Abstract
Mutations in mitochondrial DNA (mtDNA) are one of the most important causes of hearing loss. Of these, the homoplasmic A1555G and C1494T mutations at the highly conserved decoding site of the 12S rRNA gene are well documented as being associated with either aminoglycoside-induced or nonsyndromic hearing loss in many families worldwide. Moreover, five mutations associated with nonsyndromic hearing loss have been identified in the tRNASer(UCN) gene: A7445G, 7472insC, T7505C, T7510C, and T7511C. Other mtDNA mutations associated with deafness are mainly located in tRNA and protein-coding genes. Failures in mitochondrial tRNA metabolism or protein synthesis were observed from cybrid cells harboring these primary mutations, thereby causing the mitochondrial dysfunctions responsible for deafness. This review article provides a detailed summary of mtDNA mutations that have been reported in deafness and further discusses the molecular mechanisms of these mtDNA mutations in deafness expression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
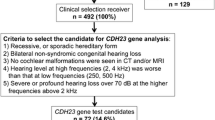
Hearing loss is one of the most common sensory disorders, affecting approximately 120 million patients all over the world. About 30% of them have syndromic hearing loss, and the remaining 70% have nonsyndromic hearing loss. In addition, a large number of elderly people worldwide suffer from age-related (late-onset) hearing loss (Lalwani and Gürtler 2008; Brown et al. 2008; Gratton and Vázquez 2003). Hearing loss can be caused by genetic and environmental factors; genetic factors account for at least half of all cases of profound congenital deafness, and single gene mutations can also lead to hearing loss (Nance 2003). It has been estimated that more than 50% of pediatric cases have a genetic etiology with autosomal dominant (DFNA), autosomal recessive (DFNB), X-linked (DFN), or mitochondrial mode of inheritance (Jacobs et al. 2005; Guan 2011). Although most hereditary hearing loss is caused by a deficiency in nuclear genes, it has become clear that mitochondrial genes also play important roles in deafness expression. Mitochondrial DNA mutations have been found to be associated with both maternally inherited syndromic and nonsyndromic hearing loss worldwide (Fischel-Ghodsian 1999; Guan 2011). This review summarizes the basic knowledge of mitochondrial genetics and the most common mtDNA mutations associated with deafness. We also briefly discuss the molecular mechanisms by which mtDNA mutations lead to human hearing loss.
The Mitochondrial Genome and Mitochondrial Genetics
Mitochondria are ubiquitous organelles in eukaryotic cells. Their primary role is to generate energy (i.e., ATP) through oxidative phosphorylation (Attardi and Schatz 1988). They have their own DNA, known as mtDNA, encoding certain essential components of mitochondrial respiratory chain and protein synthesis apparatus. Human mtDNA is a double-stranded, circular molecule (Fig. 1) encoding 13 protein subunits of 4 biochemical complexes and 24 structural RNAs (2 ribosomal RNAs and 22 transfer RNAs) that are responsible for intramitochondrial translation of protein-coding units (Anderson et al. 1981).
Mitochondrial DNA is inherited maternally and does not recombine; mutations thus accumulate sequentially through maternal lineages. Each mitochondrion contains 2–10 DNA molecules, and each cell contains multiple mitochondria. Since mtDNA is in the proximity of reactive oxygen species generation sites and mitochondria have relatively less sophisticated DNA protection and repair systems, it is therefore vulnerable to high mutation rates (DiMauro and Schon 2001). If all the mtDNAs in a cell are identical, the cell status is referred to as “homoplasmy”; if not, it is called “heteroplasmy.” Neutral polymorphisms are usually homoplasmic, whereas pathogenic mutations are usually heteroplasmic in nature (Table 1), and mtDNA mutations associated with deafness are generally homoplasmic or almost homoplasmic (>85%) (Fischel-Ghodsian 1999; Fischel-Ghodsian et al. 2004).
Mitochondrial 12S rRNA Mutations and Ototoxic Hearing Loss
Aminoglycosides (such as gentamicin, kanamycin, and streptomycin) were first discovered in the 1940s and used for the treatment of tuberculosis and bacterial infections (Schacht 1993). The ototoxic and nephrotoxic effects of aminoglycosides, however, still do not receive enough attention in developing countries. Patients treated with aminoglycosides may exhibit a high frequency of sensorineural hearing loss that is permanent and bilateral. In familial cases of ototoxic hearing loss, aminoglycoside hypersensitivity is often maternally transmitted, suggesting that mutations in mtDNA are the molecular basis for this susceptibility (Fischel-Ghodsian 1999). Since the first report that the 12S rRNA A1555G mutation played an active role in aminoglycoside-induced and nonsyndromic hearing loss (Prezant et al. 1993), many efforts have been carried out to identify other potential mtDNA pathogenic mutations associated with aminoglycoside ototoxicity (Fischel-Ghodsian et al. 2004). In fact, the A1555G mutation is located at the aminoacyl-tRNA acceptor site (A-site) of the small ribosomal subunit, which is highly conserved from bacteria to mammals (Ruiz-Pesini and Wallace 2006). This mutation has been found in many families with maternally inherited, nonsyndromic hearing loss and also in patients with hearing loss after the use of aminoglycosides. In an Arab–Israeli family carrying the A1555G mutation, under a constant nuclear background, average reductions of 35 and 37% in the rate of mitochondrial protein synthesis were observed in cybrid cell lines derived from asymptomatic or symptomatic individuals in this family (Guan et al. 2001).
