti-migratory activities of the samples by counting the number of migrating cells in a mechanical wound using a wound healing assay (Fig. 2). To minimize cell proliferation, this assay was also performed using mitomycin C and a serum-free medium as above. Compared with the results based on wound widths, hLF greatly promoted PC-14 cell migration, HSA showed a slight inhibitory effect, hLF-HSA significantly reduced the migration of PC-14 cells, while the concurrent addition of hLF and HSA (hLF + HSA) significantly enhanced PC-14 cell migration based on the high migration-promoting effects of hLF.
hLF unexpectedly promotes the migration of PC-14 cells while hLF-HSA suppresses it, as revealed by counting the migrating cell numbers in a mechanical wound in a wound healing assay. A PC-14 cells were treated with 5 µM of each protein (hLF, HSA, hLF-HSA or concurrent addition of hLF and HSA [hLF + HSA]) to serum-free medium for 48 h. Representative light microscopy images of migrating cells in a mechanical wound (the images are from the photographs in Fig. 1A) are shown. B Number of migrating cells in mechanical wounds are graphically represented. All data are presented as the mean ± SD (n = 3); *p < 0.05 and ***p < 0.001 compared with the control; ###p < 0.001, hLF vs. hLF-HSA
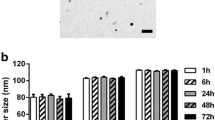
Boyden chamber assay shows that the migration of PC-14 cells was promoted by hLF but suppressed by hLF-HSA
Because the wound healing assay based on wound widths and the number of migrating cells yielded discrepant results in terms of the effects of hLF, a Boyden chamber assay was performed to evaluate the treated samples (Fig. 3). These results are consistent with those obtained in a wound healing assay based on the number of migrating cells. hLF enhanced PC-14 cell migration, HSA slightly suppressed migration, hLF-HSA suppressed migration, while the concurrent addition of hLF and HSA (hLF + HSA) enhanced migration, suggesting that covalent fusion between hLF and HSA is pivotal for the anti-migratory activity of this treatment against cancer cells.
hLF unexpectedly promotes the migration of PC-14 cells while hLF-HSA suppresses it, as revealed by a Boyden chamber assay. A Light microscopy image represents the migrating cells on underside filters with 8 μm pores after 48 h of treatment with 5 µM of each protein (hLF, HSA, hLF-HSA, or concurrent addition of hLF and HSA [hLF + HSA]). Migrating cells were stained with crystal violet. Images were captured under a microscope. B Ratio of stained area on the underside of the filter membranes are graphically represented. All data are presented as the mean ± SD (n = 3); **p < 0.01 and ***p < 0.001 compared to the control; ###p < 0.001, hLF vs. hLF-HSA
Upregulation of MMP1 expression by hLF and its downregulation by hLF-HSA
To elucidate the mechanism underlying hLF-induced cell migration and hLF-HSA-induced anti-cell migratory responses in PC-14 cells, we focused on MMPs, which are implicated in cancer cell migration because of their ability to degrade barriers formed by the extracellular matrix (Gonzalez-Avila et al. 2019). Moreover, hLF has been reported to be a transactivator of MMP1 (Oh et al. 2001). Thus, we examined MMP1 expression in treated PC-14 cells. Consistent with the experimental observations of PC-14 cell migration, hLF and hLF-HSA enhanced and suppressed MMP1 expression in PC-14 cells, respectively, as confirmed by western blotting (Fig. 4). Meanwhile, the expression levels of MMP9, which has been implicated in cancer migration, were unchanged in the treated samples, suggesting that MMP1 expression is regulated by hLF and hLF-HSA.
