Abstract
Health professionals’ roles and scopes often overlap, creating a need for role clarity in interprofessional teamwork. Yet, such clarity does not mean roles are fixed within teams and some literature suggests role flexibility can enhance team functioning. Interprofessional practice competencies and learning activities often emphasize knowledge and definition of roles, but rarely attend to the dynamic nature of roles and influential contextual factors. This study explores role fluidity in interprofessional student groups using an activity theory framework. Using a collective instrumental case study approach, the authors examine the fluidity of one physical therapy (PT) student’s role within 3 different interprofessional (medical, pharmacy, PT) student groups completing nursing home patient care plans. Field notes, group debriefing interviews, and care plans were collected and coded from all care planning sessions. Codes mapped to group-specific activity systems that compared role-influencing interactions and tensions. The PT student’s role fluidity varied in each group’s activity system, influenced primarily by system tensions from implicit rules (e.g., encouraging questions), division of labor (e.g., rigid profession-based task assignment), and tool use (e.g., computers). Attention to modifiable system elements, such as tool use and explicit rules of inclusivity, could foster role fluidity and improve interprofessional teamwork and learning environments.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Knowing your role on a team and fulfilling that role competently are key to patient safety, efficiency, and effective team dynamics (Brown et al. 2000; Suter et al. 2009). The interprofessional education (IPE) competencies reflect this premise as they include “understanding professional roles and responsibilities” as a core competency (Interprofessional Education Collaborative 2016). Didactics, simulation exercises, and small group activities used in IPE provide opportunities for students to learn designated roles of their own profession as well as of others (Furr et al. 2020; Gilbert et al. 2010; Hudson et al. 2017; O’Brien et al. 2017; O’Neill and Wyness 2005). Role-focused learning activities, though, often present narrowly defined professional roles (Bridges et al. 2011; Gunaldo et al. 2015).
Some consider interprofessional (IP) ‘role blurring’ detrimental as it departs from one of the core attributes of high-functioning IP professional teams: role clarity. Without clear role boundaries, disorder, miscommunication, and lack of ownership may disrupt the team’s success (Bittner 2018; Brown et al. 2000; Suter et al. 2009). While such concerns have merit, literature on teamwork recognizes “backup behaviors” as a key feature of high-functioning teams (Salas et al. 2005). Observational studies have also recognized the need for more fluid conceptualizations of roles based on team and patient needs rather than professional disciplinary boundaries (Lingard et al. 2012).
Being ‘fluid’ within a team means temporarily reaching beyond one’s professional role, depending on circumstances, without causing chaotic uncertainty of one’s responsibility; this differs from ‘role blurring,’ which suggests the hazy overlapping of roles without a clear sense of task assignment. Lingard and colleagues have suggested that when team members stop at merely understanding their roles and become so aligned with their perception of ‘role,’ they struggle to work outside the box to meet the demands of patient care (Lingard et al. 2012, 2017). Real-world patient-care roles are complex and this complexity is a part of everyday practice. Teams utilizing ‘role fluidity,’ or dynamic professional boundaries, can have improved efficiency and collaboration between team members, which could lead to improved patient care (Galvin et al. 2014; Harrod et al. 2016; MacNaughton et al. 2013).
IPE activities focusing solely on role clarity and demarcation miss the opportunity to teach role fluidity. In a fluid role, a student retains a core professional identity and expertise but can also transcend and ‘flow’ into another role when it would best serve the patient’s, team’s, or his or her own personal needs (Ambrose-Miller and Ashcroft 2016). Engaging students from multiple health professions in real patient care activities offers meaningful, though sometimes unpredictable, opportunities to approach role challenges as a team. Often these challenges involve issues related to power and role dynamics (Bleakley et al. 2011; Giuliante et al. 2018; Paradis and Whitehead 2018). Students’ adherence to narrowly defined professional roles can lead to dysfunction in the learning environment, as demonstrated in a study of advanced students working in outpatient IP teams. Students in these teams either incorporated or ignored the interests of colleagues and patients depending on how rigidly they conceptualized their role. Team tensions grew when students focused their attention on their professional expertise rather than the tasks and roles necessary for patient care (Kent et al. 2016). These findings suggest an opportunity to address both role clarity and role fluidity in IP learning activities. Foundational IPE competencies related to defining roles and role clarity might benefit from a concurrent introduction to role fluidity that exposes students to situations where boundary setting might impede team function. While the literature frequently discusses role clarity and professional roles in IPE, there is an underrepresentation in the literature on role fluidity within IPE activities.