The 12S rRNA C1494T mutation has been found to be associated with aminoglycoside-induced and nonsyndromic hearing loss in some Chinese and Spanish families (Zhao et al. 2004, 2005a; Rodriguez-Ballesteros et al. 2006; Wang et al. 2006; Chen et al. 2007). It is interesting to note that in the human mitochondrial 12S rRNA, C1494 forms a noncanonical RNA base pair with the adenine encoded by the 12S rRNA position 1555, both of them located in the A-site of the 12S rRNA (Ogle and Ramakrishnan 2005). The region of the 16S rRNA in Escherichia coli, corresponding to that of the human mitochondrial 12S rRNA A-site (Fig. 2), is the target for the aminoglycoside antibioitic (Recht et al. 1996; Fourmy et al. 1996) and is crucial for subunit association either by RNA–protein or RNA–RNA interaction (Zwieb et al. 1986). Moreover, the sensitivity to aminoglycosides involves their direct binding to a C–G base pair at positions 1409–1491 of the penultimate helix in the small ribosomal subunit rRNA (Purohit and Stern 1994). This transition makes the secondary structure of rRNA more closely resemble the corresponding region of Escherichia coli 16S rRNA. Similarly, the new G–C pair in 12S rRNA is expected to create a binding site for aminoglycoside, which facilitates the binding of these drugs (Hamasaki and Rando 1987) and causes the mistranslation or premature termination of protein synthesis (Chamber and Sande 1996; Davies and Davis 1968). As a result, the exposure to aminoglycosides can induce or aggravate hearing loss in individuals carrying one of these mutations.
The association of the 12S rRNA T1095C mutation (conservation index 93%) with deafness is controversial. This mutation has been found in several genetically unrelated families with nonsyndromic hearing loss (Tessa et al. 2002; Zhao et al. 2005b; Wang et al. 2005). The T1095C mutation was first identified in a family with hearing loss and neuropathic symptoms (Thyagarajan et al. 2000). Phylogenetic analysis of this mutation reveals it to be a genetic polymorphism, unlikely to be of pathogenic significance (Yao et al. 2006).
The 961insC mutation is a deletion of a single T with an insertion of a varying number of Cs in the 12S rRNA gene. In a recent study of 1,642 Han Chinese pediatric subjects with hearing loss, this mutation accounted for 1.8% in this genetic population (Lu et al. 2010a). Although it is postulated that alteration of the tertiary structure of 12S rRNA caused by 961insC may affect the binding of aminoglycoside (Guan 2005), its functional role needs to be further addressed experimentally.
Mitochondrial tRNASer(UCN): Hot Spot for Pathogenic Mutations with Deafness
Mutations in the gene encoding tRNASer(UCN) have been implicated with the development of sensorineural hearing loss. They include A→G (T or C) at position 7445 (Fischel-Ghodsian et al. 1995; Reid et al. 1994), the insertion of a new cytidine at position 7472 (Verhoeven et al. 1999; Jacobs et al. 2005), T→C transition at positions 7505 (Tang et al. 2010), 7510 (Hutchin et al. 2000; del Castillo et al. 2002; Labay et al. 2008), and 7511 (Sue et al. 1999; Li et al. 2005a). These mutations often occur in homoplasmy or in high levels of heteroplasmy, indicating a high threshold for pathogenicity. It is believed that mutations in this gene can cause a failure in tRNA metabolism, thereby altering mitochondrial translation and respiration (Guan et al. 1998; Li et al. 2004).
The homoplasmic A7445G mutation in the precursor of tRNASer(UCN) was first identified in New Zealand, Ukraine, Japanese, and Mongolian families with nonsyndromic deafness (Fischel-Ghodsian et al. 1995; Hutchin et al. 2000; Pandya et al. 1999). Structurally, this mutation is located at the stop codon (AGA) of the mRNA encoding CO1 on the H-strand. As the AGA normal codon is replaced by an AGG stop codon, however, the A7445G mutation has no effect on CO1 expression. Therefore, this mutation leaves the structure of the tRNASer(UCN) intact but affects the rate of processing of the tRNASer(UCN) precursor, which results in a reduction in tRNASer(UCN) level and also leads to a significant reduction in the amount of ND6 mRNA and protein synthesis (Guan et al. 1998; Reid et al. 1997; Li et al. 2005b). Alternatively, the A7445T or A7445C mutation is adjacent to the 3′ end site of endonucleolytic processing of the L-strand RNA precursor, spanning tRNASer(UCN) and ND6 mRNA, and may also affect the processing of the L-strand RNA precursor, causing mitochondrial dysfunction (Chen et al. 2008).
The 7472insC mutation in tRNASer(UCN) was originally described in a Sicilian family (Tiranti et al. 1995). In a large Dutch family, this mutation was found to be responsible for the nonsyndromic hearing loss in all family members; one individual in this family exhibited the syndrome of hearing loss, ataxia, and myoclonus. This mutation templates the insertion of an extra G into a run of six G residues, located within the T arm and extra arm of tRNASer(UCN) (Verhoeven et al. 1999; Tiranti et al. 1995). It impairs the 5′ and 3′ processing of tRNASer(UCN) (Toompuu et al. 2004) and decreases the steady-state level of this tRNA post-transcriptionally (Toompuu et al. 1999). Cybrid cells harboring the 7472insC mutation exhibit a significant decrease (70%) of tRNASer(UCN) abundance by affecting its synthesis rather than the stability of its structure, also causing a mild decline (25%) in steady-state aminoacylation of tRNASer(UCN) (Toompuu et al. 2004).
The homoplasmic T7505C mutation was reported from a Han Chinese pedigree with maternally inherited nonsyndromic hearing loss (Tang et al. 2010). This mutation is located at the second base-pairing (10A–20U) in the D stem of tRNA (Florentz et al. 2003). Functional analysis of cybrid cells showed that the T7505C mutation reduced the level of tRNASer(UCN) by 65%, thus impairing mitochondrial protein synthesis (Tang et al. 2010).
