Abstract
Victimization from physical and sexual violence presents global health challenges. Partner violence is higher in Kenya than Africa. Violence against drinkers and HIV-infected individuals is typically elevated, so dual vulnerabilities may further augment risk. Understanding violence risks can improve interventions. Participants were 614 HIV-infected outpatient drinkers in western Kenya enrolled in a randomized trial to reduce alcohol use. At baseline, past 90-day partner physical and sexual violence were examined descriptively and in gender-stratified regression models. We hypothesized higher reported violence against women than men, and positive violence association with HIV stigma and alcohol use across gender. Women reported significantly more current sexual (26.3 vs. 5.7%) and physical (38.9 vs. 24.8%) victimization than men. Rates were generally higher than Kenyan lifetime national averages. In both regression models, HIV stigma and alcohol-related sexual expectations were significantly associated with violence while alcohol use was not. For women, higher violence risk was also conferred by childhood violence, past-year transactional sex, and younger age. HIV-infected Kenyan drinkers, particularly women, endorse high current violence due to multiple risk factors. Findings have implications for HIV interventions. Longitudinal research is needed to understand development of risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Victimization from physical and sexual violence represents a global public health problem [1]. Adverse effects of violence include impaired physical and mental health, risky behaviors and perpetuation of the cycle of violence [2–8]. International rates of lifetime physical or sexual partner violence among ever-partnered women have been reported to be 30%, with 36.6% of women reporting violence in the Africa region [1]. In Kenya, rates of violence are reported to be higher than the regional average. In the nationally representative 2014 Kenya Demographic and Health Survey among ever-married Kenyan women age 15–49, prevalence of lifetime partner violence was reported to be 38.4% (physical) and 14% (sexual). Among these women, partner violence in the past 12 months was reported to be 23% (physical) and 10% (sexual) [3]. Studies examining partner violence against men have found much lower rates than reported by women [3]. Among ever-married Kenyan men age 15–49 surveyed in the 2014 Kenya Demographic and Health Survey, 5% reported experiencing partner physical violence in the past 12 months and 8.6% reported lifetime partner physical violence. Also 3% of men reported experiencing partner sexual violence in the past 12 months and 4.4% reported lifetime partner sexual violence [3].
Partner violence is reported to be higher among HIV-infected women than women in the general population in Kenya. For example, in a community study of women attending an STI clinic in Nairobi Kenya, Fonck and colleagues found the rate of lifetime physical partner violence among women was reported to be higher among those who are HIV-infected (26%) than seronegative women (17%) [9]. We could find no studies reporting rates of partner violence against HIV-infected heterosexual men in sub-Saharan Africa. The explanation for the association between partner violence and HIV infection is not fully understood. Some researchers have found that partner violence can predispose one to acquire HIV infection. For example, Maman and colleagues posit that violence can increase risk of HIV infection via several avenues: sexual assault by an HIV-infected person, limited condom use negotiation, or increased subsequent risky sexual behaviors [2]. Others suggest that diagnosis of HIV can lead to increased sexual and physical victimization, with evidence shown that women experience increased violence following HIV disclosure [10, 11]. The prevalence of HIV-related stigma in sub-Saharan Africa likely contributes to increased violence. In a regional study of 1073 HIV-infected Kenyan men and women, nearly 30% of respondents reported experiencing some form of stigma or discrimination in the past 12 months due to HIV infection. And just over half of Kenyan respondents had disclosed HIV to spouse or partner [12]. One study showed that stigmatized HIV-infected Kenyan women can become more susceptible to violence following eviction from marital homes and loss of property after HIV disclosure, forcing them to live in unsafe informal settlements [4].
Other factors beyond HIV can also contribute to violence. There is a large literature showing that alcohol use can increase risk of victimization from partner violence, e.g., [13–16]. This relationship has been explained by some researchers as due to disinhibition or distorted perceptions of cues associated with alcohol use [17]. Some data has shown that alcohol use reported by a woman’s partner rather than by the victim has been more predictive of violence [18]. Other variables associated with alcohol use such as expectations of alcohol’s effect have also been shown to be associated with violence [19], particularly among those with a history of sexual victimization [15]. For example, alcohol expectancies include the belief that alcohol can results in enhanced or uninhibited sex, or reduced shyness or anxiety around sex [20, 21]. Drinking alcohol may bias an individual to attend to positive sexual cues (e.g., sexual arousal) consistent with expectations instead of attending to contradictory or threatening cues suggesting increased risk of sexual violence [15].
