Abstract
Men in sub-Saharan Africa have low HIV testing rates. Social networks exert an important influence on men’s HIV-related behavior. We examined associations between network factors and HIV testing among men in Dar es Salaam, Tanzania. Data are from the baseline assessment of an HIV prevention trial with 48 primarily male networks. Among 923 sexually active men, 52 % had ever tested for HIV. In a random effects logistic regression model, men in the network core were 1.50 times more likely (p < .05) to test than those in the periphery. Percentage of women in the network was associated with men’s increased HIV testing (AOR 4.24, p < .05). Perception of network HIV stigma was negatively associated with HIV testing (AOR 0.92, p < .01). Thinking at least one close friend tested for HIV was associated with increased testing (AOR 2.66, p < .001). Social network interventions are a promising approach for scaling up men’s HIV testing.
Resumen
Las tasas de realización de pruebas de VIH son bajas entre los hombres en África sub-Sahariana. Las redes sociales ejercen una influencia importante sobre las conductas relacionadas con el VIH entre los hombres. Examinamos las asociaciones entre los factores de redes asociados y la realización de pruebas de VIH entre hombres en Dar es Salaam, Tanzania. La información proviene de una encuesta de línea basal de un ensayo de prevención del VIH con 48 redes, mayoritariamente masculinas. De los 923 hombres sexualmente activos que participaron, el 52 % habían realizado la prueba alguna vez. En un modelo de efectos aleatorios de regresión logística, los hombres dentro del núcleo de la red fueron 1.50 veces más probables (p < .05) de realizarse la prueba que aquellos en la periferia. El porcentaje de mujeres en la red estuvo asociado con una tasa mayor de realización de pruebas de VIH entre hombres (AOR 4.24, p < .05). La percepción del estigma por VIH en la red estaba negativamente relacionado con la realización de pruebas de VIH (AOR 0.92, p < .01). El pensar que al menos un amigo cercano obtuvo un resultado positivo en la prueba de VIH estaba asociado con un aumento en la cantidad de pruebas realizadas (AOR 2.66, p < .001). Las intervenciones con redes sociales tienen potencial para aumentar el uso de las pruebas de VIH entre hombres.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
To meet the UNAIDS 2020 target that 90 % of all HIV-positive people know their HIV status [1], men in sub-Saharan Africa need to be targeted for HIV testing [2]. Men in the region are consistently under-represented in HIV testing [3–5]. Men’s low uptake of testing in sub-Saharan Africa delays their entry into treatment and care, increases their risk for mortality, and heightens their potential to transmit HIV to their partners, thus effecting the HIV prevalence rates for both men and women [3, 6]. Nevertheless, a recent systematic review revealed that few HIV testing interventions in sub-Saharan Africa specifically target men [7].
There has been a call for research to understand factors that influence men’s engagement in HIV testing and treatment in sub-Saharan Africa [8]. Qualitative studies suggest that barriers to HIV testing for men include fear, stigma, perceptions that health care services are mostly for women, and norms associated with masculinity [2, 9–11]. Factors that facilitate HIV testing for men include, but are not limited to, fulfilling family obligations and their peers getting tested [9, 12].
According to a national survey in Tanzania in 2011–2012, an estimated 47 % of men aged 15–49 had ever tested for HIV [13]. A study based on 11 years of data from the HIV voluntary counseling and testing (VCT) clinic at the national hospital in Dar es Salaam found that only 35 % of men had previously had an HIV test and only 25 % knew their partner’s HIV status [4]. Previous research in Tanzania has shown that characteristics such as low education, low SES and young age have been negatively associated with HIV testing for men [4, 13].
Men’s HIV testing behavior may be shaped by the norms within their peer groups or networks [14]. Significant, positive associations have been consistently demonstrated between peer behaviors and other HIV risk behaviors among young men including inconsistent condom use [15–18], early sexual debut [19], and number of sexual partners [20], although all of these studies have been conducted outside of sub-Saharan Africa. Evidence from Tanzania indicates that young men’s HIV-related behaviors are shaped by their interactions with their peers [21–24]. Research suggests that more aggressive efforts are needed to change norms that underlie men’s HIV testing behavior in Tanzania [4].
Social network analysis is a tool for conceptualizing and quantifying social norms, network structure and composition, and these analyses can help researchers identify specific targets and pathways for interventions [25]. Studies have used network analysis to examine the relationship between social networks and HIV prevention behavior, such as condom use [15, 26]. A few studies have also examined the link between networks and HIV testing. In a study among male sex workers in China, having a small network or a network with few members who had tested for HIV was associated with an individual never having HIV tested [27]. In a study among Indian truck drivers and their apprentices, several network characteristics (having many friends, closeness among friends, and the importance of friends’ advice) were positively associated with the acceptance of rapid HIV testing [28].
Social network analysis remains underused for examining HIV-related behaviors in sub-Saharan Africa, despite the fact that network research may be important for addressing the magnitude of the epidemic in the region [29]. A recent study from Tanzania used network analysis [30] to examine network-level influence on young men’s engagement in concurrent sexual partnerships [24]. Network closeness, measured by the average number of friendships in each network, and normative concurrency behavior in the network (whether or not the majority of network members engaged in concurrency) were significantly associated with young men’s individual concurrency behavior [24]. These results suggest that network-level characteristics are an important source of influence on young men’s behavior in this context.
