Abstract
A controversial proposal to collapse sexual disorders of desire and arousal is forthcoming in the Diagnostic and Statistical Manual of Mental Disorders (5th ed.) (DSM-5). Yet, no study has attempted to empirically distinguish these disorders by using explicit criteria to recruit and compare distinct groups of low desire and arousal sufferers. The goal of the current study was to test the feasibility of finding medically healthy men and women meeting clearly operationalized DSM-IV-TR criteria for disorders of desire and/or arousal and compare them to matched controls. To assess operational criteria, participants completed a comprehensive telephone screening interview assessing DSM-IV-TR and DSM-5 criteria, as well as standardized self-report measures of sexual functioning. The use of operationalized DSM-IV-TR criteria to recruit participants led to the exclusion of over 75 % of those reporting sexual difficulties, with the primary reason for exclusion being failure to meet at least one central diagnostic criterion. The application of the DSM-5 criteria was even more restrictive and led to the exclusion of all but four men and one woman using the original four-symptom criteria, and four men and five women using the revised three-symptom criteria. Cluster analyses supported the distinction between desire and genital arousal difficulties, and suggest that different groups with distinct clusters of symptoms may exist, two of which are consistent with the DSM-5 criteria. Overall, results highlight the need for revisions to the diagnostic criteria, which, as they stand, do not capture the full range of many people’s sexual difficulties.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The questionable validity of current diagnostic conceptualizations of arousal, desire, and their distinction has been the topic of extensive ongoing discussion. This has been propelled by the controversial proposal to collapse disorders of arousal and desire in the forthcoming fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), under the new diagnosis of Sexual Interest/Arousal Disorder (SIAD) (Brotto, 2010a; Graham, 2010; see Table 1 for diagnostic criteria).
This proposal was originally made for both men and women (with small gender variations in diagnostic criteria) and has been justified on the basis of three bodies of evidence: (1) quantitative data indicating the high comorbidity of arousal and desire difficulties in men and women (Basson et al., 2003; Corona et al., 2004; Donahey & Carroll, 1993; Fugl-Meyer & Fugl-Meyer, 2002; Laumann, Paik, & Rosen, 1999; Rosen, Taylor, Leiblum, & Bachmann, 1993; Rosen et al., 2000; Sanders, Graham, & Milhausen, 2008; Segraves & Segraves, 1991); (2) qualitative data pointing to the difficulties experienced by men and women in differentiating these constructs (Brotto, Heiman, & Tolman, 2009; Graham, Sanders, Milhausen, & McBride, 2004; Janssen, McBride, Yarber, Hill, & Butler, 2008); and (3) findings indicating the non-linear sequence of sexual response stages for both men and women, with desire occasionally preceding arousal, sometimes following it, and occasionally being indistinguishable from it (Graham et al., 2004; Janssen et al., 2008). On the basis of these findings, it has been concluded that “…there is no good reason to assume that feelings of desire and arousal are two fundamentally different things” (Laan & Both, 2008, p. 510), but, rather, that they are “two sides of the same coin.”
While empirical evidence supporting the division of arousal and desire disorders is undeniably sparse, it may be premature to entirely throw out this distinction before identifying the theoretical and empirical reasons that might account for this negligible research base. At the forefront of theoretical confounds is the lack of consensus regarding the operational definitions of the constructs of desire and arousal in both women and men. Specifically, the current diagnostic conceptualization of hypoactive sexual desire disorder (HSDD), with its exclusive emphasis on deficient sexual fantasies and desire for sexual activity (American Psychiatric Association, 2000), has been strongly criticized for providing an incomplete representation of the expression of desire, particularly in women (for a review, see Brotto, 2010a). While several other formulations have been forwarded as alternatives (e.g., Basson, 2000; Everaerd & Laan, 1995; Laan & Both, 2008; Levine, 2002; Meana, 2010; Regan & Berscheid, 1999; Schnarch, 2000; Singer & Toates, 1987) to account for contextual factors, such as relationship status and satisfaction, incentives for sexual activity, aging, responsiveness to a sexual stimulus, and the adequacy of sexual stimulation, to date there has been little empirical examination of the viability of these models (for exceptions, see Giles & McCabe, 2009; Sand & Fisher, 2007).
Similarly, our conceptual understanding of female sexual arousal is no more established than it is for desire. The current diagnostic operationalization of female sexual arousal disorder (FSAD) focuses exclusively on a “persistent and recurrent” impairment in genital response, to the neglect of subjective feelings of excitement (American Psychiatric Association, 2000). Yet, in view of a substantial body of evidence indicating desynchrony between physiological and self-report measures of arousal and thus calling this definition into question, the majority of researchers now agree that physiological arousal is at best one piece of the overall picture of sexual arousal, particularly in women (for a review, see Chivers, Seto, Lalumière, Laan, & Grimbos, 2010; Graham, 2010). However, the exact nature of the interaction between self-report and genital indicators of arousal remains unknown, and so it is unclear how to weigh or reconcile the often discrepant information yielded from these different measures. To complicate matters, the construct of “subjective sexual arousal” (SA) has been operationalized in diverse and inconsistent ways, ranging from “awareness of genital change” to “feelings of mental excitement,” with little agreement about the most intrinsic features of this construct. Hence, with respect to both sexual desire and arousal, we find ourselves in a conceptual predicament: without consensus on how to define (and thus, measure) these constructs, it is difficult, if not impossible, to determine if and how they differ from each other.
While much research attention has been allocated towards better defining and distinguishing arousal and desire in women, very little has been comparatively devoted to studying this issue in men. Yet, it is noteworthy that, for men, the same conceptual dilemma exists (albeit to a lesser degree). Specifically, with respect to desire, research indicates that men experience sexual fantasies and a desire for sexual activity with greater frequency and intensity than women, yet men and women may actually be quite similar in how they express sexual desire (for a review, see Brotto, 2010b). That is, contrary to claims about a “male-centered” diagnostic conceptualization of desire, the current operationalization of HSDD may be equally narrow in its ability to capture the experience of desire in men. Significant within-gender variability is also evident in the expression of male desire, reinforcing the suggestion that for men, just as for women, no one common cognitive or behavioral definition of sexual desire exists (Regan & Berscheid, 1996). With respect to sexual arousal, the exclusive operationalization of arousal disorders as impairments in genital response (i.e., erectile dysfunction) has also been contested by men who identify their sexual arousal using multiple cues, only one of which is the presence of an erection (Janssen et al., 2008). Men also make distinctions between genital and subjective sexual arousal (such that one can be experienced without the other), and report similar difficulties distinguishing desire from mental arousal (for a review, see Brotto, 2010a). Thus, comparable conceptual difficulties exist in operationalizing and differentiating desire and arousal in men, particularly with respect to their overlap with “mental arousal”—a construct that until recently had been virtually overlooked.
In addition to theoretical arguments, empirical concerns also caution against making hasty conclusions about the differentiability of arousal and desire disorders in men and women. Specifically, as far as we know, there has yet to be a systematic attempt to assess the feasibility of empirically distinguishing these disorders by recruiting and comparing distinct groups of HSDD and arousal disorder sufferers. In fact, the few empirical studies that have purported to differentiate or compare these disorders in men and women have typically done so through the recruitment of a low desire or arousal group, or a clinical group with heterogeneous sexual difficulties, from which they have attempted to roughly partial out for comparison those with arousal versus desire disorders (e.g., Berman, Berman, Toler, Gill, & Haughie, 2003; Corona et al., 2004; Clayton, DeRogatis, Rosen, & Pyke, 2012; DeRogatis et al., 2010; el Sakka, 2006; Maserjian et al., 2012; Nutter & Condron, 1985; Schiavi, Schreiner-Engel, White, & Mandeli, 1988; Srilatha, Adaikan & Chong, 2007; Wiegel, Meston, & Rosen, 2005). The majority of these studies have also been marked by a number of other methodological limitations, each of which will be considered and improved upon within the current study.
Studies that have compared individuals with low desire to those with low arousal (with and without diagnosis of the other) have typically been characterized by vaguely specified recruitment strategies (e.g., no details provided about the textual content of advertisements, convenience samples employed etc.) (DeRogatis et al., 2010; el Sakka, 2006; Nutter & Condron, 1985; Schiavi et al., 1988; Srilatha et al., 2007; Wiegel et al., 2005), vague or narrow inclusion criteria (e.g., all participants required to be in stable, nonconflictual, long-term relationships) (Derogatis et al., 2010; el Sakka, 2006; Schiavi et al., 1988) and clinical groups that have not been selected or differentiated in accordance with standardized diagnostic criteria (and only occasionally with cutoff scores on questionnaires) (Berman et al., 2003; Corona et al., 2004; el Sakka, 2006; Nutter & Condron, 1985; Schiavi et al., 1988; Srilatha et al., 2007). These limitations cast doubt on the general representativeness of these samples to desire and arousal sufferers. In addition, researchers have often neglected to ensure or to specify that their control and clinical groups were free of other medical or psychological difficulties that might influence sexual functioning (Corona et al., 2004; el Sakka, 2006; Nutter & Condron, 1985; Srilatha et al., 2007; Wiegel et al., 2005). While comorbid sexual dysfunction has often been stipulated as an exclusion criterion, few researchers have reported the extent of co-occurring subclinical sexual difficulties in purportedly distinct clinical groups. In fact, it has not even been clear that members of the low desire groups were free of low arousal symptoms, and vice versa (e.g., Berman et al., 2003; Corona et al., 2004; Derogatis et al., 2010; Nutter & Condron, 1985; Wiegel et al., 2005). Finally, most of these studies have operationalized low arousal exclusively in physiological terms (to the neglect of subjective feelings of excitement), relied exclusively on self-report of an impaired genital response (without corroboration by physiological measurement) and made no attempt to assess or select groups on the basis of low mental arousal as compared to low desire and genital arousal (e.g., Berman et al., 2003; Corona et al., 2004; Derogatis et al., 2010; el Sakka, 2006; Nutter & Condron, 1985; Srilatha et al., 2007; Wiegel et al., 2005). Although this is in line with DSM-IV-TR definitions of FSAD/ED, this limited conceptualization and assessment of arousal has precluded researchers from better understanding the relationship between the subjective and physiological components of arousal. In summary, studies comparing low desire and arousal groups have not sufficiently described or controlled the clinical characteristics of their purportedly distinct samples, thus making it difficult to draw any strong conclusions about the similarities and differences between these study populations.
In contrast to the few studies that attempted to tease apart and compare individuals with arousal versus desire difficulties, other studies have opted instead to recruit a clinical group comprised of those suffering from disorders of both desire and arousal, which bypasses the complications of trying to separate these highly comorbid problems (e.g., Brotto, Basson, & Luria, 2008; Caruso et al., 2004; Meston & McCall, 2005). These studies presented with similar methodological issues, including ambiguous recruitment strategies, non-adherence to established diagnostic criteria in the selection of clinical groups, unclear methods regarding the assessment of comorbid and subclinical sexual difficulties (including separation of arousal and desire problems), and little detail about the exclusion of participants who may have failed to meet diagnostic criteria for both disorders. In addition, by combining people with arousal and desire difficulties into one ambiguously defined group, these studies have inadvertently assumed that one clinical condition (e.g., FSAD) is essentially unaltered by the presence of another comorbid condition (e.g., HSDD), thereby neglecting the possibility that there may be interactions between these dysfunctions that may be clinically meaningful (e.g., the forming of a new type of disorder that is different from either one alone).