MMP1 expression is specifically upregulated by hLF but downregulated by hLF-HSA. A MMP1 expression levels in the PC-14 cells treated with 5 µM of each protein (hLF, hLF-HSA, HSA, or concurrent addition of hLF and HSA [hLF + HSA]) to serum-free medium for 48 h. Relative band intensities are graphically represented (below). B MMP9 expression in PC-14 cells treated with 5 µM of each protein (hLF, hLF-HSA, HSA, or concurrent addition of hLF and HSA [hLF + HSA]) to serum-free medium for 48 h. Relative band intensities are graphically represented (below). All data are represented as the mean ± SD (n = 3); non-significant (ns), *p < 0.05, ##p < 0.01, hLF vs. hLF-HSA
Increased cell migration of PC-14 cells induced by hLF can be attenuated by an MMP inhibitor, as confirmed by a wound healing assay
An MMP inhibitor (IIomastat) was used to investigate whether MMP1 expression regulated by hLF and hLF-HSA led to enhanced and suppressed cell migration, respectively, using a wound healing assay (Fig. 5). As a background control, the MMP inhibitor attenuated PC-14 cell migration by approximately 44%. The MMP inhibitor also attenuated hLF-mediated PC-14 cell migration to a level similar to that of the control. In the presence of the MMP inhibitor, cells treated with the concurrent addition of hLF and HSA [hLF + HSA] showed a slight decrease in migration while cells treated with HSA or hLF-HSA did not show changes in migration. Taken together, the elevated MMP1 expression induced by hLF increased cell migration while the downregulated MMP1 expression induced by hLF-HSA robustly suppressed cancer migration.
MMP inhibitor treatment abolishes the migrating PC-14 cells induced by hLF as confirmed by a wound-healing assay. A PC-14 cells were treated with 5 µM of each protein (hLF, HSA, hLF-HSA or concurrent addition of hLF and HSA [hLF + HSA]) to serum-free medium with or without 20 µM MMP inhibitor for 48 h. Representative light microscopy images of migrating cells in a mechanical wound are shown. B Number of migrating cells in the mechanical wound in the presence or absence of an MMP inhibitor is graphically represented. All data are represented as the mean ± SD (n = 3); non-significant (ns), *p < 0.05, **p < 0.01
Discussion
Cancer metastasis is the process by cancer cells spread from the primary site of origin to form new tumors in other parts of the body, and it is a leading cause of cancer mortality (Fares et al. 2020). Therefore, approaches for the prevention of metastatic cancer are considered promising therapeutic strategies (Schegoleva et al. 2022). Cancer cell migration is the directed movement of individual cancer cells (single-cell migration) and cell sheets and clusters (collective cell migration) in response to mechanical and/or chemical signals, which play central roles in the process of cancer metastasis (Lintz et al. 2017). Thus, in the present study, we focused on cancer cell migration to explore the potential use of hLF and hLF-HSA as anti-metastatic drugs.
Although few studies have focused on the ability of hLF to promote cancer metastasis (Au-Yeung et al. 2020) or cancer cell migration (Ha et al. 2011), the inhibitory effects of LF on cancer metastasis, invasion, and migration have been reported in a substantial number of publications (Cutone et al. 2020). Knockout of LF in mice has been reported to facilitate metastasis of transplanted human melanoma cells to the lungs (Wei et al. 2020). This previously published study indicates that mouse LF plays a role in inhibiting metastasis.
In the current study, two widely available assays, namely, a wound healing assay (Grada et al. 2017) and Boyden chamber assay (Katt et al. 2016), were chosen to evaluate the effects of hLF and hLF-HSA on PC-14 cancer cell migration. Two different assay formats were used when the wound healing assay was employed to examine cell motility. One is based on measuring the wound width (Fig. 1), which is a more commonly used format (Grada et al. 2017), and the other is based on counting the number of migrating cells in a mechanical wound (Fig. 2). Surprisingly, these two assay formats provided opposite results regarding the effects of hLF (Figs. 1 and 2). A possible explanation for this discrepancy is the different contributions of cell proliferation to each assay format, although the proliferation inhibitor mitomycin C and serum-free medium were used in the assays. However, both assay formats clearly showed that hLF-HSA robustly blocked cancer cell migration (Figs. 1 and 2). The Boyden chamber assay also showed the same results as the wound healing assay, in which the hLF-induced promotion of migrating cells and hLF-HSA-induced complete inhibition of cancer cell migration were determined (Fig. 3). Therefore, the results indicate that hLF promotes cancer cell migration while hLF-HSA remarkably suppresses it. Here in this study, HSA alone was found to exhibit its anti-migratory effects on PC-14 cells (Figs. 1, 2 and 3). The fusion of HSA to hLF led to the synergistic action of hLF and HSA. To our knowledge, there are no previous reports on the anti-migratory properties of HSA.
