Abstract
Background: Although gamma-irradiation to platelet products is a standard method to prevent the risk of TA-GVHD in vulnerable recipients, it induces some proteomic and redox changes, of which irradiation-induced ROS increments may potentiate platelet mitochondrial dysfunction. However, whether these changes cause platelet apoptosis, or affect their viability during storage, is the main subject of this study. Methods: PLT-rich plasma PC was split into two bags, one kept as control while other was subjected to gamma-irradiation. Within 7-days storage, cytosolic and mitochondrial levels of cytochrome c and pro-apoptotic molecules of Bak and Bax were evaluated by western-blotting. Intraplatelet active caspase (using FAM-DEVD-FMK) and PS-exposure were detected by flowcytometry. Caspase activity in platelet lysate was also confirmed by immunofluorescence detection of Caspase-3/7 Substrate N-Ac-DEVD-N’-MC-R110 while platelet viability was evaluated with MTT assays. Results: Cytosolic cytochrome c gradually increased while its mitochondrial content steadily declined during 7 days of storage. In a contrary trend, reverse patterns were observed for Bak and Bax expressions. Gamma-irradiated platelets showed higher release of mitochondrial cytochrome c that reflected by higher cytosolic cytochrome c levels on day 7 of storage. Concurrently mitochondrial pro-apoptotic Bak and Bax proteins increased on day 7 in irradiated products. However, gamma-irradiation didn’t significantly increase caspase activity or PS-exposure, nor did it decrease platelet viability. Conclusion: Here, consistent with studies on “gamma-irradiation-induced oxidative stress”, we showed that gamma-ray also increases platelet pro-apoptotic signals during storage, although not strongly enough to affect platelet viability by overt apoptosis induction. Conclusively, whether supplementing ROS scavengers or antioxidants to irradiated platelets can improve their quality during storage may be of interest for future research.
Research highlights
-
Platelets cytosolic cytochrome c gradually increased during 7-days of storage.
-
Mitochondrial expression of platelets Bak/Bax steadily increased during 7-days of storage.
-
7-days stored gamma-irradiated platelets showed higher levels of cytosolic cytochrome c.
-
7-days stored gamma-irradiated platelets showed higher levels of mitochondrial Bax/Bak.
-
Gamma-irradiation did not change caspase activity or platelet viability during storage.
-
Gamma-irradiation can induce platelet pro-apoptotic status to some extent, but not apoptosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Platelet transfusion may be accompanied with transfusion associated-graft versus host disease (TA-GVHD) [1, 2], an infrequent but serious immune reaction which is caused by immunologic attack of viable donor T cells against the tissues of immunocompromised or other vulnerable recipients [3, 4]. TA-GVHD can effectively be prevented by gamma irradiation of the blood products [5] where gamma ray acts either by direct damage to T lymphocytes DNA or via producing ions and free radicals that induce T cell genomic damage, avoiding their mitotic capacity [5, 6]. Platelet concentrates (PCs) are commonly stored at room temperature (20–24 °C) with continuous gentle agitation for 5 days [7], however, recently the use of bags made of PVC plasticized with butyryltrihexylcitrate (BTHC) allows adequate gas exchange, which increases the shelf life of platelets from 5 to 7 days [8,9,10]. According to FDA guidelines, platelet concentrates can be irradiated at any time of their storage period [11] while similar to non-irradiated products, during storage, they also undergo significant structural and functional changes that are called platelet storage lesion (PSL) [7, 12].
PSL is generally orchestrated by two distinct death pathways of apoptosis and necrosis [13]. Physiologically, apoptosis, or programmed cell death, is an energy-demanding process that occurs either through the extrinsic or intrinsic pathways, which lead to in vivo elimination of unwanted, damaged or aged platelets without developing an inflammatory responses [14, 15]. However, since functional extrinsic pathway of platelet apoptosis has not been clearly demonstrated yet [16], the intrinsic pathway mainly associated with mitochondria dysfunction play a dominant role in platelet apoptosis which is generally triggered by the signals such as mitochondrial DNA damage, oxidative stress and hypoxia [17]. Alternatively activating stimuli also trigger necrosis as a none-programmed cell death mechanism with an inflammatory potential which is manifested by sustained levels of cytosolic Ca2+, granule release and loss of membrane integrity of platelets [13]. However, while necrosis and apoptosis showed to play major roles in PSL [13, 18], in stored platelets, they are not entirely distinct pathways [13], given that in the early stages of storage, PSL mainly manifests itself with platelet activation and necrosis, while in later stages, from day 5 of storage, platelets start to show some signs of apoptosis. In general the reported markers of apoptosis at this stage are included in the activation and translocation of pro-apoptotic proteins Bak/Bax to mitochondria, increased mitochondrial permeability, cytochrome c release, activation of caspases 3 and 9, cytoskeleton protein cleavage ,surface phosphatidylserine (PS) exposure and micro-particles (MPs) shedding [13, 15, 17], of those the latter two are not specific markers of apoptosis, since platelet activation leading to the necrotic pathway is also associated with PS exposure and MPs formation [19]. This is especially true for PS because its exposure in stored platelets depends on several factors, including the use of plasma substitutes (such as PAS), storage temperature, and other post-production manipulations such as the application of pathogen reduction technology [20,21,22]. In addition mitochondrial membrane permeability can also be associated with a necrotic phenotype of platelets which is mechanistically distinct from that of triggered by apoptosis, leading to mitochondrial outer membrane permeabilization (MOMP) [13, 23].
A growing body of evidence has also identified storage-dependent ROS production as an important PSL marker that is tightly associated with platelet activation and apoptosis during storage [18, 24, 25]. While increased NADPH oxidase (NOX) activity due to platelet activation is considered to be the main source of ROS production, their interaction with mitochondria can further elevate ROS production [18] which in turn damages mitochondrial function through the induction of pro-apoptotic BH3-only Bcl2 protein expression and cytochrome c release [26,27,28]. This was in line with some studies showing that accumulative ROS in stored platelets is associated with mitochondrial depolarization and platelet dysfunction [25]. In this regard, the study of Hosseini et al. which showed that either inhibition of ROS formation by NADPH oxidase (NOX) inhibitor or the scavenging of these oxidant agents by N-acetylcysteine (NAC) can reduce platelet apoptosis, while improving their viability during storage, also indicates a clear link between ROS and apoptosis [18].
Given all mechanistic pathways involved in PSL whether gamma irradiation can further affect platelet phenotype or function during storage is of some debates. In this regard whilst several studies did not reveal any significant effects of gamma irradiation on the general markers of platelet quality and function during storage [4, 21, 29,30,31], other researches have also shown proteomic and oxidative changes [21, 32,33,34] associated with some evidence of reduced post transfusion efficacy of gamma irradiated platelets [11, 35], which can be in favor of superior PSL in this product. Now in general, in view of our recent report on higher levels of oxidant agents in irradiated platelets compared to non-irradiated controls [34], and in line with the prominent effect of ROS on the progression of PSL, especially their effect on induction of apoptosis through mitochondrial pathways, the aim of this study was to compare the expression of characteristic markers of apoptosis between non-irradiated and gamma irradiated platelet concentrates to investigate whether gamma ray can affect platelet phenotypes and quality or not.