The T7510C and T7511C mutations occur at the acceptor arm of tRNA and disrupt the highly conserved secondary structure of tRNASer(UCN). The T7511C mutation has been identified in African (Sue et al. 1999; Friedman et al. 1999), French (Chapiro et al. 2002), and Japanese families (Ishikawa et al. 2002) with nonsyndromic hearing loss. In a large African family carrying the T7511C mutation, in conjunction with homoplasmic ND1 T3308C and tRNAAla T5655C mutations, 75–83% reductions in the level of tRNASer(UCN) were observed in cybrid cells carrying the T7511C mutation (Li et al. 2004). The T5655C mutation caused a 50% reduction in the tRNAAla level, which may result in a failure to aminoacylate properly and in post-transcriptional modification of this tRNA. A significant reduction in steady-state levels of both ND1 mRNA and the adjacent tRNALeu(UUR) observed in the cybrids carrying the T3308C mutation is likely due to an alteration in the processing of the H-strand polycistronic RNA precursors or the destabilization of ND1 mRNA (Rossmanith et al. 1995). Therefore, combined with the T3308C and T5655C mutations, the T7511C mutation accounts for a high penetrance of deafness in this African family (Li et al. 2004).
Other mtDNA Mutations Associated with Deafness
G1606A in the tRNAVal Gene
The heteroplasmic tRNAVal G1606A mutation was first identified in a 48-year-old man with bilateral hearing loss, vision loss, and mild muscle weakness (Tiranti et al. 1998). Later, Sacconi et al. (2002) described a 37-year-old woman with hearing loss, ataxia, retinitis pigmentosa, and hypothyroidism. This mutation was located on the acceptor arm of tRNAVal; genotype-phenotype analysis suggested that it may be related not only to changes in the DNA sequence but also to disruptions in the secondary and tertiary structure of tRNAVal (Schon et al. 1997). Moreover, analysis of single muscle fibers revealed a significantly greater level of mutant mtDNA in cytochrome c oxidase-negative fibers, suggesting that this mutation is involved in the pathogenesis of clinical diseases.
A3243G in the tRNALeu(UUR) Gene
The heteroplasmic A3243G mutation has been reported to be associated with maternally inherited diabetes and deafness syndrome (Maassen 2004; Ohkubo et al. 2001; van den Ouweland et al. 1992). The primary defect in this mutation is an inefficient aminoacylation of tRNALeu(UUR) (Chomyn et al. 2000; El Meziane et al. 1998). In addition, this mutation affects the processing of mitochondrial RNA precursors (Rossmanith and Karwan 1998). The deficiency of aminoacylation of tRNALeu(UUR) mainly contributes to a shortage of tRNALeu(UUR) (Li and Guan 2010), thereby causing a reduced rate of mitochondrial protein synthesis and respiration defects (King et al. 1992; Janssen et al. 2007).
A4295G in the tRNAIle Gene
McFarland et al. (2004) provided a program for assigning a pathogenicity score to mt-tRNA mutations. Their weighting scoring system was revised in 2011 (Yarham et al. 2011), and it predicted the A4295G mutation to be definitely pathogenic. The homoplasmic A4295G mutation reduces the efficiency with which tRNAIle can be processed by 3′-tRNase, decreases the level of functional tRNAIle (Levinger et al. 2003), and thereby leads to the defects in mitochondrial translation (Gutiérrez Cortés et al. 2012).
G8363A in the tRNALys Gene
The heteroplasmic G8363A mutation was first identified in two unrelated families carrying a syndrome consisting of encephalomyopathy, sensorineural hearing loss, and hypertrophic cardiomyopathy (Santorelli et al. 1996). Moreover, Virgilio et al. (2009) reported a large Italian family with heterogeneous mitochondrial disease phenotypes associated with the G8363A mutation. This mutation abolishes a highly conserved base-pairing at the acceptor arm of tRNALys; the absence of a hydrogen-bonded base pair at the end of the acceptor stem is likely to impair the activity of peptidyl-tRNA hydrolase, which is critical for protein translation (Dutka et al. 1993). Defects in oxidative phosphorylation metabolism were observed in muscle biopsies from a patient with the G8363A mutation, suggesting a direct pathogenic role.
T12201C in the tRNAHis Gene
The heteroplasmic T12201C mutation was originally detected in a large Chinese family with high penetrance of hearing impairment (Yan et al. 2011). The T→C transition at position 12201 disrupts a very conservative base-pairing (5A–68U) in the acceptor arm of tRNAHis and causes a failure in tRNA metabolism. Functional characterization of a cell line derived from T12201C mutation reveals a 75% reduction in the tRNAHis steady-state level, thus impairing mitochondrial translation.
ND1 C3388A and CO2 G8078A: Novel Pathogenic Mutations with Deafness
Previously, Lévêque et al. (2007) identified several novel candidate mtDNA mutations, localized in a variety of mitochondrial genes, found in patients with deafness. Of these, the homoplasmic C3388A mutation, which affects the gene encoding the ND1 subunit, causes a significant decrease in complex I protein level. The G8078A mutation results in mild defects of the respiratory chain complex IV. These findings indicate that mutations in protein-coding genes can also be responsible for nonsyndromic hearing loss (Gutiérrez Cortés et al. 2012).