Finally, unlike the above studies in which attempts were made to differentially select for disorders of desire and arousal, the majority of empirical studies on low desire and arousal have been less stringent about the “purity” of their clinical group, taking comorbidity of sexual difficulties as a “given.” In addition to the methodological limitations previously discussed, many of these studies have opted to recruit participants with either low desire (Arnow et al., 2009; Buster et al., 2005; DeRogatis et al., 2008; McCall & Meston, 2007a; Meston, 2003; Meston & Gorzalka, 1996; Rosen, Connor, & Maserejian, 2010; Segraves et al., 2001; Stoleru et al., 2003; van der Made et al., 2009), or low arousal (Brotto, Basson, & Gorzalka, 2004; Carvalheira, Brotto, & Leal, 2010; Caruso, Intelisano, Lupo, & Agnello, 2001; Ferguson et al., 2003; Laan, van Driel, & van Lunsen, 2008; Liao et al., 2008; McCall & Meston, 2007b; Meston, 2006; Meston, Rellini, & McCall, 2010; Meston, Rellini, & Telch, 2008; Rosen et al., 2000) as compared to a healthy control and/or another clinical group, with few efforts made to screen out or separate those with comorbid sexual difficulties. While some comorbidity of sexual difficulties is to be expected in a clinical sample, few studies specified the exact nature or extent of this comorbidity, and so it is unclear to which clinical populations these study results can be generalized. In addition, the possibility that interactions between these varied sexual difficulties might have altered the severity or form of the resulting dysfunction has been unacknowledged. Finally, even in those cases where differential diagnoses were made between arousal and desire disorders within a clinically heterogeneous group, the small sample sizes precluded meaningful group comparisons (Bancroft et al., 2005; McCall & Meston, 2006; Nobre, 2009; Rowland & Heiman, 1991; Segraves et al., 2001). Hence, in each of these studies, the clinical groups (even when separated into categories of low arousal or desire) had sexual difficulties that might best be characterized as heterogeneous in nature, consequently precluding the researchers from answering any specific questions they may have initially had about the distinct qualities of either disorders of desire or arousal.
Aims
The reliable identification and differentiability of arousal and desire difficulties across men and women is an issue that should be addressed by a systematic, cross-gendered attempt to empirically separate and compare these difficulties. A prerequisite to doing so, however, first involves the explicit operationalization of the diagnostic criteria for arousal and desire disorders. Hence, the initial goal of the current study was to use clearly operationalized DSM-IV-TR criteria for arousal and desire disorders to assess the probability of finding medically and psychologically healthy participants who, in fact, met these criteria (see Table 2 for criteria). Specifically, the current study aimed to recruit men and women meeting DSM-IV-TR criteria for HSDD (with no difficulties with arousal), those with ED or FSAD (and no difficulties with desire), those meeting diagnostic criteria for disorders of both desire and arousal, and those with no reported sexual difficulties. We also aimed to identify whether we could empirically separate groups on the basis of low subjective arousal difficulties (SAD), as distinct from either low desire or low genital arousal. Participants that met operational criteria went on to participate in a psychophysiological study comparing groups on their genital and subjective arousal in response to a sexual stimulus, as well as their self-reported patterns of desire and arousal.
Using explicitly operationalized DSM-IV-TR criteria to recruit participants proved to be complicated and led to the exclusion of 71.7 % of those that were screened and over 75 % of those reporting sexual difficulties (not including those that dropped out or were temporarily excluded). In view of this large exclusion rate, an analysis of this recruitment data seemed warranted. Specifically, the current study sought to provide a descriptive analysis of the sample composition, primary reasons for exclusion and predictors of study eligibility for those who were screened in accordance with selected operational criteria (for details, see Method). A secondary goal was to evaluate the relative utility of the diagnostic criteria proposed for the DSM-5 (both the original 2010 criteria and the revised 2011 version),Footnote 1 as compared to current DSM-IV-TR criteria, with respect to their ability to capture the range of sexual difficulties reported by study participants. A final goal was to explore the clustering of sexual symptoms for both men and women to identify potential sexual problem subtypes. We hypothesized that the diagnostic criteria currently proposed for the DSM-5 would also be empirically untenable and would lead to the exclusion of an even greater proportion of individuals than the DSM-IV-TR.
Method
Participants
A total of 227 men and women (113 men, 114 women) were recruited from clinics and the community in response to two sets of advertisements: the first recruited healthy controls (“Sexual Arousal: Is it in your mind or body?”) and the second recruited individuals with low desire and arousal (“Do you have low sexual interest and/or difficulty becoming sexually aroused?”). Advertisements solicited “medically healthy, heterosexual men and women between the ages of 18–50 to participate in a study examining how feelings of sexual desire and mental arousal impact physical sexual arousal.”Footnote 2 Advertisements for both groups were placed online (i.e., Craigslist, Kijiji, university classifieds, local websites), in local newspapers, on flyers posted throughout the community (e.g., laundromats, cafes, and community centers), and were read over the local radio. Low desire and arousal participants were also recruited via posters and information pamphlets (with the same headings specified above) distributed to local sexologists and psychologists, sexual health clinics, and local hospitals. Advertisements for the latter were also placed on the webpage of a university-affiliated sex and couple therapy service, and assessment staff at this clinic provided study information to all new clients seeking treatment for arousal and/or desire difficulties.
Operational criteria were assessed via a detailed telephone screening interview as well as through sexual functioning questionnaires sent to those participants who qualified for participation after the phone screening (for more details, see Measures). Participants were excluded if they reported any of the following: being outside the specified age range (18–50)Footnote 3; non-heterosexual orientationFootnote 4; untreated sexually transmitted infection or disease; diagnosis or treatment (e.g., medication use) within the past 6 months of any psychopathology known to affect sexual functioning (e.g., depression, eating disorders); current untreated Axis 1 disorders (subthreshold symptomatology was permitted); having no prior sexual experience; discomfort or objections to watching sexually explicit videos; and avoidance of gynecological/urological exams due to feared genital pain. Additionally, the following exclusion criteria were applied to rule out other factors impacting sexual function, including use (within the past 6 months) of medications with sexual side effects (e.g., antidepressants); a history of genital/pelvic surgeries or injuries (e.g., prostatectomy, oophorectomy); hormonal therapy/treatment (e.g., cancer treatment); or any chronic medical conditions with possible sexual side effects (e.g., diabetes, polycystic ovarian syndrome). Further exclusion criteria for women included being pregnant or breastfeeding, being peri- or post-menopausal, and having menstrual cycle irregularities (e.g., due to medical conditions or contraceptives such as Depo Provera) within the past 6 months; this was done in order to rule out the confounding effects of these hormonally-based reproductive factors, which have been associated with significant changes in sexual functioning (Basson, 2007; Derogatis et al., 2004; Morrell, Dixen, Carter, & Davidson, 1984; van Goozen et al., 1997; Witting et al., 2008). While no stipulations were put on contraceptive use or relationship status/duration, despite their association with changes in sexual functioning, groups were matched on these variables, as well as on age (±3 years).
In order to be selected for the control group, participants needed to deny having “any sexual difficulty” in response to an open-ended question on the telephone screening interview (i.e., “Do you believe you’re currently experiencing any sexual difficulties?”) and negate the presence of any specific sexual symptoms in response to directed interview questions assessing the diagnostic criteria for the sexual disorders. Participants were also required to have engaged in sexual activity within the past 6 months. Assignment to clinical groups required freely reporting low desire or low arousal in response to the open-ended question about whether the participant “believed they were experiencing any sexual difficulties,” in addition to endorsement of the symptom having been present 75 % of the time over the past 6 months, in the majority of sexual situations, and the cause of significant distress or interpersonal interference (see Table 2 for category-specific criteria). The only exception to this was for the question assessing the DSM-5 criterion of responsive desire to a sexual stimulus. In the absence of explicit operationalization of the criterion “sexual interest/arousal being rarely (2010 wording) or infrequently elicited (2011 wording) by a sexual stimulus,” we chose a cutoff of responsive desire occurring less than 15 % of the time.
Given the highly intertwined nature of most sexual difficulties, it was not realistic to completely exclude participants with mild comorbid sexual difficulties from our low desire and/or arousal groups (e.g., severe impairment in arousal would inevitably present some difficulties reaching orgasm). However, unlike past studies, the extent of permissible comorbid sexual symptoms was tightly regulated such that no participant was permitted to meet the diagnostic criteria for any other sexual disorder (unless they were in the combined low desire/arousal group), as assessed by items on the telephone screening interview. For example, while some difficulty reaching orgasm was allowed, it was to be of less than 6 months duration, occurring less than 75 % of the time, and not generalized across all sexual situations. Women with superficial dyspareunia were included only if their pain occurred exclusively during intercourse and could be determined to be the result of vaginal dryness resulting from low sexual arousal. In other words, comorbid sexual difficulties were permitted if they were determined to be secondary to desire or arousal difficulties. Efforts were made to keep HSDD and FSAD/ED groups homogeneous with respect to comorbid arousal and desire difficulties, respectively, by excluding anyone with more than mild, transient and situational symptoms of the other disorder.
Participants’ reports of sexual difficulties on the telephone screening were also required to be generally corroborated by their domain scores on the sexual functioning measures. In line with established cutoffs for controls, healthy women were required to obtain a total score above 26.55 on the FSFI (out of a possible total of 36) (Wiegel et al., 2005). In addition, given that a woman could meet this total cutoff score while still scoring in the dysfunctional range on an individual scale, control women were also required to have a raw score of “4” or more (out of 5) on each of the items for the individual domains. Similarly, healthy men were required to have a total score above 65 on the IIEF (out of a possible total of 75), and a raw score of “4” or more (out of 5) for each of the items across individual domains. Participants who reported sexual difficulties that were uncorroborated by domain scores (e.g., scoring “4s” or “5s” on desire questions on the FSFI/IIEF despite reports of low desire on the phone screening, or who reported sexual difficulties on the FSFI/IIEF despite reporting no sexual difficulties on the phone screening), were excluded.Footnote 5
Procedure
All respondents to study advertisements completed a detailed telephone screening, which was conducted by the principal investigator (PI), or by a trained research assistant who was instructed to regularly confer with the PI for clarification if a participant’s eligibility status was in question. During the telephone screening, all participants were first provided with a detailed description of the screening interview as well as the requirements of the larger study, and were asked for their consent to be queried about their physical and mental health, relationship and sexual history, experience with watching erotic material, and on the diagnostic criteria for the sexual disorders. If a subject was determined to be ineligible early in the telephone screening (e.g., she was postmenopausal or had an interfering medical condition), the interview was immediately terminated and the participant was thanked for their time. Those who met inclusion criteria assessed during the phone interview were emailed a measure of sexual functioning to complete and send back. Participants whose responses on the screening interview were corroborated by sexual functioning measures were then invited to participate in the psychophysiological study of desire and arousal (study in progress). Those whose responses were not corroborated were debriefed about their exclusion, thanked for their time, asked for their consent to be contacted about relevant future studies, and offered information about treatment resources. Detailed records were kept about reasons for exclusion for all ineligible participants.