Other variables such as victimization from childhood violence have been associated with adverse outcomes that may predispose to violence. Experience of victimization from childhood physical or sexual violence has been associated with a host of adverse outcomes including psychiatric symptoms, engagement in abusive adult relationships and partner violence, substance use, and risky sexual behaviors [5, 6]. In a representative study of childhood abuse among men and women ages 18–32 from four communities in Tanzania, South Africa, and Zimbabwe, Richter and colleagues found associations between childhood sexual/physical violence experienced before age 12 and adult risky behaviors including alcohol use, drug use and partner violence. Researchers also found that past childhood violence exposed adult men to a higher risk of HIV-infection and partner abuse [6]. In a study of 2782 rural South African youth age 15–26, Jewkes and colleagues found that childhood adversity and abuse led to higher rates of HIV-infection, substance abuse, and psychiatric symptoms among women, and higher rates of substance use and psychiatric symptoms among men [5].
In countries with poverty and gender inequalities such as Kenya [4, 22], risk of partner violence may also be related to income-generating activities such as transactional sex. Transactional sex, or offering sex in exchange for receiving money or goods, has been reported by sub-Saharan women in the general population who do not identify as sex workers [23, 24]. Transactional sex has been shown to be associated with increased risk of partner violence [25, 26] and HIV infection [26]. In western Kenya, Robinson and Yeh found that women engaged in transactional sex to compensate for financial losses during times of household illness [24]. Similarly, in our pilot study in western Kenya, several HIV-infected women drinkers reported engaging in transactional sex as a method to pay for college, school fees or rent [27], with reported drinking at times to facilitate transactional sex. One possible avenue for transactional sex to increase risk of victimization from violence may be less control in these sexual relationships. In a representative study in Botswana and Swaziland, food insufficiency, or not having enough to eat over the previous 12 months, was associated among 1050 women with transactional sex, lack of control in sexual relationships, inconsistent condom use with their irregular partners, and sexual relations with intergenerational partners [23]. Informal transactional sex has also been associated with higher HIV risk. In a study of 1395 women attending an antenatal clinic in South Africa, 21.1% of women reported ever engaging in transactional sex with a non-primary partner. And informal sex workers with non-primary partners were 54% more likely to be HIV-infected than those not informal sex workers [26]. Finally, a history of childhood violence has also been identified as a risk factor for engaging in transactional sex. In one of the few studies of transactional sex among men, who largely provided rather than received goods and money, Dunkle and colleagues found higher rates of victimization from childhood violence than men who did not engage in transactional sex [28]. In addition, transactional sex may also lead to violence due to women’s limit on power in the transactional relationship, with less opportunity to engage in safer sexual practices like condom use or to prevent violence [29].
In sum, the literature on violence against HIV-infected Kenyan women and men drinkers suggests increased vulnerability due to multiple potential risk factors including alcohol use, sexual expectations, HIV stigma, childhood violence and transactional sex. Given these multiple risk factors for partner violence, it is important to know more about rates and covariates of violence in this population to develop more relevant and targeted HIV prevention interventions. This study offers a unique opportunity to examine these associations in a large baseline sample. Hence, the purpose of this study was to examine rates and correlates of reported victimization from physical and sexual violence among a sample of 614 HIV-infected men and women outpatient drinkers in western Kenya. We hypothesized that women would report higher rates of victimization from physical and sexual violence than men and that alcohol use and HIV stigma would be positively associated with violence for both men and women.
Methods
Participants
Participants were 614 HIV-infected outpatient drinkers in western Kenya who were enrolled in a randomized clinical trial of a cognitive-behavioral therapy intervention to reduce alcohol use. This trial was performed within the clinical services of the US Agency for International Development—AMPATH program (AMPATH), initially established in 2001 between Moi Teaching and Referral Hospital, Moi University School of Medicine, and a consortium of universities from North America in response to the HIV epidemic in Kenya [30, 31]. AMPATH delivers care, provides education, and performs research in networks of urban and rural Ministry of Health hospitals, health centers, and dispensaries in western Kenya. AMPATH currently follows >85,000 HIV-infected patients in 22 sub-counties of 8 counties in western Kenya. Study inclusion criteria were: age ≥18 years, enrollment as an AMPATH HIV-infected outpatient attending any of four HIV clinics, hazardous or binge drinking criteria (score ≥3 on the Alcohol Use Disorders Identification Test (AUDIT-C) [32, 33] or more than six drinks per occasion at least monthly), alcohol use in the past 30 days, verbal working knowledge of Kiswahili and living within 1 h travel distance from the Eldoret AMPATH clinic, where the study was conducted. Exclusion criteria were active psychosis or active suicidality, which were assessed through screening. Any positive screens were followed with a referral to psychiatrists in the mental health services department.