To assist educators with how to incorporate role fluidity, we first need a better understanding of what role fluidity looks like and how it is influenced in IP learning activities. Our study aims to provide such understanding of role fluidity’s barriers and facilitators in a real-world IP education environment through an in-depth analysis of one student’s role in three IP groups participating in the same clinically-based IPE activity. We used activity theory to guide our analysis.
Conceptual framework
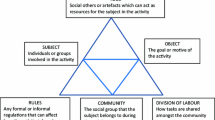
Activity theory (AT) provides a framework that can guide analysis of complex systems such as interprofessional student teams by providing a sociomaterial analytic lens through which to view interactions among individuals, rules, tools, and tasks as IP learning ‘activity systems’ (Barrow et al. 2015; Hean et al. 2018; O’Keefe and Ward 2018). AT also attends to the social and cultural context of the activity system (Barrow et al. 2015; Battista 2015; Engeström 2001; Johnston and Dornan 2015). In second generation AT, an activity system illustrates the relationships and interactions between an environment’s seven primary elements: subject (individual or group of individuals of focus), object (subject’s task or goal), tools (non-human objects or artifacts), rules (explicit or implicit), community (social group), division of labor (task division within the social group), and outcomes (result/consequence of an activity) (Fig. 1) (Engeström 2001, 2015; Yamagata-Lynch 2010, Chapter 1; Yamagata-Lynch and Smaldino 2007). Tensions, or ‘internal contradictions’, among elements of the systems are considered possible instigators of change and learning within the system. Tensions are not inherently negative; rather, they disrupt the system in ways that can alter other elements in the system and/or outcome in positive or negative ways (Engeström 2001; Yamagata-Lynch and Haudenschild 2009). Tensions are a crucial piece in understanding how a system changes.
Example of second generation activity system with system elements defined as they relate to this study. (Engeström 2001, reprinted and adapted with permission from Taylor & Francis Ltd). Key: Straight intersecting lines represent interaction between elements not leading to system tension. Squiggly line between elements represents system tension (note: squiggly line in above figure is an example, not representative of study results). *Real student’s name has been changed. #Role fluidity is defined as dynamic professional boundaries expressed as operating within or outside of professional scope
AT-based exploration of healthcare team dynamics, especially those of IP teams, can illuminate how students from different professions learn and work together (Bleakley 2006; Bleakley et al. 2011; Lingard et al. 2012; Varpio et al. 2008). Analysis of an activity system can focus on specific team factors and types of interactions, such as students and their team rules, while also offering novel relationship and tension-focused insights to enhance understanding of team goal (object) attainment (Kent et al. 2016; McMurty et al. 2016).
While prior IPE work has used the AT framework to study groups of students in authentic clinical scenarios, no study based around AT has illuminated students’ development of role fluidity in IP practice environments. Better understanding of role fluidity’s enablers and barriers could help IPE educators facilitate students’ progression to a more fluid role in clinical practice.
Methods
Design
To gain insight into the complexities of role dynamics in the context of clinically-based IPE, we chose a longitudinal design that allowed us to follow one student through three different activity systems. The student participated in similar IPE activities, but in three different groups of students caring for different patients. We treated each group, or activity system, as a case and thus consider, using Stake’s model, this a collective instrumental case study design that explores the phenomenon of role fluidity developing in three systems through the lens of a subject interacting within those separate systems (Cheek et al. 2017; Stake 1995; Thomas and Myers 2018). Combining AT with case study design supports intensive and contextual examination of elements within an activity system (e.g., material objects used by students, products created through engagement) their interplay, and the tension among such elements (Yamagata-Lynch 2010).
