Abstract
Resiliency factors such as social support have been associated with more frequent HIV testing among MSM. We examined the association between social support and delayed HIV testing in the context of structural discrimination and individual factors among young Black MSM. We combined two independent cross-sectional samples recruited 1 year apart from a venue-based, modified time-location sampling study of young Black MSM aged 18–29 years in the US South. Our subsample (N = 813) was men who self-reported not being HIV positive and who indicated they had one or more male sex partners in the past 2 months. Using a social epidemiology framework we estimated associations of structural (racism and homophobia), social (social support from other Black MSM friends) and individual factors with delayed HIV testing (>6 months ago) using logistic regression. Bivariate analyses demonstrated that individual level variables as well as experiences of racism (OR 1.20, 95% CI 1.02–1.41) and homophobia (OR 1.49, 95 % CI 1.02–2.17) were associated with higher risk of delayed HIV testing. Receiving social support from other Black MSM friends was associated with lower risk of delayed HIV testing (OR 0.80, 95 % CI 0.67–0.95). In multivariable models, social support remained significantly associated with lower risk of delayed HIV testing after inclusion of structural and individual level variables. Social support has a positive and robust association with HIV testing among young Black MSM. Whether community building and development of resiliency factors can overcome structural, social, and individual-level barriers to HIV prevention and care for young Black MSM warrants further study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the United States, Blacks have disproportionally higher HIV incidence and prevalence compared to other racial/ethnic groups [1, 2]. Young Black men who have sex with men (MSM) (aged 13–29 years) have had the largest estimated increase in HIV incidence between 2006 and 2010 [1, 3]. Black MSM have the highest estimated HIV prevalence of any group in the US, with estimated prevalence reaching 30 % in some urban areas [4, 5]. These disparities are likely exacerbated by a higher proportion of Black MSM who are unaware of their HIV infection, are more likely to be diagnosed with more advanced HIV disease, and therefore are more likely to be infectious to sexual partners [5, 6].
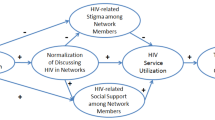
Given these HIV-related disparities among Black MSM exist despite a similar or lower prevalence of individual-level risk factors (e.g., substance use, HIV-related sexual risk behaviors), structural or social factors may better explain the origin of such disparities [7–10]. Poundstone et al. [11] provide a social epidemiologic framework for understanding HIV incidence in the context of broader social factors (e.g., social capital, neighborhoods, social networks) and structural factors (e.g., structural violence and discrimination) in addition to individual-level risk factors. By extension, this model can offer insight into structural and social factors that may drive co-factors of HIV incidence (e.g., delay in HIV testing) within vulnerable populations like young Black MSM.
HIV testing is the first step in the HIV care cascade and an important component of HIV prevention interventions focused on MSM [12–15]. A few studies have examined the role that social factors have on HIV testing among Black MSM. Lauby et al. [16, 17] showed that social support (the ability to connect with others in a social network for material, emotional, or strategic support) was associated with a lower risk of delayed testing among Black and Latino MSM. In this study, men with more social support were less likely to have unrecognized HIV infection. These findings were present after adjusting for important sociodemographic variables and the individual’s MSM network size. Furthermore, among young Black MSM in three US cities, Mashburn et al. [18] found that higher levels of social support were positively associated with having ever tested for HIV. The association between experiences of structural discrimination and HIV testing among Black MSM has been less well researched. In a recent study by Ford et al. [19], perceived everyday racism was associated with higher odds of HIV testing among Black sexually transmitted disease clinic attendees. However, the majority of participants in this study were women and the proportion of the sample who were MSM was not reported.
To date, no studies have simultaneously evaluated the structural, social, and individual factors associated with HIV testing among Black MSM. Using the Poundstone et al. multilevel framework for understanding HIV incidence as a guide, this analysis examines the impact of structural (experiences of racism and homophobia), social (social support), and individual factors (age, socioeconomic status, and sexual risk behavior) on delayed HIV testing in a sample of young Black MSM residing in two southern U.S. cities. Our hypothesis is that more social support will be associated with a lower likelihood of delayed testing even after accounting for racism, homophobia, and individual-level factors. The effect of social support should be especially pronounced in men who report more frequent experiences of discrimination and men who engage in high risk sexual behavior.