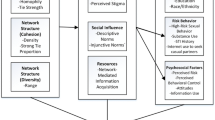
To generate hypotheses for the current study, we drew on theoretical and empirical evidence. The structural theory of social influence suggests that network structures may influence behaviors through flow of information [31]. Theory suggests that sociometric, or complete, networks can be divided into core, a sub-group in which actors are maximally connected, and periphery in which actors are loosely connected to the core [32]. Because those in the core are the most connected members of the network, they may receive the most information from other network members [33]. Therefore, they may be exposed to a wider range of views about the benefits of testing. Thus, we hypothesized that men in the network core would be more likely to have tested for HIV than men in the periphery.
We next considered network composition, or characteristics of the network members, which may influence behavior by shaping norms [25]. Women have higher rates of HIV testing and thus networks in which women are also members may make testing more normative in those networks. Therefore, we hypothesized that men who were members of networks with a greater proportion of women members would more likely have tested for HIV.
We also considered network norms for HIV stigma. Research from sub-Saharan Africa has demonstrated the relationship between social norms for HIV stigma and HIV testing for men [34–37]. A study in Nigeria showed that community-based social norms for HIV stigma were strongly and directly related to men’s, but not women’s, readiness to test for HIV [35]. In South Africa, positive attitudes towards people living with HIV/AIDS were associated with ever having tested [36]. Based on this prior literature, we hypothesized that social norms related to HIV stigma would be associated with HIV testing, such that those men who reported that their social networks held more stigmatizing norms would be less likely to have tested for HIV.
Finally, drawing on theory about social norms that suggests that network members are more likely to report making decisions about HIV risk behaviors that are in line with what they perceive is prevalent (descriptive norms) and appropriate (injunctive norms) [38], we hypothesized that the norms of men’s close friends in the network would be associated with men’s HIV testing behavior. Descriptive norms are thought to influence behavior by motivating individuals to behave in the way that they believe others are behaving and injunctive norms motivate individuals to behave in the way they perceive that others want them to behave [38]. Specifically, we hypothesized that men who thought at least one close friend had tested for HIV (descriptive norm) would be more likely to have tested than men who perceived none of their close friends had tested. Additionally, we hypothesized that men with at least one close friend who encouraged HIV testing (injunctive norm) would be more likely to have tested than men with close friends who did not encourage testing [15].
The purpose of this study was to examine how network structure, composition and norms are associated with HIV testing among men. Previous work showed that “camps”, stable social networks of mostly men, are an important source of friendship and influence for young men in Dar es Salaam [23, 24]. Camps are urban social networks of between 20 and 77 members and they have elected leaders [23]. Prior research demonstrated the stability of the camps; camps existed for an average of 8 years [23]. Most members reported being loyal to one camp, attending the camp regularly, and returning even after time away. Camps were formed by youth to have a common space within their neighborhood for socializing or engaging in activities like sports or music. A few camps moved to a different location or changed their names, but they usually remained within the same neighborhood [23]. Male members described the closeness they felt towards their fellow camp members, living “as one family in the camp”, supporting each other when they had problems, and helping each other find work and other opportunities. In addition, camp networks were diverse in their inclusion of women members; while some camps had few women members, other camps had several women members and included women in leadership positions [23]. We draw on baseline data using 48 randomized camp networks from an HIV and gender-based violence prevention intervention trial in Dar es Salaam [39].
Methods
Study Setting
Dar es Salaam is the commercial capital and largest city in Tanzania. The city has a population of 4.36 million, approximately 10 % of the total Tanzanian mainland population [40]. The HIV prevalence in Dar es Salaam is 6.9 % which is higher than the national average of 5 % [13]. The HIV prevalence among women in Dar es Salaam is 8.2 % and among men is 5.3 % [13].
Ethical Review
The study procedures and instruments were approved by the University of North Carolina at Chapel Hill Institutional Review Board as well as the Muhimbili University of Health and Allied Sciences (MUHAS) Senate Research and Publications Committee.
Study Procedures
We first enumerated all camps within four wards of Dar es Salaam. Using the PLACE (Priorities for Local AIDS Control Efforts) method [41], we identified 294 unique camps in operation and then screened them for eligibility (>20 members; <80 members; camp was in existence for at least 1 year; camp did not participate in our pilot study; camp was perceived as safe and no weapons previously used in a fight at the camp). Out of the 172 eligible camps, we randomly selected 60 for inclusion in our trial [39].
From each camp we obtained rosters of all current camp members. The roster data were collected from the camp leader. Rosters included the first name, last name, nickname, gender, birth date, and phone number of each camp member. We then contacted, confirmed eligibility and scheduled appointments with each eligible camp member. Camp members were eligible to participate if they were 15 years or older, were a camp member for more than 3 months, visited the camp at least once a week, planned on residing in Dar es Salaam for the next 30 months, and were willing to provide contact information for a friend or family member to be used in the event we could not contact the participant for future follow-up assessment. For these reasons, 112 individuals (5.7 %) were ineligible and 49 (2.5 %) refused to participate. We reached but were unable to schedule appointments with 197 participants (10.1 %) and were unable to contact 90 individuals after three attempts (4.6 %). A total of 1500 participants consented and completed the baseline behavioral assessment between October 2013 and March 2014. One camp (n = 9) was removed from the study because their leader falsified information with regards to the camp’s eligibility. The final sample was n = 1491 (1249 men and 242 women) within 59 camp networks. Our overall response rate among potentially eligible participants (n = 1836) was 81.2 %.
