Abstract
Delays in diagnosis and linkage to HIV care persist among people living with HIV (PLWH), even after expanded access to ART worldwide. Mental health may influence timely linkage to HIV care. Greater understanding of the relationship among gender, mental health, and delayed linkage to HIV care can inform strategies to improve the health of PLWH. We interviewed 426 PLWH initiating HIV care in Cameroon between June 2019 and March 2020 to estimate the prevalence of depression, anxiety, and post-traumatic stress disorder (PTSD) and the association between mental health and entry into care with advanced HIV. Separate multivariable log binomial regression models were used to estimate the association between mental health exposure and entry into HIV care with advanced HIV. Stratified analyses were used to assess effect modification by gender. Approximately 20, 15, and 12% of participants reported symptoms of depression, PTSD, and anxiety, respectively. The prevalence of mental health symptoms did not vary significantly by gender. Overall, 53% of participants enrolled in HIV care with advanced HIV: 51% of men and 54% of women. Screening positive for one of the mental health disorders assessed was associated with greater prevalence of enrollment with advanced HIV among men, but not among women. Future research should examine gender-specific pathways between mental health symptoms and entry into care with advanced HIV, particularly for men in Cameroon. The extent to which untreated mental health symptoms drive gender disparities throughout the HIV care continuum should be explored further.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
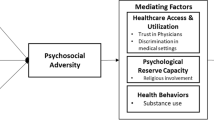
The World Health Organization recommends that all people living with HIV (PLWH) receive lifelong antiretroviral therapy (ART) as soon as possible after diagnosis, a strategy known as ‘treat all’ [1]. Initiating treatment as soon as possible after HIV diagnosis has been associated with improved health outcomes for PLWH and reduced HIV transmission [2,3,4]. The Joint United Nations Programme on HIV/AIDS (UNAIDS) has established worldwide goals of having 95% of PLWH diagnosed, 95% of those diagnosed on ART, and 95% of those on ART virally suppressed . Despite widespread implementation of treat all policies throughout sub-Saharan Africa, delays in diagnosis and linkage to HIV care persist and threaten the widespread success of treat all implementation and achievement of these goals. Delays in diagnosis and linkage to HIV care have individual and public health consequences [5, 6]. At the individual level, late entry into HIV care has been associated with increased risk of ART resistance and HIV-related mortality [7,8,9]. At the population level, late entry into HIV care increases the risk of HIV transmission [10]. The reasons people delay or avoid HIV care are often culture- and context-specific. However, in settings throughout sub-Saharan Africa, late entry into care has been associated with sociodemographic characteristics, including age, gender, and education, as well as with psychosocial stressors, such as HIV-related stigma and social support [11,12,13]. Greater understanding of barriers to timely diagnosis and engagement in HIV care in the context of treat all implementation is essential to improve the health and well-being of PLWH.
The HIV care continuum is a public health model indicating the sequence of steps that PLWH move through from HIV diagnosis to viral suppression, including linkage to HIV care, ART initiation, and retention in HIV care. Gender disparities have been consistently documented throughout the HIV care continuum across sub-Saharan Africa [14,15,16]. Compared to women, men living with HIV in sub-Saharan Africa are less likely to have been diagnosed, initiate ART, be virally suppressed, and report optimal ART adherence [14, 16,17,18]. Research focused on understanding gender disparities throughout the HIV care continuum has largely focused on the gendered nature of health services [17, 19]. That is, health services have traditionally focused largely on maternal and child health concerns, resulting in services that are or are perceived to be primarily oriented toward women [17, 19]. Greater understanding is needed regarding the extent to which other known barriers to optimal HIV outcomes, especially mental health-related barriers, contribute to gender disparities in HIV care continuum outcomes.
Mental health disorders are common among PLWH. While estimates vary across studies and populations, depression, anxiety, and post-traumatic stress disorder (PTSD) are commonly experienced among PLWH and more commonly experienced among PLWH compared to the general population [20,21,22,23,24,25]. Depression is the most prevalent mental health disorder among PLWH. Estimates of depressive symptoms among PLWH in sub-Saharan Africa have ranged between 14 and 32% [22]. Mental health disorders have been associated with suboptimal outcomes throughout the HIV care continuum, including delayed diagnosis and linkage to HIV care [20, 26,27,28]. However, little is known about the extent to which gender modifies the relationship between mental health and HIV care outcomes. Much research into the relationship between mental health and HIV care outcomes has been conducted with gender-specific populations (e.g., women living with HIV, men who have sex with men and are living with HIV), precluding the examination of modification by gender [29,30,31,32]. Among studies that have included men and women living with HIV, few have examined the extent to which gender modifies the relationship between mental health and HIV care outcomes [26, 33, 34]. In addition, much of our understanding of the relationship between mental health and HIV care continuum outcomes is informed by research conducted prior to widespread implementation of treat all policies. Prior to treat all policy implementation, most resource-limited settings implemented CD4-based treatment policies in which ART was available only to PLWH with CD4 cell counts below a specific threshold or PLWH who met other eligibility criteria (e.g., pregnancy). The population targeted by treat all policies (i.e., all PLWH) differs from the population targeted by CD4-based treatment policies in meaningful ways (e.g., less likely to feel unwell). Given the prevalence of mental health disorders among PLWH, the relationship between mental health and HIV care outcomes, gender disparities throughout the HIV care continuum, and widespread implementation of treat all policies, a more nuanced understanding of the intersection of mental health, gender, and HIV care outcomes in the context of national treat all implementation is warranted.