Researchers apply AT by focusing on the activity system, or case, as a unit of analysis. Breaking down the activity into its raw elements and examining element interactions and tensions helps explain the system’s outcome and functionality. Second-generation activity systems are traditionally represented in a triangular fashion with intersecting lines corresponding to the interactions and/or tensions between two key system elements (Fig. 1) (Engeström 2001). Activity system diagrams provide visual representations and relationships of system elements.
Participants and setting
Fourth-year medical students (MD), fourth-year pharmacy students (PH), and second/third year physical therapy students (PT) participated in an elective IP geriatrics rotation based at the San Francisco Veteran’s Administration (VA) Medical Center’s nursing home during the 2016–2017 academic year. The activity system subject, Jennifer*, was a PT student who participated in the geriatrics rotation with three consecutive student groups (labeled Group 1, 2, and 3 below) during her 12-week VA nursing home rotation between January and March 2017. MD and PH students changed for each group. Jennifer offered a unique opportunity for serial observation as the only student to participate in three student groups; as a result, we selected her as the subject of the study. Jennifer’s continuity through three groups provided a constancy that allowed for observation of how her role changed due to activity system factors while she herself did not change. Had groups consisted of completely different student teams, there would be no constancy from which to observe role fluidity. Throughout the paper, the term “group” refers to the trio of students participating on a rotation together; the term “activity system” refers to the learning group as well as its environment which includes Jennifer (subject), her group peers (community), the patient’s care plan constructed by the group (object), and group rules, tools, and division of labor. For this study, the term “outcome” is defined as the expression or lack of expression of role fluidity by Jennifer as she and the group completed the task of creating a care plan (object) (Fig. 1). As the activity system was designed for students to create a care plan, and as a product or result of that construction the researchers observed either the expression or lack of expression of role fluidity, the researchers see role fluidity as a consequence of the activity system’s completion of its object and thus as the “outcome.”
MD, PH, and PT students worked together for 2 weeks and participated in activities such as patient fall evaluations, medication regimen reviews, and functional assessments. Our study focuses on students’ performance of comprehensive patient care assessments of nursing home patients. Groups were instructed to meet and evaluate the patient, synthesize and draft an assessment and care plan based on their collective knowledge and skillsets, and present that care plan to the patient’s nursing home providers. We provided them with minimal instructions in how to construct a care plan and allowed them to determine the plan’s structure, as well as what problems and recommendations to include. Groups had 4–8 h to complete these activities; they had a workroom equipped with computers, whiteboards, and office supplies. Groups were expected to complete two comprehensive patient evaluations, but one group only completed one evaluation due to students’ schedule conflicts.
Ethical considerations
The UCSF and San Francisco VA Medical Center Institutional Review Boards approved this study as exempt. Students provided verbal consent to participate after reviewing an information sheet describing the study.
Data collection
During patient care planning sessions, the principal researcher (LKB) directly observed and audio-recorded groups as they reviewed patient charts and created care plans. LKB is a practicing geriatrician and health professions education researcher working within the nursing home. LKB observed from the corner of the students’ workroom, documenting observable interactions among students and between students and tools in field notes. LKB transcribed the audio-recordings and combined them with the field notes to create a synthesized text of the students’ actions and interactions between system elements.
Additionally, LKB conducted and audio-recorded a group debrief after each group’s care planning activities. She asked semi-structured interview questions to probe for difficult-to-observe elements of the activity system, such as the rules each group established, sense of community, how the group divided tasks (division of labor), and how the students would have approached the exercise if they had worked individually rather than as a group. Debriefing interviews were transcribed by a transcription service (Rev.com) then de-identified by LKB.
Groups submitted their patient care plans to LKB, who then de-identified them and worked with the nursing home’s primary PH and PT preceptors to review for content.