The above screening procedure received approval from our Research Ethics Board as part of the larger psychophysiological study. Participants received no monetary reimbursement for their participation in this portion of the study.
Measures
Telephone Screening Interview
This interview consisted of three parts: Part 1 provided participants with a detailed description of the larger study and with the terms of their consent; Part 2 queried those who consented to continue with the interview on their medical, reproductive and mental health, use of medications, relationship and sexual history, and experience with watching erotic material; and part three assessed participants on gender-specific DSM-IV-TR and DSM-5 criteria for the sexual disorders (including frequency, onset/duration, contextual occurrence, distress and percentage change associated with the difficulty). Specifically, Part 3 assessed women over the past 6 months on their experience of the following: (1) absent or reduced ability to attain or maintain an adequate lubrication or blood flow swelling response (despite their verbal reports of adequate sexual stimulation) (i.e., “Have you experienced any difficulty attaining or maintaining an adequate lubrication or genital blood flow response until completion of sexual activity?”) (DSM-IV-TR and DSM-5 criterion); (2) absent/reduced interest in sexual activity (i.e., “Would you say that you’ve experienced little or no interest in sexual activity?”) (DSM-IV-TR and DSM-5 criteria), and absent/reduced pleasurable sexual thoughts or fantasies (i.e., “How often have you experienced positive or pleasurable sexual thoughts or fantasies?”) (DSM-IV-TR and DSM-5 criteria); (3) absent/reduced sexual interest/receptivity demonstrated in multiple ways (e.g., including lack of initiation, rare receptivity to a partner’s attempts to initiate, no seeking of sexual material, decreased attraction to others) (i.e., “Have you noticed a lack of sexual interest and responsiveness in multiple sexual situations? Which ones?”) (DSM-5 criterion); (4) low percentage of sexual interest/responsiveness to any sexual stimulus/cue (e.g., to pornography or erotic literature, to a partner’s attempts to initiate, or to attractive others) (i.e., “What percentage of the time have you experienced sexual interest in response to being in a sexual situation, such as when your partner initiated sexual activity, or you saw or read erotic material?”) (DSM-5 criterion); (5) absent/reduced ability to attain or maintain feelings of mental excitement/pleasure (despite reports of adequate stimulation) (DSM-5 criterion) (i.e., “Have you experienced difficulty attaining or maintaining feelings of being mentally excited or ‘turned on’ until you completed sexual activity with a partner or by yourself?”)Footnote 6; (6) difficulty reaching orgasm (i.e., “Have you experienced difficulty reaching orgasm during sexual activity by yourself or with a partner?”); and (7) difficulty with genital pain (i.e., “Have you experienced difficulties with genital pain during intercourse or sexual activity?”). Items 6 and 7 (above) were assessed in order to rule out the probability of another sexual disorder taking precedence. Likewise, in addition to criteria two through seven (listed above), men were also assessed over the past 6 months on their experience of the following: (1) difficulties attaining or maintaining an erection until completion of sexual activity (i.e., “Have you experienced difficulties attaining or maintaining an erection either by yourself or with a partner?”); (2) difficulties with premature ejaculation (i.e., “Have you experienced difficulties with premature ejaculation, following minimal stimulation, before, on or shortly after penetration?”). For each of the above categories, all participants (clinical and control) were asked if they’ve had any difficulty in that domain over the past 6 months, either by themselves or with a partner, with the response options of “yes,” “no,” “not applicable,” or “I don’t know” (e.g., in response to whether they’d experienced lubrication difficulties during masturbation, or were still having morning erections). Any affirmative responses were further explored with follow up questions about the frequency and duration of the difficulty, contextual occurrence (i.e., situational vs. global), identified causes, percentage of change from normal response, and associated distress or interpersonal interference. This interview took approximately 15–20 min to complete.Footnote 7
Female Sexual Function Index (FSFI) (Rosen et al., 2000)
Women completed the FSFI, a 19-item measure divided into six factor-analytically derived subscales (desire, arousal, lubrication, orgasm, satisfaction, and pain), that yields both individual domain scores as well as a total score, with lower scores indicative of greater sexual dysfunction. Each subscale has demonstrated acceptable internal consistency (Cronbach’s alpha ranging from 0.82 to 0.98) (Wiegel, Meston, & Rosen, 2005). Previous studies have reported acceptable inter-item reliability values for sexually healthy women (Cronbach’s alpha = 0.82–0.92), and for women diagnosed with FSAD (Cronbach’s alpha = 0.89–0.95) (Meston, 2003) and HSDD (Cronbach’s alpha = 0.52–0.94) (Rosen et al., 2000). Wiegel et al. (2005) have found strong support for the discriminant validity of the FSFI between women with and without sexual dysfunction, for both the total score and the individual subscale scores, although a high degree of overlap was found across the different diagnostic groups. While specific domain cutoff scores have recently been suggested to differentiate clinical and control groups (e.g., Gerstenberger et al., 2010), these have not yet been well-validated.
International Index of Erectile Functioning (IIEF) (Rosen et al., 1997)
The IIEF is a widely used, multi-dimensional self-report instrument for the evaluation of male sexual function. It is comprised of 15 items, divided into five subscales: erectile functioning, intercourse satisfaction, orgasmic function, sexual desire, and overall satisfaction. The psychometric validity and reliability of this measure have been well-established, and it has since been adopted as the “gold standard” measure of male sexual functioning, particularly for its sensitivity and specificity as a diagnostic tool to evaluate the severity of erectile dysfunction (ED), and to measure treatment efficacy in clinical trials of ED (Rosen, Cappelleri, Lipski, Smith, & Pena, 1999). It has been recommended that a total score of 65 be considered the cutoff score that places a man at risk for sexual dysfunction. In addition, while clinical and control cutoff scores for the individual domains of the IIEF have been well-established, Rosen et al. (1997) have noted that the IIEF was designed as an assessment measure for ED and “that it [was] not intended for use as a primary measure of premature ejaculation or hypoactive sexual desire disorder” (p. 828).
Statistical Analyses
All statistical analyses were conducted with SPSS (v. 16.0.1, SPSS Inc., Chicago, IL). Descriptive analyses were conducted to examine demographic characteristics of eligible and ineligible participants and to assess primary reasons for exclusion in the latter sample. For both sexes, descriptive analyses were also used to compare inclusion rates using DSM-IV-TR versus proposed DSM-5 criteria. Chi square analyses and t tests were conducted to examine predictors of eligibility (e.g., relationship status, age) in the current study. t tests were also conducted to test for differences between eligible and ineligible participants on self-reported levels of sexual functioning (as indicated by scores on the FSFI/IIEF). In order to handle “zero category scores” on these measures (so as not to bias domain scores towards the dysfunctional pole of the response scale), we followed the recommendations of Meyer-Bahlburg and Dolezal (2007), whereby “missing values” were estimated on the basis of group means for those without sexual activity within the past month. Finally, k-means cluster analysis, using pairwise deletion for missing data, was used to determine potential sexual disorder subtypes using desire and arousal symptom variables. K-means cluster analysis is non-hypothesis driven and non-hierarchical method that uses Euclidean distance to group cases into potential clinically relevant groups (McLachlan, 1992). Pairwise deletion for missing data was used in order to avoid the exclusion of too many participants, given that unequal numbers of participants provided responses to each of the items. The only substantial amount of missing data occurred for the variable of subjective arousal during masturbation (due to its late inclusion as a question on the screening interview), with 49 women and 59 men providing information.
Only participants that met basic inclusion criteria (e.g., were medically and psychologically healthy) were asked questions regarding their sexual functioning on the screening interview. In addition, healthy control participants who denied any sexual difficulties in response to the open-ended and DSM disorder-specific questions on the telephone interview were not asked any follow-up questions pertaining to the sexual categories (e.g., regarding frequency, duration, generalizability, etc.). Both of these situations resulted in significant amounts of missing data. Ineligible participants with missing data on all sexual functioning variables (part three of the screening interview) were included only in preliminary descriptive analyses (i.e., demographics, reason for exclusion). To manage missing data for any sexual category for which a control participant denied difficulties (both with a partner and during masturbation), the following assumptions were made: (1) frequency of the sexual difficulty occurred less than 75 % of the time (dichotomous variable: 1 = more than 75 % of the time; 0 = less than 75 % of the time); (2) the duration of the difficulty was zero months; (3) there was no distress or interpersonal difficulty caused by performance in that sexual domain. The same assumptions were made regarding those sexual categories for which clinical participants reported no sexual difficulty (by themselves or with a partner).
Results
Participant Demographics
A total of 227 people (113 men, 114 women) responded to study advertisements. For the men, 29 called to participate in the control group and 65 to participate in the clinical group; the remaining 19 men were excluded before their sexual functioning status could be determined. For women, 33 were screened for the control group and 65 for the clinical group; the sexual functioning status for the remaining 16 women was unknown. A breakdown of recruitment by site for eligible and ineligible participants is showed in Table 3.
Overall, the mean age for men in this study was 32.57 years (SD = 11.00) and for women was 28.35 years (SD = 9.18). Mean ages for men and women according to sexual functioning status are shown in Figs. 1 and 2. Of the 113 men who were interviewed, approximately half were single (n = 56) and the other half (n = 45) were in committed sexual relationships. This was true for those reporting sexual difficulties (37 single, 27 partnered) as well as healthy controls (14 single, 15 partnered). The majority (n = 76) spoke English as a first language, 29 spoke French, and the remaining eight identified another language as their mother tongue. Of the 114 women who were interviewed, most were in committed sexual relationships (n = 68) and only 38 were single. This was the case for those reporting sexual difficulties (41 in committed sexual relationships, 24 single), as well as for healthy controls (23 in committed sexual relationships, 10 single). The majority of women spoke English (n = 88), 21 spoke French, and five identified another language as their mother tongue.
Flow of inclusion/exclusion of men through recruitment stages. The number of men included/excluded at each stage are presented, along with mean ages and SDs for main subgroups. a N’s for reasons for exclusion may exceed subsample totals, as more than one reason for exclusion may apply to a single participant. b “Other” reasons for exclusion from the clinical group include the following: language barrier, non-heterosexual orientation, discomfort with procedure Note SD, sexual dysfunction; SAD, subjective arousal difficulties
Flow of inclusion/exclusion of women through recruitment stages. The number of women included/excluded at each stage are presented, along with mean ages and SDs for main subgroups. a N’s for reasons for exclusion may exceed subsample totals, as more than one reason for exclusion may apply to a single participant. b Other” reasons for exclusion from the clinical group included the following: non-heterosexual orientation, discomfort with the procedure, and no prior sexual experience. SD sexual dysfunction, SAD subjective arousal difficulties
Reasons for Exclusion: Stage 1
Of the 227 participants who were assessed over the phone, 15 (6.7 %) (10 men, 5 women) were excluded early on in the screening interview before providing any demographic or sexual functioning information (e.g., because they were outside of the prescribed age range, had no prior sexual experience, etc.). Another 20 (9.4 %) participants (9 men, 11 women) were excluded after providing information about medical, reproductive, and mental health (but prior to providing information on sexual functioning). Hence, the sexual functioning status (i.e., sexual difficulties vs. no sexual difficulties) for the abovementioned participants was unknown. Primary reasons for exclusion (more than one may apply per person) for the above groups are shown in Figs. 1 and 2.