Approximately 540,000 people are living with HIV throughout Cameroon, representing 3.6% of the adult population [35]. Cameroon remains one of the countries in sub-Saharan Africa furthest from achieving the UNAIDS 95-95-95 goals, with 74% of PLWH knowing their HIV status and 52% of PLWH on ART [35]. Similar to many other sub-Saharan African settings, the prevalence of HIV is higher among women than men in Cameroon (4.2% vs. 2.0%, respectively) [35]. However, among PLWH in Cameroon, men are less likely than women to be receiving ART (56% vs. 67%, respectively) and are more likely than women to die from HIV-related causes [35]. ART is available free-of-charge at all levels of the health system in Cameroon. The government of Cameroon began implementation of ‘treat all’ policies in 2016. However, little is known about the impact of mental health disorders on entry into care with advanced HIV among PLWH since implementation of ‘treat all’ policies throughout Cameroon.
This work assessed the prevalence of symptoms of depression, anxiety, and PTSD and the relationship between symptoms of these disorders and entry into care with advanced HIV, a measure reflecting the suboptimal care continuum outcomes of delayed diagnosis and linkage to care. The extent to which gender modified the relationship between mental health symptoms and entry into care with advanced HIV was also explored.
Methods
Data Collection
Data were collected from in-person interviews with 426 individuals newly initiating HIV care at three HIV treatment clinics in Cameroon between June 2019 and March 2020. Study sites were selected because they were participating in the Central Africa International epidemiology Databases to Evaluate AIDS (CA-IeDEA) Cameroon study. IeDEA is a research consortium established with funding from the National Institute of Allergy and Infectious Diseases to collect and harmonize global HIV data [36]. All study sites provide outpatient HIV care and treatment services. Individuals were eligible to participate if they were 21 years or older and newly enrolling in HIV care at one of the three HIV clinics. Individuals transferring care were ineligible. Data collection consisted of one structured interview conducted by a trained research assistant and included questions on mental health, substance use, psychosocial stressors, and sociodemographics. Research assistants were fluent in English and French. Interviews were conducted in English or French, based on the preference of the participant. Study participants also had their CD4 cell counts measured at the HIV care facility within two weeks of enrollment into HIV care. This study was approved by the Institutional Review Board at the University of North Carolina at Chapel Hill and from the National Ethical Committee of Research for Human Health in Yaoundé, Cameroon. All participants provided written informed consent.
Measures
Depressive Symptoms
Depressive symptoms were assessed with the Patient Health Questionnaire-9 (PHQ-9) [37]. The PHQ-9 is a 9-item screener that assesses the presence of depressive symptoms within the last two weeks. Scores for the PHQ-9 range from 0 to 27. Scores of 10 or greater are commonly considered as an indication of a likely depressive disorder [37]. The PHQ-9 has been previously validated in French and with PLWH in sub-Saharan Africa [38,39,40,41].
Anxiety Symptoms
Anxiety symptoms were assessed with the General Anxiety Disorder-7 (GAD-7) [42]. The GAD-7 is a 7-item screener that assesses the presence of anxiety symptoms within the past two weeks. Scores for the GAD-7 range from 0 to 21. Scores of 10 or greater are commonly considered as an indication of moderate or severe anxiety symptoms. The GAD-7 has been validated in French and in clinical and research environments in a range of cultural settings, including among a primary care population with a high prevalence of HIV in sub-Saharan Africa [43,44,45,46].
Post-traumatic Stress Disorder Symptoms
Post-traumatic stress disorder (PTSD) symptoms were assessed with the PTSD Checklist for DSM-5 (PCL-5) [47]. The PCL-5 is a 20-item screener that assesses the presence of PTSD symptoms in the past month. Scores range from 0 to 80. Scores of 31 or greater are indicative of probable PTSD [48]. The PCL-5 has been validated in French and across a range of cultural settings, including among a primary care population with a high prevalence of HIV in Zimbabwe [49,50,51,51].
Any Mental Health Disorder
Individuals who screened positive for a likely depressive disorder, moderate or severe or anxiety symptoms, or probable PTSD were categorized as screening positive for one or more of the mental health disorders assessed. Individuals who screened negative for a likely depressive disorder, moderate or severe anxiety symptoms, and probable PTSD were categorized as screening negative for all mental health disorders assessed.
