Abstract
The anti-metastatic effect of curcumin on papillary thyroid cancer K1 cells and its underlying mechanisms were investigated. Curcumin at 12.5, 25 and 50 μM promoted mesenchymal–epithelial transition and decreased the migration rate of K1 cells by 24–87 %. Its mechanism may involve the up-regulation of E-cadherin expression levels and down-regulation of the activity and expression of matrix metalloproteinase-9.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Papillary thyroid carcinoma (PTC) is the most frequently occurring form of differentiated thyroid cancer. Although the prognosis for PTC using traditional therapies is usually good, PTC can undergo de-differentiation and progression to become a anaplastic carcinoma, a formidable disease characterised by widespread invasion and early distant metastasis (Zuo et al. 2010). The loss of intercellular adhesion and acquisition of degradative properties are prerequisites for tumour cells to become fully invasive (Nawrocki-Raby et al. 2003), which is the beginning of metastasis. As a result, there is significant interest in developing an agent with the potential to restrain both of these prerequisites and thus inhibit metastasis.
An accumulating body of data supports the concept that phytochemicals in the human diet are devoid of toxicity and may have numerous long-lasting beneficial effects on human health (Shankar and Srivastava 2012). Considering its unique anti-metastatic property and low toxicity, curcumin (diferuloylmethane), the chief component of the spice turmeric and derived from the rhizome of the East Indian plant Curcuma longa, is one such potential candidate. Curcumin has been demonstrated to affect a number of the cellular adhesion molecules that are involved in the processes of metastasis (Ray et al. 2003), such as E-cadherin. E-cadherin expression is important in maintaining the integrity of intercellular adhesion through binding to various catenins (including β-catenin), and the loss of E-cadherin is associated with an increased tendency for tumour metastasis (Onder et al. 2008). In addition, the degradation of the basement membrane and extracellular matrix occurs primarily through matrix metalloproteinases (MMPs). Of these proteases, the expression of MMP-9 and -2 is high in various malignant tumours, and is closely related to the ability of these cells to invade and metastasise (Weng and Yen 2012). Many reports have shown that curcumin inhibits the expression of MMP-9 both in vitro and in vivo (Kunnumakkara et al. 2008).
As curcumin has an ill-defined effect on the metastasis of PTC and related mechanisms, in this paper we show how it affects the epithelial–mesenchymal transition (EMT) and cell migration involved in cell metastasis. We further discuss its impact on E-cadherin and MMPs.
Materials and methods
Reagents
Curcumin (purity ≥94 %), dimethyl sulfoxide, concanavalin A, propidium iodide and Hoechst 33342 were from Sigma. Dulbecco’s Modified Eagle Medium (DMEM) and foetal bovine serum (FBS) were purchased from Gibco (Logan, UT, USA) and Sijiqing Biological Engineering Materials Co Ltd. (Hangzhou, China), respectively. Bovine serum albumin (BSA) was purchased from Sangon (Shanghai, China). All other chemicals were analytical reagents, and purchased from Sinopharm Chemical Reagent Co Ltd. (Shanghai). Curcumin was dissolved in DMSO at 10 mg/ml, and stored at −20 °C until dilution before use.
Cell line and culture conditions
Papillary thyroid cancer cell line K1 was obtained from the European Collection of Cell Cultures and maintained in DMEM containing 10 % (v/v) FBS, 100 U penicillin/ml and 100 U streptomycin/ml in a humid atmosphere of 5 % (v/v) CO2 and 95 % (v/v) air at 37 °C. K1 cells in the log phase were plated in cell culture plates (Corning, NY, USA). Control cells were treated with the same medium, but without curcumin or solvent. The solvent control contained an equivalent amount of DMSO corresponding to the highest used concentration of curcumin.
Cell viability assay
Cell viability was determined by propidium iodide and Hoechst 33342 staining (see Song et al. 2012).
Cell spreading assay
Ninety-six-well culture plates were coated with concanavalin A (Con A; 25 μg/ml) in phosphate-buffered saline (PBS) overnight at 4 °C, blocked with 0.2 % BSA for 2 h at room temperature and then washed twice with PBS. The cells were harvested with trypsin/EDTA, washed twice and resuspended in DMEM at 8 × 104 cells/ml. Then, to 100 μl cells different concentrations of curcumin (12.5, 25 and 50 μM) were added. The plates were incubated for another 2 h at 37 °C, and then photographed.