Methods
Sample
Data for this analysis were collected from a larger community-level HIV prevention intervention trial of young Black MSM in Dallas, TX with a control community of Houston, TX. Prior to the implementation of the intervention two independent cross-sectional samples, separated by 1 year, were conducted in each community for baseline assessment. To be eligible for the survey, men had to be between the ages of 18–29, report their race as Black or African American, live in either the Dallas or Houston metropolitan areas, be able to complete the survey in English, and report sex with another man in the past 12 months.
A total of 1,329 men completed the survey during the two survey cycles (666 in February–May 2009, 337 in Dallas and 329 in Houston; 663 in June–August 2010, 328 in Dallas and 335 in Houston), including 40 men who participated in both assessments, for whom only the first survey assessment was utilized. Because this analysis focused on HIV testing among men who are currently sexually active, we excluded men who did not report any male sex partners in the past 2 months (n = 391, 30 %). The 2 months recall time frame for sexual partners was pre-determined by the original study protocol. An additional 79 men were excluded who self-reported testing HIV positive. The final analytic sub-sample includes 813 young Black MSM who were sexually active with at least one male partner in the past 2 months and self-reported that their last HIV test was negative, that they did not receive the results of their last HIV test, or that they had never tested for HIV.
Recruitment
A modified venue-based time-location sampling (TLS) approach adapted from the National HIV Behavioral Surveillance Survey (NHBS) was used, following formative work to establish feasibility to recruit young Black MSM [20]. A variety of venues were eligible for inclusion including bars, clubs, retail establishments, restaurants and cafes, adult bookstores and bathhouses, high-traffic street locations, parks, and other social or religious organizations. Venues which provided health services (including HIV/sexually transmitted infection [STI] testing or prevention services) were excluded from the sampling frame. For feasibility considerations, two modifications were made to the NHBS TLS venue sampling method: (1) venues and sampling periods were selected to maximize representation and efficiency in sampling for 4-h sampling time periods, and (2) at least eight young Black MSM had to be present at the beginning of the sampling period in order for data collection to proceed. No more than 20 surveys were collected at any venue during a sampling time period.
Procedures
At each sampling venue, potential participants were consecutively approached and screened for eligibility. The majority of men approached agreed to screening (92 %), and 94 % of those screened agreed to participate in the study. Participants completed the survey using hand-held personal digital assistants (PDAs) that presented written questions sequentially and allowed participants to respond directly on the device. The survey took, on average, 24 min (interquartile range 17–29 min) to complete and included assessments of demographic characteristics, psychosocial variables (e.g., social support, experiences of homophobia and racism, religiosity/spirituality, experiences with difficult sexual situations), HIV testing history, sexual behavior in the past 2 months, socioeconomic distress, and perception of their neighborhood environment. Data were collected anonymously. All study procedures were approved by the institutional review boards at the principal investigator’s home institution, the institution of the data collection subcontractor in each city, and the Centers for Disease Control and Prevention (CDC).
Measures
Structural Discrimination
Experiences of racism and homophobia measures were assessed for this domain. We used eleven items adapted from Díaz et al.’s [21] scale to assess men’s experiences of racism in the past year. Sample items included assessment of experience of racism in various domains (e.g., “How often have your civil rights been violated (i.e., job or housing discrimination due to racism, racial discrimination, or racial prejudice)?”; and “How often have others reacted to you as if they were afraid of you because of your racial and/or ethnic group?”). Five point Likert-scale responses ranged from “never” to “very often” (Cronbach’s alpha = 0.92).
Participant experiences of homophobia in the past year were assessed using seven items adapted from Díaz et al.’s [21] longer eleven item scale. Sample items included assessment of experience of homophobia in various domains (e.g., “How often were you made fun of or called names for being effeminate (“girly”) or for being attracted to other men (or gay or bisexual)?”; and “How often did you feel your attraction to other men (or being gay or bisexual) hurt or embarrass your family?”). Again, five point Likert-scale responses ranged from “never” to “very often” (Cronbach’s alpha = 0.81).