Research suggests that missing data from a significant number of network members will have a negative effect on the estimation of network properties, as strength of relationships is underestimated [42], centrality and degree measures become unstable [43], and network mapping becomes unreliable [44]. Following a recommended approach [45], we included in the analysis only those networks with >60 % response rates. Thus, we excluded 11 out of 59 networks. The non-response rate among the 48 remaining networks ranged from 0.0 to 36.4 %. Out of the 1540 individuals that were listed as members of the 48 camps, 269 did not complete the baseline survey and 54 were excluded from the analytic sample because they did not provide information on whether they had tested or some other key network variables. We also excluded 206 women from the analysis because this study was focused on men’s HIV testing. Women in the networks were included in the estimates of network properties, but not in the assessment of the outcome variable. We also excluded 115 men who never had sex because they represented a unique sub-group of men, with low rates of HIV testing, that was unlikely to have been motivated to test due to decreased risk for infection. 27 male members provided all baseline data, but no information on their social networks. Their network ties were imputed as described below. Therefore, the total number of male respondents included in the final sample of 48 networks was 923.
Survey Procedure
During the baseline assessment, we asked each member if he or she would be willing to spend up to 1 h to complete a structured survey with a study interviewer. Those members who were interested were asked to provide written informed consent to participate. After consent, camp members were interviewed in private study offices close to their camp. All participants were given 5000 Tanzanian shillings, as well as a referral card describing local health resources.
The baseline survey was implemented using tablets programmed with a custom-designed CAPI (computer-assisted personal interviewing) instrument. The baseline survey assessed demographic characteristics, age of sexual debut, and HIV risk behaviors, among other characteristics. The relevant measures are described in greater detail below.
Outcome Variable: HIV Testing
The outcome variable was dichotomous. Participants were asked “Have you ever had a test for HIV/AIDS?” Affirmative responses were coded with a one and negative responses were coded with a zero.
Demographic Characteristics
Participants were asked for their age in years and whether they were ever married. They were also asked how many children they had. A dichotomous variable was created to indicate whether or not the respondent had at least one child. Socioeconomic status (SES) was assessed using responses to a wealth index assessing ownership of 10 different household assets [46]. Principal components analysis was conducted on the assets index and then SES was categorized into terciles using the entire baseline sample of men and women.
Education
Respondents were asked “What is the highest level of school you have completed?” In order to assess whether increasingly higher levels of education were associated with greater odds of testing, we created three dummy-coded variables to indicate completion of three different education levels: “form three”; “form four”; and “above form four”, which were all compared to the same reference value of “form two or less”. We also created one dichotomous variable to indicate whether the respondent was currently a student.
Camp Average for Members’ Time Spent in Camp
We included a variable to represent, on average, how much time camp members spent in each camp, as an indication of the extent to which the camp was a meaningful socialization site for camp members. Each respondent was asked “How often would you say you come to your camp?” Response options endorsed included: every day, several times a week, and one time per week. Only 5 % of the sample endorsed coming one time per week, and the other respondents all came more often. To create a meaningful comparison we dichotomized responses to “every day” versus “once to several times per week”. We aggregated responses by camp to compute the average for each camp.
Social Network Assessment
The tablet was programed to display the camp roster for the participant’s particular camp. The camp rosters included the first name, last name, nickname, age and gender for every person in the camp. The interviewer read each name aloud and the participant was asked whether he/she knew that person. Next, the tablet was programed to display all the known camp members and the participant was asked whether each of the known camp members was a friend, acquaintance, or somebody he/she didn’t get along with.
Network Structure: Core
The “core” is a network sub-group in which actors are maximally connected. The actors who are not maximally connected form the “periphery” of the network [33]. We used UCINET for Windows [47] to fit a discrete core/periphery model for each camp network using only the friendship ties. UCINET finds a partition for each network graph such that the correlation between the data and the pattern matrix induced by the partition is maximized. UCINET uses a genetic algorithm for detecting the ideal core-periphery structure [33]. UCINET also generates a fit index, defined as the correlation between the observed data matrix and a hypothetical ideal core-periphery matrix for a network of the same size. The fit index can be interpreted as a correlation coefficient. The correlation coefficient was .94 for the camp networks, indicating that our data strongly conform to the core-periphery structure. Each respondent was given a value indicating whether he was in the core or not. Those who were in the core were given a value of one and those who were not in the core were given a value of zero. Figure 1 depicts one camp’s core-periphery structure.
Network Composition: Proportion of Women in the Camp
We included a continuous variable indicating proportion of women members in the camp.