Mitochondrial Secondary Variants
Variable phenotypes of hearing loss within and among the families carrying A1555G or A7445G mutations indicate the involvement of mitochondrial secondary variants (Lu et al. 2010b; Maász et al. 2008). In a recent mutational screening of 1,642 pediatric subjects with hearing loss from Zhejiang Province in China, 69 families exhibited the homoplasmic A1555G mutation; in particular, nine mitochondrial secondary variants (tRNAThr G15927A, T15908C, tRNASer(UCN) G7444A, ND5 T12338C, tRNAGlu A14693G, tRNAArg T10454C, tRNASer(AGY) C12224T, tRNACys T5802C, G5821A) were implicated in enhancing the penetrance and expressivity of hearing loss among those families (Lu et al. 2010b) (Table 1; Fig. 3). Of these, the G15927A variant is located at the fourth base in the anti-codon stem of tRNAThr (conventional position 42). The abolished base-pairing (28C-42G) of this tRNA alters tRNAThr metabolism (Florentz et al. 2003; Wang et al. 2008). Moreover, the G7444A variant results in a read-through of the stop codon AGA of the CO1 message, thereby adding three amino acids (Lys–Gln–Lys) to the C-terminal of the polypeptide (Pandya et al. 1999; Yuan et al. 2005). The ND5 T12338C variant results in the replacement of the first amino acid, translation-initiating methionine, with a threonine (Chen et al. 2008). Thus, the truncated ND5 mRNA is shortened by two amino acids. In addition, the T12338C variant is also located in two nucleotides adjacent to the 3′ end of tRNALeu(CUN). Consequently, the T12338C variant may lead to a reduction in the tRNALeu(CUN) level. Furthermore, the A14693G variant occurs at position 54 in the T arm of tRNAGlu, and the T10454C variant is located at position 55 in the T arm of tRNAArg. Nucleotides at position 54 and 55 of the T arm are often modified and thereby contribute to the structural formation and stabilization of functional tRNAs (Björk 1995). In addition, the T5802C, G5821A, and T15908C variants disrupt the highly conserved base-pairing of tRNACys and tRNAThr. The C12224T variant in tRNASer(AGY) occurs adjacent to the anti-codon of this tRNA. Thus, the alteration of the tertiary structure of the mitochondrial tRNA may result in a failure in this tRNA metabolism. Therefore, these secondary variants may worsen mitochondrial dysfunction caused by the A1555G mutation, increasing the penetrance and expressivity of hearing loss in these Chinese families.
Deletions
Mitochondrial DNA deletions associated with deafness do not occur frequently in population genetics. Three deletions have been reported: the 10.4 kb deletion, the 7 kb deletion, and the common deletion of 4,977 bp. Ballinger et al. (1992) first reported a three-generation family with maternally inherited diabetes mellitus and deafness. Mutational analysis of the mitochondrial genome showed a large deletion of 10.4 kb, which removed the light strand origin (OL) of mtDNA replication and inhibited mitochondrial protein synthesis. The heteroplasmic deletion of 7 kb in mtDNA was identified in a 17-year-old patient with diabetes, deafness, cataract, and maculopathy (Souied et al. 1998), but the molecular pathogenesis of this deletion remains mysterious. The common deletion of 4,977 bp (Bai and Seidman 2001) may alter the mitochondrial copy number (Chen et al. 2011) and affect mitochondrial protein synthesis, and it is anticipated that individuals carrying these deletions would have an oxidative phosphorylation level lower than that of the normal genotype.
Molecular Mechanism of mtDNA Mutations with Deafness
Mitochondrial DNA mutations have structural and functional effects, including altering the RNA structure, reducing the steady-state level of tRNA or mRNA, and causing tRNA modification. Failures in mitochondrial tRNA metabolism or protein synthesis were observed from cybrid cells carrying these primary mutations, which subsequently reduced the ATP synthesis. Deficiencies in oxidative phosphorylation appear to be the main pathogenic factors (McKenzie et al. 2004); increased ROS may damage the hair cells and cochlear neurons. As a result, the mitochondrial permeability transition pore opens and activates apoptosis, leading to hearing loss.
Accumulating evidence shows that mtDNA mutations play important roles in both syndromic and nonsyndromic hearing loss. Mitochondrial dysfunctions caused by these mtDNA mutations or secondary mutations are the major molecular mechanisms responsible for deafness. These data will offer valuable information for early diagnosis, management, and treatment of maternally transmitted hearing loss.
References
Anderson S, Bankier AT, Barrell BG, de Bruijn MH, Coulson AR, Drouin J, Eperon IC, Nierlich DP, Roe BA, Sanger F, Schreier PH, Smith AJ, Staden R, Young IG (1981) Sequence and organization of the human mitochondrial genome. Nature 290:457–465
Attardi G, Schatz G (1988) Biogenesis of mitochondria. Annu Rev Cell Biol 4:289–333