The Diaz scales above were originally developed for Latino MSM who were immigrants to the US and we adapted the scale items and dropped any that were culturally inappropriate for Black MSM. Exploratory factor analysis confirmed that each of the newly adapted scales is unidimensional, and the high scores on the Cronbach’s alpha statistic for each of the scales (all above 0.8) show that they are internally consistent.
Social Support
Instrumental and emotional support that participants received from Black gay/bisexual male friends was measured using four items adapted from our previous research [22]. Sample items included assessment of social support in various domains (e.g., “Being with my African American gay/bi male friend(s) help me feel good about myself”; and “My African American gay/bi male friend(s) is (are) good at helping me solve problems”). Responses ranged from “disagree strongly” to “agree strongly” along a six-point scale (Cronbach’s alpha = 0.83).
Socioeconomic Distress
Seven dichotomous indicators of low socioeconomic status were used to create a composite score of socioeconomic distress. These included: (1) not having a high school degree or GED, (2) not currently being employed full time, (3) having a personal annual income of less than $20,000, (4) running out of money in at least 1 month out of the past 12, (5) borrowing money from friends or family to get by financially in the past year, (6) ever being incarcerated, and (7) ever being homeless. The socioeconomic distress score is a count of how many of those seven socioeconomic distress indicators were reported by the respondent.
High Risk Sexual Behavior
Respondents were asked to report the number of times they engaged in unprotected anal intercourse (UAI) with a male partner in the past 2 months and the HIV serostatus of those partners. Respondents defined as having had UAI with a non-concordant partner (UAINON) included men of unknown HIV serostatus who reported any UAI in the prior 2 months, and HIV-negative men who reported UAI with an HIV-positive partner or a partner of unknown HIV serostatus.
Delayed HIV Testing
The outcome variable is a dichotomization of HIV testing latency based on the self-reported date of last HIV test. Delayed HIV testing was operationalized as last testing for HIV more than 6 months prior to the survey completion date. Semiannual HIV testing for sexually active MSM was consistent with the recommendations of the CDC and state public health officials at the time of data collection [23].
Data Analysis
Our objective was to test associations between structural discrimination (experiences of racism, experiences of homophobia), social (social support from African American gay/bisexual male friends), and individual variables (age, socioeconomic distress score, UAI with a non-concordant male partner in the past 2 months) and delayed HIV testing. All of these variables except the dichotomous UAINON were continuous and so were evaluated to determine if they met the assumption that their relationship with the logit of the outcome variable was linear. Age had a curvilinear relationship and was categorized into three groups (18 years, 19–26 years, and 27–29 years). Both experiences of homophobia and the socioeconomic distress score displayed threshold effects and were dichotomized at the observed break points. Despite their statistical significance, the remaining two correlates manifested odds ratios close to 1 with standard errors close to 0, which indicated that a 1-point change in scale score was not the appropriate unit of measurement. Consequently, the experiences of racism scale score was divided by 10 and the social support scale score was divided by 6 so that odds ratios would reflect the change in the odds of delayed testing per 10-point and 6-point changes in the respective scale scores.
Logistic regression was used to estimate the odds of delayed HIV testing in three hierarchical models. Using the social epidemiologic framework from Poundstone et al., we estimated the odds of delayed testing for structural discrimination factors (experiences of racism and homophobia) (Model 1), the components of Model 1 with social support (Model 2), and finally the components of Model 2 with individual variables (age, socioeconomic distress, and UAINON) (Model 3). Statistical analysis was conducted using Stata Release 12 (College Station, TX).
Results
Of the 813 non-HIV positive young Black MSM who self-reported having one or more male sex partners in the prior 2 months, 750 (92.3 %) had tested HIV-negative on their last test while 63 (7.7 %) were of unknown HIV serostatus. Their median age was 23 (interquartile range 20-25). Three-quarters of the participants had at least a high school degree or GED, and 11.2 % had at least a college degree (Table 1). While slightly more than half reported being employed full-time, a similar percentage of respondents reported running out of money in the prior 12 months. Almost 30 % of the sample had been incarcerated at least once, and 1 in 7 reported ever experiencing homelessness. Just under half of the participants reported more than one anal sex partner in the prior 2 months, and 51.4 % reported UAI during this same time period, although only a small minority (15 %) did so with a non-concordant partner.