Methods and materials
Reagents and chemicals
For reagents and chemicals, see Supplementary Material Appendix S1.
Sample preparation
Similar to our previous protocol [34], with a random selection, whole blood units were collected from volunteer donors referred to Iranian Blood Transfusion Organization (IBTO) and platelet-rich plasma PCs (PRP-PCs) were then prepared after passing a release process according to IBTO guidelines. Briefly, According to AABB standard protocol [36], to prepare platelet concentrate by PRP method, whole blood was first centrifuged with soft spin (2100 g for 4 min based on the standard operating procedure of IBTO) within 8 h of collection. PRP was then expressed into the transfer bag intended for platelet storage, and the lateral blood bag was sealed and removed. To pellet the platelets, the obtained PRP was then subjected to a heavy spin centrifugation (4100 g for 8 min based on the standard operating procedure of IBTO). All but about 70 mL of platelet-poor plasma was expressed in the second transfer bag, which was removed, while the tube was sealed. The pellet in platelet bag was left intact for 1 h. The pellet was then resuspended in the remaining PRP by gently kneading the bag, which was finally placed on a shaking incubator (platelet agitator) to be released for use a few hours later [37]. Each PC had a volume of ~ 70 mL with more than 1 × 109 PLTs/mL. Upon the release of product (day 0 of storage), for each run of study, equivalent ABO- and D-matched pairs of PRP-PCs were pooled, mixed well and were again split into two homogeneous PC units with identical volume, using a connecting device instrument under a sterile closed system (TSCD-TT, Terumo Sterile Tubing Welder, Japan). One of the bag pairs was gamma irradiated (using BioBeam 8000, with the radiation source of cesium-137) at 30 Gy with a dose rate of 5 Gy/min for 6 min, while its counter pair was considered as control and both PCs were then kept for 7 days at 22 °C with gentle agitation. To collect samples for required analyses, on each of the 1st, 3rd, 5th, and 7th days of storage, the platelet bags were moved from agitator to a sterile hood, in which ~ 5 mL of platelet was taken from the cord of bag under sterile condition. The cords were then sealed back and the bag replaced in agitator till the next collection time. Therefore, on the day 7 of storage the bag have the volume of ~ 55mL, which was still at the standard limit for random PRP-derived platelets according to AABBs standard protocol. For each part of study washed platelets were isolated and re-suspended in Tyrode’s buffer (10 mM HEPES, 12 mM NaHCO3, 137 mM NaCl, 2.7 mM KCl, 5 mM glucose, 1 mM CaCl2; pH 7.2–7.4) as described previously [38]. For western blot analysis, the platelet count was adjusted to 1 × 109/mL in Tyrode buffer whereas for flow cytometry analysis and MTT assay, platelet count was adjusted to 2 × 107 /mL and 3 × 105/mL respectively. The study was approved by the local ethical committee.
Cytosolic and mitochondrial proteins analysis using the western blotting technique
1 × 109/mL platelets were resuspended in a permeabilization buffer containing 100 µg/ml digitonin, 75 mM KCl, 1mM NaH2PO4, 8 mM Na2HPO4 and 250 mM sucrose. After centrifugation at 16,000 g for 20 min at 4 ºC, the supernatants were collected as the cytosolic fractions. Pellets were then lysed in a lysis buffer containing 1% Triton-X100, 0.5mM Na2-EDTA, and Protease Inhibitor Cocktail plus PMSF 1mM phenylmethylsulfonyl fluoride (PMSF) for 30 min on ice. After centrifugation at 16,000 g for 10 min, supernatants were used as mitochondrial fractions [39]. For setting up the analysis and especially to adjust the optimal concentration of digitonin in this study, as an important indicator for mitochondrial purity the levels of cytochrome c in different fractions obtained from rest platelets (Day 0/none irradiated platelets with the lowest levels of P-selectin expression) were monitored where the highest levels of cytochrome c were detected in mitochondrial fraction compared to negligible amount in cytosolic fraction. In addition, we also showed insignificant MTT activity in cytosolic fraction compared to its crude mitochondrial pellets suspension (without lysis buffer). Equivalent amounts of cytosolic and mitochondrial proteins were separated by 12% SDS-PAGE electrophoresis, according to the Laemmli method. The gels were then electro-blotted onto PVDF membranes. At next step, membranes were blocked 1 h with 5% nonfat milk in TBS, and probed with specific primary monoclonal antibodies, and HRP conjugated secondary antibody. Membranes were then treated with the enhanced chemiluminescence reagent, and subjected to the ChemiDoc XRS + system to visualize the bands (Bio-Rad Laboratories, Inc. USA). Each band then selected by free hand tool where its adjusted intensity was calculated with regard to background intensity of the band, all quantified using Image lab software (Version 5 build18 from Bio-Rad Laboratories, Inc. USA). To achieve similar loading for each fractions, their protein concentrations were determined using the Bradford assay (homemade: 100 mg Coomassie Blue G250 in 100mL ethanol, 100mL of 85% H3PO4, and 800mL H2O) and the equivalent amounts (40 µg) of proteins for any samples were subjected to 12% SDS-PAGE electrophoresis. Furthermore while for the cytosolic fraction, we measured the housekeeping protein β-actin in each sample as a loading control, however, since we did not have an antibody against any mitochondrial-specific housekeeping protein (such as case Voltage-dependent anion-selective channel protein 1; VDAC1 or Cytochrome C Oxidase; COX IV), we only confined to a protocol of loading the same concentration of extracted protein for each samples ( by loading the same volume of each sample in the amount of 25µL containing 40 µg of protein).
Analysis of platelet caspase activity by immunofluorescence detection
To analyze the levels of caspase activity, 2 × 107 platelets were added into a 96-well plate containing lysis buffer with active Caspase-3/7 Substrate N-Ac-DEVD-N’-MC-R110. After 30 min incubation, plate was visualized by ChemiDoc XRS + system adjusted in fluorescence channel (Bio-Rad Laboratories, inc. USA) and fluorescence intensities were analyzed with image Lab software (Version 5 build18 from Bio-Rad Laboratories, Inc. USA).
Flow cytometry for intraplatelet caspase analysis
As already described [18], APO LOGIX Carboxyfluoroscein caspase Detection Kit was applied to examine active caspase in living platelets undergoing apoptosis. Further details are available on Supplementary Material Appendix S1.