Network Norm: HIV Stigma
Respondents’ perception of the network norm for HIV stigma was assessed by asking a series of questions about whether they perceived their fellow camp members as endorsing HIV stigma. We used items from a study on community level HIV stigma in Uganda [48]. In the Ugandan study, the items were internally consistent and demonstrated significant associations with HIV testing [48]. We included three items from this study and related them specifically to the respondent’s own camp: “In your camp, how many people think people with HIV have brought shame on their families?”; “In your camp, how many people would avoid visiting the homes of people with HIV?”; and “In your camp, how many people think that if you have HIV you have done wrong behaviors?”. For each question, the responses included “no one” with a value of one; “very few people” with a value of two; “some people” with a value of three; and “most people” with a value of four. Among the sample included in this analysis, the reliability of these items was α = .80. The items were summed and included as a total score in the analysis.
Descriptive and Injunctive Norms: Closest Friends
Each participant was asked to identify his two closest friends from the list of camp members he had identified as friends. If the participant did not have two or more friends in the camp, the tablet displayed both friends and acquaintances. Each participant was then asked a series of follow-up questions for the two closest friends. The follow-up question to assess descriptive norms was “Do you think friend X ever had an HIV test?” The question to assess injunctive norms was “Has friend X encouraged you to get an HIV test?” The response options included “yes”, “no”, or “declined to answer”. For those who declined to answer for either friend or both friends, we imputed a zero, conservatively assuming that the participant did not have a friend whom they thought had tested for HIV or that the participant did not have a friend who encouraged him to have an HIV test. A dichotomous variable was created for each type of norm indicating an affirmative response for at least one of the respondent’s two closest friends.
Network Imputation
We imputed outgoing ties from those network members who did not respond to the behavioral or network assessments. We used information on who nominated the non-respondents as friends because the non-respondents were included on the rosters. Following recommendations by Znidarsic et al. [45], imputation by reconstruction was used for networks in which reciprocity, or mutual friendship connections between network actors (range 0.0–1.0), among respondents was above 0.4 (14 camps). In the reconstruction procedure, all missing ties from non-respondents to respondents were replaced with the observed value of the tie in the opposite direction. Hence, whenever there was a tie from respondent i to non-respondent j, we imputed a tie from j to i. For ties between non-respondents, we used random imputation based on the observed density of the network. Mode imputation was used in networks where reciprocity was below 0.4 (34 camps) [45]. In this method, for each actor missing, ties were imputed based on the mean value of known incoming ties. Setting the threshold at 0.5, missing ties were imputed when an actor was chosen as a friend by at least half of the respondent actors.
Analysis
Descriptive statistics, including the mean, standard deviation, as well as the minimum and maximum for all variables were calculated to characterize the entire study sample. We conducted random effects logistic regression, accounting for the clustering of men within camp networks, to assess unadjusted and adjusted associations between our independent variables of interest, including camp-level variables, and HIV testing. The intraclass correlation (ICC) was computed using a method for binary outcomes (σ2 = π2/3) [49] and the significance of the group variance was used to assess the significance of the ICC [50]. We conducted a robustness check by running the models with and without imputed ties. All the effect sizes remained significant in both models. The effects for age and percentage of women in the camp were slightly attenuated and dropped one level of significance (one asterisk) in the model with imputation. The variables of having at least one child and HIV stigma increased one level of significance in the imputed model. Based on these limited differences, we present the results with imputed network ties. All analyses were conducted in Stata software Version 13.
Results
Among 923 men in the 48 camps included in the analysis (average age = 27), 51.5 % reported ever having tested for HIV (Table 1). Among the camps, the proportion of men who had tested ranged from 20.0 to 84.2 %. Camp network membership explained 4.08 % (ICC) of the total variance in HIV testing (τ00 = 0.14, p = .03). 76 % of the women in the 48 camps had ever tested for HIV (data not shown). Table 1 shows other characteristics of the men in the sample.
In Table 2 we present adjusted odds ratios (AORs) from the random effects logistic regression model predicting HIV testing and incorporating all imputed ties. We tested all possible interactions in the model and none were significant. Regarding demographic characteristics, age (AOR 1.03, 95 % CI 1.00–1.05) and having children (AOR 1.83, 95 % CI 1.21–2.78) were positively associated with ever testing, while ever having been married and currently being a student were not associated with testing. Those men who were categorized in the middle (AOR 1.61, 95 % CI 1.08–2.38) or highest level (AOR 1.54, 95 % CI 0.97–2.43) on the household asset index, compared to the lowest, were more likely to have tested. Having education level of form four (AOR 2.01, 95 % CI 1.39–2.89) or above form four (AOR 2.59, 95 % CI 1.40–4.80), compared to form 2 or less, was positively associated with testing. Regarding camp characteristics, the average for the amount of time members spent in the camp was not significantly associated with testing. In terms of camp network structure, men in the network core were 1.50 times (95 % CI 1.10–2.04) more likely than those who were in the periphery to have ever tested. In terms of camp network composition, the higher the proportion of women in the respondent’s camp network, the more likely a male respondent was to have ever tested for HIV (AOR 4.24, 95 % CI 1.39–12.98). Respondents’ perception of the network norm for HIV stigma was negatively associated with testing, such that higher levels of perceived HIV stigma in the network meant a lower likelihood for testing (AOR 0.92, 95 % CI 0.87–0.98). When both descriptive and injunctive norms were included in the model, only descriptive norms were significantly associated with HIV testing. Men who thought that at least one close friend in their network had ever tested were 2.66 times (95 % CI 1.76–4.00) more likely to have ever tested than those whose thought that neither of their two closest friends had tested. We also present illustrations of the results with network graphs in Fig. 2a and b.