Entry Into Care with Advanced HIV
CD4 cell count was measured for each participant at the HIV care facility within two weeks of study enrollment. Entry into care with advanced HIV was defined as having a CD4 cell count below 200 cells/μL.
Household Hunger
Household hunger was assessed using the Household Hunger Scale which was developed and validated to measure a household’s ability to access food within the last 30 days [52]. This scale consisted of three questions about household hunger in the past 30 days: was there ever no food to eat of any kind in your house because of lack of resources to get food; did you or any household member go to sleep at night hungry because there was not enough food; did you or any household member go a whole day and night without eating anything because there was not enough food. If participants responded affirmatively to any question, they were asked about frequency of the occurrence. Responses indicating the event never occurred received a score of 0, responses indicating the event occurred “Rarely/Sometimes” received a score of 1, and responses indicating the event occurred “Often” received a score of 2, yielding an overall scale score ranging from 0 to 6. Scores of 2 and greater were considered indicative of moderate to severe household hunger [53].
Sociodemographic Characteristics
Sociodemographic characteristics explored included age, gender, education, relationship status, employment, and number of children.
Data Analysis
Univariate analyses were conducted to assess the prevalence of symptoms of depression, anxiety, and PTSD, overall and separately by gender. Bivariate analyses between each mental health exposure (i.e., depression, anxiety, PTSD) and entry into care with advanced HIV were conducted using Pearson chi-squared tests. Among the entire sample population, separate multivariable log binomial regression models were used to estimate the association of each mental health exposure with entry into care with advanced HIV. Stratified analyses were used a priori to assess effect measure modification by gender. All adjusted analyses controlled for age. Relationship status was highly correlated with age and not included in multivariable analyses. All analyses adjusted for clustering by health facility.
Missing CD4 data. Approximately midway through data collection (November 2019), CD4 testing ceased being available at two of the health facilities at which this survey was conducted. As a result, CD4 cell count was missing for 183 (43%) study participants. Multiple imputation was used to account for missingness of entry into care with advanced HIV under the assumption that these data were missing at random. Pearson’s chi-squared tests were used to identify measured covariates associated with entry into care with advanced HIV in the complete case analysis and measured covariates associated with missingness. One hundred imputations were conducted using the monotone logistic method for each of the three exposure/outcome relationships of interest (i.e., depression, anxiety, and PTSD and entry into care with advanced HIV.) Each separate imputation model included the exposure, age (operationalized as 21–39 or 40 years or older), clinic, an interaction term between gender and the exposure (to allow for stratification of effect estimates by gender), and three auxiliary variables, each of which was independently associated with entry into care with advanced HIV in bivariate analyses. Estimates obtained from the imputed datasets were combined and summarized using standard multiple imputation techniques.
Multivariable Analysis
Log binomial regression was used to estimate unadjusted and adjusted associations between each exposure and entry into care with advanced HIV. These estimates were compared to estimates obtained from the complete case analysis (See supplementary material).
Results
A total of 426 individuals were included in this analysis. Most study participants were women (59%; n = 250), between 21 and 39 years of age (58%; n = 249) and currently in a relationship (58%; n = 249) (Table 1). The majority of participants had some formal education, with 42% (n = 177) having completed secondary school or higher. The majority of participants (81%; n = 345) had at least one child and were working for pay (65%; n = 275). Twenty-eight percent (n = 119) of participants reported moderate or severe household hunger. Men were more likely than women to be in a relationship (65% vs. 53%, respectively) and more likely to be working for pay (74% vs. 58%, respectively).
Approximately 20% (n = 86), 15% (n = 64), and 12% (n = 51) of participants reported symptoms of depression, PTSD, and anxiety, respectively (Table 2). Approximately 30% (n = 119) of participants screened positive for at least one mental health disorder assessed. The prevalence of depression, PTSD, and anxiety symptoms did not differ significantly by gender. Similarly, the severity of depression, PTSD, and anxiety symptoms did not differ significantly by gender (data not shown). That is, among individuals who reported moderate or severe depressive symptoms, the mean PHQ-9 score was not significantly different among men compared to women (14.3 vs. 13.1, respectively). Findings were also similar when comparing mean GAD-7 and PCL-5 scores between men and women (GAD-7: 12.1 vs. 12.9; PCL-5: 43.6 vs. 43.6, respectively).
Among participants for whom CD4 at enrollment into care was available (n = 243), entry into HIV care with advanced HIV was common, with 53% (n = 128) of participants entering care with a CD4 cell count less than 200 cells/μL (Table 3) and 79% entering care with a CD4 cell count under 350 cells/μL. The prevalence of advanced HIV at care entry was not significantly different by gender (51% among men compared to 54% among women).