Data analysis
Guided by a methodological process described by Yamagata-Lynch, LKB used the AT framework to code all raw field notes and group interview transcripts in Dedoose (Version 8.0.31, SocioCultural Research Consultants, LLC, Manhattan Beach, CA), a qualitative analysis software program. BO’B then reviewed the coded data to compare interpretations. LKB and BO’B met weekly to discuss the evolving findings and interpretations. LKB then used an iterative process to construct narrative descriptions and diagrams of activity systems (Yamagata-Lynch 2010, Chapter 6)(Fig. 2). As LKB constructed narratives and activity systems, she focused on examples that demonstrated how students took on a role within or outside of professional scope (e.g., how ‘fluid’ their role appeared) throughout patient care planning. The narratives and activity system diagrams allowed us to identity elements, relationships, and tensions in each group’s activity system that influenced Jennifer’s role fluidity (the outcome of interest).
Study activity system analysis process. This sequence was completed for all 3 groups, concurrently. Light gray components are part of traditional activity system analysis (narratives, activity system diagrams); dark gray component represents an additional source of data (reviewed care plans) that was incorporated into the final activity system
Concurrently, LKB and the two additional nursing home rotation preceptors representing pharmacy and physical therapy reviewed student group care plans for components that preceptors deemed applicable for all nursing home patients regardless of medical history: functional assessment, medication review, and psychosocial assessment. Preceptors discussed care plans and noted where components were adequately addressed or missing from care plans. Completeness of care plans was incorporated into the activity system as part of the object (Table 1).
Reflexivity
The primary researcher (LKB) was a non-participant observer. She is a geriatrician familiar with the nursing home and students’ patients and thus an insider to the clinical care environment. LKB’s insider knowledge allowed her to easily follow content discussed by the students and informed her interpretation of students’ interactions and plans. When LKB interacted with the students outside of her non-participant observer role, conversations focused on patient care not the activity system or team roles. She had no role in grading students that might affect her ability to remain impartial in her observations. She regularly discussed her interpretations with other team members (LCF and MY) who also worked with students in the rotation, and BO’B (who did not work with the students), to ensure other perspectives were considered and represented in the findings and that her roles as clinician and observer did not affect her interpretations. BO’B had no contact with the students, patients, or clinical environment and thus provided the secondary coding and critical review of data analysis and interpretations.
Results
We observed the care planning sessions of the three consecutive student groups in which Jennifer participated. Table 1 consolidates the elements of each group’s activity system, noting similarities and differences; Fig. 3 shows the elements of the care planning activity included in each group’s activity system diagram; Figs. 4, 5 and 6 delineate interactions and tensions present in each activity system. Below, we describe differences among the three, chronological groups’ activity systems and their impact on Jennifer’s role fluidity.
Group 1 activity system
Group 1’s activity system (Fig. 4) shows how tools, rules, community, and division of labor within the group led to both an integrated group care plan (object) as well as an expansion of Jennifer’s role within the system during the care planning activity (outcome). Her role characterization capitalized on system tensions, pushing her beyond her primary PT expertise-driven role into new role territory (e.g., consideration of medical decision-making and pharmacological treatment) while she still maintained her PT expertise.
Group 1: tools and division of labor
Group 1’s use of tools, such as computers and the electronic chart (Table 1), to construct the care plan created opportunities for both role fulfillment as well as role fluidity. While students worked initially within their profession-based division of labor (e.g., MD1 focusing on medical decision making, PH1 reviewing patient medication list, Jennifer providing functional assessment), composing the patient care plan together broadened roles beyond these traditional divisions of labor and encouraged Jennifer’s role fluidity.
A group 1 tension developed when Jennifer added ‘scribing’ tasks to her PT role. Jennifer used the scribe role to query and request clarification from her peers about the entire care plans as she composed the note. Her questions prompted care plan changes related to tasks outside of her traditional division of labor. For example, when MD1 and PH1 discussed a patient’s angina, Jennifer reviewed the care plan and identified a point for clarification:
- PT:
-
(pauses while scribing) “So you know how we said [in the plan] that the angina was “well-managed”… can we actually say that since it’s getting worse? The chest pain is managed [overall] but the angina seems to be getting worse…
(group decides to write “Chest pain occurring with increase in frequency” and they make appropriate recommendations) [Group 1 Week 1 Field Notes]
Though defining the angina’s instability might not be within PT’s traditional scope of responsibilities, Jennifer’s scribing with the computer and note template (tools) afforded her the opportunity to actively synthesize the group’s recommendations and broaden her role to include assisting in medical management of a patient’s chest pain.