Study Procedures
Recruitment of participants occurred between July 2012 and September 2015. Outpatients were approached by same-sex research staff and asked for verbal consent for a brief interview to describe a health behavior study and to determine eligibility. Written informed consent was obtained from all eligible and interested participants. All participant interviews were audio-taped and conducted by same-sex research staff in a private setting using a computer survey interface. The current study presents measures administered at baseline prior to the intervention. The institutional review boards of the participating research organizations approved the study protocols.
Instruments
All instruments were culturally and linguistically adapted using WHO-modified methods [34]. Instruments were translated into Kiswahili, the national language of Kenya. We conducted forward and back translations by local experts, with review by a multidisciplinary panel of health experts and alcoholics in recovery. We then pre-tested measures and discussed the measures during two focus groups, one consisting of 11 women and the other attended by 9 men, all of whom were HIV-infected outpatients, and who drank alcohol in the past 6 months. Modifications in language were made in response to group and multidisciplinary panel input. Our adaptation methods are described elsewhere [27]. Seven-day test–retest reliability was conducted among 36 study trial participants following recruitment into the study. Retest analyses were conducted using Pearson correlation for continuous variables. For dichotomous variables, we analyzed both percent agreement and kappa statistics. For some variables, kappa scores were lower regardless of high agreement due to low variability (e.g., relatively fewer participants endorsed occurrence of sexual violence).
Current Physical and Sexual Violence
Questions on interpersonal violence assessed victimization from physical or sexual violence within the past 90 days. Items were adapted from the 2003 Kenya Demographic and Health Survey [35] which has demonstrated validity and reliability. They were modified to assess the past 90 days. The sexual violence item was worded to capture “anyone” rather than “partner” so that all sexual assaults were captured. Items were: In the past 90 days did any partner physically assault you such as pushing, slapping, punching, kicking, strangling, burning or threatening you with a weapon? In the past 90 days, did anyone force you to have sex, rape you, or force you to perform a sexual act that you did not want? Seven-day test–retest reliability for these adapted measures in this study was as follows: current physical violence percent agreement was 80.6% (kappa = 0.48), current sexual violence percent agreement was 88.9% (kappa = 0.28).
Childhood Physical and Sexual Violence
Questions on interpersonal violence assessed victimization from physical or sexual violence in childhood. Items were adapted from the 2003 Kenya Demographic and Health Survey [35]. They were modified to assess a childhood history. The violence items were worded to capture “anyone” rather than “partner”. Items were: When you were a child, did anyone physically assault you such as pushing, slapping, punching, kicking, strangling, burning or threatening you with a weapon? When you were a child, did anyone force you to have sex, rape you, or force you to perform a sexual act that you did not want? Seven-day test–retest reliability for these adapted measures in this study was: childhood physical violence percent agreement was 77.8% (kappa = 0.57), childhood sexual violence percent agreement was 80.6% (kappa = 0.13).
Demographic Variables
We asked participant age. For relationship status, we asked whether participant was: (1) married and living with spouse, (2) married and not living with a spouse, (3) not married and living with a partner and (4) not married and not living with a partner. We combined the first two items into a “married” variable and the last two items into a “single” variable.
Income
We assessed total estimated income for the past year in Kenyan shillings. We also assessed whether income was earned in the past year from “having sex with someone (even if occasionally).” We did not assess receipt of any other forms of remuneration such as goods. Seven-day test–retest reliability for these items in this survey was: total income r = 0.69, income from having sex - percent agreement was 91.7% (kappa = 0.81). Median income is shown in Kenyan shillings, which can be divided by 90 consistent with the current exchange rate to US dollars.