Analysis Using Multiple Imputation
In the analysis using multiple imputation, among the entire study population, no significant association was observed between depression, anxiety, or PTSD symptoms and advanced HIV at care entry (Table 4). However, among men, adjusted prevalence of advanced HIV at entry into care with moderate or severe depressive symptoms was 1.7 [95% Confidence Interval (CI) 1.1, 2.6] times that among men with no or mild depressive symptoms. In addition, the prevalence of advanced HIV at entry into care among men who screened positive for any mental health disorder assessed was 1.7 (95% CI 1.1, 2.7) times that of men who screened negative for all mental health disorders assessed. Among men, no significant association was observed between anxiety or PTSD and advanced HIV at care entry. Among women, no significant association was observed between anxiety, PTSD, depression, or any mental health disorder assessed and advanced HIV at care entry.
Complete Case Analysis
Similar to findings using multiple imputation, among the entire study population, no significant association was observed between anxiety or PTSD and advanced HIV at care entry. However, in the complete case analysis, among the entire population, the adjusted prevalence of advanced HIV at care entry among those with moderate or severe depressive symptoms was 1.3 (95% CI 1.0, 1.7) times that among individuals with no or mild depressive symptoms (See supplementary materials). In the complete case analysis, among men, in adjusted analyses, symptoms of depression and anxiety, but not PTSD were significantly associated with greater prevalence of advanced HIV at care entry. Similar to findings using multiple imputation, in the complete case analysis, among women, no significant association was observed between depression, anxiety, PTSD, or any mental health disorder and advanced HIV at care entry.
Discussion
Symptoms of three mental health disorders were common among study participants, with 30% of study participants reporting symptoms of one or more of the mental health disorders assessed. Twenty percent of participants reported moderate or severe depressive symptoms, 12% reported moderate or severe symptoms of anxiety, and 15% reported symptoms of probable PTSD. Among the entire study population, in analyses using multiple imputation, no significant association was observed between depression, anxiety, or PTSD symptoms and advanced HIV at care entry. When stratified by gender, moderate or severe depressive symptoms were associated with greater prevalence of advanced HIV at care entry among men, but not among women.
While research is limited, our findings are consistent with previous estimates of depression among PLWH in Cameroon. For example, a study of 202 PLWH on ART in rural North West Cameroon found that 29% screened positive for depressive symptoms while a study of PLWH in Yaounde estimated that 21% of 889 participants screened positive for depressive symptoms [54, 55]. Previous estimates of anxiety among PLWH in Cameroon are also limited. However, one study with PLWH in Yaounde, Cameroon estimated that 11% of participants screened positive for anxiety using the GAD-7 [55]. The authors know of no previous estimates of PTSD among PLWH in Cameroon or of estimates of depression, anxiety, or PTSD among the general population in Cameroon. However, one population-based study in a district in North West Cameroon found that 24% of participants reported moderate or severe depressive symptoms and 31% reported moderate or severe anxiety symptoms [56]. Caution is warranted when comparing the prevalence of mental health symptoms across studies due to differences in measurement, samples, and timing of assessments.
Advanced HIV at care entry was also very common under implementation of a national treat all policy. Among individuals for whom CD4 data were available, approximately half (53%) enrolled in care with a CD4 cell count less than 200 cells/μL. The authors are not aware of previous estimates of entry into care with advanced HIV among PLWH in Cameroon under the implementation of a national treat all policy. A study which examined late presentation to HIV care in Cameroon prior to the implementation of a national treat all policy (between 1996 and 2004) found that 90% of PLWH first presented to HIV care with a CD4 cell count under 350 cells/μL or WHO stage 3 or 4 [57]. In the current study, 79% of PLWH first presented to HIV care with a CD4 cell count under 350 cells/μL, suggesting very little progress towards more timely diagnosis and engagement in HIV care. Entry into care with advanced HIV remains a significant public health problem in Cameroon, despite national implementation of treat all policies. There is an urgent need to advance understanding of barriers to timely diagnosis and engagement in HIV care in the context of national treat all policies. In addition, strategies to monitor and evaluate the impact of national treat all policies should consider incorporating metrics that reflect the timeliness of achievement of key care continuum outcomes, including HIV diagnosis and ART initiation to better track progress towards achieving public health goals of diagnosing and treating all PLWH as soon as possible after seroconversion [6].