Reasons for Exclusion: Stage 2
Of the 192 participants who provided information about their sexual functioning (94 men, 98 women), 108 (56 %) (51 men, 57 women) did not meet inclusion criteria for either the clinical or control group. Exclusion rates, broken down by sexual functioning status, are shown in Figs. 1 and 2. Of the remaining 84 participants, an additional 15 (18 %) dropped out (10 men, 5 women), and another 20 (24 %) (10 men, 10 women) were temporarily excluded (i.e., because we had reached our half-way mark in the desired sample size for the control group and wanted to recruit remaining subjects to match our clinical subjects or because clinical subjects did not yet meet the duration criteria for a sexual difficulty).Footnote 8 This left 23 men (11 controls, and 12 clinical) and 26 women (10 controls, 16 clinical) who met the operational criteria for the larger study.
Overall, primary reasons for exclusion for both men and women were the presence of ongoing sexual fantasies despite reports of low desire, frequency of sexual difficulties lasting less than 75 % of the time, duration of sexual difficulties less than 6 months, situational (partner or context specific) nature of sexual difficulties, having another sexual difficulty that was considered primary, FSFI/IIEF scores that were outside of the appropriate range for their group, and lack of distress about sexual difficulties. In addition, for female controls, a primary reason for exclusion was reports of sexual difficulties and FSFI scores beyond what was considered normative for the healthy control group. Reasons for exclusion, exclusion rates, and sexual functioning status for the abovementioned participants are shown in Figs. 1 and 2. All remaining analyses were conducted exclusively with the data from the 192 participants who provided information about their sexual functioning.
Predictors of Eligibility
Comparisons between eligible and ineligible participants were made on a number of variables, including sexual functioning scores, age, and relationship status. The results from t tests comparing women on FSFI scores are shown in Table 4; similar comparisons for men on IIEF scores are shown in Table 5. Results pertaining to women revealed that eligible controls had significantly higher (or more “sexually functional”) levels of desire, lubrication and total FSFI scores than ineligible controls. Similarly, women eligible for the HSDD and/or FSAD group had significantly lower scores on the domains of desire, lubrication and their total FSFI scores than their ineligible counterparts, but did not differ from ineligible subjects on their domain scores for arousal, orgasm, pain, or satisfaction. Results pertaining to men revealed significant differences between eligible and ineligible controls on the domains of desire, orgasm function, and total IIEF scores (all higher in those eligible); in contrast, men eligible for the HSDD and/or ED group had a significantly lower total IIEF score, as well as lower scores on all IIEF domains, except intercourse satisfaction and overall satisfaction.
Relationship status and age were also examined as predictors of study eligibility. For men, of those who were eligible, 12 were single and 11 were in committed sexual relationships; of those who were ineligible, 27 were single and 23 were in committed sexual relationships. For women, of those eligible, four were single, and 22 were in committed sexual relationships; of those excluded, 25 were single and 32 were in committed sexual relationships. The Chi square test assessing the relationship between eligibility and relationship status in men was not significant, χ2 (1) < 1, but was significant in women, χ2(1) = 6.36, p < .05, indicating that women were more likely to meet operational criteria if they were in a committed sexual relationship than if they were single. With respect to age, the mean for men who met screening criteria was 29.70 (SD = 8.97), and for women was 27.08 (SD = 6.89). For those ineligible, mean age for men was 34.04 (SD = 11.76), and mean age for women was 28.46 (SD = 9.73). t tests assessing the impact of age were non-significant, indicating that age was not a significant determinant of eligibility status in the current study for either men, t(88) = −1.62, or women, t(93) < 1.
Of the 23 men that were considered eligible, 11 were entered in the control group, six met criteria for HSDD, four for ED and low subjective arousal, and two for a combination of HSDD, ED, and SAD. Of the 26 women that were eligible, 10 were entered in the control group, three met criteria for HSDD, one for FSAD, four for HSDD and SAD, three for FSAD and low SAD, two for HSDD and FSAD, and three for a combination of HSDD, SAD, and FSAD.
Comparing DSM-IV-TR and DSM-5 Criteria
In the absence of explicit quantitative operationalization of the frequency, responsivity and distress criteria in the proposed DSM-5 criteria for SIAD, the following (arbitrary) assumptions were made: (1) the frequency of each reported difficulty should be greater than 75 %; (2) responsivity to a partner’s initiations should occur less than 25 % of the time to meet criteria for being “rarely or never receptive to a partner’s attempts to initiate” (wording of 2010 proposal); (3) only those reporting responsivity to a sexual stimulus less than 15 % of the time were considered to have “desire rarely or never triggered by a sexual stimulus” (wording of 2010 proposal); and (4) only those reporting distress about at least two of their symptoms met distress criteria for SIAD.
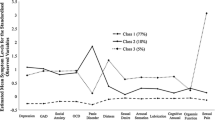
As compared to the 12 men and 16 women who were considered eligible for a clinical group using DSM-IV-TR criteria, only four men and one woman would have been eligible using the 2010 DSM-5 criteria for SIAD (following the above assumptions). Using the modified three-symptom cutoff recently proposed for a diagnosis of SIAD (American Psychiatric Association, 2011), four men and five women would have been eligible (see Table 6 for a detailed presentation of the proportion of people meeting criteria for each of the SIAD symptoms and for SIAD diagnoses, as well as means for symptom number, distress, frequency, and duration; see Fig. 3 for a proportional depiction of the distribution of SIAD symptoms across men and women).
Frequency distribution of SIAD symptoms for men and women with sexual difficulties. The proportion of participants (as an absolute number) with a given number of symptoms is presented on the Y axis. Number of symptoms is presented on the X axis. Frequency distributions were normally distributed for both men and women: the majority presented with either two or three symptoms
K-Means Cluster Analyses
K-means cluster analyses were run separately for men and women using all participant responses to screening interview questions for desire and arousal related variables. Any participant (eligible or ineligible, clinical or control) who provided information on sexual functioning variables (93 men, 95 women) was included in the analyses. The following standardized variables from the phone screening interview were entered into exploratory cluster analyses: frequency of sexual fantasies, presence/absence of sexual interest, presence/absence of sexual pleasure/excitement with a partner, presence/absence of sexual pleasure/excitement during masturbation, percentage of receptivity to a sexual stimulus, presence/absence of genital arousal with a partner, presence/absence of genital arousal during masturbation, and presence/absence of distress about each of the sexual difficulties.
We explored solutions of two to seven clusters for both men and women, comparing them on the bases of theoretical integrity, sample size, symptom profile coherence, distance between cluster centroids, and pooled within group variation for each solution. For both men and women, a four-group solution provided the most coherent and homogenous clusters. For men, the four-cluster solution resulted in the correct classification of 91.4 % of the sample, and yielded clusters with reasonable sample sizes (each cluster was comprised of 20–30 % of the total sample). Clusters also significantly differed on all variables, and symptom profiles within each cluster appeared to be distinct and meaningful (see Table 7). The following represents the results from these analyses:
Cluster 1: Erectile Dysfunction Group. Almost exclusively, this group reported erectile difficulties with a partner and during masturbation, with high accompanying distress about these difficulties. However, they retained relatively normal levels of sexual interest, sexual thoughts, responsiveness, and mental arousal, and were not distressed in these domains.
Cluster 2: Healthy Sexual Functioning Group (Controls). This group was primarily comprised of people who were screened for the control group and that reported no sexual difficulties. They also reported high sexual responsiveness, frequent thoughts about sex, and no distress.
Cluster 3: Relational dysfunction. The men in this group were experiencing sexual difficulties almost exclusively within their relationships, and not within their solitary sexual lives. The group was marked by very low sexual interest, low sexual responsiveness, low mental arousal with a partner, and high distress about these difficulties. The men in this group experienced no difficulties with erection, normal frequency of sexual thoughts/fantasies, and no difficulties with mental arousal during masturbation.
Cluster 4: Combined low desire and arousal group. The men in this group experienced significant symptoms in every domain. They had erectile difficulties with a partner and by themselves, low mental arousal with a partner and while masturbating, low sexual interest, low frequency of sexual thoughts, and distress about all of these difficulties.
For women, the four-cluster solution resulted in the correct classification of 84.4 % of the sample (which was larger than for any other cluster solution) and yielded clinical groups with reasonable sample sizes (the control group represented 45 % of the sample; all others comprised approximately one-third of the remaining sample). Groups identified by the four-cluster solution significantly differed on all variables and symptom profiles within each cluster appeared to be distinct and meaningful (see Table 8). The following represents the results from these analyses:
Cluster 1: Low Desire Group. The women in this group suffered from low sexual interest, low sexual responsiveness, low to moderate mental arousal with a partner, and distress about each of these difficulties. They reported no difficulties with genital arousal, either by themselves or with a partner, and mental arousal during masturbation remained normal. Frequency of sexual thoughts was lower, but remained within the normal range.
Cluster 2: Healthy Sexual Functioning Group (Controls). This group was primarily comprised of people who were screened for the control group and that reported no sexual difficulties. They also reported high sexual responsiveness, frequent thoughts about sex, and no distress.
Cluster 3: Relational dysfunction group. Parallel to men, the women in this group had sexual difficulties primarily within their relationships, and not within their solitary sexual lives. Like the women in cluster one, they reported low sexual interest, moderate sexual responsiveness, and low mental arousal with a partner, but also experienced low genital arousal only with a partner. They experienced distress only about their mental and physical arousal difficulties. The women in this group experienced no difficulties with mental or physical arousal during masturbation, and reported a normal frequency of sexual thoughts/fantasies.
Cluster 4: Combined low desire/arousal group. Parallel to the men, the women in this group experienced significant symptoms in every domain. They had lubrication difficulties with a partner and by themselves, low mental arousal with a partner and while masturbating, low sexual interest, low frequency of sexual thoughts, and distress about all of these difficulties.
Discussion
The current study represents the first empirical attempt to differentiate disorders of desire and arousal through the targeted recruitment of distinct groups of individuals meeting clearly operationalized DSM-IV-TR criteria for either or both of these disorders. To our surprise, the operational criteria used in the current study resulted in the exclusion of 71.7 % of those screened, and over 75 % of those complaining specifically of arousal and desire difficulties. The primary reason for exclusion for the latter was the failure to meet central DSM-IV-TR criteria for HSDD or an arousal disorder. Furthermore, secondary findings indicated that the application of proposed DSM-5 criteria was even more restrictive. Using the 2010 criteria for the DSM-5 led to the exclusion of 96 % of those reporting sexual difficulties, while using the most recently modified criteria led to the exclusion of 92 % of those with sexual complaints.