Discussion
This is the first study to our knowledge that examines network structure, composition, and norms and their association with men’s HIV testing in sub-Saharan Africa. Men have low rates of HIV testing in the region and few interventions have specifically targeted these men for testing [3, 7]. Innovative strategies to promote men’s testing are needed in order to meet the UNAIDS 2020 goal that 90 % of those who are HIV positive should be diagnosed [1]. In this analysis, we examined 48 sociometric networks comprising 923 men in Dar es Salaam, Tanzania. Although 52 % of our sample reported ever having an HIV test, there was significant variation of HIV testing by network, with the proportion of men testing in each network ranging from 20.0 to 84.2 %. This variation warranted a closer look at network influence on HIV testing for men in this context. Building on prior studies that have shown the importance of men’s peers in their willingness to test for HIV [9, 12], we found that structural and compositional characteristics of men’s peer networks and norms within these networks were associated with HIV testing. Our results suggest that leveraging networks, their structure, and the norms they propagate, could increase rates of HIV testing for men.
We found that men in the network core were more likely to have tested for HIV than men in the network periphery. Core network members can serve as gatekeepers of information within these networks, allowing information to flow rapidly [51]. Therefore, it could be that men in the core of the camps learned more information about HIV testing, and were more likely to test. Theoretically, people at the network core can reach many people in the network quickly with information [25]. An intervention implication is that targeting core network members to spread messages about behavior change may result in rapid diffusion of those messages [51]. Thus, targeting core network members to promote HIV testing may be a useful intervention strategy for men.
In terms of network composition, we found that men who were members of networks with greater proportions of women were more likely to have tested for HIV. The effect of women in the networks may be because testing was more normative for women; 76 % of women included in the networks in this study had ever HIV tested. Camps with more women members may have experienced a more normative environment for HIV testing for all members of those camps. It is worth noting that this composition effect was significant above and beyond the descriptive norms of closest friends.
Like other studies, we found that men who perceived higher levels of HIV stigma in their networks were less likely to have HIV tested [35, 52]. This suggests that despite efforts to reduce HIV stigma in Tanzania, the negative influence of HIV stigma on testing persists [53]. Research from sub-Saharan Africa has shown that stigma is more associated with men’s HIV testing than women’s [35]. Interventions that target social networks have the potential to reduce stigma by changing harmful stigmatizing norms that may prevent the uptake of HIV prevention behaviors [51, 54]. Other researchers have shown that the process of having an HIV testing experience in and of itself is associated with a reduction in HIV stigma [55].
Our study showed that the descriptive norm for testing, measured by participants’ perceptions that at least one of their close friends had HIV tested, was strongly and positively associated with men’s HIV testing. When we included both the descriptive norm and the injunctive norm in our model, only the descriptive norm was significant, suggesting that the descriptive norm may be more strongly associated with HIV testing behavior. We note that our study focused on examining men’s perceptions of descriptive and injunctive norms. We know from theory that these perceptions may not match actual norms in that individuals tend to underestimate healthy behaviors in their peers [56]. In fact, other studies in this region have shown that to be true with regard to HIV testing [57]. However, our results highlight the importance of perceived norms and echo calls to correct perceptions when they are incorrect to maximize prevention efforts [57]. Furthermore, qualitative studies from sub-Saharan Africa show that men are more likely to test when they go with a friend or when a friend advises them to test [9, 12]. Thus, these findings collectively suggest that intervention efforts should promote communication about HIV testing among men and their closest friends in order to shift the descriptive norms about testing within these networks. Other research has similarly suggested that although men generally talk about HIV with friends in their networks, few men explicitly communicate with their friends about HIV testing [58]. Interventions that specifically target peer normative influence by engaging men within networks to talk about HIV testing are needed.
Limitations
Missing data are a problem in network analysis because of the dependent structure of networks and the need to have information from all network actors to constitute network variables [42, 45]. In our study, we excluded 11 out of 59 camps because they had more than 40 % missing respondents and thus assessment of their network characteristics would have been imprecise. At relatively low levels of non-response (<40 % missing), imputation methods perform better in estimating network variables than ignoring the non-respondents. We followed a current recommended approach by imputing missing network data for those camps that had >60 % response [45]. Future research, however, may develop more complex methods for dealing with network nonresponse [45].