The use of hLF produced in A. niger may raise potential concerns about its glycosylation-dependent properties (Zlatina and Galuska 2021). hLF expressed in A. niger has high-mannose structures, whereas CHO-derived hLF has mammalian sialylated glycans (Kruzel et al. 2013). This different glycosylation pattern may lead to discrepant results between hLF and hLF-HSA in this study. However, like hLF produced in A. niger, hLF derived from both rice (Lacromin, InVitria, Junction City, KS, USA) and transgenic goats (Neolactoferrin, Transgenepharm LLC, Moscow, Russia) (Goldman et al. 2012) also promoted the migration of PC-14 cells (data not shown). These results indicated the possibility that the amino acid sequence of hLF participates in its induced promotion of migrating PC-14 cells. In any case, the migration-promoting effects of hLF produced in CHO cells need to be further clarified.
In terms of the mechanism by which hLF and hLF-HSA modulate cancer cell migration, we found that the regulation of MMP1 expression by hLF and hLF-HSA could at least partly account for their effects on cancer cell migration (Fig. 4). In the presence of an MMP inhibitor, hLF-treated PC-14 cells exhibited a reduction in cell migration to the basal levels of the control while hLF-HSA-treated cancer cells did not exhibit such a change and presented migration levels lower than those of the control, which suggests that hLF-HSA might function in cell migration pathways other than MMP1-related cell migratory signaling (Fig. 5).
Reports have indicated that the binding of hLF to its receptor low-density lipoprotein receptor-related protein 1 (LRP-1) leads to elevated MMP1 expression in chondrocytes (Brandl et al. 2010). hLF is a transactivator of MMP1 expression (Oh et al. 2001). These reports support hLF-induced cell migratory signaling via MMP1 in cancer cells. A recent report described that hLF elicited cell migratory signaling through MMP1 in human ovarian cancer cells (Au-Yeung et al. 2020).
To date, the molecular mechanisms underlying the enhanced anti-migratory activities of hLF-HSA in cancer cells are unknown. The concurrent addition of hLF and HSA did not show any effect, indicating the importance of the fusion between hLF and HSA. To confirm this finding, the preparation of hLF-HSA with a cleavable linker between hLF and HSA in cells would be useful.
Recently, we found that the fusion of HSA with hLF is required for the enhanced intracellular uptake and anti-proliferative effects of hLF on cancer cells (Kurimoto, D. et al., manuscript in preparation). Thus, similar to the anti-proliferative effects of hLF-HSA on cancer cells, the enhanced inhibitory effects of hLF-HSA on cancer cell migration may be related to its intracellular uptake. Intracellular expression of hLF in nasopharyngeal carcinoma has been reported to suppress invasiveness (Deng et al. 2013). However, further research is needed to determine the mechanism underlying the enhanced anti-migratory activity of hLF-HSA in cancer cells.
Conclusion
Although hLF unexpectedly promoted the migration of PC-14 lung cancer cells, the fusion of HSA with hLF (hLF-HSA) clearly blocked this enhanced cell migration. Regulation of MMP1 expression by hLF and hLF-HSA accounts for at least a proportion of their effects on the migration of PC-14 lung cancer cells.