Overall, 30.3 % of the sample had not been tested for HIV in the past 6 months, including 6.3 % who had never been tested before. More frequent experiences of racism (OR 1.20, 95 % CI 1.02–1.41) and homophobia (OR 1.49, 95 % CI 1.02–2.17) were associated with delayed HIV testing in bivariate analyses (Table 2). Young Black MSM who reported receiving more social support from other Black MSM were less likely to report delayed HIV testing (OR 0.80, 95 % CI 0.67–0.95). In addition, participants were more likely to report delayed HIV testing if they scored higher on the socioeconomic distress index (OR 1.60, 95 % CI 1.17–2.19), were at either extreme of the age distribution (age 18 vs. ages 19–26, OR 3.36, 95 % CI 1.80–6.29, ages 27–29 vs. ages 19–26, OR 1.53, 95 % CI 1.02–2.27), or reported UAI with a non-concordant partner (OR 3.08, 95 % CI 2.07–4.57).
The results of the hierarchical logistic regression analysis are shown in Table 3. When the experiences of racism and homophobia in the past year are both included in Model 1, the point estimates decrease compared to the bivariate analyses and they are no longer statistically significant individually. However, the combined structural discrimination domain remained significantly associated with delayed HIV testing (p = 0.019). Social support from Black gay or bisexual male friends was included with structural measures in Model 2. The magnitude of its association with delayed HIV testing is nearly identical with the bivariate analysis (p = 0.012). The odds ratios for the structural discrimination variables are slightly attenuated as compared to the Model 1 results (p = 0.037). Individual level variables were added in Model 3 and were significantly associated with delayed HIV testing (p < 0.001), although the socioeconomic distress variable no longer achieved statistical significance. The relationship of the structural domain with delayed HIV testing was further attenuated, resulting in statistical nonsignificance (p = 0.206), but the magnitude of the relationship between social support and delayed HIV testing was virtually unchanged and remained significant (p = 0.047). Model 3 displayed adequate fit with a logit model (Hosmer–Lemeshow goodness-of-fit test p = 0.426).
In order to evaluate the hypothesis that the relationship between delayed HIV testing and social support from African American gay/bisexual male friends may be moderated by structural discrimination (experiences of homophobia and racism) and current sexual risk behavior (UAINON), we tested all possible social support-based two-way interactions and three-way interactions (e.g., social support by UAINON by discrimination). None achieved statistical significance.
Discussion
In this study we demonstrate that for currently sexually active young Black MSM, having social support from their peers is associated with more recent HIV testing. That association was robust to adjustment for experiences of racism and homophobia, socioeconomic disadvantage, sexual risk behavior, and age. These findings align with other studies that have shown that social support has an association with positive health outcomes such as lower rates of unprotected anal sex and unrecognized HIV infection [16, 24]. Lauby et al. demonstrated that potential behavioral pathways for the association with lower unrecognized infections were more recent HIV testing and lower rates of high-risk sexual behavior. Our results are consistent with those findings, and also demonstrate that specifically having the support of other Black gay and bisexual male friends facilitates recent HIV testing. Being aware of one’s HIV serostatus is the first step in the HIV treatment cascade, and has important implications for potentially reducing incident HIV infections [25, 26].
It is likely that having strong social support serves as a buffer against many of the structural barriers which can impede positive health behavior, and may help the young men to cope with fear or anxiety they may have about testing itself, or about finding out that they are HIV infected. Thus, having the social support of other Black MSM friends may foster an environment that provides more support for accessing HIV testing and other HIV prevention services. These findings demonstrate the resiliency of young Black MSM in the context of structural discrimination.
Socioeconomic distress also has been documented in the literature as a potential driver of HIV infection among Black MSM [7]. However, there have been very few studies which have examined measures of socioeconomic distress on HIV testing among Black MSM in the setting of other structural and social factors. Possible explanations for the association between socioeconomic distress and delayed HIV testing include access to healthcare services and other HIV prevention services, and competing needs such as housing, food security, and employment [27]. While access to HIV testing is necessary, it is not sufficient and HIV testing utilization is also dependent on other factors like perceived HIV risk, stigma, and medical distrust [28–31]. In this urban sample of young Black MSM, men who reported more indicators of socioeconomic distress were more likely to have delayed HIV testing, but the effect no longer achieves statistical significance after adjustment for other factors like social support and sexual risk behavior.