Alcohol use
The Alcohol Use Disorders Identification Test-Consumption (AUDIT-C)—is a reliable, valid 3-item quantity-frequency measure of alcohol use which was used as a screening tool to measure at risk harmful alcohol use [32, 33]. AUDIT-C methods were adapted in this study based on our previous work [36] and additional pre-testing in this study. Standard drinks about commercial alcohol were augmented with standard drinks about traditional brew: 550 ml of busaa (maize beer) and 100 ml of changaa (spirits). Included were typical receptacles showing volumes of a standard drink of busaa and of chang’aa. For item 1, the response of “monthly or less” was split into two options: “less than monthly” and “monthly.” An illustration of the “less than monthly” frequency was also displayed. The AUDIT-C assessed alcohol use in the past year. Seven-day test–retest reliability for the AUDIT-C in this study was r = 0.61. Results showed that AUDIT-C scores were lower at retest than during original baseline administration (Mean (M) of 7.1 vs (M) 6.3), suggesting reactivity to enrollment in the intervention study.
HIV-Related Stigma
This 11-item stigma scale assessed perception of HIV-related stigma in the past 30 days. This valid, reliable scale demonstrates four factors: public attitudes toward HIV infection, feeling ostracized for HIV, discrimination, and personal life disruption [37, 38]. We included this variable in this analysis of violence for past 90 days because we have found that stigma is this setting is persistent and not acute, particularly given average 6.8 years on average since HIV diagnosis. Seven-day test–retest reliability in this study was r = 0.81.
Sexual Expectations Related to Alcohol Use
The 13-item scale assessed sexual expectations about alcohol use. This valid, reliable scale has 3 factors: alcohol will: (1) enhance sex, (2) decrease nervousness around sex, and (3) increase risky behaviors around sex [20, 21]. Seven-day test–retest reliability in this study was r = 0.67.
Statistical Analyses
We examined baseline demographic characteristics and prevalence of physical and sexual violence separately by gender. To assess differences by gender, we used χ 2 test for dichotomous variables and used Wilcoxon rank sum test for continuous variables. Distribution of age was symmetric and therefore we used t test to assess gender difference.
Outcome was defined to be whether a participant experienced victimization from either sexual or physical violence in the past 90 days (yes or no). We developed logistic regression models to identify predictors of current violence for women and men based on the literature review. First, we adjusted for all listed covariates in the logistic model to examine their relationship with the outcome. Then we selected factors shown to be associated with the outcome at 0.10 level. We then fit a reduced model showing the effect of selected covariates on the outcome. We selected a significance level of 0.10 to reflect the exploratory nature of examining covariates of violence among HIV-infected drinkers in a resource-limited setting.
Results
Descriptive Data
Demographics
With regard to age, men (M = 40.3 years, standard deviation (SD) = 8.1) were somewhat older than women (M = 37.5, SD = 7.6, p < 0.001). More men than women reported being married (77.9 vs. 28.8%, p < 0.001). Estimated median past-year income was significantly higher among men than women (U.S. $444.44 vs. U.S. $127.78, p < 0.001). With regard to income-generating activities in the past year, more women than men reported earning income from having sex with someone (66.1 vs. 11.7%, p < 0.001) (Table 1).
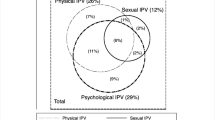
Current Physical and Sexual Violence
For both men and women, being victimized in the past 90 days by physical violence was more prevalent than sexual violence. More women than men reported victimization from current sexual violence (26.3 vs. 5.7%, p < 0.001) and current partner physical violence (38.9 vs. 24.8%, p < 0.001). Similarly, when current physical and sexual violence were combined into one variable, more women than men reported victimization from violence in the past 90 days (48.1 vs. 27.5%, p < 0.001).
Covariates
With regard to childhood violence, more women reported a history of sexual violence (25.3 vs. 12.8%, p < 0.001), while more men reported a history of physical violence (62.1 vs. 52.2%, p < 0.001). When childhood physical and sexual violence were combined into one variable, differences in frequency between men and women were not significant (64.1 vs. 57.9%, p = 0.117). Alcohol risk measured by the AUDIT-C (which was an inclusion criterion for the study) was reported to be in the at-risk range on average. However, men (M = 6.9, SD = 2.6) endorsed a significantly higher quantity-frequency of alcoholic drinks in the past year than women (M = 6.3, SD = 2.3, p < 0.001). Sexual expectations related to alcohol use were not significantly different between women and men (Women, M = 20.6, SD = 11.5 vs. Men, M = 19.0, SD = 10.1, p = 0.101). With regard to HIV-related stigma, women reported perceiving significantly more HIV-related stigma than men (M = 33.2, SD = 12.3 vs. M = 25.5, SD = 11.4, p < 0.001) (Table 1).