Migration assay
The transwell migration assay was performed as described previously (Rajoria et al. 2011) with some modification.
Gelatin zymography
Zymography assay was performed as described previously (Forsyth et al. 1999) with some modification.
Western blot assay
K1 cells pretreated with curcumin (12.5, 25 or 50 μM) were incubated for 24 h. A western blot was then performed (see Song et al. 2012). The antibodies were anti-β-actin (1:1,000, v/v), anti-E-cadherin (1:1,000, v/v) or anti-MMP-9 (1:100, v/v) (Santa Cruz Biotechnology, CA, USA) and an appropriate horseradish peroxidase-conjugated secondary antibody (goat anti-mouse IgG, 1:500, 1:500 or 1:250, respectively) (Santa Cruz Biotechnology).
Statistical analysis
The results were expressed as mean ± standard errors (SE), and three group comparisons were evaluated using the Student’s t test. Differences were considered statistically significant at P < 0.05.
Results
Curcumin inhibits the cell viability of K1 cells
Figure 1a shows that the number of red-emitting fluorescent cells increased as the curcumin concentration increased. Compared to the control groups, treatment with curcumin at 12.5 and 25 μM increased the cell death rate to 2.6 ± 0.02 % (P = 4.96e−1) and 5.5 ± 0.05 % (P = 2.33e−1), respectively, whilst at 50 μM, it increased the death rate to 21.6 ± 0.04 % (P = 6.17e−3 < 0.01). Figure 1c shows that 50 μM curcumin also inhibited cell viability in a time-dependent manner after 24 h of treatment.
Effects of curcumin on the cell viability of K1 cells. Cells were incubated with or without curcumin (12.5, 25 and 50 μM) for 24 h at 37 °C and stained by propidium iodide and Hoechst 33342. All data are represented as the mean ± SE of three independent experiments. SC solvent control. **P < 0.01 versus SC (Student’s two tailed t test)
Curcumin inhibits K1 cell spreading
As illustrated in Fig. 2a, all cells treated with solvent alone spread out with large and flat lamellipodia. 12.5 μM curcumin had a modest effect on the morphology of cell spreading (Fig. 2b). However, curcumin 25 μM partially inhibited cell spreading on Con A, as can be seen from the arrows in Fig. 2c. Moreover, in Fig. 2d, the cells pre-treated with 50 μM curcumin were small and round.
Effects of curcumin on K1 cell spreading. Cells with or without different concentrations of curcumin (12.5, 25 and 50 μM) were added to plates pre-coated with Con A (25 μg/ml), incubated for an additional 2 h at 37 °C and then photographed with a microscope. Arrows indicate non-spreading cells. SC solvent control
Curcumin inhibits K1 cell migration
Figure 3A, B shows that curcumin significantly inhibited cell migration in a dose-dependent manner in this study. After cells had been treated with 12.5, 25 or 50 μM curcumin, the migration rate of the K1 cells through the membrane decreased to 87.4 ± 12 % (P = 3.55e−1), 45 ± 1.3 % (P = 1.68e−6 < 0.01), 24.2 ± 5.8 % (P = 2e−4 < 0.01), respectively.
Effects of curcumin on cell migration. Cancer cell migration ability was examined using a transwell system. After being serum-starved for 24 h, cells with or without curcumin (12.5, 25 and 50 μM) were seeded onto the upper wells of transwells, while a conditional medium (DMEM with 10 % FBS) was added to the lower wells. Cells were incubated at 37 °C for 3 h. A Morphology of cells stained with Hoechst 33342 and inspected with a fluorescence microscope. B Quantification of cells attached to the lower surface of the polycarbonate filter. All data are represented as the mean ± SE of three independent experiments. SC solvent control. *P < 0.05 versus SC. **P < 0.01 versus SC (Student’s two tailed t test)
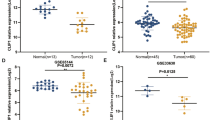
Curcumin up-regulates the expression of E-cadherin
Figure 4 shows that curcumin increased the expression of E-cadherin in a dose-dependent manner. In particular, the protein expression level of E-cadherin increased significantly when the cells were treated with 50 μM curcumin.