Among the entire population, screening positive for depression was associated with greater prevalence of entry into care with advanced HIV in the complete case analysis, but not in the imputed analysis. When stratified by gender, screening positive for any mental health disorder assessed and screening positive for depression were significantly associated with greater prevalence of entry into care with advanced HIV among men. However, among women, there was no significant association between depression, anxiety, PTSD, or any mental health disorder and prevalence of entry into care with advanced HIV in either the imputed analysis or the complete case analysis. The authors are not aware of previous research that examined the extent to which gender modifies the relationship between mental health and entry into care with advanced HIV in sub-Saharan Africa. Much research on the relationship between mental health and HIV care continuum outcomes in sub-Saharan Africa has either focused exclusively on gender-specific populations (e.g., women living with HIV, men who have sex with men and are living with HIV) or has included men and women living with HIV but has not examined effect modification by gender. The directionality of the association between mental health symptoms and delayed entry into HIV care among men and women remains unclear. Mental health disorders may serve as barriers to early engagement in HIV care for men living with HIV in Cameroon. Alternately, HIV diagnosis and physical health challenges associated with advanced HIV may lead to subsequent mental health disorders among men with advanced HIV. Among women, mental health symptoms may serve as a catalyst for earlier care-seeking. Investigation of gender-specific, bidirectional pathways between mental health disorders and HIV care continuum outcomes can inform the adaptation and implementation of evidence-based interventions for men and women living with HIV in Cameroon and other resource-limited settings. Identification of potential mediators and modifiers of the relationship between mental health symptoms and advanced HIV at care initiation among men living with HIV, including mental health- or HIV-related stigma, alcohol or other substance use, history of traumatic life events, food insecurity, and sexual orientation or behavior, can identify men particularly vulnerable to suboptimal mental health or HIV care outcomes. Greater understanding of the extent to which gender modifies the relationship between mental health and other HIV care continuum outcomes, including HIV diagnosis, ART initiation, and sustained viral suppression is also needed. Longitudinal research which examines the incidence and persistence of mental health symptoms as men and women move through the HIV care cascade may yield important insights into windows for intervention and support.
Similar to many resource-limited settings, integration of mental health services into HIV care in Cameroon remains limited [58]. Implementation strategies to expand and strengthen the mental health workforce in HIV treatment settings and beyond are needed, particularly as the integration of mental health and HIV services has been identified as a promising strategy to improve mental health and HIV treatment outcomes among PLWH [59]. Greater understanding of patient, provider, and health-facility level barriers to integration of mental health and HIV treatment services in Cameroon should be explored. For example, a study of primary care providers in Cameroon found that while the majority of providers (93%) recognized that depression warrants medical intervention, 66% reported feeling uncomfortable working with patients who were depressed and less than half (49%) had received formal mental health training [60]. Implementation strategies that address modifiable multilevel barriers to the integration of mental health screening and treatment into routine HIV care services should be developed, implemented, and evaluated.
Because the date of first HIV-positive diagnosis was not available, the current analysis could not distinguish between late testers (e.g., PLWH who received their first HIV positive diagnosis with CD4 < 200 cells/μL) and delayed presenters (e.g., PLWH newly engaging in care more than three months after receiving their first HIV-positive test). Research to understand the extent to which mental health symptoms are associated with both late testing and delayed presentation in the context of treat all policy implementation is needed. Research conducted with PLWH in South Africa prior to the implementation of a national treat all strategy found that severe depression was associated with both late testing and delayed presentation while anxiety was associated only with delayed presentation [23]. Future research into the relationship between gender, mental health, and entry into care with advanced HIV should distinguish between late testers and delayed presenters.
This study has limitations worth noting. All data were collected at entry into HIV care. Thus, we cannot distinguish between individuals with mental health symptom onset prior to versus concurrent with HIV engagement in care. As discussed, we were unable to distinguish between late testers and delayed presenters. In addition, data were collected from three public hospital-based HIV treatment clinics participating in IeDEA Cameroon and may not be generalizable to other populations or settings. Because IeDEA sites have the capacity to routinely contribute electronic data to the IeDEA consortium, these sites may function at a higher level than HIV treatment sites in Cameroon that are not participating in IeDEA. As discussed, due to discontinuation of CD4 testing at two study clinics, 43% of participants were missing CD4 data. However, multiple imputation methods were used to account for missingness of CD4 data, under the assumption that data were missing at random. If the missing at random assumption is violated (i.e. data are missing not at random and missingness is associated with CD4 cell count), estimates from the multiple imputation analysis may be biased. We found no evidence of association between CD4 cell count and date of enrollment, but did identify other observed predictors of CD4 count and missingness.
Conclusions
Depression, anxiety, and PTSD symptoms were common among PLWH entering HIV care in this setting. Screening positive for a mental health disorder was associated with greater prevalence of advanced HIV at care initiation for men but not women in Cameroon. Future research should examine whether gender-specific pathways between mental health symptoms and entry into care with advanced HIV exist. The extent to which untreated mental health symptoms drive gender disparities throughout the HIV care cascade warrants investigation.
Data Availability
The dataset contains sensitive information and is not publicly available. However, it could be made available from the first author (AMP) on reasonable request, with approval from the IRB at the University of North Carolina at Chapel Hill to maintain confidentiality.
Code Availability
All analyses were conducted using SAS. SAS code could be made available from the first author (AMP) on reasonable request.
References
World Health Organization. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. Geneva: World Health Organization; 2015.
Lundgren JD, Babiker AG, Gordin F, Emery S, Grund B, Sharma S, et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;373(9):795–807.