Bai U, Seidman MD (2001) A specific mitochondrial DNA deletion (mtDNA4977) is identified in a pedigree of a family with hearing loss. Hear Res 154:73–80
Ballinger SW, Shoffner JM, Hedaya EV, Trounce I, Polak MA, Koontz DA, Wallace DC (1992) Maternally transmitted diabetes and deafness associated with a 10.4 kb mitochondrial DNA deletion. Nat Genet 1:11–15
Björk GR (1995) Biosynthesis and function of modified nucleotides. In: Söll D, RajBhandary UL (eds) tRNA: structure, biosynthesis and function. ASM, Washington, DC, pp 165–206
Brown SD, Hardisty-Hughes RE, Mburu P (2008) Quiet as a mouse: dissecting the molecular and genetic basis of hearing. Nat Rev Genet 9:277–290
Chamber HF, Sande MA (1996) The aminoglycosides. In: Hardman JG, Limbird LE, Molino PB, Ruddon RW, Gilman AG (eds) The pharmacological basis of therapeutic, 9th edn. McGraw-Hill, New York, pp 1103–1221
Chapiro E, Feldmann D, Denoyelle F, Sternberg D, Jardel C, Eliot MM, Bouccara D, Weil D, Garabédian EN, Couderc R, Petit C, Marlin S (2002) Two large French pedigrees with nonsyndromic sensorineural deafness and the mitochondrial DNA T7511C mutation: evidence for a modulatory factor. Eur J Hum Genet 10:851–856
Chen J, Yang L, Yang A, Zhu Y, Zhao J, Sun D, Tao Z, Tang X, Wang J, Wang X, Lan J, Li W, Wu F, Yuan Q, Feng J, Wu C, Liao Z, Li Z, Greinwald JH, Lu J, Guan MX (2007) Maternally inherited aminoglycoside-induced and nonsyndromic hearing loss is associated with the 12S rRNA C1494T mutation in three Han Chinese pedigrees. Gene 401:4–11
Chen J, Yuan H, Lu J, Liu X, Wang G, Zhu Y, Cheng J, Wang X, Han B, Yang L, Yang S, Yang A, Sun Q, Kang D, Zhang X, Dai P, Zhai S, Han D, Young WY, Guan MX (2008) Mutations at position 7445 in the precursor of mitochondrial tRNA(Ser(UCN)) gene in three maternal Chinese pedigrees with sensorineural hearing loss. Mitochondrion 8:285–292
Chen T, He J, Shen L, Fang H, Nie H, Jin T, Wei X, Xin Y, Jiang Y, Li H, Chen G, Lu J, Bai Y (2011) The mitochondrial DNA 4,977-bp deletion and its implication in copy number alteration in colorectal cancer. BMC Med Genet 12:8
Chomyn A, Enriquez JA, Micol V, Fernez-Silva P, Attardi G (2000) The mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episode syndrome-associated human mitochondrial tRNALeu(UUR) mutation causes aminoacylation deficiency and concomitant reduced association of mRNA with ribosomes. J Biol Chem 275:19198–19209
Davies J, Davis BD (1968) Misreading of ribonucleic acid code words induced by aminoglycoside antibiotics. J Biol Chem 243:3312–3316
del Castillo FJ, Villamar M, Moreno-Pelayo MA, Almela JJ, Morera C, Adiego I, Moreno F, del Castillo I (2002) Maternally inherited nonsyndromic hearing impairment in a Spanish family with the 7510T>C mutation in the mitochondrial tRNASer(UCN) gene. J Med Genet 39:e82
DiMauro S, Schon EA (2001) Mitochondrial DNA mutations in human disease. Am J Med Genet 106:18–26
Dutka S, Meinnel T, Lazennec C, Mechulam Y, Blanquet S (1993) Role of the 1–72 base pair in tRNAs for the activity of Escherichia coli peptidyl-tRNA hydrolase. Nucleic Acid Res 17:4025–4030
El Meziane A, Lehtinen SK, Hance N, Nijtmans LGJ, Dunbar D, Holt IJ, Jacobs HT (1998) A tRNA suppressor mutation in human mitochondria. Nat Genet 18:350–353
Fischel-Ghodsian N (1999) Mitochondrial deafness mutations reviewed. Hum Mutat 13:261–270
Fischel-Ghodsian N, Prezant TR, Fournier P, Stewart IA, Maw M (1995) Mitochondrial mutation associated with nonsyndromic deafness. Am J Otolaryngol 16:403–408
Fischel-Ghodsian N, Kopke RD, Ge X (2004) Mitochondrial dysfunction in hearing loss. Mitochondrion 4:675–694
Florentz C, Sohm B, Tryoen-Toth P, Putz J, Sissler M (2003) Human mitochondrial tRNAs in health and disease. Cell Mol Life Sci 60:1356–1375
Fourmy D, Recht MI, Blanchard SC, Puglisi JD (1996) Structure of the A-site of Escherichia coli 16S ribosomal RNA complexed with an aminoglycoside antibiotic. Science 274:1367–1371
Friedman RA, Bykhovskaya Y, Sue CM, DiMauro S, Bradley R, Fallis-Cunningham R, Paradies N, Pensak ML, Smith RJ, Groden J, Li XC, Fischel-Ghodsian N (1999) Maternally inherited nonsyndromic hearing loss. Am J Med Genet 84:369–372
Gratton MA, Vázquez AE (2003) Age-related hearing loss: current research. Curr Opin Otolaryngol Head Neck Surg 11:367–371
Guan MX (2005) Prevalence of mitochondrial 12S rRNA mutations associated with aminoglycoside ototoxicity. Volta Rev 105:211–227
Guan MX (2011) Mitochondrial 12S rRNA mutations associated with aminoglycoside ototoxicity. Mitochondrion 11:237–245
Guan MX, Enriquez JA, Fischel-Ghodsian N, Puranam RS, Lin CP, Maw MA, Attardi G (1998) The deafness-associated mitochondrial DNA mutation at position 7445, which affects tRNASer(UCN) precursor processing, has long-range effects on NADH dehydrogenase subunit ND6 gene expression. Mol Cell Biol 18:5868–5879