Effects of curcumin on expression of E-cadherin. Western blot analysis of the expression level of E-cadherin of cells pretreated with or without curcumin (12.5, 25, 50 μM) for 24 h. Beta-actin was used as a loading control. All data are represented as the mean ± SE of three independent experiments. SC solvent control. *P < 0.05 versus control. **P < 0.01 versus control (Student’s two tailed t test)
Curcumin down-regulates the activity and expression of MMP-9
Figure 5a shows that the activity of MMP-9 was notably inhibited by curcumin in a dose-dependent manner compared with the controls. In addition, we tested protein expression of MMP-9 through a western blot assay and found that the cytoplasmic expression level of MMP-9 was also down-regulated by curcumin (Fig. 5b). More importantly, at curcumin up to 50 μM, almost no obvious MMP-9 expression was observed.
Effects of curcumin on the activity and expression of MMP-9. a Gelatin zymography analysis of the activity of MMP-9 of cells pretreated with or without curcumin (12.5, 25 and 50 μM) for 24 h. b Western blot analysis of the expression level of MMP-9 of cells pretreated with or without curcumin (12.5, 25 and 50 μM) for 24 h. An equal amount of total proteins was loaded into each lane. All data are represented as the mean ± SE of three independent experiments. SC solvent control. *P < 0.05 versus control. **P < 0.01 versus control (Student’s two tailed t test)
Discussion
Over the past several years, concerted efforts have been made to define the pathways involved in invasion and metastasis, and it has been suggested that the reactivation of embryonic pathways could promote cell movement and induce epithelial to mesenchymal transition and collective cell migration (Vasko and Saji 2007). In a previous study, we found that curcumin could induce apoptosis in K1 papillary thyroid cancer cells (Song et al. 2012). In this paper, we further discuss how it affects EMT and the cell migration involved in cell metastasis.
We found treatment with curcumin induced dramatic morphological changes in K1 cells, which altered from a spindle-like, mesenchymal phenotype to become a more pronounced epithelial phenotype (Fig. 2). Moreover, the results of cell migration using the transwell assay showed curcumin to have a unique anti-migration property, as evidenced by the very high inhibition rate on K1 cell migration of 25–50 μM of curcumin treatment (Fig. 3). These results suggest that curcumin has the ability to suppress both the epithelial to mesenchymal transition of K1 cells and cell migration.
The disorganisation of E-cadherin/catenin complexes and the overexpression of MMPs are frequently involved in epithelial cells’ ability to acquire an invasive phenotype (Nawrocki-Raby et al. 2003). An agent that can efficiently inhibit the loss of E-cadherin and the overexpression of MMPs would then be an ideal candidate for the suppression of cancer progression. Our data demonstrate that curcumin may exert these effects on thyroid cancer (Figs. 4 and 5). Zymography analysis revealed a loss of MMP-9 activation ability after curcumin treatment. Moreover, the up-regulation of the E-cadherin expression level rose in K1 cells treated with curcumin.
These effects of curcumin on E-cadherin and MMP-9 expression have been reported in many other cancers. For example, decreased migration and invasion was observed in osteosarcoma cells after treatment with curcumin, and that decrease was correlated with the activity and protein level of MMP-9 (Leow et al. 2010). Another study found that curcumin could inhibit lung cancer cell invasion and metastasis by modulating E-cadherin expression (Chen et al. 2008). Moreover, a study of invasive bronchial tumour cells demonstrated that E-cadherin transfection could down-regulate MMP expression (Nawrocki-Raby et al. 2003). However, the connections between E-cadherin and MMP-9 in papillary thyroid cancer and the signal transduction pathways involved in these processes are not well known. We present novel data on the anti-metastasis mechanism of curcumin, which will benefit our further research into the treatment of thyroid cancer via naturally occurring phytochemicals.
Conclusion
We provide the first evidence of curcumin’s ability to promote mesenchymal–epithelial transition and decrease tumour cell migration that is involved in the invasion and metastasis of papillary thyroid cancer. Its anti-metastatic mechanism may be involved in up-regulating E-cadherin expression levels and down-regulating the activity and expression of MMP-9. These data suggest that curcumin is a potential preventive agent for the adjuvant treatment of thyroid cancers.