Flow cytometry to determine the levels of phosphatidylserine (PS)
Platelets were stained with annexin V for 30 min. Cells were then immediately subjected to flow cytometer (CyFlowSpace, Partec GmbH, Germany) where a total of 20,000 platelet events were acquired. Further details are available on Supplementary Material Appendix S1.
Viability/mitochondrial metabolic activity analysis using the MTT assay
As already described [18], MTT assay was used to measure the mitochondrial metabolic activity of stored platelets. Further details are available on Supplementary Material Appendix S1.
QC parameters of PCs
QC parameters were monitored as already described [34], (details are available on Supplementary Material Appendix S1).
Statistical analysis
To compare changes occurring during storage days within each group of PC, data were analyzed by the Kruskal–Wallis with Dunn’s multiple comparison tests. Two-way anova with Bonferroni’s multiple comparisons test was also applied to compare between irradiated and non-irradiated PCs. In addition, due to the paired nature of some data (when comparing treated samples with their reference control), Wilcoxon matched-pairs signed rank test was used for analysis. P values of less than 0.05 were considered to be significant, using GraphPad Prism software (GraphPad Prism Software, Inc., San Diego, CA, USA).
Results
The changes of cytosolic and mitochondrial cytochrome c and pro-apoptotic proteins during storage during storage
As shown in supplementary Figure S-1A (the left section of the graph), the levels of cytosolic cytochrome c gradually increased during 7 days of storage in non-irradiated platelets where the increments were significant on Days 7 of storage (P = 0. 013). Unlike cytosolic cytochrome c, the levels of mitochondrial cytochrome c steadily decreased during storage in non-irradiated PLTs while its levels were showed to be significantly lower than baseline from day 5 of storage (P = 0.041). Similar patterns were also detected in gamma-irradiated platelets throughout the storage period. As shown in Figure S-1B ,during storage, a gradual decrease in the levels of cytosolic Bak was observed in non-irradiated PCs while the cytosolic pro-apoptotic Bak levels indicated to be significantly lower than baseline on Days 5 (P = 0.043) and 7 (P = 0.0039) of storage (left section of the graph). A similar pattern of gradual decreasing levels was also detected for Bax (data not shown). As shown in the right section of graph of Figure S-1B, the level of mitochondrial pro-apoptotic Bak gradually increased during storage in non-irradiated PLTs where the increments were significant on Days 5 and 7 of storage (P = 0.048 and P = 0.0025, respectively). A similar pattern of gradual increasing levels was also detected for Bax during storage (data not shown).
The levels of cytosolic and mitochondrial cytochrome c changes during storage in gamma-irradiated versus non-irradiated platelet concentrates. Equal amount of proteins (40 µg) from each cytosolic and mitochondrial fractions were subjected to 12% SDS-PAGE electrophoresis and transferred to PVDF for western blot analysis. Bands were visualized by ChemiDoc XRS + system. Each band selected by free hand tool where its adjusted intensity was quantified using Image lab software (Version 5 build18 from Bio-Rad Laboratories, Inc. USA). A) shows representative western blot image illustrating cytosolic cytochrome c intensities in gamma-irradiated versus non-irradiated PCs on Days 1, 3, 5, and 7 of storage with corresponding graph that exhibits and compares its levels during 7 days of storage in irradiated cells (gray) compared to non-irradiated PCs (black). Similarly, B also presents representative western blot image and its relevant graph for mitochondrial levels of cytochrome c. Data were analyzed by Two-way anova with Bonferroni’s multiple comparisons test. Adj. Vol. (Int); adjusted volume intensity, Irradiated; gamma irradiated, ns; not significant p > 0.05, *P < 0.05. n = 10. Data presented as mean ± SD. Note: the actual molecular weight of cytochrome c is 13 KD which was corresponded to the range detected by ladder (MW marker from BioBasic)
The effect of gamma irradiation on cytosolic and mitochondrial levels of cytochrome c
As illustrated in representative blots and corresponding tables (Fig. 1A), gamma-irradiated PCs showed higher levels of cytosolic cytochrome c compared to non-irradiated samples, which on day 7 of storage this increase was significant (P = 0.036). Alternatively, representative blots and corresponding tables (Fig. 1B) indicated lower levels of mitochondrial cytochrome c in irradiated platelets compared to non-irradiated PCs, with a significant decrease starting from day 7 of storage (P = 0.032).
The effect of gamma irradiation on the levels of cytosolic and mitochondrial pro-apoptotic Bak and Bax during storage
As shown in representative blots and corresponding tables (Fig. 2A &B), gamma-irradiated PCs showed lower levels of cytosolic Bak and Bax compared to non-irradiated samples, which on day 7 of storage the observed decrements were significant (P = 0.014). Alternatively, representative blots and corresponding tables (Fig. 3) indicated higher levels of mitochondrial Bak and Bax in irradiated platelets compared to non-irradiated PCs, with significant increases observed on day 7 of storage. (P = 0.011) for Bax and on either day 5 (P = 0.048) or 7 (P = 0.0089) of storage for Bak.
The levels of cytosolic Bak and Bax changes during storage in gamma-irradiated versus non-irradiated platelet concentrates. Equal amount of proteins (40 µg) from cytosolic fraction were subjected to 12% SDS-PAGE electrophoresis and transferred to PVDF for western blot analysis. Bands were visualized by ChemiDoc XRS + system. Each band selected by free hand tool where its adjusted intensity was quantified using Image lab software (Version 5 build18 from Bio-Rad Laboratories, Inc. USA). Figure shows representative western blot image illustrating the intensities of cytosolic Bak (A) or Bax (B) in gamma-irradiated versus non-irradiated PCs on Days 1, 3, 5, and 7 of storage with their corresponding graphs that exhibit and compare their levels during 7 days of storage in irradiated cells (gray) compared to non-irradiated PCs (black). Data were analyzed by Two-way anova with Bonferroni’s multiple comparisons test. Adj. Vol. (Int); adjusted volume intensity, Irradiated; gamma irradiated, ns; not significant p > 0.05, *P < 0.05. n = 10. Data presented as mean ± SD. Note: the actual molecular weight of Bak and Bax aew 28 and 23 KD respectively, which were corresponded to the range detected by ladder (MW marker from BioBasic)
The levels mitochondrial pro-apoptotic Bak and Bax during storage in gamma-irradiated versus non-irradiated platelet concentrates. Equal amount of proteins (40 µg) from mitochondrial fraction were subjected to 12% SDS-PAGE electrophoresis and transferred to PVDF for western blot analysis. Bands were visualized by ChemiDoc XRS + system. Each band selected by free hand tool where its adjusted intensity was quantified using Image lab software (Version 5 build18 from Bio-Rad Laboratories, Inc. USA). Figure shows representative western blot image illustrating the intensities of mitochondrial Bak (A) or Bax (B) in gamma-irradiated versus non-irradiated PCs on Days 5 and 7 of storage with their corresponding graphs (C) that exhibit and compare their levels during storage in irradiated cells (gray) compared to non-irradiated PCs (black). Data were analyzed by Two-way anova with Bonferroni’s multiple comparisons test. Adj. Vol. (Int); adjusted volume intensity, Irradiated; gamma irradiated, ns; not significant p > 0.05, *P < 0.05. n = 10. Data presented as mean ± SD
The effect of gamma irradiation on the levels of platelet caspase activity
Based on technique used to detect caspase activity in different platelet products, previous studies have shown an increase in caspase activity between day 5 to 7 of platelet concentrate storage [22, 34, 40]. Therefore here while as a control study, the levels of platelet caspase activity (detected by active Caspase-3/7 Substrate N-Ac-DEVD-N’-MC-R110) in response to either ABT 737 (2 µM) or CCCP (100 µM) were detected in one day-stored platelets, its levels also compared between one-day and 5-day stored platelets (either in irradiated or non-irradiated PCs). As showed in representative Fig. 4 and its corresponding graph, whereas one-day stored platelet in presence of BH3 mimetic agent, ABT 737 obviously (~ 5-fold) increased caspase activity, as a potent necrotic agent, CCCP moderately (~ 2-fold) changed its activation compared to non-treated platelets. 5-days stored platelets (both irradiated and non-irradiated ) also showed more than 3-fold increase in caspase activity compared to one-day stored platelets, noting that gamma irradiation had no increasing effect on caspase activity compared to any corresponding samples.