Guan MX, Fischel-Ghodsian N, Attardi G (2001) Nuclear background determines biochemical phenotype in the deafness-associated mitochondrial 12S rRNA mutation. Hum Mol Genet 10:573–580
Gutiérrez Cortés N, Pertuiset C, Dumon E, Börlin M, Hebert-Chatelain E, Pierron D, Feldmann D, Jonard L, Marlin S, Letellier T, Rocher C (2012) Novel mitochondrial DNA mutations responsible for maternally inherited nonsyndromic hearing loss. Hum Mutat 33:681–689
Hamasaki K, Rando RR (1987) Specific binding of aminoglycosides to a human rRNA construct based on a DNA polymorphism, which causes aminoglycoside-induced deafness. Biochemistry 36:12323–12328
Hutchin TP, Parker MJ, Young ID, Davis AC, Pulleyn JL, Deeble J, Lench NJ, Markham AF, Muller RF (2000) A novel mutation in the mitochondrial tRNASer(UCN) gene in a family with nonsyndromic sensorineural hearing impairment. J Med Genet 37:692–694
Ishikawa K, Tamagawa Y, Takahashi K, Kimura H, Kusakari J, Hara A, Ichimura K (2002) Nonsyndromic hearing loss caused by a mitochondrial T7511C mutation. Laryngoscope 112:1494–1499
Jacobs HT, Hutchin TP, Kappi T, Gillies G, Minkkinen K, Walker J, Thompson K, Rovio AT, Carella M, Melchionda S, Zelante L, Gasparini P, Pyykko I, Shah ZH, Zeviani M, Mueller RF (2005) Mitochondrial DNA mutations in patients with postlingual, nonsyndromic hearing impairment. Eur J Hum Genet 13:26–33
Janssen GM, Hensbergen PJ, van Bussel FJ, Balog CI, Maassen JA, Deelder AM, Raap AK (2007) The A3243G tRNALeu(UUR) mutation induces mitochondrial dysfunction and variable disease expression without dominant negative acting translational defects in complex IV subunits at UUR codons. Hum Mol Genet 16:2472–2481
King MP, Koga Y, Davidson M, Schon EA (1992) Defects in mitochondrial protein synthesis and respiratory chain activity segregate with the tRNALeu(UUR) mutation associated with mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke like episodes. Mol Cell Biol 12:480–490
Labay V, Garrido G, Madeo AC, Nance WE, Friedman TB, Friedman PL, del Castillo I, Griffith AJ (2008) Haplogroup analysis supports a pathogenic role for the 7510T>C mutation of mitochondrial tRNASer(UCN) in sensorineural hearing loss. Clin Genet 73:50–54
Lalwani AK, Gürtler N (2008) Sensorineural hearing loss, the aging inner ear, and hereditary hearing impairment. Current diagnosis and treatment in otolaryngology, head and neck surgery, 2nd edn. McGraw-Hill, New York, pp 683–704
Lévêque M, Marlin S, Jonard L, Procaccio V, Reynier P, Amati-Bonneau P, Baule S, Pierron D, Lacombe D, Duriez F, Francannet C, Mom T, Journel H, Catros H, Drouin-Garraud V, Obstoy MF, Dollfus H, Eliot MM, Faivre L, Duvillard C, Couderc R, Garabedian EN, Petit C, Feldmann D, Denoyelle F (2007) Whole mitochondrial genome screening in maternally inherited nonsyndromic hearing impairment using a microarray resequencing mitochondrial DNA chip. Eur J Hum Genet 15:1145–1155
Levinger L, Giege R, Florentz C (2003) Pathology-related substitutions in human mitochondrial tRNA(Ile) reduce precursor 3′ end processing efficiency in vitro. Nucleic Acids Res 31:1904–1912
Li R, Guan MX (2010) Human mitochondrial leucyl-tRNA synthetase corrects mitochondrial dysfunctions due to the tRNALeu(UUR) A3243G mutation, associated with mitochondrial encephalomyopathy, lactic acidosis, and stroke-like symptoms and diabetes. Mol Cell Biol 30:2147–2154
Li X, Fischel-Ghodsian N, Schwartz F, Yan Q, Friedman RA, Guan MX (2004) Biochemical characterization of the mitochondrial tRNASer(UCN) T7511C mutation associated with nonsyndromic deafness. Nucleic Acids Res 32:867–877
Li R, Ishikawa K, Deng JH, Yang L, Tamagawa Y, Bai Y, Ichimura K, Guan MX (2005a) Maternally inherited nonsyndromic hearing loss is associated with the mitochondrial tRNASer(UCN) 7511C mutation in a Japanese family. Biochem Biophys Res Commun 328:32–37
Li X, Zhang LS, Fischel-Ghodsian N, Guan MX (2005b) Biochemical characterization of the deafness-associated mitochondrial tRNASer(UCN) A7445G mutation in osteosarcoma cell cybrids. Biochem Biophys Res Commun 328:491–498
Lu J, Li Z, Zhu Y, Yang A, Li R, Zheng J, Cai Q, Peng G, Zheng W, Tang X, Chen B, Chen J, Liao Z, Yang L, Li Y, You J, Ding Y, Yu H, Wang J, Sun D, Zhao J, Xue L, Wang J, Guan MX (2010a) Mitochondrial 12S rRNA variants in 1642 Han Chinese pediatric subjects with aminoglycoside-induced and nonsyndromic hearing loss. Mitochondrion 10:380–390
Lu J, Qian Y, Li Z, Yang A, Zhu Y, Li R, Yang L, Tang X, Chen B, Ding Y, Li Y, You J, Zheng J, Tao Z, Zhao F, Wang J, Sun D, Zhao J, Meng Y, Guan MX (2010b) Mitochondrial haplotypes may modulate the phenotypic manifestation of the deafness-associated 12S rRNA 1555A>G mutation. Mitochondrion 10:69–81
Maassen JA, ‘tHart LM, van Essen E, Heine RJ, Nijpels G, Jahangir Tafrechi RS, Raap AK, Janssen GMC, Lemkes HH (2004) Mitochondrial diabetes: molecular mechanisms and clinical presentation. Diabetes 53:103–109