Due to the cross-sectional nature of this study, we cannot assess the direction of the effects reported here. We don’t know whether camp membership preceded HIV testing. Although we know that most of these young men were members of their camps for an average of 6 years (Table 1), suggesting that they probably were camp members before they tested. Our cross-sectional study also limits our ability to evaluate recall bias regarding HIV testing. In the trial of which the data for this study come from, we plan to assess how network factors influence HIV testing over the course of the intervention. In addition, it is unlikely that men were in the network core because they had tested for HIV. Given that HIV testing is not yet normative among men in this context, it would be highly unlikely for a respondent to move from the periphery to the core because they had HIV tested. Furthermore, HIV testing may lead to lower levels of stigma, rather than vice versa. Longitudinal or intervention research is warranted to assess the causality of this relationship. Our study is also limited in that we only assessed the descriptive and injunctive HIV testing norms for men’s two closest friends. Therefore, we were not able to examine associations between HIV testing behavior and the social norms of men’s larger peer networks.
Finally, the networks we studied are not generalizable to networks of other young men in Tanzania. We cannot compare our results to networks of young men who are not camp members, or who do not live in impoverished urban areas like the ones in our study setting. Future studies of young men’s networks in sub-Saharan Africa will be useful for exploring these comparisons.
Conclusion
We showed that network structure, composition, and norms were associated with HIV testing behavior among urban Tanzanian men. Interventions that target social networks and core network members to diffuse behavior change, as well as change descriptive norms and norms related to stigma, may hold promise for increasing men’s HIV testing rates. Social network interventions have resulted in sustained changes for a number of health behaviors [59], including promotion of condom use [60, 61] and reduction of multiple partners [62]. Network interventions are likely to have greater reach and be more cost-effective than interventions aimed at individuals because they can disseminate health promotion messages more rapidly and to a wider target audience [51, 63, 64]. Reaching a large number of men quickly may be a worthwhile strategy in sub-Saharan Africa where many more men need to know their HIV status. Targeting naturally occurring networks, like the camps in this study, is a feasible and effective intervention approach because it facilitates access to men in settings where they regularly socialize [23, 65]. Future studies should assess whether network interventions can effectively scale up HIV testing for men in sub-Saharan Africa.
References
UNAIDS. 90-90-90 An ambitious treatment target to help end the AIDS epidemic. Geneva; 2014. http://www.unaids.org/en/resources/documents/2014/90-90-90.
World Health Organization. Consolidated guidelines on HIV testing services. 5Cs: Consent, confidentiality, counselling, correct results and connection. Geneva; 2015. http://www.who.int/hiv/pub/guidelines/hiv-testing-services/en/.
Mills EJ, Beyrer C, Birungi J, Dybul MR. Engaging men in prevention and care for HIV/AIDS in Africa. PLoS Med. 2012;9(2):e1001167.
Conserve D, Sevilla L, Mbwambo J, King G. Determinants of previous HIV testing and knowledge of partner’s HIV status among men attending a voluntary counseling and testing clinic in Dar es Salaam, Tanzania. Am J Mens Health. 2013;7(6):450–60.
Johannessen A. Are men the losers of the antiretroviral treatment scale-up? AIDS. 2011;25(9):1225–6.
Mills EJ, Bakanda C, Birungi J, Chan K, Hogg RS, Ford N, et al. Male gender predicts mortality in a large cohort of patients receiving antiretroviral therapy in Uganda. J Int AIDS Soc. 2011;14(1):52.
Hensen B, Taoka S, Lewis JJ, Weiss H, Hargreaves J. Systematic review of strategies to increase men’s HIV-testing in sub-Saharan Africa. AIDS. 2014;28(14):2133–45.
Shand T. Thomson-de Boor H, van den Berg W, Peacock D, Pascoe L. The HIV blind spot: men and HIV testing, treatment and care in sub-Saharan Africa. IDS Bull. 2014;1(1):53–60.
Siu GE, Wight D, Seeley JA. Masculinity, social context and HIV testing: an ethnographic study of men in Busia district, rural eastern Uganda. BMC Public Health. 2014;14(1):33.
Skovdal M, Campbell C, Madanhire C, Mupambireyi Z, Nyamukapa C, Gregson S. Masculinity as a barrier to men’s use of HIV services in Zimbabwe. Glob Health. 2011;7(1):13.
Izugbara CO, Undie C-C, Mudege NN, Ezeh AC. Male youth and voluntary counseling and HIV testing: the case of Malawi and Uganda. Sex Educ. 2009;9(3):243–59.
Denison J, McCauley P, Dunnett-Dagg W, Lungu N, Sweat MD. The HIV testing experiences of adolescents in Ndola, Zambia: do families and friends matter? AIDS Care. 2008;20(1):101–5.
Tanzania Commission for AIDS (TACAIDS), Zanzibar AIDS Commission (ZAC), National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), ICF International (ICF). Tanzania HIV/AIDS and Malaria Indicator Survey 2011–12. Dar es Salaam, Tanzania; 2013.
Agadjanian V. Men’s talk about “women’s matters”: gender, communication, and contraception in urban Mozambique. Gend Soc. 2002;16(2):194–215.
Barrington C, Latkin C, Sweat MD, Moreno L, Ellen J, Kerrigan D. Talking the talk, walking the walk: social network norms, communication patterns, and condom use among the male partners of female sex workers in La Romana, Dominican Republic. Soc Sci Med. 2009;68(11):2037–44.
Blum RW. Youth in sub-Saharan Africa. J Adolesc Health. 2007;41(3):230–8.