The effect of gamma irradiation on the levels of platelet caspase activity. (A) shows the representative image of micro-titer plate containing 1-day stored non-irradiated and gamma irradiated platelet lysate and fluorescence sensitive dye (active Caspase-3/7 Substrate N-Ac-DEVD-N’-MC-R110) in presence or absence of either ABT 737 (2 µM) or CCCP (100 µM) compared to their corresponding 5-days stored platelets. Table also shows samples’ intensities detected by ChemiDoc XRS + system adjusted in fluorescence channel. (B) is a graph that shows different levels of caspase activity of abovementioned samples. Here, the black stars and ns shows statistical values compared to Day 1 platelets (non-irradiated) and the red stars and ns shows comparisons against Day-1 irradiated platelets, whereas the blue ns shows the comparison between irradiated and non-irradiated platelets where analyses made by Wilcoxon matched-pairs signed rank test. PLT; platelet, Adj. Vol. (Int); adjusted volume intensity, Irradiated; gamma irradiated, ns; not significant p > 0.05, *P < 0.05 and **P < 0.01. n = 10. Data presented as mean ± SD
The effect of gamma irradiation on the levels of intraplatelet active caspase in stored platelets
To confirm the above-mentioned results showing no significant increasing effect of gamma irradiation on platelet caspase activity, intraplatelet active caspase in irradiated and non-irradiated platelets was also analyzed by flow cytometry technique. Figure 5A shows the levels of intra-platelet active caspase in both groups of control (non-irradiated platelets) and gamma irradiated platelets during storage with significant increase from day 5 of storage (P = 0.041 and P = 0.02 respectively). It also compares caspase levels between two groups with no significant effects between groups during storage. As shown by representative histograms and corresponding graphs (Fig. 5B&C), although gamma irradiation slightly increased caspase levels, these increases were not significant. However, this increase for day 5 of storage was almost higher than day 7, albeit it remained insignificant (P = 0.07). As a control study, intraplatelet caspase levels in response to ionophore A23187 (5 µM) were also detected in irradiated and non-irradiated platelets stored for 5 or 7 days, where addition of ionophore to each sample (with 30 min incubation time) significantly increased caspase activity.
The effect of gamma irradiation on the levels of intraplatelet active caspase in stored platelets. Here, using APO LOGIX Carboxyfluoroscein caspase Detection Kit, intraplatelet active caspase in irradiated and non-irradiated platelets was analyzed by flow cytometry technique. A shows the levels of intra-platelet active caspase in both groups of control (non-irradiated platelets) and gamma irradiated platelets during storage with significant increase from day 5 of storage analyzed by Kruskal–Wallis with Dunn’s multiple comparison tests. It also compares caspase levels between two groups with significant difference observed on day 7 of storage (analyzed by Two-way anova with Bonferroni’s multiple comparisons test). B and C also show the representative dotted plots and corresponding histograms with their relevant graphs compare the levels of intraplatelet active caspase in gamma irradiated versus non irradiated stored platelets on days 5 and 7 of storage respectively. As a controls, intraplatelet caspase levels in response to ionophore A23187 (5 µM) were also detected in irradiated and non-irradiated platelets stored for 5 or 7 days (analyzed by Wilcoxon matched-pairs signed rank test). Rad; gamma irradiated, ns; not significant p > 0.05, * p < 0.05, ** p < 0.01, *** p < 0.001, n = 10. Data presented as mean ± SD. Note: The MFI ratio represents the ratio of the geometric mean fluorescence of the sample to the corresponding control isotype
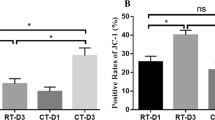
The effect of gamma irradiation on PS exposure in stored platelets
Previous studies have shown that the significant increase of platelet PS exposure begins between day 5 and 7 of PCs storage [34, 41]. Given this the effects of gamma irradiation on PS exposure were evaluated in this study where did not show any significant increasing effects compared to non-irradiated platelets (Fig. 6A).
The effect of gamma irradiation on the levels of platelet PS exposure and viability. A) shows representative dotted plots and corresponding histograms with their relevant graphs which compare the levels of platelet PS exposure in gamma irradiated versus non irradiated stored platelets on days 5 and 7 of storage. Graph B shows a gradual decrease in soluble formazan (an MTT product) during platelet storage in both irradiated and non-irradiated platelets, reflecting the steady loss of cell viability with a significant fall that started on day 5 of storage. No significant change in the ability of living cells to reduce MTT substrate to the formazan is also observed between non-irradiated and irradiated platelets. ns; not significant p > 0.05, *P < 0.05 and **P < 0.01. Data presented as mean ± SD
The effect of gamma irradiation on platelet viability
The platelet viability during storage was evaluated by MTT method. A gradual decrease in soluble formazan (an MTT product) during platelet storage were observed in both irradiated and non-irradiated platelets, reflecting the steady loss of mitochondrial respiration capacity (index of cell viability) with a significant fall that started on day 5 of storage (P = 0.036 for non-irradiated and P = 0.028 for gamma-irradiated platelet; Fig. 6B). As shown in this figure, no significant change in the ability of living cells to reduce MTT substrate to the formazan is observed between non-irradiated and irradiated PCs.