Implications for the DSM-IV-TR Criteria
These significant exclusion rates in part cast doubt on the validity and relevance of current DSM-IV-TR operationalizations of disorders of arousal, and particularly desire. For example, the primary reason for exclusion from the HSDD group was the presence of regular sexual thoughts/fantasies (averaging multiple times/week for men, and three times/month for women) despite reports of drastically reduced sexual interest in almost all partnered sexual activity. This suggests that contrary to the assumption inherent in the central DSM-IV-TR criterion for HSDD, the occurrence of sexual thoughts/fantasies and the desire or motivation to engage in sexual activity may reflect distinct sexual processes, that although comorbid, do not inevitably co-occur. This notion was supported by the cluster analyses, which revealed one group with low sexual interest (e.g., for their partners) despite ongoing sexual thoughts, and another group that experienced a dampening in all facets of desire (including fantasies). Whether this separation between sexual thoughts and interest reflects differences in syndrome severity (with more severe problems of desire marked by impairment in more aspects of desire), or a distinction between relational versus solitary sexual difficulties, is a question that remains to be tested by future research. Some recent work however has yielded preliminary support for the distinction between dyadic and solitary desire in healthy men and women, and suggests that the two subtypes might involve different facets of desire, and distinct underlying processes (Spector, Carey, & Steinberg, 1996; van Anders, 2012).
Overall, it seems that the desire to engage in sexual activity may be a relational process that is determined more by the type of mental associations one has with the prospect of a sexual interaction with a particular partner, than by any independent libidinal state. Hence, in an unsatisfying sexual relationship, an individual may experience little desire to engage in sexual activity with his or her current partner, while still retaining the ability to experience pleasurable thoughts or fantasies about sexual activity that is independent of their current relationship (e.g., of past or imagined positive sexual encounters). In such cases, the individual may simply be suffering from low sexual desire for the kind of sexual activity they expect to have with a partner. As a result, it is perhaps not surprising that where there is low interest for partnered sexual activity, there is often low sexual responsivity, and low mental arousal during that activity (as revealed in the cluster analyses), as one’s thoughts and feelings during the sexual activity are likely shaped by negative expectations or a decision of “non-interest,” thus preventing an openness to the sexual experience (e.g., pleasurable sensations). While this theory requires empirical examination, overall, these results suggest the need for modifications to current operationalizations of these diagnostic criteria as well as exploration of possible desire subtypes that might better capture the range of the sexual difficulties experienced by numerous men and women.
Implications for the DSM-5 Criteria
The abovementioned eligibility problems are compounded when using the proposed DSM-5 operationalization for SIAD. A closer examination of the symptom distribution across participants indicated that despite the high comorbidity of sexual difficulties in this study, the 2010 proposed DSM-5 requirement of four out of six symptoms was in fact empirically untenable for most participants, and resulted in the exclusion of many participants with clinically significant sexual difficulties (i.e., only 22 % of women, and 12 % of men endorsed four symptoms). The more recent three-symptom version of the DSM-5 criteria was much more viable: approximately 61 % of women and 43 % of men presented with three symptoms (see Table 6). On average, the men in this study presented with two sexual symptoms, while the women had approximately three. However, after considering the full operational criteria (e.g., frequency, duration, distress), the three-symptom version led to the exclusion of only four fewer participants than the four-symptom version. This is because of those participants with multiple sexual difficulties, only a few actually met the frequency, duration and distress criteria for the requisite number of symptoms. In fact, as shown in Table 6, the number one reason for exclusion from the category of SIAD (three-symptom version) was because of an insufficient frequency of comorbid symptoms (average around 50 %), and not because of the criteria for duration, distress or even number of symptoms. Consequently, the majority of individuals meeting DSM-IV-TR criteria for a disorder of desire or arousal in the current study were excluded when using DSM-5 criteria. On the other hand, these results support the recent symptom amendment to the DSM-5 criteria (requiring three, rather than four symptoms), and suggest that it may be a step in the right direction.
In addition, results from exploratory cluster analyses support the possible existence of distinct syndromes marked by the presence of multiple symptoms of both low desire and arousal. For example, the men and women in cluster four presented with significant sexual symptoms in every domain-low desire, low thought frequency, low mental arousal, low genital arousal, and marked distress about each of these difficulties. While not all of these difficulties had necessarily occurred for a sufficient duration and frequency of time to warrant a diagnosis of SIAD, the conglomeration of symptoms presented by these men and women is consistent with the profile for SIAD. However, as the DSM-5 criteria currently stand, different permutations of three (or four) symptoms could all result in a diagnosis of SIAD, despite the fact that there may be meaningful differences in the resulting group profiles, symptom development and underlying processes. It would be worthwhile for future researchers to explore patterns in the order of appearance of these symptoms, as well as differential etiologies that might have shaped the emergence of these different syndromes (for a recent attempt, see Brotto, Pekau, Labrie, & Basson, 2011).
Specifically in addition to a combined low sexual arousal and desire group, cluster analyses also suggested the possible existence of two other clinical syndromes, both for men and women. For men, one of these groups was characterized exclusively by genital arousal difficulties (with no accompanying problems with desire), whereas for women, the parallel group was marked by low desire and low responsiveness (with no accompanying problems with genital arousal). In line with recruitment patterns, these results support the separation of desire and genital arousal difficulties for both men and women (indicating that they do not always go hand-in-hand), and point to the presence of other “subtypes” of arousal and desire difficulties, potentially with distinct etiologies and profiles. It is noteworthy that for men, one of these subtypes was marked exclusively by impaired arousal, whereas for women, the parallel group was marked by low desire, which is consistent with empirical evidence pointing to erectile dysfunction as the most common sexual disorder amongst men, and low desire as the most common problem amongst women (Laumann et al., 2005).
Finally, it is also noteworthy that for both men and women, another group emerged that could best be described as having sexual problems exclusively within their relationships, and not within their solitary sexual lives. These men and women had low sexual interest, low sexual responsiveness, and low mental arousal with a partner, but a normal frequency of sexual thoughts, and no difficulties with mental or physical arousal during masturbation. While the men experienced distress about each of these difficulties, the women experienced distress only about their difficulties with arousal (including their lubrication problems with a partner). This highlights the importance of examining context, and particularly the relationship context, when assessing sexual difficulties, and may encourage the use of more couple-based or interpersonal treatment approaches when treating men and women with this pattern of difficulties (e.g., Davies, Katz, & Jackson, 1999).
Although exploratory, these results support the possible existence of combined sexual interest/arousal groups for both men and women, but also reveal other syndromes marked uniquely by desire or arousal symptoms that may warrant diagnosis. As a parallel to this, a diagnosis of mixed anxiety-depressive disorder was included in the DSM-IV-TR to represent the frequent comorbidity of depression and anxiety symptoms, yet the individual diagnoses were retained to account for the proportion of people presenting almost exclusively with one symptom (depression or anxiety), with its distinct etiology and action mechanism. Future research should continue to examine whether these desire and arousal subtypes can be replicated, or others uncovered, using larger and more representative samples, and with greater attention to identifying distinct symptom patterns and etiological mechanisms that might shape these profiles.
Sample Representativeness
In addition to having implications for the operationalization of disorders of desire and arousal, the high exclusion rates in the current study may also reflect the presence of a large subpopulation of individuals concerned about what are subclinical sexual difficulties, and often the byproduct of bigger relationship problems. An examination of the characteristics of ineligible participants (particularly men) revealed that they had higher scores on multiple scales of sexual functioning measures (indicating better sexual functioning), with the exception of “overall satisfaction,” on which they scored no differently from participants with clinically significant difficulties. They were also more likely to report situational (context-specific) sexual difficulties, rather than generalized dysfunction, as well as sexual difficulties of diagnostically insufficient frequency and duration, or that were likely the result of other comorbid health problems. This was as true of those recruited from hospitals and clinics (treatment-seekers) as those recruited from the community. These results suggest that there may be a large proportion of individuals who experience more mild and transient sexual difficulties about which they are nonetheless concerned, reportedly in fear that something is “wrong with them” or because of the relationship conflict that ensues for them. This raises the possibility that distress about sexual difficulties may be a byproduct of the belief that one has a sexual difficulty (perhaps as suggested by one’s partner), than from actual symptom severity. This finding also suggests that misconceptions about sexual functioning may be quite common, and speaks to the need for widespread sexual education about the influence of context, and the line between “normal” and “abnormal” sexual functioning. Before doing so, however, it seems imperative that a consensus be reached on where this distinction actually lies.
At the same time, the high exclusion rates in the current study may also cast doubt on the representativeness of some of the samples studied by previous investigators, and consequently, on the generalizability of their findings. For example, the same individual who was excluded from participating in the current study due to situational and subthreshold arousal or desire difficulties (e.g., of insufficient severity or duration) would likely have been included in many previous studies that did not use clearly operationalized diagnostic criteria. Secondly, participants that failed to meet operational criteria in the current study were more likely to have a comorbid sexual problem of equal or greater salience, had more psychological and medical disorders and treatment, and were more likely to be single and of older age. In contrast, most past studies have allowed high levels of comorbidity with other psychological, medical and sexual difficulties; thus it is likely that previous investigators have diagnosed individuals with a sexual dysfunction whose difficulties might have been better accounted for within a medical or relational context. Finally, the majority of past studies have primarily included only those in stable sexual relationships. Given that recent work has found relationship status to be one of the strongest predictors of distress about sexual difficulties, and was found to be a robust predictor of eligibility in the current study, the exclusion of single individuals from past studies significantly limits our understanding of the generalizability of past study findings and of their selected diagnostic criteria (e.g., distress). With all this in mind, it is not surprising that the use of more explicit and stringent operational criteria in the current study resulted in a higher exclusion rate than has been seen in previous clinical research.
However, attempts to compare current exclusion rates with the relevant literature are complicated by the fact that the majority of clinical trials on sexual dysfunction have not reported exclusion rates, those that reported rates rarely reported reasons, and when reasons were reported, seldom were people excluded because they did not fit the diagnostic criteria for a sexual dysfunction. In the case of the latter, this is likely partially due to the fact that most of these studies have not clearly operationalized diagnostic criteria for the sexual disorders (even when they use the DSM), but instead tended to select participants on the basis of FSFI/IIEF scores or otherwise self-reported problems.
To exemplify this problem, of the eighty-three clinical trials that we were able to find on sexual dysfunction via computerized searches of the literature, the majority (44/83; 53 %) did not report exclusion rates for those found to be ineligible after screening (e.g., Berman et al., 2001; Bradford & Meston, 2011; Goldstein et al., 2012; Heiman et al., 2006; Jones & McCabe, 2011). Of the remaining thirty-nine studies that did report exclusion rates, rates ranged from 2.9 % (Van Ahlen, Zumbé, Stauch, & Hanisch, 2010) to 90 % (Meston & Worcel, 2002), with a mean of 33.02 %, median of 29.15 %, and mode of 35.2 %. These rates were considerably lower than the overall exclusion rate in the current study. In addition, the majority of these studies (32/39; 82 %) did not discuss the reasons why people were excluded, except to note that they didn’t meet general inclusion criteria (which included a very wide variety of issues) (e.g., Carrier et al., 2005; Goldfischer et al., 2011; Meston & Worcel, 2002).