Group 1: community and rules
Group 1’s community and rules allowed Jennifer to expand beyond traditional PT role boundaries (Table 1). Jennifer asked questions, integrated knowledge, and explored new ideas as the community’s implicit ‘rules of inclusivity’ fostered such actions. Her reflections on this implicit rule connect it to the broadening of her role in the care planning session.
- PT:
-
You can get out of your box when you’re not dealing with your own role. I think that was probably the best part of it–being like, “Well, is that [medical problem] important?” That was cool. [Group 1 Week 1 Debrief]
In Group 1, inclusivity appeared to be more important than efficiency. For example, when Jennifer delved into a patient’s incontinence, she pushed the community to get at ‘why’ he might be incontinent, including for functional mobility reasons. Her colleagues encouraged her line of reasoning even though it slowed the care plan construction:
- PT:
-
He’s…inconsistently incontinent…it’s almost like…he doesn’t want to wear the briefs but then he’s…
- MD1:
-
Right, right! (nodding)
- PT:
-
I’m just thinking if it’s because he’s not getting [help] to the bathroom quick enough? …should we educate him about asking for help when he needs [to urinate]?
- PH1:
-
That’s a good idea!
- PT:
-
(scribes in Word Document about incontinence, pauses, looks up) Is it really incontinence though? (more discussion) [Group 1 Week 1 Field Notes]
Group 1 members engaged Jennifer in medical problem planning, which broadened discussion of patient problems. Working within a community in which rules encouraged inclusivity and inquiry gave Jennifer the time and space to entertain a more fluid role related to medical decision making.
Overall group 1 impact on student role fluidity
In group 1, Jennifer’s role expanded into territory beyond the usual focus of PT’s work (e.g., medical problem solving), fueled by the collaborative use of, and Jennifer’s central position with, the care planning tools as well as the community’s encouragement of her inquisitiveness. When asked to consider patient care issues beyond function and mobility, Jennifer exhibited interest in a fluid role as it related to a specific patient. Her comments in the group debrief suggest ways in which group 1’s activity system both embodied IP competencies regarding roles and promoted role fluidity.
- PT:
-
It was really helpful to have different disciplines involved … it just kind of cleared up the picture of the patient, I think, and gave me a deeper understanding of what [the patient] was going through and how my role could change based on how [the other students] explained their specific roles, which I thought was really helpful. [Group 1 Week 1 Debrief]
Group 2 activity system
Group 2, occurring two weeks after group 1, had noticeably different elements within its activity system (Table 1), including overall lower care plan scores, and a different outcome for Jennifer’s role fluidity. Notably, system tensions contributed to reducing Jennifer’s scope and flexibility in roles (Fig. 5).
Group 2: tools, rules, and community
Group 2 had the same tools at their disposal as group 1 (e.g., computers, charts) but divided its tool use and created implicit and explicit rules that supported efficiency, resulting in a task-driven tone within the community (Table 1). MD2 and PH2 worked together on one note and computer while Jennifer worked independently on a second. Tools caused physical separation within the community and seemed to contribute to the rule of prioritizing efficiency:
- LKB:
-
So how did you feel about two different screens going…how did that feel as a team?
- PH2:
-
For me, I felt like it was more efficient. Just because we’re focused on different things…I thought it was efficient
- MD2:
-
I agree. I think what would actually be more efficient would be to have three computers. [Group 2 Week 1 Debrief]
The use of separate tools (computers) allowed group 2 to complete care plans quickly and efficiently (50–60 min vs 70–120 min in groups 1 and 3), but also led to clear divisions between community members. Creating two distinct care plans on two computers, while merged at the end of the session, reduced the community’s opportunities for teaching and learning. Without the opportunity to participate in care plan construction, ask for clarification about medical problems, and work within an open and collaborative space, Jennifer was isolated from the rest of the community. Tools physically separated her from the rest of the community and group rules contracted her role in other aspects of medical care planning.