References
Au-Yeung CL, Yeung TL, Achreja A, Zhao H, Yip KP, Kwan SY, Onstad M, Sheng J, Zhu Y, Baluya DL, Co NN, Rynne-Vidal A, Schmandt R, Anderson ML, Lu KH, Wong STC, Nagrath D, Mok SC (2020) ITLN1 modulates invasive potential and metabolic reprogramming of ovarian cancer cells in omental microenvironment. Nat Commun 11:3546. https://doi.org/10.1038/s41467-020-17383-2
Bezault J, Bhimani R, Wiprovnick J, Furmanski P (1994) Human lactoferrin inhibits growth of solid tumors and development of experimental metastases in mice. Cancer Res 54:2310–2312
Brandl N, Zemann A, Kaupe I, Marlovits S, Huettinger P, Goldenberg H, Huettinger M (2010) Signal transduction and metabolism in chondrocytes is modulated by lactoferrin. Osteoarthritis Cartilage 18:117–125. https://doi.org/10.1016/j.joca.2009.08.012
Cutone A, Rosa L, Ianiro G, Lepanto MS, Bonaccorsi di Patti MC, Valenti P, Musci G (2020) Lactoferrin’s anti-cancer properties: safety, selectivity, and wide range of action. Biomolecules. https://doi.org/10.3390/biom10030456
Deng M, Zhang W, Tang H, Ye Q, Liao Q, Zhou Y, Wu M, Xiong W, Zheng Y, Guo X, Qin Z, He W, Zhou M, Xiang J, Li X, Ma J, Li G (2013) Lactotransferrin acts as a tumor suppressor in nasopharyngeal carcinoma by repressing AKT through multiple mechanisms. Oncogene 32:4273–4283. https://doi.org/10.1038/onc.2012.434
Dillekås H, Rogers MS, Straume O (2019) Are 90% of deaths from cancer caused by metastases? Cancer Med 8:5574–5576. https://doi.org/10.1002/cam4.2474
Fares J, Fares MY, Khachfe HH, Salhab HA, Fares Y (2020) Molecular principles of metastasis: a hallmark of cancer revisited. Signal Transduct Target Ther 5:28. https://doi.org/10.1038/s41392-020-0134-x
Goldman IL, Georgieva SG, Gurskiy YG, Krasnov AN, Deykin AV, Popov AN, Ermolkevich TG, Budzevich AI, Chernousov AD, Sadchikova ER (2012) Production of human lactoferrin in animal milk. Biochem Cell Biol 90:513–519. https://doi.org/10.1139/o11-088
Gonzalez-Avila G, Sommer B, Mendoza-Posada DA, Ramos C, Garcia-Hernandez AA, Falfan-Valencia R (2019) Matrix metalloproteinases participation in the metastatic process and their diagnostic and therapeutic applications in cancer. Crit Rev Oncol Hematol 137:57–83. https://doi.org/10.1016/j.critrevonc.2019.02.010
Grada A, Otero-Vinas M, Prieto-Castrillo F, Obagi Z, Falanga V (2017) Research techniques made simple: analysis of collective cell migration using the wound healing assay. J Invest Dermatol 137:e11–e16. https://doi.org/10.1016/j.jid.2016.11.020
Guan X (2015) Cancer metastases: challenges and opportunities. Acta Pharm Sin B 5:402–418. https://doi.org/10.1016/j.apsb.2015.07.005
Ha NH, Nair VS, Reddy DN, Mudvari P, Ohshiro K, Ghanta KS, Pakala SB, Li DQ, Costa L, Lipton A, Badwe RA, Fuqua S, Wallon M, Prendergast GC, Kumar R (2011) Lactoferrin-endothelin-1 axis contributes to the development and invasiveness of triple-negative breast cancer phenotypes. Cancer Res 71:7259–7269. https://doi.org/10.1158/0008-5472.Can-11-1143
Hulkower KI, Herber RL (2011) Cell migration and invasion assays as tools for drug discovery. Pharmaceutics 3:107–124. https://doi.org/10.3390/pharmaceutics3010107
Iigo M, Kuhara T, Ushida Y, Sekine K, Moore MA, Tsuda H (1999) Inhibitory effects of bovine lactoferrin on colon carcinoma 26 lung metastasis in mice. Clin Exp Metastasis 17:35–40. https://doi.org/10.1023/a:1026452110786
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458. https://doi.org/10.1038/bmt.2012.244
Katt ME, Placone AL, Wong AD, Xu ZS, Searson PC (2016) In vitro tumor models: advantages, disadvantages, variables, and selecting the right platform. Front Bioeng Biotechnol 4:12. https://doi.org/10.3389/fbioe.2016.00012