Discussion
Although for many years apoptosis was exclusively attributed to nucleated cells, several lines of evidence indicated that it also occurs in platelets where their viability is maintained by Bcl-xl pro-survival proteins via restraining the pro-apoptotic Bak and Bax proteins [42]. During platelet storage, Bcl-xl expression gradually decreases, leading to the release of pro-apoptotic Bak/Bax molecules, which once released, are translocated to the mitochondrial outer membrane, where they form oligomers causing the permeability of the mitochondrial outer membrane (MOMP) and the release of cytochrome c from mitochondria. The increased level of cytosolic cytochrome c causes the formation of the apoptosome complex and the activation of caspase 3, which ultimately leads to the proteolysis of the substrates resulting in apoptosis [13, 43]. Long-term storage of platelets also leads to increased production of ROS, molecules that interfere with apoptosis [25, 26, 44]. Such findings, along with numerous observations that indicate the role of ionizing radiation, especially gamma rays in increasing ROS generation [34, 45], draw attention to whether gamma irradiation, like other ionized rays, can lead to apoptosis in platelets. Therefore, according to these observations, the study presented here investigated the effect of gamma irradiation on platelets where we found higher levels of cytochrome c release along with higher mitochondrial pro-apoptotic Bax/Bak expression in long stored irradiated PCs. However, these pro-apoptotic changes did not meet actual apoptotic features evaluated by PS exposure, caspase activity or platelet viability. In this regard, at least regarding phosphatidylserine, there are some studies that indicate no significant change in its platelet exposure following gamma irradiation to stored platelet products [31, 46].
As presented in this study cytosolic cytochrome c gradually increased in both irradiated and non-irradiated PCs during storage with significant raise beginning from day 5, while conversely the contents of mitochondrial cytochrome c reduced during 7 days of storage with the significant reduction on day 7. Although similar studies were somewhat indicated such trends [43, 47, 48] of which only the studies by Reid et al. fractionated mitochondrial fragments of platelets where they showed similar decreasing trend of mitochondrial cytochrome c during storage [47]. However, to the best of knowledge our study is the first that demonstrated a clear mirror counterbalance between cytosolic and mitochondrial sources of cytochrome c during platelet storage. In contrast to cytochrome c levels, the expression of cytosolic pro-apoptotic molecules of Bak and Bax gradually decreased during storage with the significant reduction started from day 5 (versus significant increase of cytochrome c from this time point), whereas the levels of their mitochondrial source increased during storage in a mirror counterbalance with cytosolic levels. Considering other studies, this stored-dependent mirror trends is expected, since by the progression of apoptotic pathways with the gradual reduction of anti-apoptotic proteins (such as decreasing levels of Bcl-xL in platelets [43]), unbound pro-apoptotic molecules of Bax/BaK are translocated on mitochondrial membrane that leading to their decreased cytosolic levels versus increases in mitochondrial fraction [34, 49]. However notably, to rule out discrepant findings, any studies on apoptotic protein profiling in platelets should be interpreted by caution as fractionation of cytosolic and mitochondrial sources is a very important concern for a proper evaluation of anti-apoptotic and pro-apoptotic proteins during platelet storage. For example in a study by Johnson et al., although they showed an increasing levels of Bax and Bak expression during storage, since they measured total levels of these pro-apoptotic molecules in platelet lysate (without mitochondrial and cytosolic fractionation) [38], the results cannot be clearly extended to the corresponding levels of BCL-xl which did not show any relevant trend. Similarly in the study by Reid et al. [47] where they only used mitochondrial fractionation kit for cytochrome c, as they did not apply same fractionation strategy for Bak and Bax analysis, a logical trend was also not observed during storage, mainly due the fact that using total platelet lysate (mixture of mitochondrial and cytosolic sources) could not properly show any distinct trend. However, it is worth mentioning that in both studies platelets stored in a mixture of SSP + and plasma instead of plasma alone and it should be noted that keeping platelets in such conditions that provide a richer metabolic environment may also affect the interpretation of the results.
Previous studies have shown that gamma irradiation, by affecting the platelet proteome, leads to some PSL-dependent alterations, the evidence that is accompanied by changes in the redox balance of platelets and an increase in intracellular ROS levels [21, 32,33,34]. Given these findings and several studies that made a link between oxidant stress and necrotic or apoptotic pathways [26, 50, 51], it is likely that gamma irradiation can also affect the platelet apoptosis via ROS generation. As shown by Yoshida et al. gamma irradiation on rat A7r5 cells can robustly increase intracellular ROS levels within minutes, that able to oxidize mitochondrial structural lipids including cardiolipin, a molecule that normally plays an important role in the proper functioning of the electron transport chain (ECT) in association with cytochrome c. Therefore, given that cardiolipin peroxidation by elevated ROS causes the release of cytochrome c and mitochondrial ECT dysfunction [45, 51], it is assumed that the release of cytochrome c by gamma irradiation-induced ROS generation may also promote apoptotic pathways. Especially since, the increased cytochrome c release from mitochondria during storage in turn, also stimulates ROS generation due to the ECT dysfunction, that further enhances apoptosis [26]. Of course, it is worth noting that due to the lack of nuclei in platelets, the above findings may not fully correspond to the conditions of platelets, although on the other hand, the lack of nuclei of platelets and as a result their limited access to sources of reducing enzymes and proteins makes them more sensitive to oxidative signals. Therefore, considering all the facts, we tried for the first time to investigate whether gamma irradiation on the platelet product can affect the release of mitochondrial cytochrome c and the pro-apoptotic state of platelets and if there are any changes, are they at a level to significantly increase platelets apoptosis or affect their viability during storage or not.
According to our results from day 7 of storage significantly higher release of mitochondrial cytochrome c was observed in gamma-irradiated platelets compared to non-irradiated PCs, which was also reflected by significantly higher levels of cytosolic cytochrome c in the gamma-irradiated platelets on day 7 of storage. Interestingly this finding was in accordance with our previously published observation that showed significantly higher levels of ROS generation in longer stored gamma irradiated platelets, that confirms Yoshida et al. findings about the effects of gamma ray-induced peroxidation of mitochondrial lipids [45] that can lead to cytochrome c release [51]. This is also in addition to the other observations that showed an early impairment of the cellular redox status due to GSH oxidation/efflux can trigger the mitochondrial apoptotic signaling [27, 52, 53]. The observations that are in accordance with our previous findings where we also showed significant decreases in intracellular GSH upon gamma irradiation [34] that may precede oxidant-induced apoptosis. Concurrently in this study the expression of mitochondrial pro-apoptotic Bak and Bax proteins significantly increased on day 7 of storage in irradiated compared to non-irradiated products. Higher levels of mitochondrial Bak and Bax in irradiated platelets than non-irradiated ones suggests that the apoptotic process may be accelerated in stored-irradiated PCs, the finding that can be supported by previous proteomic studies indicating gamma irradiation may exacerbate platelet storage lesion [21]. Although other than this observations here, there has been no report of increased levels of the pro-apoptotic proteins Bak and Bax in gamma-irradiated PCs yet, the closest research to the this study was done by Reid et al. where they showed higher levels of Bak and Bax in riboflavin and ultraviolet light PRT-treated PCs during storage [47]. This is considered the closest study to ours, especially since, similar to gamma irradiation, UV illumination to platelets was shown to significantly induce oxidative stress in stored platelet concentrates [21].