Danel C, Moh R, Gabillard D, Badje A, Le Carrou J, Ouassa T, et al. A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N Engl J Med. 2015;373(9):808–22.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med. 2016;375(9):830–9.
Iwuji CC, Orne-Gliemann J, Larmarange J, Okesola N, Tanser F, Thiebaut R, et al. Uptake of home-based HIV testing, linkage to care, and community attitudes about ART in Rural KwaZulu-Natal, South Africa: descriptive results from the first phase of the ANRS 12249 TasP cluster-randomised trial. PLoS Med. 2016;13(8):e1002107.
Nash D, Robertson M. How to evolve the response to the global HIV epidemic with new metrics and targets based on pre-treatment CD4 counts. Curr HIV/AIDS Rep. 2019;16(4):304–13.
Grangeiro A, Escuder MM, Menezes PR, Alencar R, de Ayres Castilho E. Late entry into HIV care: estimated impact on AIDS mortality rates in Brazil, 2003–2006. PLoS ONE. 2011;6(1):e14585.
Krawczyk CS, Funkhouser E, Kilby JM, Kaslow RA, Bey AK, Vermund SH. Factors associated with delayed initiation of HIV medical care among infected persons attending a southern HIV/AIDS clinic. South Med J. 2006;99(5):472–81.
Haskew J, Turner K, Rø G, Ho A, Kimanga D, Sharif S. Stage of HIV presentation at initial clinic visit following a community-based HIV testing campaign in rural Kenya. BMC Public Health. 2015;15:16.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
Gesesew HA, Tesfay Gebremedhin A, Demissie TD, Kerie MW, Sudhakar M, Mwanri L. Significant association between perceived HIV related stigma and late presentation for HIV/AIDS care in low and middle-income countries: a systematic review and meta-analysis. PLoS ONE. 2017;12(3):e0173928.
Gelaw YA, Senbete GH, Adane AA, Alene KA. Determinants of late presentation to HIV/AIDS care in Southern Tigray Zone, Northern Ethiopia: an institution based case-control study. AIDS Res Ther. 2015;12:40.
Abaynew Y, Deribew A, Deribe K. Factors associated with late presentation to HIV/AIDS care in South Wollo ZoneEthiopia: a case-control study. AIDS Res Ther. 2011;8:8.
Takuva S, Brown AE, Pillay Y, Delpech V, Puren AJ. The continuum of HIV care in South Africa: implications for achieving the second and third UNAIDS 90–90-90 targets. AIDS. 2017;31(4):545–52.
Nsanzimana S, Kanters S, Remera E, Forrest JI, Binagwaho A, Condo J, et al. HIV care continuum in Rwanda: a cross-sectional analysis of the national programme. Lancet HIV. 2015;2(5):e208–15.
Lippman SA, Shade SB, El Ayadi AM, Gilvydis JM, Grignon JS, Liegler T, et al. Attrition and opportunities along the HIV care continuum: findings from a population-based sample, North West Province, South Africa. J Acquir Immune Defic Syndr. 2016;73(1):91–9.
Cornell M, Cox V, Wilkinson L. Public health blindness towards men in HIV programmes in Africa. Trop Med Int Health. 2015;20(12):1634–5.
Osler M, Cornell M, Ford N, Hilderbrand K, Goemaere E, Boulle A. Population-wide differentials in HIV service access and outcomes in the Western Cape for men as compared to women, South Africa: 2008 to 2018: a cohort analysis. J Int AIDS Soc. 2020;23(Suppl 2):e25530.
Cornell M, McIntyre J, Myer L. Men and antiretroviral therapy in Africa: our blind spot. Trop Med Int Health. 2011;16(7):828–9.
Brandt R. The mental health of people living with HIV/AIDS in Africa: a systematic review. Afr J AIDS Res. 2009;8(2):123–33.
Nanni MG, Caruso R, Mitchell AJ, Meggiolaro E, Grassi L. Depression in HIV infected patients: a review. Curr Psychiatry Rep. 2015;17(1):530.
Bernard C, Dabis F, de Rekeneire N. Prevalence and factors associated with depression in people living with HIV in sub-Saharan Africa: a systematic review and meta-analysis. PLoS ONE. 2017;12(8):e0181960.
Rane MS, Hong T, Govere S, Thulare H, Moosa M-Y, Celum C, et al. Depression and anxiety as risk factors for delayed care-seeking behavior in human immunodeficiency virus-infected individuals in South Africa. Clin Infect Dis. 2018;67(9):1411–8.
Choi KW, Sikkema KJ, Velloza J, Marais A, Jose C, Stein DJ, et al. Maladaptive coping mediates the influence of childhood trauma on depression and PTSD among pregnant women in South Africa. Arch Womens Ment Health. 2015;18(5):731–8.