We found only seven studies that presented both exclusion rates after screening, as well as reasons for exclusion (Andersson et al., 2011; Maserjian et al., 2012; Melnik & Abdo, 2005; Padma-Nathan et al., 2003; Schiavi, White, Mandell, & Levine, 1997; Schneider et al., 2011; Segraves, Clayton, Croft, Wolf, & Warnock, 2004) Of these, four (57 %) excluded people because they did not meet operationalized criteria for a sexual disorder (Andersson et al., 2011; Maserjian et al., 2012; Melnik & Abdo, 2005; Padma-Nathan et al., 2003), with the three others excluding participants because of general, medical or comorbid psychiatric conditions (Schiavi et al., 1997; Schneider et al., 2011; Segraves et al., 2004). Of the four studies that excluded people because of failure to meet diagnostic criteria for the sexual disorders, exclusion rates ranged from .04 % (where the diagnosis couldn’t be verified) (Andersson et al., 2011), to 41 % (where subjects did not meet cutoffs on the FSFI arousal scale) (Maserjian et al., 2012), with a mean exclusion rate of 17.8 %. Again, this is considerably lower than in the current study, where approximately 63 % of women (or 80 %, when including those ineligible due to general medical or psychological conditions) and approximately 80 % of men (or 85 %, when including general medical or psychological conditions) were excluded because they did not meet operationalized sexual dysfunction diagnostic criteria. In sum, while the majority of past clinical trials have not reported rates or reasons for exclusion, those that have done so have typically produced rates much lower than those in the current study, thus highlighting the importance of examining the operational criteria employed when drawing conclusions about sample representativeness and the generalizability of study findings.
Finally, it could also be said that despite our wide recruitment of individuals from both clinical and community contexts, our high exclusion rates reflect difficulties with reaching our target demographic. Unfortunately, there currently remains a large gap in the empirical literature that speaks to exactly who the target demographic for recruitment is. To date, there have been few attempts to validate diagnostic criteria for HSDD or arousal disorders on specific populations, and so it remains unclear for whom these criteria are most relevant.
Limiting the generalizability of our findings, the current study excluded those who were pregnant, breastfeeding, and peri or postmenopausal, groups in which decreases in desire and arousal have frequently been reported. Like many other community based studies in this field, participants also self-selected for the study, and hence may not have been representative of the general population of desire and arousal sufferers. In addition, no restrictions were placed on contraceptive use, including combined contraceptives, which have been associated with changes in sexual functioning. However, attempts were made in this case to match participants in different groups on the basis of their chosen type of contraceptive, and so sexual functioning differences due to contraceptive use would likely have evened out across subjects. Finally, study results can only be generalized to heterosexual participants, as anyone identifying as queer, homosexual or bisexual was excluded from participating (see operational criteria for rationale). Future work is clearly needed in order to ascertain the validity of the operational criteria for disorders of desire and arousal, as well as the populations for whom these diagnostic criteria are most valid.
Limitations
Several important limitations of the current study should be noted, the first of which pertains to the operational criteria employed in the current study. In the absence of explicit operationalization of DSM-IV-TR and DSM-5 criteria for disorders of desire and arousal, several reasoned assumptions needed to be made. For example, given the lack of normative data regarding the frequency of sexual thoughts/fantasies in both normal and low desire populations, it was not clear what cutoff to use in deciding whether one’s frequency of sexual thoughts was in fact “deficient.” Hence, a somewhat arbitrary cutoff of less than once/week (which marked the bottom half of the response option distribution) was chosen. In addition, while the proposed diagnostic criteria for SIAD comprise specifications about the frequency (e.g., “rarely or never,” “typically,” “all or almost all occasions”), severity (e.g., “absent or markedly reduced”) and distress-related aspects of sexual difficulties (e.g., “problem causes clinically significant distress”), it is not clear how these terms are being operationalized, and whether they pertain to each symptom, or to the syndrome as a whole. Thus, in the absence of explicit operationalization of these qualifiers, once again, several reasoned assumptions needed to be made (see “Results”). It is, therefore, important when interpreting study findings about the viability of DSM-IV-TR and DSM-5 criteria that the results of the current study be examined within the context of the operationalization that was chosen. Moreover, future researchers should continue to test and compare other operationalizations to ascertain the set of criteria that best captures these underlying clinical syndromes.
Second, the current study was not designed specifically to test the viability of DSM-5 criteria and was conducted prior to the most recent criteria modifications. As such, while we were able to examine most components of this diagnosis on the basis of self-report, the assessment was not ideal. Specifically, it was not possible during the phone screening to comprehensively ascertain whether the individual’s “desire was rarely or never triggered by any internal or external sexual/erotic stimulus,” as prescribed by the DSM-5 criterion nor is it clear exactly how to accurately test this criterion. Other symptoms such as the “frequency or intensity of genital and non-genital sensations during sexual activity” were assessed during psychophysiological testing for our larger ongoing study, but not at the time of screening, and so are being approximated by participant responses to questions about other common indicators of genital arousal (e.g., lubrication and blood flow/swelling for women and erectile difficulties for men).Footnote 9 Moreover, in the absence of a finalized set of criteria for SIAD in men at the time of study conduction, it was decided that the same criteria that has been proposed for women be tested on men. It is noteworthy that overall, similar patterns were found for both men and women. Cluster analyses supported the existence of a combined arousal/desire disorder for men as well as women, and suggest that speculated gender differences might not in fact be so large. Future research should continue to test the relevance of these criteria on men and women using more comprehensive, sophisticated and multifaceted measures than are traditionally employed in this area.
Next, as previously noted, only those participants that met basic inclusion criteria during the phone screening went on to provide detailed information about sexual functioning and to complete measures of sexual functioning. Moreover, those who did not endorse difficulties (in response to question probes assessing the sexual disorders) were not asked all follow-up questions about their sexual functioning in that domain (i.e., regarding the frequency, duration, and generalizability of symptoms). This resulted in a fair amount of missing data. In order to statistically deal with this missing data, several reasoned assumptions once again had to be made (see “Statistical Analyses”) that may not have been entirely representative of the individual’s experience.
Finally, decisions about sexual functioning status in the current study were made exclusively on the basis of self-report on sexual functioning measures, and in response to diagnostic questions on the phone interview. Given the inherent subjectivity of self-report measures, and their susceptibility to errors and biases in reporting (e.g., regarding the frequency of a difficulty), exclusive reliance on such measures is limiting. In addition, despite their strong psychometrics, neither the FSFI nor the IIEF were designed to be primary measures of hypoactive sexual desire (e.g., Rosen et al., 1997). Hence, the resulting assignment to clinical groups (e.g., HSDD or FSAD/ED) in the current study should not be considered the equivalent of formal clinical diagnoses. At the same time, it is noteworthy that the domain and total sexual functioning scores on the FSFI/IIEF for clinical participants were at the more dysfunctional end of the ranges reported by previous investigators (e.g., Meston, 2003; Gerstenberger et al., 2010; Rosen et al., 1997, 2000; Wiegel et al., 2005).Footnote 10
Conclusion
The results of the current study, although preliminary, support the separation of desire and genital arousal difficulties, as well as the possible existence of multiple sexual syndromes marked by different arousal and desire symptoms. This was true for both men and women, suggesting that the sexes might not be that different in terms of their experiences of desire and arousal. Overall, these results speak to the need for a revision of the DSM-IV-TR criteria for disorders of desire and arousal, but also call for a re-examination of the operationalization of the proposed DSM-5 diagnostic criteria, and the investigation of other disorder subtypes not currently captured by a diagnosis of SIAD. Future research should continue to examine the validity of distinct operational criteria for different disorders of arousal and/or desire, using more diverse samples and sophisticated methodology, and with attention to the nature of the demographic represented by these criteria (e.g., gender, age, culture/ethnicity, relationship status, psychiatric/medical history, developmental history, etc.). In addition, attempts should be made to compare subgroups of desire and arousal sufferers on the basis of the time course and severity of their symptoms, risk and vulnerability factors, treatment responsiveness, and underlying mechanisms. This work is imperative in order to better understand and treat the full range and nature of these complicated sexual difficulties.
Notes
At the time of study administration and article preparation, revisions to the proposed 2010 DSM-5 criteria had not been released. While we have attempted to test the impact of the majority of these changes on inclusion rates (e.g., the 3 symptom requirement, instead of 4), others could not be examined (e.g., the intensity of sexual thoughts or sexual excitement). In addition, a major change in the 2011 criteria for SIAD is its exclusive reference to women, while the current study tested criteria for both men and women. Criteria presented in Table 1 are those proposed in the original 2010 version. See http://www.DSM-5.org/ProposedRevision/Pages/proposedrevision.aspx?rid=432 for recent revisions to these criteria.
The remaining text of the ad comprised a description of the procedure for the larger study, terms of confidentiality, and other ethical information presented in accordance with Research Ethics Board guidelines. The full textual content of advertisements is available upon request.
The upper end of the age range was extended from 45 to 50 after a few months of study recruitment. Providing that women were not yet menopausal, there was no empirical reason to assume that women between the ages of 45 and 50 would differ from their slightly younger counterparts. Prior to this modification in criteria, one man and one woman between the ages of 45–50 were excluded.
Since participants were being recruited for a larger psychophysiological study in which the sexual stimulus employed across all subjects was an erotic film clip depicting heterosexual activity, individuals who self-identified as non-heterosexual had to be excluded.
Low desire and arousal participants were initially selected based on whether they met specific cutoff scores on the sexual functioning questionnaires (chosen in accordance with means reported by previous investigators for control and clinical groups) (Meston, 2003; Rosen et al., 2000). However, this criteria was later modified in recognition of the fact that the FSFI was not designed to be a diagnostic tool, and does not yet possess well-validated clinical cutoff scores for all sexual domains (for recent efforts at this, see Gerstenberger et al., 2010; Wiegel et al., 2005).
Due to experimental error, questions about subjective arousal were not included in the initial version of the screening interview. The late addition of these questions resulted in missing data for this diagnostic criterion for the first 73 participants.
Copies of this interview are available upon request.
Drop-outs and those temporarily excluded from participating were not included in the calculation of overall exclusion rates or any further statistical analyses.
An examination of participant responses to interview questions posed at the time of psychophysiological testing revealed high levels of consistency between reported levels of genital and non-genital sensations and lubrication/erectile difficulties (unpublished raw data).
An examination of participant diagnoses obtained through comprehensive interviews at the time of psychophysiological testing revealed consistency with those provided at the time of screening.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author.
American Psychiatric Association. (2011). Sexual interest/arousal disorder in women. In American Psychiatric Association DSM-5 Development. Retrieved July 14, 2011, from http://www.DSM-5.org/ProposedRevision/Pages/proposedrevision.aspx?rid=432.