Rai A, Stanton B, Wu Y, Li X, Galbraith J, Cottrell L, et al. Relative influences of perceived parental monitoring and perceived peer involvement on adolescent risk behaviors: an analysis of six cross-sectional data sets. J Adolesc Health. 2003;33(2):108–18.
Romer D, Black M, Ricardo I, Feigelman S, Kaljee L, Galbraith J, et al. Social influences on the sexual behavior of youth at risk for HIV exposure. Am J Public Health. 1994;84(6):977–85.
Maxwell KA. Friends: the role of peer influence across adolescent risk behaviors. J Youth Adolesc. 2002;31(4):267–77.
Ali MM, Dwyer DS. Estimating peer effects in sexual behavior among adolescents. J Adolesc. 2011;34(1):183–90.
Dilger H. No sexuality, AIDS, and the lures of modernity: reflexivity and morality among young people in rural Tanzania. Med Anthropol Q. 2003;22(1):23–52.
Setel P. AIDS as a paradox of manhood and development in Kilimanjaro, Tanzania. Soc Sci Med. 1996;43(8):1169–78.
Yamanis TJ, Maman S, Mbwambo JK, Earp JAE, Kajula LJ. Social venues that protect against and promote HIV risk for young men in Dar es Salaam, Tanzania. Soc Sci Med. 2010;71(9):1601–9.
Yamanis TJ, Fisher JC, Moody JW, Kajula LJ. Young men’s social network characteristics and associations with sexual partnership concurrency in Tanzania. AIDS Behav. 2016;20(6):1244–55.
Valente TW. Social networks and health: models, methods, and applications. Oxford: Oxford University Press; 2010.
Latkin C, Forman V, Knowlton A, Sherman S. Norms, social networks, and HIV-related risk behaviors among urban disadvantaged drug users. Soc Sci Med. 2003;56(3):465–76.
Huang ZJ, He N, Nehl EJ, Zheng T, Smith BD, Zhang J, et al. Social network and other correlates of HIV testing: findings from male sex workers and other MSM in Shanghai, China. AIDS Behav. 2012;16(4):858–71.
Schneider J, Kumar R, Dandona R, Kumar P, Kumar A, Lakshmi V, et al. Social network and risk-taking behavior most associated with rapid HIV testing, circumcision, and preexposure prophylaxis acceptability among high-risk Indian men. AIDS Patient Care STDs. 2012;26(10):631–40.
Perkins JM, Subramanian SV, Christakis N. Social networks and health: a systematic review of sociocentric network studies in low- and middle-income countries. Soc Sci Med. 2015;125:60–78.
Wasserman S, Faust K. Social network analysis: methods and applications. New York: Cambridge University Press; 1994.
Friedkin NE. A structural theory of social influence. Cambridge: Cambridge University Press; 2006.
White HC, Boorman SA, Breiger RL. Social structure from multiple networks I: blockmodels of roles and positions. Am J Sociol. 1976;81:730–81.
Borgatti SP, Everett MG. Models of core/periphery structures. Soc Netw. 1999;21:375–95.
Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape Town, South Africa. Sex Transm Infect. 2003;79:442–8.
Babalola S. Readiness for HIV testing among young people in northern Nigeria: the roles of social norm and perceived stigma. AIDS Behav. 2007;11(5):759–69.
Young SD, Hlavka Z, Modiba P, Gray G, Van Rooyen H, Richter L, et al. HIV-related stigma, social norms, and HIV testing in Soweto and Vulindlela, South Africa: National Institutes of Mental Health Project Accept (HPTN 043). J Acquir Immune Defic Syndr. 2010;55(5):620–4.
Pyne JM, Kuc EJ, Schroeder PJ, Fortney JC, Edlund M, Sullivan G. Relationship between perceived stigma and depression severity. J Nerv Ment Dis. 2004;192(4):278–83.
Cialdini R, Reno R, Kallgren C. A focus theory of normative conduct: recycling the concept of norms to reduce littering in public places. J Pers Soc Psychol. 1990;58:1015–26.
Kajula L, Balvanz P, Kilonzo MN, Mwikoko G, Yamanis T, Mulawa M, et al. Vijana Vijiweni II : a cluster-randomized trial to evaluate the efficacy of a microfinance and peer health leadership intervention for HIV and intimate partner violence prevention among social networks of young men in Dar es Salaam. BMC Public Health. 2016;16(113):1–12.
Tanzania National Bureau of Statistics (NBS). The United Republic of Tanzania 2012 Population and Housing Census: Population Distribution by Administrative Areas. Dar es Salaam; 2013.
Weir SS, Morroni C, Coetzee N, Spencer J, Boerma JT. A pilot study of a rapid assessment method to identify places for AIDS prevention in Cape Town, South Africa. Sex Transm Infect. 2002;78(Suppl 1):i106–13.
Burt RS. A note on missing network data in the general social survey. Soc Netw. 1987;9:63–73.
Kossinets G. Effects of missing data in social networks. Soc Netw. 2006;28:247–68.
Borgatti SP, Molina JL. Ethical and strategic issues in organizational social network analysis. J Appl Behav Sci. 2003;39:337–49.