Myer L, Smit J, Roux LL, Parker S, Stein DJ, Seedat S. Common mental disorders among HIV-infected individuals in South Africa: prevalence, predictors, and validation of brief psychiatric rating scales. AIDS Patient Care STDs. 2008;22(2):147–58.
Nakimuli-Mpungu E, Bass JK, Alexandre P, Mills EJ, Musisi S, Ram M, et al. Depression, alcohol use and adherence to antiretroviral therapy in sub-Saharan Africa: a systematic review. AIDS Behav. 2012;16(8):2101–18.
Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum EE, Schuman P, Boland RJ, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV epidemiology research study. J Am Med Assoc. 2001;285(11):1466–74.
Memiah P, Shumba C, Etienne-Mesubi M, Agbor S, Hossain MB, Komba P, et al. The effect of depressive symptoms and CD4 count on adherence to highly active antiretroviral therapy in sub-Saharan Africa. J Int Assoc Provid AIDS Care. 2014;13(4):346–52.
Tao J, Vermund SH, Lu H, Ruan Y, Shepherd BE, Kipp AM, et al. Impact of depression and anxiety on initiation of antiretroviral therapy among men who have sex with men with newly diagnosed HIV infections in China. AIDS Patient Care STDs. 2017;31(2):96–104.
Prabhu S, McFall AM, Mehta SH, Srikrishnan AK, Kumar MS, Anand S, et al. Psychosocial barriers to viral suppression in a community-based sample of human immunodeficiency virus-infected men who have sex with men and people who inject drugs in India. Clin Infect Dis. 2020;70(2):304–13.
Govender K, Durevall D, Cowden RG, Beckett S, Kharsany AB, Lewis L, et al. Depression symptoms, HIV testing, linkage to ART, and viral suppression among women in a high HIV burden district in KwaZulu-Natal, South Africa: a cross-sectional household study. J Health Psychol. 2020. https://doi.org/10.1177/1359105320982042.
Onono M, Odwar T, Abuogi L, Owuor K, Helova A, Bukusi E, et al. Effects of depression, stigma and intimate partner violence on postpartum women’s adherence and engagement in HIV care in Kenya. AIDS Behav. 2020;24(6):1807–15.
Tlhajoane M, Eaton JW, Takaruza A, Rhead R, Maswera R, Schur N, et al. Prevalence and associations of psychological distress, HIV infection and HIV care service utilization in East Zimbabwe. AIDS Behav. 2018;22(5):1485–95.
Wagner GJ, Slaughter M, Ghosh-Dastidar B. Depression at treatment initiation predicts HIV antiretroviral adherence in Uganda. J Int Assoc Provid AIDS Care. 2017;16(1):91–7.
UNAIDS. Country overview: Cameroon. Geneva: UNAIDS; 2020.
Chammartin F, Dao Ostinelli CH, Anastos K, Jaquet A, Brazier E, Brown S, et al. International epidemiology databases to evaluate AIDS (IeDEA) in sub-Saharan Africa, 2012–2019. BMJ Open. 2020;10(5):e035246.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Pence BW, Gaynes BN, Atashili J, O’Donnell JK, Tayong G, Kats D, et al. Validity of an interviewer-administered patient health questionnaire-9 to screen for depression in HIV-infected patients in Cameroon. J Affect Disord. 2012;143(1–3):208–13.
Monahan PO, Shacham E, Reece M, Kroenke K, Ong’or WO, Omollo O, et al. Validity/reliability of PHQ-9 and PHQ-2 depression scales among adults living with HIV/AIDS in western Kenya. J Gen Intern Med. 2009;24(2):189–97.
Akena D, Joska J, Obuku EA, Stein DJ. Sensitivity and specificity of clinician administered screening instruments in detecting depression among HIV-positive individuals in Uganda. AIDS Care. 2013;25(10):1245–52.
Carballeira Y, Dumont P, Borgacci S, Rentsch D, de Tonnac N, Archinard M, et al. Criterion validity of the French version of patient health questionnaire (PHQ) in a hospital department of internal medicine. Psychol Psychother. 2007;80(Pt 1):69–77.
Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Chibanda D, Verhey R, Gibson LJ, Munetsi E, Machando D, Rusakaniko S, et al. Validation of screening tools for depression and anxiety disorders in a primary care population with high HIV prevalence in Zimbabwe. J Affect Disord. 2016;198:50–5.
Zhong QY, Gelaye B, Zaslavsky AM, Fann JR, Rondon MB, Sánchez SE, et al. Diagnostic validity of the generalized anxiety disorder—7 (GAD-7) among pregnant women. PLoS ONE. 2015;10(4):e0125096.
Ruiz MA, Zamorano E, García-Campayo J, Pardo A, Freire O, Rejas J. Validity of the GAD-7 scale as an outcome measure of disability in patients with generalized anxiety disorders in primary care. J Affect Disord. 2011;128(3):277–86.