Andersson, E., Walén, C., Hallberg, J., Paxling, B., Dahlen, M., Almlöv, J., et al. (2011). A randomized controlled trial of guided Internet-delivered cognitive behavioral therapy for erectile dysfunction. Journal of Sexual Medicine, 8, 2800–2809.
Arnow, B. A., Millheiser, L., Garrett, A., Lake Polan, M., Glover, G. H., Hill, K. R., et al. (2009). Women with hypoactive sexual desire disorder compared to normal females: A functional magnetic resonance imaging study. Neuroscience, 158, 484–502.
Bancroft, J., Herbenick, D., Barnes, T., Hallam-Jones, R., Wylie, K., Janssen, E., et al. (2005). The relevance of the dual control model to male sexual dysfunction: The Kinsey Institute/BASRT collaborative project. Sexual and Relationship Therapy, 20, 13–30.
Basson, R. (2000). The female sexual response: A different model. Journal of Sex & Marital Therapy, 26, 51–64.
Basson, R. (2007). Hormones and sexuality: Current complexities and future directions. Maturitas, 57, 66–70.
Basson, R., Leiblum, S., Brotto, L., Derogatis, L., Fourcroy, J., Fugl-Meyer, K., et al. (2003). Definitions of women’s sexual dysfunctions reconsidered: Advocating expansion and revision. Journal of Psychosomatic Obstetrics and Gynaecology, 24, 221–229.
Berman, J. R., Berman, L. A., Lin, H., Flaherty, E., Lahey, N., Goldstein, I., et al. (2001). Effect of sildenafil on subjective and physiologic parameters of the female sexual response in women with sexual arousal disorder. Journal of Sex & Marital Therapy, 27, 411–420.
Berman, J. R., Berman, L. A., Toler, S. M., Gill, J., & Haughie, S. (2003). Safety and efficacy of sildenafil citrate for the treatment of female sexual arousal disorder: A double-blind, placebo controlled study. Journal of Urology, 170, 2333–2338.
Bradford, A., & Meston, C. M. (2011). Behavior and symptom change among women treated with placebo for sexual dysfunction. Journal of Sexual Medicine, 8, 191–201.
Brotto, L. A. (2010a). The DSM diagnostic criteria for hypoactive sexual desire disorder in women. Archives of Sexual Behavior, 39, 221–239.
Brotto, L. A. (2010b). The DSM diagnostic criteria for hypoactive sexual desire disorder in men. Journal of Sexual Medicine, 7, 2015–2030.
Brotto, L. A., Basson, R., & Gorzalka, B. B. (2004). Psychophysiological assessment in premenopausal sexual arousal disorder. Journal of Sexual Medicine, 1, 266–277.
Brotto, L. A., Basson, R., & Luria, M. (2008). A mindfulness-based group psychoeducational intervention targeting sexual arousal disorder in women. Journal of Sexual Medicine, 5, 1646–1659.
Brotto, L. A., Heiman, J. R., & Tolman, D. L. (2009). Narratives of desire in mid-age women with and without arousal difficulties. Journal of Sex Research, 46, 387–398.
Brotto, L. A., Petkau, J., Labrie, F., & Basson, R. (2011). Predictors of sexual desire disorders in women. Journal of Sexual Medicine, 8, 742–753.
Buster, J. E., Kingsberg, S. A., Aguirre, O., Brown, C., Breaux, J. G., Buch, A., et al. (2005). Testosterone patch for low sexual desire in surgically menopausal women: A randomized trial. Obstetrics and Gynecology, 105, 938–940.
Carrier, S., Brock, G. B., Pommerville, P. J., Shin, J., Anglin, G., Whitaker, S., et al. (2005). Efficacy and safety of oral Tadalafil in the treatment of men in Canada with erectile dysfunction: A randomized, double-blind, parallel, placebo-controlled clinical trial. Journal of Sexual Medicine, 2, 685–698.
Caruso, S., Agnello, C., Intelisano, G., Farina, M., Di Mari, L., & Cianci, A. (2004). Placebo-controlled study on efficacy and safety of daily apomorphine SL intake in premenopausal women affected by hypoactive sexual desire disorder and sexual arousal disorder. Urology, 63, 955–959.
Caruso, S., Intelisano, G., Lupo, L., & Agnello, C. (2001). Premenopausal women affected by sexual arousal disorder treated with sildenafil: A double-blind, cross-over, placebo-controlled study. British Journal of Obstetrics and Gynaecology, 108, 623–628.
Carvalheira, A. A., Brotto, L. A., & Leal, I. (2010). Women’s motivations for sex: Exploring the Diagnostic and Statistical Manual, fourth edition, text revision criteria for hypoactive sexual desire and female sexual arousal disorders. Journal of Sexual Medicine, 7, 1454–1463.
Chivers, M. L., Seto, M. C., Lalumière, M. L., Laan, E., & Grimbos, T. (2010). Agreement of self-reported and genital measures of sexual arousal in men and women. Archives of Sexual Behavior, 39, 5–56.
Clayton, A. H., DeRogatis, L. R., Rosen, R. C., & Pyke, R. (2012). Intended or unintended consequences? The likely implications of raising the bar for sexual dysfunction diagnosis in the proposed DSM-V revisions: 1. For women with incomplete loss of desire or sexual receptivity. Journal of Sexual Medicine, 9, 2027–2039.
Corona, G., Mannucci, E., Petrone, L., Giommi, R., Mansani, R., Fei, L., et al. (2004). Psychobiological correlates of hypoactive sexual desire in patients with erectile dysfunction. International Journal of Impotence Research, 16, 275–281.
Davies, S., Katz, J., & Jackson, J. L. (1999). Sexual desire discrepancies: Effects on sexual and relationship satisfaction in heterosexual dating couples. Archives of Sexual Behavior, 28, 53–567.
DeRogatis, L. R., Allgood, A., Auerbach, P., Eubank, D., Greist, J., Bharmal, M., et al. (2010). Validation of a women’s sexual interest diagnostic interview–short form (WSID-SF) and a daily log of sexual activities (DLSA) in postmenopausal women with hypoactive sexual desire disorder. Journal of Sexual Medicine, 7, 917–927.
DeRogatis, L. R., Allgood, A., Rosen, R. C., Leiblum, S., Zipfel, L., & Guo, C.-Y. (2008). Development and evaluation of the women’s sexual interest diagnostic interview (WSID): A structured interview to diagnose hypoactive sexual desire disorder (HSDD) in standardized patients. Journal of Sexual Medicine, 5, 2827–2841.
DeRogatis, L., Rust, J., Golombok, S., Bouchard, C., Nachtigall, L., Rodenburg, C., et al. (2004). Validation of the Profile of Female Sexual Function (PFSF) in surgically and naturally menopausal women. Journal of Sex & Marital Therapy, 30, 25–36.
Donahey, K. M., & Carroll, R. A. (1993). Gender differences in factors associated with hypoactive sexual desire. Journal of Sex & Marital Therapy, 19, 25–40.
el Sakka, A. I. (2006). Efficacy of sildenafil citrate in treatment of erectile dysfunction: Impact of associated premature ejaculation and low desire. Urology, 68, 642–647.
Everaerd, W., & Laan, E. (1995). Desire for passion: Energetics of sexual response. Journal of Sex & Marital Therapy, 21, 255–263.
Ferguson, D. M., Steidle, C. P., Singh, G. S., Alexander, J. S., Weihmiller, M. K., & Crosby, M. G. (2003). Randomized, placebo-controlled, double-blind, crossover design trial of the efficacy and safety of Zestra for Women in women with and without female sexual arousal disorder. Journal of Sex & Marital Therapy, 29, 33–44.
Fugl-Meyer, K. S., & Fugl-Meyer, A. R. (2002). Sexual disabilities are not singularities. International Journal of Impotence Research, 14, 487–493.
Gerstenberger, E. P., Rosen, R. C., Brewer, J. V., Meston, C. M., Brotto, L. A., Wiegel, M., et al. (2010). Sexual desire and the Female Sexual Function Index (FSFI): A sexual desire cutpoint for clinical interpretation of the FSFI in women with and without hypoactive sexual desire disorder. Journal of Sexual Medicine, 7, 3096–3103.
Giles, K. R., & McCabe, M. P. (2009). Conceptualizing women’s sexual function: Linear vs. circular models of sexual response. Journal of Sexual Medicine, 6, 2761–2771.
Goldfischer, E. R., Breaux, J., Katz, M., Kaufman, J., Smith, W. B., Kimura, T., et al. (2011). Continued efficacy and safety of flibanserin in premenopausal women with hypoactive sexual desire disorder (HSDD): Results from a randomized withdrawal trial. Journal of Sexual Medicine, 8, 3160–3170.
Goldstein, I., McCullough, A. R., Jones, L. A., Hellstrom, W. J., Bowden, C. H., Didonato, K., et al. (2012). A randomized, double-blind, placebo-controlled evaluation of the safety and efficacy of avanafil in subjects with erectile dysfunction. Journal of Sexual Medicine, 9, 1122–1133.
Graham, C. A. (2010). The DSM diagnostic criteria for female sexual arousal disorder. Archives of Sexual Behavior, 39, 240–255.
Graham, C. A., Sanders, S. A., Milhausen, R. R., & McBride, K. R. (2004). Turning on and off: A focus group study of the factors that affect women’s sexual arousal. Archives of Sexual Behavior, 33, 527–538.
Heiman, J. R., Gittelman, M., Costabile, R., Guay, A., Friedman, A., Heard-Davison, A., et al. (2006). Topical alprostadil (PGE1) for the treatment of female sexual arousal disorder: In-clinic evaluation of safety and efficacy. Journal of Psychosomatic Obstetrics & Gynecology, 27, 31–41.
Janssen, E., McBride, K. R., Yarber, W., Hill, B. J., & Butler, S. M. (2008). Factors that influence sexual arousal in men: A focus group study. Archives of Sexual Behavior, 37, 252–265.
Jones, L. M., & McCabe, M. P. (2011). The effectiveness of an Internet-based psychological treatment program for female sexual dysfunction. Journal of Sexual Medicine, 8, 2781–2792.
Laan, E., & Both, S. (2008). What makes women experience desire? Feminism and Psychology, 18, 505–515.
Laan, E., van Driel, E. M., & van Lunsen, R. H. W. (2008). Genital responsiveness in healthy women with and without sexual arousal disorder. Journal of Sexual Medicine, 5, 1424–1435.
Laumann, E. O., Nicolosi, A., Glasser, D. B., Paik, A., Gingell, C., Moreira, E., et al. (2005). Sexual problems among women and men aged 40–80 y: Prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. International Journal of Impotence Research, 17, 39–57.
Laumann, E. O., Paik, A., & Rosen, R. C. (1999). Sexual dysfunctions in the United States: Prevalence and predictors. Journal of the American Medical Association, 281, 537–544.
Levine, S. B. (2002). Reexploring the concept of sexual desire. Journal of Sex & Marital Therapy, 28, 39–51.
Liao, Q., Zhang, M., Geng, L., Wang, X., Song, X., Xia, P., et al. (2008). Efficacy and safety of alprostadil cream for the treatment of female sexual arousal disorder: A double-blind, placebo-controlled study in Chinese population. Journal of Sexual Medicine, 5, 1923–1931.