Maász A, Komlósi K, Hadzsiev K, Szabó Z, Willems PJ, Gerlinger I, Kosztolányi G, Méhes K, Melegh B (2008) Phenotypic variants of the deafness-associated mitochondrial DNA A7445G mutation. Curr Med Chem 15:1257–1262
McFarland R, Elson JL, Taylor RW, Howell N, Turnbull DM (2004) Assigning pathogenicity to mitochondrial tRNA mutations: when “definitely maybe” is not good enough. Trends Genet 20:591–596
McKenzie M, Liolitsa D, Hanna MG (2004) Mitochondrial disease: mutations and mechanisms. Neurochem Res 3:589–600
Nance WE (2003) The genetics of deafness. Ment Retard Dev Disabil Res Rev 2:109–119
Ogle JM, Ramakrishnan V (2005) Structural insights into translational fidelity. Annu Rev Biochem 74:129–177
Ohkubo K, Yamano A, Nagashima M, Mori Y, Anzai K, Akehi Y, Nomiyama R, Asano T, Urae A, Ono J (2001) Mitochondrial gene mutations in the tRNALeu(UUR) region and diabetes: prevalence and clinical phenotypes in Japan. Clin Chem 47:1641–1648
Pandya A, Xia XJ, Erdenetungalag R, Amendola M, Landa B, Radnaabazar J, Dangaasuren B, Van Tuyle G, Nance WE (1999) Heterogenous point mutations in the mitochondrial tRNASer(UCN) precursor coexisting with the A1555G mutation in deaf students from Mongolia. Am J Hum Genet 65:1803–1806
Prezant TR, Agapian JV, Bohlman MC, Bu X, Oztas S, Qiu WQ, Arnos KS, Cortopassi GA, Jaber L, Rotter JI, Shohat M, Fischel-Ghodsian N (1993) Mitochondrial ribosomal RNA mutation associated with both antibiotic-induced and nonsyndromic deafness. Nat Genet 4:289–294
Purohit P, Stern S (1994) Interactions of a small RNA with antibiotic and RNA ligands of the 30S subunit. Nature 370:659–662
Recht MI, Fourmy D, Blanchard SC, Dahlquist KD, Puglisi JD (1996) RNA sequence determinants for aminoglycoside bind to an A-site rRNA model oligonucleotide. J Mol Biol 262:421–436
Reid RM, Vernham GA, Jacobs HT (1994) A novel mitochondrial point mutation in a maternal pedigree with sensorineural deafness. Hum Mutat 3:243–247
Reid FM, Rovio A, Holt IJ, Jacobs HT (1997) Molecular phenotype of a human lymphoblastoid cell-line homoplasmic for the np 7445 deafness-associated mitochondrial mutation. Hum Mol Genet 6:443–449
Rodriguez-Ballesteros M, Olarte M, Aguirre LA, Galan F, Galan R, Vallejo LA, Navas C, Villamar M, Moreno-Pelayo MA, Moreno F, del Castillo I (2006) Molecular and clinical characterisation of three Spanish families with maternally inherited nonsyndromic hearing loss caused by the 1494C>T mutation in the mitochondrial 12S rRNA gene. J Med Genet 43:e54
Rossmanith W, Karwan R (1998) Impairment of tRNA processing by point mutations in mitochondrial tRNALeu(UUR) associated with mitochondrial diseases. FEBS Lett 433:269–274
Rossmanith W, Tullo A, Potuschak T, Karwan R, Sbisà E (1995) Human mitochondrial tRNA processing. J Biol Chem 270:12885–12891
Ruiz-Pesini E, Wallace DC (2006) Evidence for adaptive selection acting on the tRNA and rRNA genes of human mitochondrial DNA. Hum Mutat 27:1072–1081
Sacconi S, Salviati L, Gooch C, Bonilla E, Shanske S, DiMauro S (2002) Complex neurologic syndrome associated with the G1606A mutation of mitochondrial DNA. Arch Neurol 59:1013–1015
Santorelli FM, Mak SC, El-Schahawi M, Casali C, Shanske S, Baram TZ, Madrid RE, DiMauro S (1996) Maternally inherited cardiomyopathy and hearing loss associated with a novel mutation in the mitochondrial tRNA(Lys) gene (G8363A). Am J Hum Genet 58:933–939
Schacht J (1993) Biochemical basis of aminoglycoside ototoxicity. Otolaryngol Clin North Am 26:845–856
Schon EA, Bonilla E, DiMauro S (1997) Mitochondrial DNA mutations and pathogenesis. J Bioenerg Biomembr 29:131–149
Souied EH, Salès MJ, Soubrane G, Coscas G, Bigorie B, Kaplan J, Munnich A, Rötig A (1998) Macular dystrophy, diabetes, and deafness associated with a large mitochondrial DNA deletion. Am J Ophthalmol 125:100–103
Sue CM, Tanji K, Hadjigeorgiou G, Andreu AL, Nishino I, Krishna S, Bruno C, Hirano M, Shanske S, Bonilla E, Fischel-Ghodsian N, DiMauro S, Friedman R (1999) Maternally inherited hearing loss in a large kindred with a novel T7511C mutation in the mitochondrial DNA tRNASer(UCN) gene. Neurology 52:1905–1908
Tang X, Li R, Zheng J, Cai Q, Zhang T, Gong S, Zheng W, He X, Zhu Y, Xue L, Yang A, Yang L, Lu J, Guan MX (2010) Maternally inherited hearing loss is associated with the novel mitochondrial tRNASer(UCN) 7505T>C mutation in a Han Chinese family. Mol Genet Metab 100:57–64
Tessa A, Giannotti A, Tieri L, Vilarinho L, Marotta G, Santorelli FM (2002) Maternally inherited deafness associated with a T1095C mutation in the mDNA. Eur J Hum Genet 9:147–149
Thyagarajan D, Bressman S, Bruno C, Przedborski S, Shanske S, Lynch T, Fahn S, DiMauro S (2000) A novel mitochondrial 12S rRNA point mutation in parkinsonism, deafness, and neuropathy. Ann Neurol 48:730–736
Tiranti V, Chariot P, Carella F, Toscano A, Soliveri P, Girla P, Carrara F, Fratta GM, Reid FM, Mariotti C, Zeviani M (1995) Maternally inherited hearing loss, ataxia and myoclonus associated with a novel point mutation in mitochondrial tRNASer(UCN) gene. Hum Mol Genet 4:1421–1427