Logistic Regression Analysis by Gender
When we included all variables in the logistic regression model for women, several variables were independently associated with current violence at the p < 0.10 significance level. Reporting a childhood history of experiencing violence, reporting earned income from having sex in the past year, sexual expectations about alcohol use and HIV-related stigma were significantly associated with higher risk of experiencing current violence, while older age was associated with lower risk of current violence (Table 2). The final model contained these five variables, which were significantly associated with current violence (Table 3). In the logistic regression model for men, two variables were associated with current violence at the p < 0.10 significance level: sexual expectations about alcohol use and HIV-related stigma (Table 4). The final model contained these two variables, which were significantly associated with current violence (Table 5).
Discussion
This study examined rates and covariates of current victimization from physical and sexual violence against HIV-infected women and men drinkers in Kenya. As expected, the rates of reported physical partner violence and sexual violence were significantly higher among HIV-infected women than men. More women than men reported victimization from current sexual violence (26.3 vs. 5.7%) and current partner physical violence (38.9 vs. 24.8%). A noteworthy finding was that rates of current violence for women and men were equivalent to or higher than lifetime national averages in Kenya, and higher than a community study of violence among HIV infected women in Kenya [9]. In our study, 38.9% of HIV-infected women drinkers reported victimization from recent physical partner violence, nearly equivalent to lifetime rates of partner physical violence (38.4%) reported by women in a nationally representative Kenyan study [3]. The rates of reported victimization from current sexual violence (26.3%) were higher than lifetime partner sexual violence reported in the Kenyan nationally representative study (14.0%). Among HIV-infected men, 24.8% in our study reported experiencing recent physical partner violence, which is almost 3 times the national reported average for lifetime physical partner violence (9.0%) among Kenyan men [3]. The prevalence of reported victimization from current sexual violence among men (5.7%) was also higher than lifetime partner sexual violence reported in the national survey (4.4%). It should be noted that our sexual violence variable was broadened to include violence initiated by anyone not only a partner, which may contribute to higher prevalence of sexual violence. However, studies have shown that sexual violence is most often committed by a casual, former or current partner than another perpetrator [3]. Also, while a majority of women in our study were not married, data shows that partner violence is typically higher among married or formerly married women than single women [3].
In the regression models, we hypothesized that alcohol use would be positively associated with victimization from violence for both men and women. This hypothesis was not supported as alcohol use was not significantly associated with violence for men or women. This finding was somewhat surprising given the strong associations between alcohol use and violence in the literature [13, 14]. However, our finding that sexual expectations associated with alcohol use were significantly associated with violence for both women and men is consistent with other research showing that the expectation about alcohol’s effect on shyness and sexuality is associated with violence [15, 19] Also, studies have shown that violence against women has been correlated with alcohol use of the partner rather than of the victim [18]. Another possible contributor to this finding includes the different time interval of past 12 months for the AUDIT measure as compared to past 3 months for rates of violence. A more sensitive test of the current association between violence and alcohol use would be examined if both variables encompassed the same time period identified as “current.” We also hypothesized that HIV stigma would be positively associated with violence for men and women. This hypothesis was supported, indicating that Kenyan women and men can be dually burdened by both HIV stigma and violence in a climate where HIV stigma and discrimination are commonplace.
In the regression model for women, a history of childhood violence additionally conferred 1.8 times the risk of partner physical or sexual violence. Our finding is consistent with literature showing that victimization from childhood physical or sexual violence can predispose or increase adverse outcomes associated with violence and other covariates of violence [5, 6]. It should be noted that reported rates of victimization from childhood sexual violence in our study were consistent with local and regional data. In our study, 25.3% of women and 12.8% of men reported experiencing childhood sexual violence. Our findings were similar to those of two nationally representative studies of childhood sexual violence in Kenya. In one study, researchers found rates of 23.1% (girls) and 11.8% boys [39]. Results of a second study showed rates of 14.8% of sexual violence against Kenyan boys before age 18 in 3 countries including Kenya [40]. Finally, our results are consistent with sexual violence rates of 27.9% (girls) and 13.4% (boys) before age 18 found in a nationally representative study in Tanzania [41]. We could find no studies examining rates of childhood physical violence to compare against our rates of 52.2% (women) and 62.1% (men). However, Richter and colleagues found that 14.9% of boys and 4.3% of girls in a Muslim region of Tanzania had experienced “serious physical violence” before 12 years of age [6]. A representative study of young men and women 18–25 in rural South Africa found that 89.3% of women and 94.4% men had experienced physical punishment at home during childhood [5]. It is not clear who the perpetrators of the childhood violence were, but in a nationally representative study in Kenya, teachers were found to be the most common perpetrators of physical violence against men and against never married women starting in adolescence (since age 15) [3]. A history of childhood violence was not associated with current violence for men in our study. One possible explanation is that victimization from childhood violence predisposed men to become the aggressors rather than the victims in adult interactions [7, 8].