Maserjian, N., Shifren, J., Parish, S. J., Segraves, R. T., Huang, L., & Rosen, R. (2012). Sexual arousal and lubrication problems in women with clinically diagnosed hypoactive sexual desire disorder: Preliminary findings from the hypoactive sexual desire disorder registry from women. Journal of Sex & Marital Therapy, 38, 41–62.
McCall, K., & Meston, C. M. (2006). Cues resulting in desire for sexual activity in women. Journal of Sexual Medicine, 3, 838–852.
McCall, K., & Meston, C. M. (2007a). Differences between pre- and postmenopausal women in cues for sexual desire. Journal of Sexual Medicine, 4, 364–371.
McCall, K., & Meston, C. M. (2007b). The effects of false positive and false negative physiological feedback on sexual arousal: A comparison of women with and without sexual arousal disorder. Archives of Sexual Behavior, 36, 518–530.
McLachlan, G. J. (1992). Cluster analysis and related techniques in medical research. Statistical Methods in Medical Research, 1, 27–48.
Meana, M. (2010). Elucidating women’s (hetero)sexual desire: Definitional challenges and content expansion. Journal of Sex Research, 47, 104–122.
Melnik, T., & Abdo, C. H. (2005). Psychogenic erectile dysfunction: Comparative study of three therapeutic approaches. Journal of Sex & Marital Therapy, 31, 243–255.
Meston, C. M. (2003). Validation of the Female Sexual Function Index (FSFI) in women with female orgasmic disorder and in women with hypoactive sexual desire disorder. Journal of Sex & Marital Therapy, 29, 39–46.
Meston, C. M. (2006). The effects of state and trait self-focused attention on sexual arousal in sexually functional and dysfunctional women. Behaviour Research and Therapy, 44, 515–532.
Meston, C. M., & Gorzalka, B. B. (1996). Differential effects of sympathetic activation on sexual arousal in sexually dysfunctional and functional women. Journal of Abnormal Psychology, 105, 582–591.
Meston, C. M., & McCall, K. M. (2005). Dopamine and norepinephrine responses to film-induced sexual arousal in sexually functional and sexually dysfunctional women. Journal of Sex & Marital Therapy, 31, 303–317.
Meston, C. M., Rellini, A. H., & McCall, K. M. (2010). The sensitivity of continuous laboratory measures of physiological and subjective sexual arousal for diagnosing women with sexual arousal disorder. Journal of Sexual Medicine, 7, 938–950.
Meston, C. M., Rellini, A. H., & Telch, M. J. (2008). Short and long-term effects of ginkgo biloba extract on sexual dysfunction in women. Archives of Sexual Behavior, 37, 530–547.
Meston, C. M., & Worcel, M. (2002). The effects of yohimbine plus l-arginine glutamate on sexual arousal in postmenopausal women with Sexual Arousal Disorder. Archives of Sexual Behavior, 31, 323–332.
Meyer-Bahlburg, H. F. L., & Dolezal, C. (2007). The Female Sexual Function Index: A methodological critique and suggestions for improvement. Journal of Sex & Marital Therapy, 33, 217–224.
Morrell, M. J., Dixen, J. M., Carter, C. S., & Davidson, J. M. (1984). The influence of age and cycling status on sexual arousability in women. American Journal of Obstetrics and Gynecology, 148, 66–71.
Nobre, P. J. (2009). Determinants of sexual desire problems in women: Testing a cognitive-emotional model. Journal of Sex & Marital Therapy, 35, 360–377.
Nutter, D. E., & Condron, M. K. (1985). Sexual fantasy and activity patterns of males with inhibited sexual desire and males with erectile dysfunction versus normal controls. Journal of Sex & Marital Therapy, 11, 91–98.
Padma-Nathan, H., Brown, C., Fendl, J., Salem, S., Yeager, J., & Harninger, R. (2003). Efficacy and safety of topical Alprostadil cream for the treatment of female sexual arousal disorder (FSAD): A double-blind, multicenter, randomized, and placebo-controlled clinical trial. Journal of Sex & Marital Therapy, 29, 32–344.
Regan, P. C., & Berscheid, E. (1996). Beliefs about the state, goals and objects of sexual desire. Journal of Sex & Marital Therapy, 22, 110–120.
Regan, P. C., & Berscheid, E. (1999). Lust: What we know about human sexual desire. Thousand Oaks, CA: Sage Publications.
Rosen, R. C., Brown, C., Heiman, J., Leiblum, S., Meston, C., Shabsigh, R., et al. (2000). The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. Journal of Sex & Marital Therapy, 26, 191–208.
Rosen, R. C., Cappelleri, J. C., Smith, M. D., Lipski, J., & Pena, B. M. (1999). Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. International Journal of Impotence Research, 11, 319–326.
Rosen, R. C., Connor, M. K., & Maserejian, N. N. (2010). The HSDD registry for women: A novel patient registry for women with generalized acquired hypoactive sexual desire disorder. Journal of Sexual Medicine, 7, 1747–1756.
Rosen, R. C., Riley, A., Wagner, G., Osterloh, I. H., Kirkpatrick, J., & Mishra, A. (1997). The International Index of Erectile Function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology, 49, 822–830.
Rosen, R. C., Taylor, J. F., Leiblum, S. R., & Bachmann, G. A. (1993). Prevalence of sexual dysfunction in women: Results of a survey study of 329 women in an outpatient gynaecological clinic. Journal of Sex & Marital Therapy, 19, 171–188.
Rowland, D. L., & Heiman, J. (1991). Self-reported and genital arousal changes in sexually dysfunctional men following a sex therapy program. Journal of Psychosomatic Research, 35, 609–619.
Sand, M., & Fisher, W. (2007). Women’s endorsement of models of female sexual response: The nurses’ sexuality study. Journal of Sexual Medicine, 4, 708–719.
Sanders, S. A., Graham, C. A., & Milhausen, R. R. (2008). Predicting sexual problems in women: Relevance of sexual inhibition and sexual excitation. Archives of Sexual Behavior, 37, 241–251.
Schiavi, R. C., Schreiner-Engel, P., White, D., & Mandeli, J. (1988). Pituitary-gonadal function during sleep in men with hypoactive sexual desire and in normal controls. Psychosomatic Medicine, 50, 304–318.
Schiavi, R. C., White, D., Mandell, J., & Levine, A. C. (1997). Effect of testosterone administration on sexual behavior and mood in men with erectile dysfunction. Archives of Sexual Behavior, 26, 231–241.
Schnarch, D. (2000). Desire problems: A systematic perspective. In S. Leiblum & R. C. Rosen (Eds.), Principles and practice of sex therapy (3rd ed., pp. 17–56). New York: Guilford Press.
Schneider, T., Gleissner, J., Merfort, F., Hermanns, M., Beneke, M., & Ulbrich, E. (2011). Efficacy and safety of vardenafil for the treatment of erectile dysfunction in men with metabolic syndrome: Results of a randomized, placebo-controlled trial. Journal of Sexual Medicine, 8, 2904–2911.
Segraves, R. T., Clayton, A., Croft, H., Wolf, A., & Warnock, J. (2004). Bupropion sustained release for the treatment of hypoactive sexual desire disorder in premenopausal women. Journal of Clinical Psychopharmacology, 24, 339–342.
Segraves, R. T., Croft, H., Kavoussi, R., Ascher, J. A., Batey, S. R., Foster, V. J., et al. (2001). Bupropion sustained release (SR) for the treatment of hypoactive sexual desire (HSDD) in non-depressed women. Journal of Sex & Marital Therapy, 27, 303–316.
Segraves, R. T., & Segraves, K. B. (1991). Hypoactive sexual desire disorder: Prevalence and comorbidity in 906 subjects. Journal of Sex & Marital Therapy, 17, 55–58.
Singer, B., & Toates, F. (1987). Sexual motivation. Journal of Sex Research, 23, 481–501.
Spector, I. P., Carey, M. P., & Steinberg, L. (1996). The sexual desire inventory: Development, factor structure, and evidence of reliability. Journal of Sex & Marital Therapy, 22, 175–190.
Srilatha, B., Adaikan, P. G., & Chong, Y. S. (2007). Relevance of oestradiol-testosterone balance in erectile dysfunction patients’ prognosis. Singapore Medical Journal, 48, 114–118.
Stoleru, S., Redoute, J., Costes, N., Lavenne, F., Le Bars, D., Dechaud, H., et al. (2003). Brain processing of visual sexual stimuli in men with hypoactive sexual desire disorder. Psychiatry Research: Neuroimaging, 124, 67–86.
Van Ahlen, H., Zumbé, J., Stauch, K., & Hanisch, J. U. (2010). The real-life safety and efficacy of vardenafil (REALISE) study: Results in men from Europe and overseas with erectile dysfunction and cardiovascular or metabolic conditions. Journal of Sexual Medicine, 7, 3161–3169.
van Anders, S. (2012). Testosterone and sexual desire in healthy women and men. Archives of Sexual Behavior, 41, 1471–1484.
van der Made, F., Bloemers, J., van Ham, D., El Yassem, W., Kleiverda, G., Everaerd, W., et al. (2009). Childhood sexual abuse, selective attention for sexual cues, and the effects of testosterone with or without vardenafil on physiological sexual arousal in women with sexual dysfunction: A pilot study. Journal of Sexual Medicine, 6, 429–439.
van Goozen, S. H. M., Wiegant, V. M., Endert, E., Helmond, F. A., & van de Poll, N. E. (1997). Psychoendocrinological assessment of the menstrual cycle: The relationship between hormones, sexuality and mood. Archives of Sexual Behavior, 26, 359–382.
Wiegel, M., Meston, C. M., & Rosen, R. C. (2005). The Female Sexual Function Index (FSFI): Cross-validation and development of clinical cutoff scores. Journal of Sex & Marital Therapy, 31, 1–20.
Witting, K., Santtila, P., Alanko, K., Harlaar, N., Jern, P., Johansson, A., et al. (2008). Female sexual function and its association with number of children, pregnancy and relationship satisfaction. Journal of Sex & Marital Therapy, 34, 89–106.
Acknowledgments
This work has been supported by a grant from the Canadian Institutes of Health Research (CIHR) and a fellowship from the Social Sciences and Humanities Research Council of Canada (SSHRC). The authors thank current and former members of the Binik lab for their thoughtful feedback on earlier versions of this manuscript and for their assistance with data collection and data entry (Tuuli Kukkonen, Marie-Andrée Lahaie, Alina Kao, Melissa Farmer, Laurel Paterson, Seth Davis, Caroline Maykut, Natalie Stratton, Catherine Moreau, Debra Langleben, Jackie Huberman, Marie Faaborg-Anderson, and Amber Lynch).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sarin, S., Amsel, R.M. & Binik, Y.M. Disentangling Desire and Arousal: A Classificatory Conundrum. Arch Sex Behav 42, 1079–1100 (2013). https://doi.org/10.1007/s10508-013-0100-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-013-0100-6