Group 2: tools and division of labor
Separate tool use created system tensions by causing profession-based divisions of labor not present in group 1 (Table 1). These tensions led to Jennifer completing functional assessments alone on her computer and MD2 completing, by MD2’s account, “everything else”:
- MD2:
-
I basically wrote the subjective portion regarding the symptoms… And then Jennifer wrote the last paragraph which was [the patient’s] functional status… And then for assessment and plan, Jennifer wrote…the functional bullet point, and I think I wrote everything else
- LKB:
-
Would you do it differently in retrospect at all?
- MD2:
-
No [Group 2 Week 1 Debrief]
Jennifer subsequently commented in the debriefing session about focusing on her role as a PT while writing the note:
- PT:
-
I think because it felt more individualized this time, I was focused very strongly on his functional mobility and how he was doing in that sense. [Group 2 Week 2 Debrief]
Group 2: rules and division of labor
Group 2 brings out system tensions between rules and division of labor, which impacted students’ expansion of their roles (Table 1). Rules of efficiency and professional, task-based focus kept community members focused on profession-based division of labor. Jennifer tackled tasks related to her professional role, reserving for herself PT items on which she would work:
- PT:
-
Here’s some things I’ll want to look at. Bed mobility, and then just put transfers there in the note, and gait
- MD2:
-
(adds these things to skeleton note, silently goes back to reviewing patient labs) [Group 2 Week 1 Field Notes]
Group 2’s aversion to overlap or redundancy in tasks caused system tensions whenever a group member tried to contribute to a problem that was out of his or her professional scope. When Jennifer included something in the note that MD2 did not consider part of her professional division of labor, MD2 remarked:
- MD2:
-
My idea was each person could come and take ownership of the area that they are most specialized in….I think in Jennifer’s original assessment, she was also writing a neuro exam and I was like, ‘we already did that.’ I think sometimes… it felt like there were almost too many cooks in the kitchen. [Group 2 Week 1 Debrief]
When Jennifer and PH2 attempted to incorporate a patient’s psychosocial concern, outside of their traditional professional scope, they were rebuffed by MD2:
- MD2:
-
Anything you guys want to add?
- PH2:
-
He also has depression
- MD2:
-
I don’t think we need to list every single thing on his problem list, there’s like a million things
- PT:
-
But, I think that we actively saw [low mood] yesterday… I think it would be a good problem to put on there. (brief negotiation in group of extent of problem list)
- PT:
-
I think that for me, as far as the mood thing goes, I feel like that since we saw it… because we actually were aware that…
- MD2:
-
(cuts her off) That’s not really…that’s just like, I wouldn’t call that, that’s not part of depression…. [Group 2 Week 1 Field Notes]
This interaction highlights an observable difference in rules and division of labor between groups 1 and 2 (Table 1). While in group 1, all students might have been encouraged to express concerns about a patient’s mood, group 2’s rules curtailed dialogue that had previously allowed Jennifer the opportunity to expand her role.
Overall group 2 impact on student role fluidity
The observable differences between group 1 and group 2’s activity systems illustrates how slight variability in system elements influences learner roles. Group 2’s activity system suggests Jennifer had limited scope and flexibility to expand beyond tasks associated with PT expertise. System elements appeared to change Jennifer’s more fluid role in group 1 to a role of professional, expertise-driven tasks in group 2. In Jennifer’s own words, with this group she focused on her “part” of the exercise.
- PT:
-
… I just wanted to make sure on my part to hit the basics that I get with most notes that I write for PT… [Group 2 Week 2 Debrief]
Group 3 activity system
In group 3, which occurred directly after group 2, Jennifer was part of what was observably a more inclusive and collaborative group that fostered role fluidity compared to group 2, and even group 1 (Table 1). Group 3’s activity system reinforced elements contributing to Jennifer’s broader role in group 1, and highlighted elements that were observably less supportive of her role expansion in group 2 (Fig. 6).