Earning income from sex in the past year conferred 1.7 times the risk of current violence among women. This finding is consistent with data showing increased vulnerability of women due to less power in the transactional relationship [29]. The high rates of transactional sex reported in this study, 66.1% (women) and 11.7% (men), were surprising. Our findings showed much higher rates than 21.1% reported by outpatient women in South Africa [26]. Although we cannot rule out that some study participants identified as sex workers, the dialogue during intervention sessions was largely consistent with mainstream transactional sex to fund everyday needs. Women in our study reported earning approximately 1/3 less income than men in the past year, namely approximately $128. These findings suggest that women with limited income-generating opportunities may resort to transactional sex to meet basic needs. Note that average per capita income in 2015 in Kenya was $1,340 according to the World Bank [22].
Finally, older women experienced reduced risk of current violence. These data are inconsistent with nationally representative data showing that risk of lifetime physical violence increases with age [3]. It may be that these women have learned how to better protect themselves over time, or may engage in fewer high-risk relationships with age.
Together these results create a picture of HIV-infected heavier drinkers, particularly women, who are more vulnerable to high rates of victimization from violence and coercion due to multiple risk factors—childhood violence, transactional sex, HIV-related stigma, history of drinking, and sexual expectations about alcohol use. Because of the correlational nature of our study, we were not able to disentangle the chronology of these multiple risks. Given an average of 6.8 years since HIV diagnosis among individuals in our study, it is likely that victimization from childhood violence preceded HIV infection for the majority of individuals. Prospective studies could help to delineate the contribution and course of development after childhood violence of alcohol use, HIV infection, transactional sex and partner violence.
These data have implications for HIV prevention interventions in the following ways. Interventionists can include education about the role of childhood violence and other risk factors like transactional sex, alcohol use and risky behaviors in predisposing toward heightened risk for violence. HIV prevention programs that do not take into account the role of violence and these risk factors may be less successful in reducing sexual risk behaviors when women do not always have control over sexual decision making. For example, it may be helpful to nonjudgmentally educate victims of violence about their heightened risk for reduced attention toward cues of subsequent victimization and to teach them how to accurately identify potential individual cues and develop coping plans for how to respond to such cues. As violence can be fostered by cultural norms about gender, Dunkle and colleagues suggest that changing the cultural norms of masculinity and control over women might reduce both gender-based violence and transactional sex [28, 42]. One intervention that has been helpful to reduce violence in the community is called the Stepping Stones intervention, which is intended to improve sexual health through building strong, more gender-equitable relationships using enhanced communication. A randomized controlled trial in South Africa found that the program not only reduced HSV infection, but also resulted in lower reported rates by men of perpetrating partner violence [43]. Given the multifaceted stressors experienced by HIV-infected drinkers, it may be effective to integrate CBT alcohol reduction interventions into programs such as Stepping Stones, to reduce alcohol use and address the interactive nature of these risk factors.
Limitations
Limitations of our study include that it employed a cross-sectional and observational design and therefore cannot infer causality. Our study was not designed to be representative and may not be generalizable to other HIV-infected drinkers in the region or country. With regard to our violence assessment, our items were inclusive of multiple acts of violence and the specific nature or number of times of the act cannot be discerned. Also our childhood violence item did not include specific age categories so it is not known at what ages the childhood violence was experienced. In addition, there also may be recall bias associated with childhood violence (although 7-day test–retest reliability was acceptable).
Conclusion
Findings of our study suggest that HIV-infected heavier drinkers particularly women are at increased risk of victimization from violence due to the burden of multiple stressors—childhood violence, poverty, transactional sex, HIV-related stigma, history of drinking, and sexual expectations about alcohol use. For women, childhood violence and transactional sex explained largest magnitude of association with current violence. For both men and women HIV stigma and sexual expectations associated with alcohol use conferred risk. Given the dearth of studies examining rates and covariates of violence among HIV-infected drinkers in Kenya, our study offers preliminary data about the relationships associated with risk of violence in these individuals. Further research is needed to determine the chronological development and interplay of these risks among these individuals.