References
Chen H-W, Lee J-Y, Huang J-Y, Wang C-C, Chen W-J, Su S-F, Huang C-W, Ho C-C, Chen JJW, Tsai M-F, Yu S-L, Yang P-C (2008) Curcumin inhibits lung cancer cell invasion and metastasis through the tumor suppressor HLJ1. Cancer Res 68:7428–7438
Forsyth PA, Wong H, Laing TD, Rewcastle NB, Morris DG, Muzik H, Leco KJ, Johnston RN, Brasher PM, Sutherland G, Edwards DR (1999) Gelatinase-A (MMP-2), gelatinase-B (MMP-9) and membrane type matrix metalloproteinase-1 (MT1-MMP) are involved in different aspects of the pathophysiology of malignant gliomas. Br J Cancer 79:1828–1835
Kunnumakkara AB, Anand P, Aggarwal BB (2008) Curcumin inhibits proliferation, invasion, angiogenesis and metastasis of different cancers through interaction with multiple cell signaling proteins. Cancer Lett 269:199–225
Leow PC, Tian Q, Ong ZY, Yang Z, Ee PL (2010) Antitumor activity of natural compounds, curcumin and PKF118-310, as Wnt/beta-catenin antagonists against human osteosarcoma cells. Invest New Drugs 28:766–782
Nawrocki-Raby B, Gilles C, Polette M, Martinella-Catusse C, Bonnet N, Puchelle E, Foidart JM, Van Roy F, Birembaut P (2003) E-Cadherin mediates MMP down-regulation in highly invasive bronchial tumor cells. Am J Pathol 163:653–661
Onder TT, Gupta PB, Mani SA, Yang J, Lander ES, Weinberg RA (2008) Loss of E-cadherin promotes metastasis via multiple downstream transcriptional pathways. Cancer Res 68:3645–3654
Rajoria S, Suriano R, George A, Shanmugam A, Schantz SP, Geliebter J, Tiwari RK (2011) Estrogen induced metastatic modulators MMP-2 and MMP-9 are targets of 3,3′-diindolylmethane in thyroid cancer. PLoS One 6:e15879
Ray S, Chattopadhyay N, Mitra A, Siddiqi M, Chatterjee A (2003) Curcumin exhibits antimetastatic properties by modulating integrin receptors, collagenase activity, and expression of Nm23 and E-cadherin. J Environ Pathol Tox 22:49–58
Shankar S, Srivastava RK (2012) Curcumin: structure, biology and clinical applications. In: Shankar S, Srivastava RK (eds) Nutrition, diet and cancer, 1st edn. Springer, Netherlands, pp 413–457
Song F, Zhang L, Yu H-X, Lu R-R, Bao J-D, Tan C, Sun Z (2012) The mechanism underlying proliferation-inhibitory and apoptosis-inducing effects of curcumin on papillary thyroid cancer cells. Food Chem 132:43–50
Vasko VV, Saji M (2007) Molecular mechanisms involved in differentiated thyroid cancer invasion and metastasis. Curr Opin Oncol 19:11–17
Weng CJ, Yen GC (2012) Chemopreventive effects of dietary phytochemicals against cancer invasion and metastasis: phenolic acids, monophenol, polyphenol, and their derivatives. Cancer Treat Rev 38:76–87
Zuo H, Gandhi M, Edreira MM, Hochbaum D, Nimgaonkar VL, Zhang P, DiPaola J, Evdokimova V, Altschuler DL, Nikiforov YE (2010) Downregulation of Rap1GAP through epigenetic silencing and loss of heterozygosity promotes invasion and progression of thyroid tumors. Cancer Res 70:1389–1397
Acknowledgments
This study was supported by grants from the National Natural Science Foundation of China (Nos. 31071491 and 31171627), Program for New Century Excellent Talents in University (NCET-09-0436), Natural Science Foundation of Jiangsu Province (No. BK2010156) and “Twelfth 5-year” National Key Technology R&D Program of China (2012BAD33B05).
Author information
Authors and Affiliations
Corresponding author
Additional information
Chi-Yu Zhang and Li Zhang contributed equally to the study.
Rights and permissions
About this article
Cite this article
Zhang, CY., Zhang, L., Yu, HX. et al. Curcumin inhibits the metastasis of K1 papillary thyroid cancer cells via modulating E-cadherin and matrix metalloproteinase-9 expression. Biotechnol Lett 35, 995–1000 (2013). https://doi.org/10.1007/s10529-013-1173-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10529-013-1173-y