Group 3: tools and community
Going beyond group 1’s tool use, where the computer and note provided a point for conversation and supported Jennifer’s engagement in medical conversations, group 3’s use of the same tools (Table 1) helped create a community of collaboration and discovery for all group members by serving as a focal point for discussions,
- PT:
-
Let’s do the A&P together if that’s ok?
- MD3:
-
Sure! (dictates aloud while writing)
- PT:
-
(actively watches her type and follows text)
Looks like he’s been having that pain from before the fracture too (pointing to screen) (discussion with MD3 and PH3 about prior injuries to hips) [Group 3 Week 1 Field Notes]
and teaching between group members as they wrote the note together:
- MD3:
-
You want to look at any PT stuff?
- PT:
-
Yup. (takes mouse and scrolls)
(teaches the MD3/PH3 about home stairlift setup, explains initial PT assessment she did while looking through the chart) [Group 3 Week 1 Field Notes]
Group 3: rules and division of labor
Group 3 developed additional rules not seen in prior groups that fostered expression of views and inclusivity (Table 1) while creating care plans, which allowed group members, primarily Jennifer, to broaden her role. While almost jokingly stated by MD3 during week 1,
- PT:
-
Ok so can I ask another stupid question?
- MD3:
-
There are no stupid questions! [Group 3 Week 1 Field Notes]
this rule encouraged conversations and led to numerous student questions and contributions related to tasks outside the traditional profession-based division of labor. The community’s rules reinforced their collaborative space, allowing for knowledge sharing. For example, when group 3 initially suggested that PH3 assess a patient’s pain medication regimen, Jennifer’s questions helped clarify the plan:
- PT:
-
What’s the difference that you see between morphine and oxycodone?
- PH3:
-
Well, there are dose conversions between morphine and oxycodone
- PT:
-
Is one stronger than the other? Is there a raising of risk of one vs the other aside from renal impairment?
- PH3:
-
I’m not sure why they switched him… (pauses, thinks) (PH3 clarifies pain plan) [Group 3 Week 1 Field Notes]
During the debrief, MD3 acknowledged the group’s intent behind creating this open space and how it affected the group’s learning experience:
- MD3:
-
What I did like about the exercise was that, especially Jennifer, but I think all of us to some extent, felt open enough to ask questions about stuff we didn’t know. I thought that was a good learning process that gives us some insight into the other person’s discipline. [Group 3 Week 2 Debrief]
Group 3 also encouraged everyone to contribute to problem planning regardless of profession, particularly when a student’s profession was not easily represented in the care plan:
- MD3:
-
Even though Jennifer and PH3 were limited in what they were able to contribute specific to their disciplines, they both did a really good job of suggesting things, just behaviorally. Even though Jennifer… wasn’t able to do a physical assessment [due to the patient’s severe dementia], we were all brainstorming on ideas to help with the issue of behavior. [Group 3 Week 2 Debrief]
When unable to provide a functional assessment, Jennifer found ways of incorporating PT-related knowledge into other medical problems, such as suggesting exercise to improve a patient’s hypertension. Jennifer noted that hypertension management is not typically a task she tackles, but that in this group, she broadened her role to use her PT skills in medical plan creation:
- LKB:
-
Is that something you usually think about when you’re in PT?
- PT:
-
I think it came up more for this patient…where maybe [suggesting exercise] wouldn’t have been my first instinct of jumping in on the hypertension, but for this patient, I was just more along the lines of “what else could we provide to him that would help that?” [Group 3 Week 2 Debrief]
Overall group 3 impact on student role fluidity
We observed that while group 3’s activity system included similar system tensions affecting Jennifer’s role fluidity as group 1, in this system she integrated as an active collaborator in the medical plans. In group 3 she took an active participatory role in medical decision making, beyond her group 1 role as an inquisitive explorer.