In response to increased mitochondrial pro-apoptotic Bak/Bax levels and cytochrome c release, platelet storage was shown to be associated with a significant increase in caspase activity and PS exposure, which together serve as a specific marker of pro-apoptotic shift to an overt apoptotic condition [13, 18]. Experimentally, apoptosis and activation pathways in platelets can be induced separately from each other, but physiologically, it is not easy to separate these pathways, and the same is true for PSL. To induce a robust and pure MOMP-dependent apoptosis in platelets, they can be treated with ABT-737, a BH3 mimetic agent that known to have no significant effects on platelet activation detected by granule release or integrin activation. This is an exclusive experimental pathway for apoptosis, which is induced without significant involvement of platelet-activating signals raised by sustained increased Ca 2+ influx [1,2,3]. Another chemical that induces platelet apoptosis and death in a different way is carbonyl cyanide m-chlorophenylhydrazone (CCCP), a lipophilic proton shuttling compound which violates the integrity of proton-impermeable inner mitochondrial membrane leading to depolarization and reduced ΔΨm in platelets [4]. CCCP also increases ROS generation due to the uncoupling effects on oxidative phosphorylation mediated by its proton shuttling mechanism. On the other hand, the compound can mimic the function of the mitochondrial permeability pore, MPTP which causes activation-dependent necrosis in platelets due to Ca 2+ efflux from mitochondria [3, 5] leading to a sustainable increase in cytosolic Ca 2+ with a modest PS exposure (although less than that induced by calcium ionophore A23187)[4]. Despite its role in necrotic pathway, CCCP per se cannot directly induce apoptosis by releasing proapoptotic factors in the same way that ABT-737 does, and therefore, it has been suggested that its moderate apoptotic function is related to increased ROS generation [6] or Cytochrome C leakage from mitochondria as a prerequisite of the cytoplasmic apoptosome complex which leads to caspase activation [7]. This is a path that more closely resembles the conditions created during long-term storage of platelets than the pathway mimicked by ABT-737. However stored platelet activation cannot physiologically or experimentally be differentiated from apoptosis, because platelet post-activation generally leads to apoptotic events mainly due to induced mitochondrial damage by overlapping mechanisms of MPTP formation or MOMP function [3]. Therefore, although both ABT-737 and CCCP are generally used as the cell death and apoptotic agents, they may not properly represent physiological pattern of platelet apoptosis that is commonly triggered by Ca 2+ influx within platelet activation. This is also come true when we are monitoring platelet storage lesion with the sequential events of platelet pro-aggregatory function (monitored by platelet aggregation or PAC-1 binding), platelet granule releases (detected by P-selectin/CD40L expression) and pro-coagulant state (indicated by PS exposure) which all be triggered by Ca2 + influx and finally leads to mitochondrial damage and apoptosis [8, 9]. Thereby the closest experimental set up that mechanistically mimics PSL could be the treatment of platelets with calcium ionophore A23187 as a proper agent that robustly enhances Ca2 + influx and platelet activation, which by linking between MTPT- and MOMP-dependent mechanisms leads to apoptosis [3, 10, 11]. Notably, in both conditions, whether activation of platelets by ionophore or pure apoptosis of platelets by ABT-737, higher levels of PS are observed, which albeit are at comparable levels, they are partially induced by different mechanisms. This means that despite some literature, PS exposure cannot be considered as a specific marker of platelet apoptosis [12].
Thereby considering all the facts, for this study two different setups have been designed to evaluate caspase activity during PSL. In the first setup to monitor different paths of cell death leading to caspase activity and compare those with what occurs in PSL, we applied CCCP (that mimic MTPT-dependent death) and ABT-737 ( as an inducer of MOMP-dependent apoptosis), alongside 5 days-stored platelets (as a highest limit for standard storage). Interestingly, for 5-day stored platelets, this experimental approach revealed a level of caspase activity somewhere between that induced by CCCP and ABT-737. Given the most effective concentration of CCCP applied for this experiment, our finding of higher levels of caspase activity in stored platelets than CCCP may indicate the combined involvement of apoptotic pathway for caspase activation in PSL. Therefore, according to this result, for the next stages of study that designed to compare the caspase activities between two groups of irradiated and non-irradiated platelets, calcium ionophore A23187 has been chosen as a positive control that induces both necrosis and apoptosis efficiently more resemble to that occurs during PSL. On the other hand, regardless of control studies, having two different methods for the evaluation of caspase activity, of which one measured caspse activity on lysed stored platelets and another evaluated its activity in intact stored platelets also provides more credit to the obtained result in PSL.
Similar to our previous study, here we found a significant increase in caspase activity from day 5 of storage in irradiated and non-irradiated platelets. However, in this study the observation of no significant difference in caspase activity or PS exposure between irradiated and non-irradiated platelets did not attribute any specific apoptotic changes to gamma irradiation. This is also consistent with previous studies that showed no changes in PS exposure due to gamma irradiation [31, 34, 46], all together suggesting that although gamma ray can induce pro-apoptotic signals in 7-day stored platelets, the alterations may not be sufficient to induce a clear apoptosis. On the other hand, as shown by different studies, the time gap between cytochrome c release and caspase activation is a well-known pattern that varies significantly between cells,, such that wider intervals in some cells may be due to more efficient post cytochrome c negative regulators of caspase-3 [54, 55]. A growing body of evidence has also shown decreasing viability of platelets during storage at room temperature [14, 18, 56]. Similarly, our result also emerged a decrease in the mitochondrial metabolic activity of platelets in both irradiated and non-irradiated PCs; however, platelet viability was not affected by gamma irradiation, again suggesting that further ROS generation or higher pro-apoptotic signals induced by gamma irradiation cannot actually affect platelet survival during storage.
Conclusion
Taken together, the study presented here has completed the previous research indicating the oxidant stress caused by gamma irradiation in stored platelets, by highlighting the message that although the change in platelet redox status leads to the induction of pro-apoptotic signals, these changes cannot result in an apparent platelet apoptosis during PC standard storage. However, since gamma irradiation is an inevitable approach to prevent TA-GVHD and considering the fact that ROS inhibition can prevent some PSL-dependent changes and improve platelet viability, further research may be recommended to determine whether the addition of antioxidant supplements or ROS scavengers to gamma-irradiated products can be beneficial to improve their quality, particularly at longer storage times.
Data availability
The corresponding author can make available dataset upon reasonable request.