Tiranti V, D’Agruma L, Pareyson D, Mora M, Carrara F, Zelante L, Gasparini P, Zeviani M (1998) A novel mutation in the mitochondrial tRNA(Val) gene associated with a complex neurological presentation. Ann Neurol 43:98–101
Toompuu M, Tiranti V, Zeviani M, Jacobs HT (1999) Molecular phenotype of the np7472 deafness-associated mitochondrial mutation in osteosarcoma cell cybrids. Hum Mol Genet 8:2275–2283
Toompuu M, Levinger LL, Nadal A, Gomez J, Jacobs HT (2004) The 7472insC mtDNA mutation impairs 5′ and 3′ processing of tRNASer(UCN). Biochem Biophys Res Commun 322:803–813
van den Ouweland JM, Lemkes HH, Ruitenbeek W, Sandkuijl LA, de Vijlder MF, Struyvenberg PA, van de Kamp JJ, Maassen JA (1992) Mutation in mitochondrial tRNALeu(UUR) gene in a large pedigree with maternally transmitted type II diabetes mellitus and deafness. Nat Genet 1:368–371
Verhoeven K, Ensink RJ, Tiranti V, Huygen PL, Johnson DF, Schatteman I, Van Lae L, Verstreken M, Van de Heyning P, Fischel-Ghodsian N, Zeviani M, Cremers CW, Willems PJ, Van Camp G (1999) Hearing impairment and neurological dysfunction associated with a mutation in the mitochondrial tRNASer(UCN) gene. Eur J Hum Genet 7:45–51
Virgilio R, Ronchi D, Bordoni A, Fassone E, Bonato S, Donadoni C, Torgano G, Moggio M, Corti S, Bresolin N, Comi GP (2009) Mitochondrial DNA G8363A mutation in the tRNALys gene: clinical, biochemical and pathological study. J Neurol Sci 281:85–92
Wang Q, Li R, Zhao H, Peters JL, Liu Q, Yang L, Han D, Greinwald JH Jr, Young WY, Guan MX (2005) Clinical and molecular characterization of a Chinese patient with auditory neuropathy associated mitochondrial 12S rRNA T1095C mutation. Am J Med Genet 133:27–30
Wang Q, Li QZ, Han D, Zhao Y, Zhao L, Qian Y, Yuan H, Li R, Zhai S, Young WY, Guan MX (2006) Clinical and molecular analysis of a four-generation Chinese family with aminoglycoside-induced and nonsyndromic hearing loss associated with the mitochondrial 12S rRNA C1494T mutation. Biochem Biophys Res Commun 340:583–588
Wang X, Lu J, Zhu Y, Yang A, Yang L, Li R, Chen B, Qian Y, Tang X, Wang J, Zhang X, Guan MX (2008) Mitochondrial tRNAThr G15927A mutation may modulate the phenotypic manifestation of ototoxic 12S rRNA A1555G mutation in four Chinese families. Pharmacogenet Genomics 12:1059–1070
Yan X, Wang X, Wang Z, Sun S, Chen G, He Y, Mo JQ, Li R, Jiang P, Lin Q, Sun M, Li W, Bai Y, Zhang J, Zhu Y, Lu J, Yan Q, Li H, Guan MX (2011) Maternally transmitted late-onset nonsyndromic deafness is associated with the novel heteroplasmic T12201C mutation in the mitochondrial tRNAHis gene. J Med Genet 48:682–690
Yao YG, Salas A, Bravi CM, Bandelt HJ (2006) A reappraisal of complete mtDNA variation in East Asian families with hearing impairment. Hum Genet 119:505–515
Yarham JW, Al-Dosary M, Blakely EL, Alston CL, Taylor RW, Elson JL, McFarland R (2011) A comparative analysis approach to determining the pathogenicity of mitochondrial tRNA mutations. Hum Mutat 32:1319–1325
Yuan H, Qian Y, Xu Y, Cao J, Bai L, Shen W, Ji F, Zhang X, Kang D, Mo JQ, Greinwald JH, Han D, Zhai S, Young WY, Guan MX (2005) Cosegregation of the G7444A mutation in the mitochondrial COI/tRNA(Ser(UCN)) genes with the 12S rRNA A1555G mutation in a Chinese family with aminoglycoside-induced and nonsyndromic hearing loss. Am J Med Genet A. 2:133–140
Zhao H, Li R, Wang Q, Yan Q, Deng JH, Han D, Bai Y, Young WY, Guan MX (2004) Maternally inherited aminoglycoside-induced and nonsyndromic deafness is associated with the novel C1494T mutation in the mitochondrial 12S rRNA gene in a large Chinese family. Am J Hum Genet 74:139–152
Zhao H, Young WY, Yan Q, Li R, Cao J, Wang Q, Li X, Peters JL, Han D, Guan MX (2005a) Functional characterization of the mitochondrial 12S rRNA C1494T mutation associated with aminoglycoside-induced and nonsyndromic hearing loss. Nucleic Acids Res 33:1132–1139
Zhao L, Wang Q, Qian Y, Li R, Cao J, Hart LC, Zhai S, Han D, Young WY, Guan MX (2005b) Clinical evaluation and mitochondrial genome sequence analysis of two Chinese families with aminoglycoside-induced and nonsyndromic hearing loss. Biochem Biophys Res Commun 336:967–973
Zwieb CD, Jemiolo DK, Jacob WF, Wagner R, Dahlberg AE (1986) Characterization of a collection of deletion mutants at the 3′-end of 16S ribosomal RNA of Escherichia coli. Mol Gen Genet 203:256–264
Acknowledgments
This work was supported by grants from Nanjing Medical University (No. 2010NJMU011) and the Ministry of Science and Technology of Zhejiang Province (No. 2008R40G2090027).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ding, Y., Leng, J., Fan, F. et al. The Role of Mitochondrial DNA Mutations in Hearing Loss. Biochem Genet 51, 588–602 (2013). https://doi.org/10.1007/s10528-013-9589-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10528-013-9589-6