Kruzel ML, Actor JK, Zimecki M, Wise J, Płoszaj P, Mirza S, Kruzel M, Hwang SA, Ba X, Boldogh I (2013) Novel recombinant human lactoferrin: differential activation of oxidative stress related gene expression. J Biotechnol 168:666–675. https://doi.org/10.1016/j.jbiotec.2013.09.011
Lintz M, Muñoz A, Reinhart-King CA (2017) The mechanics of single cell and collective migration of tumor cells. J Biomech Eng 139:0210051–0210059. https://doi.org/10.1115/1.4035121
Matsuzaki T, Nakamura M, Nogita T, Sato A (2019) Cellular uptake and release of intact lactoferrin and its derivatives in an intestinal enterocyte model of Caco-2 Cells. Biol Pharm Bull 42:989–995. https://doi.org/10.1248/bpb.b19-00011
Noro R, Gemma A, Kosaihira S, Kokubo Y, Chen M, Seike M, Kataoka K, Matsuda K, Okano T, Minegishi Y, Yoshimura A, Kudoh S (2006) Gefitinib (IRESSA) sensitive lung cancer cell lines show phosphorylation of Akt without ligand stimulation. BMC Cancer 6:277. https://doi.org/10.1186/1471-2407-6-277
Oh SM, Hahm DH, Kim IH, Choi SY (2001) Human neutrophil lactoferrin trans-activates the matrix metalloproteinase 1 gene through stress-activated MAPK signaling modules. J Biol Chem 276:42575–42579. https://doi.org/10.1074/jbc.M107724200
Schegoleva AA, Khozyainova AA, Gerashchenko TS, Zhuikova LD, Denisov EV (2022) Metastasis prevention: targeting causes and roots. Clin Exp Metastasis. https://doi.org/10.1007/s10585-022-10162-x
Ueda K, Shimizu M, Ohashi A, Murata D, Suzuki T, Kobayashi N, Baba J, Takeuchi T, Shiga Y, Nakamura M, Kagaya S, Sato A (2020) Albumin fusion at the N-terminus or C-terminus of human lactoferrin leads to improved pharmacokinetics and anti-proliferative effects on cancer cell lines. Eur J Pharm Sci 155:105551. https://doi.org/10.1016/j.ejps.2020.105551
Wei L, Zhang X, Wang J, Ye Q, Zheng X, Peng Q, Zheng Y, Liu P, Zhang X, Li Z, Liu C, Yan Q, Li G, Ma J (2020) Lactoferrin deficiency induces a pro-metastatic tumor microenvironment through recruiting myeloid-derived suppressor cells in mice. Oncogene 39:122–135. https://doi.org/10.1038/s41388-019-0970-8
Yoo YC, Watanabe S, Watanabe R, Hata K, Shimazaki K, Azuma I (1997) Bovine lactoferrin and lactoferricin, a peptide derived from bovine lactoferrin, inhibit tumor metastasis in mice. Jpn J Cancer Res 88:184–190. https://doi.org/10.1111/j.1349-7006.1997.tb00364.x
Zlatina K, Galuska SP (2021) The N-glycans of lactoferrin: more than just a sweet decoration. Biochem Cell Biol 99:117–127. https://doi.org/10.1139/bcb-2020-0106
Acknowledgements
The authors thank Hiroto Ishida (School of Bioscience and Biotechnology, Tokyo University of Technology) for providing technical assistance. We are grateful to Prof. Yuko Murakami (School of Bioscience and Biotechnology, Tokyo University of Technology), Dr. Misa Imai (Graduate School of Medicine, Juntendo University, Tokyo, Japan), and Dr. Masao Nakamura (Sasaki Institute, Sasaki Foundation, Tokyo, Japan) for their useful discussions.
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
HN: investigation, writing, review, and editing. DK: investigation and review. AS: conceptualization, writing, reviewing, editing, and supervision. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
A. Sato was the founder of S&K Biopharma Inc. (Kawasaki, Kanagawa, Japan).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nopia, H., Kurimoto, D. & Sato, A. Albumin fusion with human lactoferrin shows enhanced inhibition of cancer cell migration. Biometals 36, 629–638 (2023). https://doi.org/10.1007/s10534-022-00447-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10534-022-00447-9