References
Zimmermann R, Schmidt S, Zingsem J, Glaser A, Weisbach V, Ruf A et al (2001) Effect of gamma radiation on the in vitro aggregability of WBC-reduced apheresis platelets. Transfusion 41(2):236–242
Smethurst PA (2016) Aging of platelets stored for transfusion. Platelets 27(6):526–534
Mallhi R, Biswas A, Philip J, Chatterjee T (2016) To study the effects of gamma irradiation on single donor apheresis platelet units by measurement of cellular counts, functional indicators and a panel of biochemical parameters, in order to assess pre-transfusion platelet quantity and quality during the shelf life of the product. Med J armed forces india 72(1):19–26
Tynngård N, Studer M, Lindahl TL, Trinks M, Berlin G (2008) The effect of gamma irradiation on the quality of apheresis platelets during storage for 7 days. Transfusion 48(8):1669–1675
Moroff G, Luban N (1997) The irradiation of blood and blood components to prevent graft-versus-host disease: technical issues and guidelines. Transfus Med Rev 11(1):15–26
Jacobs GP (1998) A review on the effects of ionizing radiation on blood and blood components. Radiat Phys Chem 53(5):511–523
Shrivastava M (2009) The platelet storage lesion. Transfus Apheres Sci 41(2):105–113
Handigund M, Cho YG (2015) Insights into platelet storage and the need for multiple approaches. Annals of Clinical & Laboratory Science 45(6):713–719
Korte D (2000) Comparison between a new PVC platelet storage container (UPX80) and a polyolefin container. Transfus Med 10(2):131–139
Hornsey VS, McColl K, Drummond O, Macgregor I, Prowse C (2008) Platelet storage in Fresenius/NPBI polyolefin and BTHC-PVC bags: a direct comparison. Transfus Med 18(4):223–227
Julmy F, Ammann RA, Fontana S, Taleghani BM, Hirt A, Leibundgut K (2014) Transfusion efficacy of apheresis platelet concentrates irradiated at the day of transfusion is significantly superior compared to platelets irradiated in advance. Transfus Med hemotherapy 41(3):176–181
Ohto H, Nollet KE (2011) Overview on platelet preservation: better controls over storage lesion. Transfus Apheres Sci 44(3):321–325
Jackson SP, Schoenwaelder SM (2010) Procoagulant platelets: are they necrotic? Blood. J Am Soc Hematol 116(12):2011–2018
Li J, Xia Y, Bertino AM, Coburn JP, Kuter DJ (2000) The mechanism of apoptosis in human platelets during storage. Transfusion 40(11):1320–1329
Gyulkhandanyan AV, Mutlu A, Freedman J, Leytin V (2012) Markers of platelet apoptosis: methodology and applications. J Thromb Thrombolysis 33(4):397–411
Lebois M, Josefsson EC (2016) Regulation of platelet lifespan by apoptosis. Platelets 27(6):497–504
Leytin V, Gyulkhandanyan AV, Freedman J (2019) Platelet apoptosis can be triggered bypassing the death receptors. Clin Appl Thromb Hemost 25:1076029619853641
Hosseini E, Ghasemzadeh M, Atashibarg M, Haghshenas M (2019) ROS scavenger, N-acetyl‐l‐cysteine and NOX specific inhibitor, VAS2870 reduce platelets apoptosis while enhancing their viability during storage. Transfusion 59(4):1333–1343
Lopez J, Salido G, Gomez-Arteta E, Rosado J, Pariente J (2007) Thrombin induces apoptotic events through the generation of reactive oxygen species in human platelets. J Thromb Haemost 5(6):1283–1291
Josefsson EC, Hartwig JH, Hoffmeister KM (2007) Platelet storage temperature–how low can we go? Transfus Med hemotherapy 34(4):253–261
Hosseini E, Kianinodeh F, Ghasemzadeh M (2021) Irradiation of platelets in Transfusion Medicine: risk and benefit judgments.Platelets. :1–13
Johnson L, Schubert P, Tan S, Devine DV, Marks DC (2016) Extended storage and glucose exhaustion are associated with apoptotic changes in platelets stored in additive solution. Transfusion 56(2):360–368
Schoenwaelder SM, Yuan Y, Josefsson EC, White MJ, Yao Y, Mason KD et al (2009) Two distinct pathways regulate platelet phosphatidylserine exposure and procoagulant function. Blood. J Am Soc Hematol 114(3):663–666
Ghasemzadeh M, Hosseini E, Roudsari ZO, Zadkhak P (2018) Intraplatelet reactive oxygen species (ROS) correlate with the shedding of adhesive receptors, microvesiculation and platelet adhesion to collagen during storage: does endogenous ROS generation downregulate platelet adhesive function? Thromb Res 163:153–161
Villarroel JPP, Figueredo R, Guan Y, Tomaiuolo M, Karamercan MA, Welsh J et al (2013) Increased platelet storage time is associated with mitochondrial dysfunction and impaired platelet function. J Surg Res 184(1):422–429
Redza-Dutordoir M, Averill-Bates DA (2016) Activation of apoptosis signalling pathways by reactive oxygen species. Biochim et Biophys Acta (BBA)-Molecular Cell Res 1863(12):2977–2992
Circu ML, Aw TY (2012) Glutathione and modulation of cell apoptosis. Biochim et Biophys Acta (BBA)-Molecular Cell Res 1823(10):1767–1777
Nunnari J, Suomalainen A (2012) Mitochondria: in sickness and in health. Cell 148(6):1145–1159
Sweeney J, Holme S, Moroff G (1994) Storage of apheresis platelets after gamma radiation. Transfusion 34(9):779–783
Van Der Meer P, Pietersz R (2005) Gamma irradiation does not affect 7-day storage of platelet concentrates. Vox Sang 89(2):97–99
Johnson L, Vekariya S, Wood B, Costa M, Waters L, Green S et al (2021) The in vitro quality of X-irradiated platelet components in PAS‐E is equivalent to gamma‐irradiated components. Transfusion 61(11):3075–3080
Thiele T, Sablewski A, Iuga C, Bakchoul T, Bente A, Görg S et al (2012) Profiling alterations in platelets induced by Amotosalen/UVA pathogen reduction and gamma irradiation-a LC-ESI-MS/MS-based proteomics approach. Blood Transfus 10(Suppl 2):s63
Marrocco C, D’Alessandro A, Girelli G, Zolla L (2013) Proteomic analysis of platelets treated with gamma irradiation versus a commercial photochemical pathogen reduction technology. Transfusion 53(8):1808–1820
Nodeh FK, Hosseini E, Ghasemzadeh M (2021) The effect of gamma irradiation on platelet redox state during storage. Transfusion 61(2):579–593
Slichter SJ, Davis K, Enright H, Braine H, Gernsheimer T, Kao K-J et al (2005) Factors affecting posttransfusion platelet increments, platelet refractoriness, and platelet transfusion intervals in thrombocytopenic patients. Blood 105(10):4106–4114
Gammon R, Boyd T, Chanez T (2020) Standards for blood banks and transfusion services. AABB, Bethesda, MD
Rudmann SV (2005) Textbook of blood banking and transfusion medicine. Elsevier Health Sciences