Our findings have implications for HIV prevention interventions that can target these risk factors. Multifaceted interventions promoting both gender-equitable relationships as well as alcohol reduction techniques may provide benefits.
References
World Health Organization. Global Status Report on Violence Prevention 2014. http://www.refworld.org/docid/54aa8de14.html. Accessed 4 Aug 2016.
Maman S, Campbell J, Sweat MD, Gielen AC. The intersections of HIV and violence: directions for future research and interventions. Soc Sci Med. 2000;50(4):459–78.
National Bureau of Statistics-Kenya and ICF International. 2015. 2014 Kenya Demographic and Health Survey Final Report. Rockville MD USA. http://dhsprogram.com/pubs/pdf/FR308/FR308.pdf. Accessed 11 Aug 2016.
Amuyunzu-Nyamongo M, Okeng’O L, Wagura A, Mwenzwa E. Putting on a brave face: the experiences of women living with HIV and AIDS in informal settlements of Nairobi, Kenya. AIDS Care. 2007;19(sup1):25–34.
Jewkes RK, Dunkle K, Nduna M, Jama PN, Puren A. Associations between childhood adversity and depression, substance abuse and HIV and HSV2 incident infections in rural South African youth. Child Abuse Negl. 2010;34(11):833–41.
Richter L, Komarek A, Desmond C, et al. Reported physical and sexual abuse in childhood and adult HIV risk behaviour in three African countries: findings from Project Accept (HPTN-043). AIDS Behav. 2014;18(2):381–9.
Dodge KA, Bates JE, Pettit GS. Mechanisms in the cycle of violence. Science. 1990;250(4988):1678–83.
Duke NN, Pettingell SL, McMorris BJ, Borowsky IW. Adolescent violence perpetration: associations with multiple types of adverse childhood experiences. Pediatrics. 2010;125(4):e778–86.
Fonck K, Els L, Kidula N, Ndinya-Achola J, Temmerman M. Increased risk of HIV in women experiencing physical partner violence in Nairobi, Kenya. AIDS Behav. 2005;9(3):335–9.
Maman S, Mbwambo JK, Hogan NM, et al. HIV-positive women report more lifetime partner violence: findings from a voluntary counseling and testing clinic in Dar es Salaam, Tanzania. Am J Public Health. 2002;92(8):1331–7.
Kiarie JN, Farquhar C, Richardson BA, et al. Domestic violence and prevention of mother-to-child transmission of HIV-1. AIDS (London, England). 2006;20(13):1763.
PLHIV Stigma Index Kenyan Country Assessment: Nairobi: NEPHAK; 2011. http://www.stigmaindex.org/sites/default/files/reports/Kenya%20People%20Living%20with%20HIV%20Stigma%20Index%20Report%202009.pdf. Accessed 11 Aug 2016.
Foran HM, O’Leary KD. Alcohol and intimate partner violence: a meta-analytic review. Clin Psychol Rev. 2008;28(7):1222–34.
Leonard KE. Alcohol and intimate partner violence: when can we say that heavy drinking is a contributing cause of violence? Addiction. 2005;100(4):422–5.
Corbin WR, Bernat JA, Calhoun KS, McNair LD, Seals KL. The role of alcohol expectancies and alcohol consumption among sexually victimized and nonvictimized college women. J Interpers Viol. 2001;16(4):297–311.
Klostermann KC, Fals-Stewart W. Intimate partner violence and alcohol use: Exploring the role of drinking in partner violence and its implications for intervention. Aggress Violent Behav. 2006;11(6):587–97.
Steele CM, Josephs RA. Alcohol myopia: Its prized and dangerous effects. Am Psychol. 1990;45(8):921.
Makayoto LA, Omolo J, Kamweya AM, Harder VS, Mutai J. Prevalence and associated factors of intimate partner violence among pregnant women attending Kisumu District Hospital, Kenya. Matern Child Health J. 2013;17(3):441–7.
Leonard KE. Alcohol consumption and escalatory aggression in intoxicated and sober dyads. J Stud Alcohol. 1984;45(1):75–80.
Leigh BC. Alcohol expectancies. Psychol Addict Behav. 1990;4:91–106.
Leigh BC. The relationship of sex-related alcohol expectancies to alcohol consumption and sexual behavior. Br J Addict. 1990;85(7):919–28.