The structural discrimination domains of homophobia and racism were broad in this analysis and similar to those used in prior studies [21]. It is likely that experiences of racism and homophobia affect HIV prevention utilization as Voisin et al. [32] reported in a qualitative study of young Black MSM. In that study, although young Black MSM reported access to HIV prevention information, apathy, homophobia, and stigma were key barriers reported for not adopting HIV prevention strategies. Our results support this finding, and suggest that the resiliency obtained from having social support from other Black MSM has the potential to mitigate some of these barriers. Thus, an intervention that emphasizes community building among young Black MSM may be efficacious in achieving positive HIV-related health outcomes [22, 33, 34].
In our analysis we found that men who reported UAI with a non-concordant partner had a significantly higher risk of delayed HIV testing. Mimiaga et al. [35] also reported that UAI with a non-concordant partner was associated with delayed HIV testing. These data suggest that the young men at the highest risk for HIV acquisition through high risk non-concordant sexual activity are not undergoing recent HIV testing. Understanding the structural, social, and individual motivations and barriers for accessing HIV testing should be a focus of prevention interventions targeting these men [36].
There are important limitations to this study. This was a cross-sectional survey of young Black MSM in two southern US cities who were sampled using a modified TLS approach. Men who do not identify with or frequent these venues will likely be missed in our sampling methodology. However, TLS has been used in multiple large cross-sectional studies of MSM, and over 1200 young Black MSM were sampled in this study [37–39]. In this study, we did not assess frequency of HIV testing, only date of last HIV test. We use a 6 months time period to define delayed testing among these men, while other studies have used a longer (12 months or more) reference period [16, 36, 40]. The shorter time period used for this analysis is reflective of current recommendations for semiannual HIV testing among MSM with multiple sex partners. Nearly half of participants reported more than one male anal sex partner in the prior 2 months, and this proportion is likely higher for longer recall periods. Given the high incidence of HIV among young Black MSM, disparities in unrecognized infections, and the importance of HIV testing for entry into the treatment cascade, undergoing HIV testing every 6 months is in line with current public health messaging [12, 41].
Since we only had data for self-reported HIV status, we were not able to assess the association between social support and unrecognized HIV infection directly. Given that rates of unrecognized infections are higher among younger MSM and Black MSM, this may have led to inclusion of HIV seropositive men in our HIV negative sub-sample. However, HIV testing for these men is still relevant given that they self-report being HIV negative or of unknown HIV serostatus. Finally, recall and social desirability biases are important considerations given the content of our survey. Participants were asked to recall individual risk behaviors over the past 2 months and entered data anonymously using PDAs in an effort to reduce these biases.
Conclusions
Among young Black MSM who are sexually active, social support is positively associated with adherence to HIV testing recommendations in the setting of structural discrimination and individual risk factors. The development of interventions to increase HIV testing among these men should include components which leverage this important source of resiliency. Feeling that one has support for dealing with the potentially difficult situation and outcome of HIV testing appears to be beneficial in helping young men engage in this health behavior. Future cross-sectional and longitudinal cohorts should include social support measures in order to facilitate the exploration of the association between resiliency among these men and utilization of HIV prevention services.
References
CDC. Estimated HIV incidence in the United States, 2007–2010. HIV surveillance supplemental report 2012, vol. 17, No 4, 2012.
CDC. HIV surveillance report, 2011, vol 23. http://www.cdc.gov/hiv/topics/surveillance/resources/reports (2013). Accessed 11 Aug 2013.
Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS ONE. 2011;6(8):e17502.
Chen M, Rhodes PH, Hall IH, Kilmarx PH, Branson BM, Valleroy LA, et al. Prevalence of undiagnosed HIV infection among persons aged ≥13 years—National HIV Surveillance System, United States, 2005–2008. MMWR Morb Mortal Wkly Rep. 2012;61(Suppl):57–64.