Kulkarni S, Woollard KJ, Thomas S, Oxley D, Jackson SP (2007) Conversion of platelets from a proaggregatory to a proinflammatory adhesive phenotype: role of PAF in spatially regulating neutrophil adhesion and spreading. Blood 110(6):1879–1886
Jacquemin G, Granci V, Gallouet AS, Lalaoui N, Morlé A, Iessi E et al (2012) Quercetin-mediated Mcl-1 and survivin downregulation restores TRAIL-induced apoptosis in non-hodgkin’s lymphoma B cells. Haematologica 97(1):38
Perrotta PL, Perrotta CL, Snyder EL (2003) Apoptotic activity in stored human platelets. Transfusion 43(4):526–535
Albanyan AM, Harrison P, Murphy MF (2009) Markers of platelet activation and apoptosis during storage of apheresis-and buffy coat–derived platelet concentrates for 7 days. Transfusion 49(1):108–117
Kile BT (2009) The role of the intrinsic apoptosis pathway in platelet life and death. J Thromb Haemost 7:214–217
Bertino A, Qi X, Li J, Xia Y, Kuter D (2003) Apoptotic markers are increased in platelets stored at 37 C. Transfusion 43(7):857–866
Skripchenko A, Myrup A, Thompson-Montgomery D, Awatefe H, Moroff G, Wagner SJ (2010) Periods without agitation diminish platelet mitochondrial function during storage. Transfusion 50(2):390–399
Yoshida T, Goto S, Kawakatsu M, Urata Y, Li T-s (2012) Mitochondrial dysfunction, a probable cause of persistent oxidative stress after exposure to ionizing radiation. Free Radic Res 46(2):147–153
Tynngård N, Trinks M, Berlin G (2015) In vitro function of platelets treated with ultraviolet C light for pathogen inactivation: a comparative study with nonirradiated and gamma-irradiated platelets. Transfusion 55(6):1169–1177
Reid S, Johnson L, Woodland N, Marks DC (2012) Pathogen reduction treatment of buffy coat platelet concentrates in additive solution induces proapoptotic signaling. Transfusion 52(10):2094–2103
Dasgupta SK, Argaiz ER, Mercado JEC, Maul HOE, Garza J, Enriquez AB et al (2010) Platelet senescence and phosphatidylserine exposure. Transfusion 50(10):2167–2175
Vogler M, Hamali HA, Sun X-M, Bampton ET, Dinsdale D, Snowden RT et al (2011) BCL2/BCL-XL inhibition induces apoptosis, disrupts cellular calcium homeostasis, and prevents platelet activation. Blood The Journal of the American Society of Hematology 117(26):7145–7154
Pallepati P, Averill-Bates DA (2011) Mild thermotolerance induced at 40 C protects HeLa cells against activation of death receptor-mediated apoptosis by hydrogen peroxide. Free Radic Biol Med 50(6):667–679
Circu ML, Aw TY (2010) Reactive oxygen species, cellular redox systems, and apoptosis. Free Radic Biol Med 48(6):749–762
Ekshyyan O, Aw T (2005) Decreased susceptibility of differentiated PC12 cells to oxidative challenge: relationship to cellular redox and expression of apoptotic protease activator factor-1. Cell Death & Differentiation 12(8):1066–1077
Pias EK, Yee Aw T (2002) Apoptosis in mitotic competent undifferentiated cells is induced by cellular redox imbalance independent of reactive oxygen species production. FASEB J 16(8):781–790
Deming PB, Schafer ZT, Tashker JS, Potts MB, Deshmukh M, Kornbluth S (2004) Bcr-abl-mediated protection from apoptosis downstream of mitochondrial cytochrome c release. Mol Cell Biol 24(23):10289–10299
Seervi M, Joseph J, Sobhan P, Bhavya B, Santhoshkumar T (2011) Essential requirement of cytochrome c release for caspase activation by procaspase-activating compound defined by cellular models. Cell Death Dis 2(9):e207–e
Baghdadi V, Yari F, Nikougoftar M, Rafiee MH (2020) Platelets apoptosis and clearance in the Presence of Sodium Octanoate during storage of platelet concentrate at 4 C. Cell J (Yakhteh) 22(2):212
Acknowledgements
This work was part of Dr. Ghasemzadeh’s approved project (No. 1396-06-33-2099. Parts of this work were presented as a dissertation for PhD students Fatemeh Kiani nodeh. The authors wish to thank Mr. Reza Ranjbar from Tehran Blood Transfusion Center, Iranian Blood Transfusion Organization.
Funding
The study has been supported by High Institute for Research and Education in Transfusion Medicine, Tehran, Iran.
Author information
Authors and Affiliations
Contributions
Mehran Ghasemzadeh provided conceptual input, supervised and designed the study, did the experiments, analyzed the data and wrote the paper. Ehteramolsadat Hosseini, provided conceptual input, co-supervised the study, did the experiments and co-wrote the paper. Fatemeh Kiani nodeh provided conceptual input, performed the experiments and co-wrote the paper.
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the local ethical committee. Ethic committee approval number: IR.TMI.REC.1396.032 issued by High Institute for Research and Education in Transfusion Medicine.
Conflict of interest
The authors declare no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

10495_2023_1841_MOESM1_ESM.jpg
Supplementary Material 1: Figure S1: The changes of cytosolic and mitochondrial cytochrome c and BAK during storage in non-irradiated PCs. According to “Method” section equal amount of proteins (40 µg) from each cytosolic and mitochondrial fractions were subjected to 12% SDS-PAGE electrophoresis and transferred to PVDF for western blot analysis. Bands were visualized by ChemiDoc XRS + system. Each band selected by free hand tool where its adjusted intensity was quantified using Image lab software (Version 5 build18 from Bio-Rad Laboratories, Inc. USA) (A) shows cytosolic cytochrome c levels in non-irradiated products on Days 1, 3, 5, and 7 of storage (gray section of graph) while the right section of graph (blue) demonstrates the levels of mitochondrial cytochrome c of PLT during the 7 days of storage. (B) shows a gradual decrease in the levels of cytosolic Bak (left section of the graph, gray) while the level of mitochondrial pro-apoptotic Bak gradually increased during storage (blue section of graph). Data were analyzed by the Kruskal–Wallis with Dunn’s multiple comparison tests. Note: ns; not significant p > 0.05, * P < 0 0.05 and **P < 0 0.01. n = 10. Data presented as mean ± SD
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hosseini, E., Nodeh, F.K. & Ghasemzadeh, M. Gamma irradiation induces a pro-apoptotic state in longer stored platelets, without progressing to an overt apoptosis by day 7 of storage. Apoptosis 28, 1141–1153 (2023). https://doi.org/10.1007/s10495-023-01841-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10495-023-01841-5