World Bank. Kenya: GNI per capita, Atlas method (current US$) 2016 http://data.worldbank.org/country/kenya. Accessed 10 Dec 2016
Weiser SD, Leiter K, Bangsberg DR, et al. Food insufficiency is associated with high-risk sexual behavior among women in Botswana and Swaziland. PLoS Med. 2007;4(10):e260.
Robinson J, Yeh E. Transactional sex as a response to risk in Western Kenya. Am Econ J Appl Econ. 2011;3(1):35–64.
Hunter M. The materiality of everyday sex: thinking beyond’prostitution’. Afr Stud. 2002;61(1):99–120.
Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Transactional sex among women in Soweto, South Africa: prevalence, risk factors and association with HIV infection. Soc Sci Med. 2004;59(8):1581–92.
Papas RK, Sidle JE, Martino S, et al. Systematic cultural adaptation of cognitive-behavioral therapy to reduce alcohol use among HIV-infected outpatients in western Kenya. AIDS Behav. 2010;14(3):669–78.
Dunkle KL, Jewkes R, Nduna M, et al. Transactional sex with casual and main partners among young South African men in the rural Eastern Cape: prevalence, predictors, and associations with gender-based violence. Soc Sci Med. 2007;65(6):1235–48.
Luke N. Age and economic asymmetries in the sexual relationships of adolescent girls in sub-Saharan Africa. Stud Fam Plann. 2003;34(2):67–86.
Einterz RM, Kimaiyo S, Mengech HNK, et al. Responding to the HIV pandemic: the power of an academic medical partnership. Acad Med. 2007;82(812):818.
Mamlin J, Kimaiyo S, Nyandiko W, Tierney W, Einterz R. Academic institutions linking access to treatment and prevention: Case study. Geneva: World Health Organization; 2004.
Gordon AJ, Maisto SA, McNeil M, et al. Three questions can detect hazardous drinkers. J Fam Pract. 2001;50(4):313–20.
Saunders JB, Aasland OG, Babor TF, DeLaFuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804.
World Health Organization. WHO—Process of translation and adaptation of instruments. 2009. http://www.who.int/substance_abuse/research_tools/translation/en/. Accessed 10 Aug 2016.
National Bureau of Statistics-Kenya and ICF International. 2004. 2003 Kenya Demographic and Health Survey Final Report. Rockville MD USA: Kenya National Bureau of Statistics (KNBS) and ICF Macro. http://dhsprogram.com/pubs/pdf/FR151/FR151.pdf Accessed 10 Aug 2016.
Papas RK, Sidle JE, Wamalwa ES, et al. Estimating alcohol content of traditional brew in Western Kenya using culturally relevant methods: the case for cost over volume. AIDS Behav. 2010;14(4):836–44.
Kingori C, Reece M, Obeng S, et al. Psychometric evaluation of a cross-culturally adapted felt stigma questionnaire among people living with HIV in Kenya. AIDS Patient Care STDS. 2013;27(8):481–8.
Reece M. HIV-related mental health care: factors influencing dropout among low-income, HIV-seropositive individuals. AIDS Care. 2003;15(5):707–16.
Mwangi MW, Kellogg TA, Brookmeyer K, et al. Perpetrators and context of child sexual abuse in Kenya. Child Abuse Negl. 2015;44:46–55.
Sumner SA, Mercy JA, Buluma R, et al. Childhood sexual violence against boys: a study in 3 countries. Pediatrics. 2016;137(5):e20153386.
Vagi KJ, Brookmeyer KA, Gladden RM, et al. Sexual violence against female and male children in the United Republic of Tanzania. Violence Against Women. 2016.
Dunkle KL, Jewkes R. Effective HIV prevention requires gender-transformative work with men. Sex Transm Infect. 2007;83(3):173–4.
Jewkes R, Nduna M, Levin J, et al. Impact of stepping stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. BMJ. 2008;337:a506.
Acknowledgments
This research was funded by Grant R01AA020805 from the U.S. National Institute on Alcohol Abuse and Alcoholism (NIAAA). It was also supported in part by a grant to the USAID-AMPATH Partnership from the United States Agency for International Development as part of the President’s Emergency Plan for AIDS Relief. Preparation of this manuscript was supported in part by NIAAA Grant 2K05 16928. We thank the participants for their role in this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Papas, R.K., Gakinya, B.N., Mwaniki, M.M. et al. Rates and Covariates of Recent Sexual and Physical Violence Against HIV-Infected Outpatient Drinkers in Western Kenya. AIDS Behav 21, 2243–2252 (2017). https://doi.org/10.1007/s10461-017-1684-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1684-y