Wejnert C, Le B, Zhu J, Finlayson T, Oster A, Smith A, et al. HIV Prevalence and awareness of infection in 2008 and 2011 among men who have sex with men: 20 US Cities. In: Conference on retroviruses and opportunistic infections; 2013, abstract #902013.
CDC. Disparities in diagnoses of HIV infection between blacks/African Americans and other racial/ethnic populations—37 States, 2005–2008. MMWR Morb Mortal Wkly Rep. 2011;60:93–8.
Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8.
Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21(15):2083–91.
Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of black men who have sex with men: a critical literature review. Am J Public Health. 2006;96(6):1007–19.
Magnus M, Kuo I, Phillips G, Shelley K, Rawls A, Montanez L, et al. Elevated HIV prevalence despite lower rates of sexual risk behaviors among black men in the District of Columbia who have sex with men. AIDS Patient Care STDS. 2010;24(10):615–22.
Poundstone KE, Strathdee SA, Celentano DD. The social epidemiology of human immunodeficiency virus/acquired immunodeficiency syndrome. Epidemiol Rev. 2004;26:22–35.
Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800.
CDC. Vital signs: HIV prevention through care and treatment–United State. MMWR Morb Mortal Wkly Rep. 2011;60(47):1618–23.
Kellerman SE, Lehman JS, Lansky A, Stevens MR, Hecht FM, Bindman AB, et al. HIV testing within at-risk populations in the United States and the reasons for seeking or avoiding HIV testing. J Acquir Immune Defic Syndr. 2002;31(2):202–10.
Helms DJ, Weinstock HS, Mahle KC, Bernstein KT, Furness BW, Kent CK, et al. HIV testing frequency among men who have sex with men attending sexually transmitted disease clinics: implications for HIV prevention and surveillance. J Acquir Immune Defic Syndr. 2009;50(3):320–6.
Lauby JL, Marks G, Bingham T, Liu KL, Liau A, Stueve A, et al. Having supportive social relationships is associated with reduced risk of unrecognized HIV infection among black and Latino men who have sex with men. AIDS Behav. 2012;16(3):508–15.
Cohen S. Social relationships and health. Am Psychol. 2004;59(8):676–84.
Mashburn AJ, Peterson JL, Bakeman R, Miller RL, Clark LF. Influences on HIV Testing among young African-American men who have sex with men and the moderating effect of the geographic setting. J Commun Psychol. 2004;32:45–60.
Ford CL, Daniel M, Earp JA, Kaufman JS, Golin CE, Miller WC. Perceived everyday racism, residential segregation, and HIV testing among patients at a sexually transmitted disease clinic. Am J Public Health. 2009;99(Suppl 1):S137–43.
MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, Sullivan PS. Surveillance of HIV risk and prevention behaviors of men who have sex with men—a national application of venue-based, time-space sampling. Public Health Rep. 2007;122(Suppl 1):39–47.
Díaz RM, Ayala G, Bein E. Sexual risk as an outcome of social oppression: data from a probability sample of Latino gay men in three U.S. cities. Cultur Divers Ethnic Minor Psychol. 2004;10(3):255–67.
Kegeles SM, Hays RB, Coates TJ. The Mpowerment Project: a community-level HIV prevention intervention for young gay men. Am J Public Health. 1996;86(8):1129–36.
CDC. Sexually transmitted diseases treatment guidelines. MMWR Morb Mortal Wkly Rep. 2010;59:1–109.
Peterson JL, Coates TJ, Catania JA, Middleton L, Hilliard B, Hearst N. High-risk sexual behavior and condom use among gay and bisexual African-American men. Am J Public Health. 1992;82(11):1490–4.
Pinkerton SD, Holtgrave DR, Galletly CL. Infections prevented by increasing HIV serostatus awareness in the United States, 2001 to 2004. J Acquir Immune Defic Syndr. 2008;47(3):354–7.
Holtgrave DR, Pinkerton SD. Can increasing awareness of HIV seropositivity reduce infections by 50% in the United States? J Acquir Immune Defic Syndr. 2007;44(3):360–3.
Adimora AA, Schoenbach VJ. Social context, sexual networks, and racial disparities in rates of sexually transmitted infections. J Infect Dis. 2005;191(Suppl 1):S115–22.