Micoulaud-Franchi JA, Lagarde S, Barkate G, Dufournet B, Besancon C, Trébuchon-Da Fonseca A, et al. Rapid detection of generalized anxiety disorder and major depression in epilepsy: validation of the GAD-7 as a complementary tool to the NDDI-E in a French sample. Epilepsy Behav. 2016;57(Pt A):211–6.
Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489–98.
Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, et al. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders-fifth edition (PCL-5) in veterans. Psychol Assess. 2016;28(11):1379–91.
Verhey R, Chibanda D, Gibson L, Brakarsh J, Seedat S. Validation of the posttraumatic stress disorder checklist—5 (PCL-5) in a primary care population with high HIV prevalence in Zimbabwe. BMC Psychiatry. 2018;18(1):109.
Ibrahim H, Ertl V, Catani C, Ismail AA, Neuner F. The validity of posttraumatic stress disorder checklist for DSM-5 (PCL-5) as screening instrument with Kurdish and Arab displaced populations living in the Kurdistan region of Iraq. BMC Psychiatry. 2018;18(1):259.
Ashbaugh AR, Houle-Johnson S, Herbert C, El-Hage W, Brunet A. Psychometric validation of the English and French versions of the posttraumatic stress disorder checklist for DSM-5 (PCL-5). PLoS ONE. 2016;11(10):e0161645.
Ballard T, Coates J, Swindale A, Deitchler M. Household hunger scale: indicator definition and measurement guide. Washington DC: Food and Nutrition Technical Assistance II Project, FHI; 2011. p. 360.
USAID. Fanta III Food and Nutrition Technical Asstance. Household hunger scale: indicator definition and measurement guide. 2011. https://www.fantaproject.org/sites/default/files/resources/HHS-Indicator-Guide-Aug2011.pdf
Asangbeh SL, Sobngwi JL, Ekali GL, Eyoum C, Msellati P. Predictors of depression among patients on art in a rural health district in North West Cameroon. AIDS Care. 2016;28(2):205–8.
Pefura-Yone EW, Soh E, Kengne AP, Balkissou AD, Kuaban C. Non-adherence to antiretroviral therapy in Yaounde: prevalence, determinants and the concordance of two screening criteria. J Infect Public Health. 2013;6(4):307–15.
Wallace S, Mactaggart I, Banks LM, Polack S, Kuper H. Association of anxiety and depression with physical and sensory functional difficulties in adults in five population-based surveys in low and middle-income countries. PLoS ONE. 2020;15(6):e0231563.
Luma HN, Jua P, Donfack O-T, Kamdem F, Ngouadjeu E, Mbatchou HB, et al. Late presentation to HIV/AIDS care at the Douala general hospital, Cameroon: its associated factors, and consequences. BMC Infect Dis. 2018;18(1):298.
Parcesepe AM, Mugglin C, Nalugoda F, Bernard C, Yunihastuti E, Althoff K, et al. Screening and management of mental health and substance use disorders in HIV treatment settings in low- and middle-income countries within the global IeDEA consortium. J Int AIDS Soc. 2018;21(3):e25101.
Kaaya S, Eustache E, Lapidos-Salaiz I, Musisi S, Psaros C, Wissow L. Grand challenges: Improving HIV treatment outcomes by integrating interventions for co-morbid mental illness. PLoS Med. 2013;(10)5:e1001447
Mulango ID, Atashili J, Gaynes BN, Njim T. Knowledge, attitudes and practices regarding depression among primary health care providers in Fako division, Cameroon. BMC Psychiatry. 2018;18(1):66.
Funding
This research was supported by NIMH Grant K01 MH114721, NICHD Grant P2C HD050924 (Carolina Population Center), NIAID Grant P30 AI050410 (UNC Center for AIDS Research), and NIAID Grant U01AI096299. This work is solely the responsibility of the authors and does not necessarily represent the official views of any of the institutions mentioned above.
Author information
Authors and Affiliations
Contributions
AP: Conceptualization, funding, analysis, Writing—original draft; LF: Analysis; Writing—review & editing; PVE: Project administration; Writing—review & editing; AD: Project administration; Supervision; Writing—review & editing; RA: Writing—review & editing; MW: Conceptualization; Writing—review & editing; BP: Conceptualization; Writing—review & editing; EP: Project administration; Writing—review & editing; MY: Writing—Review & editing; DNsame: Writing—Review & editing; KA: Writing—review & editing; DNash: Conceptualization; Writing—review & editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by the Institutional Review Board at the University of North Carolina at Chapel Hill and the National Ethical Committee of Research for Human Health in Cameroon.
Informed Consent
All participants provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Parcesepe, A.M., Filiatreau, L.M., Ebasone, P.V. et al. Gender, Mental Health, and Entry Into Care with Advanced HIV Among People Living with HIV in Cameroon Under a National ‘Treat All’ Policy. AIDS Behav 25, 4018–4028 (2021). https://doi.org/10.1007/s10461-021-03328-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-021-03328-3