Znidarsic A, Doreian P, Ferligoj A. Non-response in social networks: the impact of different non-response treatments on the stability of blockmodels. Soc Netw. 2012;34(4):438–50.
Filmer D, Pritchett L. Estimating wealth effects withoutexpenditure data—or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–32.
Borgatti SP, Everett MG, Freeman L. Ucinet for Windows: Software for Social Network Analysis. 2002.
Singer S, Steward W, Ekstrand M, Milagro-Fotre S, Walusimbi M, Havlir D, et al. Differences and similarities between perceived community HIV stigma and TB stigma among TB evaluation patients offered same-day HIV counseling and testing. In: International AIDS Conference 2008 (AIDS 2008), Mexico City; 2008. http://caps.ucsf.edu/uploads/pubs/presentations/pdf/charlebois_VCT_ias08.pdf.
Ridout MS, Demétrio CGB, Firth D. Estimating intraclass correlation for binary data. Biometrics. 1999;55(1):137–48.
Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. Thousand Oaks: SAGE Publications; 2002.
Valente TW. Network interventions. Science. 2012;337(6090):49–53.
Pettifor A, MacPhail C, Suchindran S, Delany-Moretlwe S. Factors associated with HIV testing among public sector clinic attendees in Johannesburg, South Africa. AIDS Behav. 2010;14(4):913–21.
United Republic of Tanzania. Third National Multi-sectoral Strategic Framework for HIV and AIDS (2013/14- 2017/18). Dar es Salaam; 2013. http://www.tacaids.go.tz/index.php?option=com_content&view=article&id=44:nmsf&catid=25:strategic-documents&Itemid=140.
Latkin C, Knowlton A. Micro-social structural approaches to HIV prevention: a social ecological perspective. AIDS Care. 2005;17(Suppl 1):S102–13.
Jürgensen M, Sandøy IF, Michelo C, Fylkesnes K. Effects of home-based Voluntary Counselling and Testing on HIV-related stigma: findings from a cluster-randomized trial in Zambia. Soc Sci Med. 2013;81:18–25.
Prentice D, Miller D. Pluralistic ignorance and the perpetuation of social norms by unwitting actors. In: Mark P, editor. Advances in experimental social psychology. 28th ed. Cambridge: Academic Press; 1996. p. 161–209.
Mulawa M, Yamanis TJ, Balvanz P, Kajula LJ, Maman S. Comparing perceptions with actual reports of close friend’s HIV testing behavior among urban Tanzanian men. AIDS Behav. 2016. doi:10.1007/s10461-016-1335-8.
Tobin KE, Yang C, Sun C, Spikes P, Latkin CA. Discrepancies between HIV prevention communication attitudes and actual conversations about HIV testing within social and sexual networks of African American men who have sex with men. Sex Transm Dis. 2014;41(4):221–6.
Webel AR, Okonsky J, Trompeta J, Holzemer WL. A systematic review of the effectiveness of peer-based interventions on health-related behaviors in adults. Am J Public Health. 2010;100(2):247–53.
Basu I, Jana S, Rotheram-Borus MJ, Swendeman D, Lee S-J, Newman P, et al. HIV prevention among sex workers in India. J Acquir Immune Defic Syndr. 2004;36:845–52.
Kelly JA, Amirkhanian YA, Kabakchieva E, Vassileva S, Mcauliffe TL, Difranceisco WJ, et al. Prevention of HIV and sexually transmitted diseases in high risk social networks of young Roma (Gypsy) men in Bulgaria: a randomised controlled trial. Br Med J. 2006;333(7578):1098–101.
Agha S, Van Rossem R. Impact of a school-based peer sexual health intervention on normative beliefs, risk perceptions, and sexual behavior of Zambian adolescents. J Adolesc Health. 2004;34(5):441–52.
Valente TW, Pumpuang P. Identifying opinion leaders to promote behavior change. Health Educ Behav. 2007;34(6):881–96.
Heckathorn DD, Broadhead RS, Anthony DL, Weakliem DL. AIDS and social networks: HIV prevention through network mobilization. Sociol Focus. 1999;32(2):159–79.
Latkin C, Davey-Rothwell M, Knowlton AR, Alexander K, Williams CT, Boodram B. Social network approaches to recruitment, HIV prevention, medical care, and medication adherence. J Acquir Immune Defic Syndr. 2013;1(63 Suppl 1):S54–8.
Acknowledgments
We wish to acknowledge the work and dedication of our research team in Chapel Hill and Dar es Salaam including Peter Balvanz, Lauren Hill, Mrema Noel Kilonzo, Deus Kajuna, Brenda Mkony, Joyce Kondela and Gema Lambert. We would like to thank the participants of our study for their time and cooperation.
Funding
Research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health under Award Numbers R01MH098690 (awarded to S. Maman) and F31MH103062 (awarded to M. Mulawa), and T32AI007001, a training grant from the National Institute of Allergy and Infectious Diseases (awarded to D. Conserve). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Yamanis, T.J., Dervisevic, E., Mulawa, M. et al. Social Network Influence on HIV Testing Among Urban Men in Tanzania. AIDS Behav 21, 1171–1182 (2017). https://doi.org/10.1007/s10461-016-1513-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1513-8