Graham JL, Grimes RM, Slomka J, Ross M, Hwang LY, Giordano TP. The role of trust in delayed HIV diagnosis in a diverse, urban population. AIDS Behav. 2013;17(1):266–73.
German D, Sifakis F, Maulsby C, Towe VL, Flynn CP, Latkin CA, et al. Persistently high prevalence and unrecognized HIV infection among men who have sex with men in Baltimore: the BESURE study. J Acquir Immune Defic Syndr. 2011;57(1):77–87.
Nelson KM, Thiede H, Hawes SE, Golden MR, Hutcheson R, Carey JW, et al. Why the wait? Delayed HIV diagnosis among men who have sex with men. J Urban Health. 2010;87(4):642–55.
Seekins D, Scibelli A, Stryker R, Das A. Barriers to accessing HIV testing, care, and treatment in the United States. In: 18th international AIDS conference, Vienna; 2010, abstract THPE0624.
Voisin DR, Bird JD, Shiu CS, Krieger C. “It’s crazy being a Black, gay youth.” Getting information about HIV prevention: a pilot study. J Adolesc. 2013;36(1):111–9.
Hays RB, Rebchook GM, Kegeles SM. The Mpowerment Project: community-building with young gay and bisexual men to prevent HIV 1. Am J Community Psychol. 2003;31(3–4):301–12.
Kegeles SM, Hays RB, Pollack LM, Coates TJ. Mobilizing young gay and bisexual men for HIV prevention: a two-community study. AIDS. 1999;13(13):1753–62.
Mimiaga MJ, Reisner SL, Bland S, Skeer M, Cranston K, Isenberg D, et al. Health system and personal barriers resulting in decreased utilization of HIV and STD testing services among at-risk black men who have sex with men in Massachusetts. AIDS Patient Care STDS. 2009;23(10):825–35.
MacKellar DA, Valleroy LA, Secura GM, Behel S, Bingham T, Celentano DD, et al. Unrecognized HIV infection, risk behaviors, and perceptions of risk among young men who have sex with men: opportunities for advancing HIV prevention in the third decade of HIV/AIDS. J Acquir Immune Defic Syndr. 2005;38(5):603–14.
CDC. HIV risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance System, 21 US Cities, United States, 2008. MMWR Morb Mortal Wkly Rep. 2011;SS 60(14):1–34.
Sanchez T, Finlayson T, Drake A, Behel S, Cribbin M, Dinenno E, et al. Human immunodeficiency virus (HIV) risk, prevention, and testing behaviors–United States, National HIV Behavioral Surveillance System: men who have sex with men, November 2003-April 2005. MMWR Surveill Summ. 2006;55(6):1–16.
Karon JM, Wejnert C. Statistical methods for the analysis of time-location sampling data. J Urban Health. 2012;89(3):565–86.
Bowleg L, Burkholder GJ, Massie JS, Wahome R, Teti M, Malebranche DJ, et al. Racial discrimination, social support, and sexual HIV risk among Black heterosexual men. AIDS Behav. 2013;17(1):407–18.
CDC. Sexually transmitted diseases treatment guidelines, 2010. MMWR Morb Mortal Wkly Rep. 2010;59(RR-12):1–109.
Acknowledgments
The authors would like to thank Dr. Agatha Eke and Dr. Wayne Johnson, from the CDC; Dr. Kenneth Jones, formerly of the CDC; Dr. Jan Risser, formerly of the University of Texas, Houston; Paige Wermuth of University of Texas, Houston; and Anne Freeman and Doug Sheehan of the University of Texas Southwestern, Dallas, Texas. This work was supported by cooperative agreement #UR6PS000334 from the Centers for Disease Control and Prevention. HMS received support from the Traineeship in AIDS Prevention Studies T32 postdoctoral fellowship (MH-19105-23) from the National Institutes of Mental Health of the U.S. Public Health Service.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scott, H.M., Pollack, L., Rebchook, G.M. et al. Peer Social Support is Associated with Recent HIV Testing Among Young Black Men Who Have Sex with Men. AIDS Behav 18, 913–920 (2014). https://doi.org/10.1007/s10461-013-0608-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-013-0608-8