Discussion
Our study of role fluidity and its barriers and facilitators in a clinically-based IP learning activity identified ways in which a student’s role can expand and contract as health professional students work together to care for a patient. By analyzing group processes as activity systems and following one student across three groups, we found key interactions among community (working together or independently); rules guiding the group process (emphasizing collaboration or efficiency, encouraging or discouraging inquiry); tool use (computers as unifiers or dividers); and division of labor (strict or flexible task assignment) that influenced the student’s role fluidity as seen by her expansion from, or constriction to, professional role. Given the complexity of psychosocial and material factors impacting a clinical learning environment, it is unlikely that even the most thoughtfully constructed IP activity system will consistently yield role fluidity of all members (Gruppen et al. 2019; Papp et al. 2003). However, these group elements have the potential for intervention by educators working in IP learning environments. Our study can inform the design of such interventions. In the remainder of the discussion, we explore how our findings about these system elements can be incorporated in the design and facilitation of clinically based IPE activities and environments to foster role fluidity.
We found that implicit or explicit rules that emphasized collaboration and learning over efficiency and role siloing helped groups construct inclusive, encouraging, and inquisitive learning communities that fostered role expansion. Implicit rules in groups 1 and 3 encouraged Jennifer’s questions and participation in care planning; by contrast, group 2’s prioritization of efficiency through sharp division of labor reduced the potential for collaboration and all-encompassing plan construction. Rules represent sociocultural aspects of the environment, and particularly affect peer relationships that are a valuable part of the learning environment (Jessee 2016). As educators, we can help guide group rules through our instructions and explicit encouragement of an environment that promotes students’ role fluidity. Instructions that emphasize working together, encourage students to teach each other, and allow sufficient time rather than imposing tight time constraints, may help students see their goal as more than efficient task completion and help students go beyond their internalized basic professional rules to work interprofessionally. While in professional teams, some work has shown the need for explicit internalized rules of behavior (Pype et al. 2018), and others have described that authentic rules, unique to team dynamics, could help improve teamwork, student teams likely need more direction on rules to help foster collaboration (Lingard et al. 2004). Social rules are more likely implicit and can be challenging to infer; there could be a role for establishing social rules that foster role fluidity (Ching et al. 2020). Educators need to address implicit ‘leader’ roles within a group that set a silent hierarchy and unspoken rule of operating within a role and/or in isolation. Providing explicit instructions to students that make it okay to both express role clarity and engage in role fluidity (e.g., expansion or contraction of role depending on the clinical and team circumstances), could reduce resistance to dynamic roles.
Division of labor closely relates to the role fluidity of each group member as it defines the tasks, and flexibility of tasks, each member ‘owns’ in their role. When Jennifer participated in group 2, which had tight division of labor based on professional expertise, she displayed minimal role fluidity. By remaining firmly fixed in her role as a PT in group 2, Jennifer and her fellow students missed a key goal of IP collaboration; this was not seen in the more flexible division of labor employed by groups 1 and 3. Jennifer’s reflections in the debriefing indicated dissatisfaction with this constrained PT role and the team care plans from this group were notably less holistic and comprehensive than others in which her role was less constrained. We speculate that when division of labor tasks are not allocated solely by profession (e.g., all students think through functional assessment), students participate in a broader variety of tasks that lead to more complete care plans.
Influencing division of labor in IP groups to foster role fluidity might require reconsidering how we teach IP roles. Focusing on what tasks could be completed by multiple healthcare providers as opposed to focusing on the tasks that healthcare providers traditionally do could open a dialogue between students as to role fluidity’s place in patient care. Our results mirror those of Jakobsen’s team, who noted that when nursing and medical students shared tasks, whether related or unrelated necessarily to their profession, students demonstrated positive social emotions and learned from each other (Jakobsen et al. 2018). We speculate that by encouraging IP student teams to approach tasks with the goal of task sharing, rather than tasks being assigned to the supposed ‘expert,’ educators allow for the organic processes of growing and bending beyond normal role constraints.
We found that tools—in our case, the team’s computers—serve as unifiers or dividers for communities that foster or inhibit role fluidity. In groups 1 and 3, students clustered around a shared computer and the computers became a focus for collaboration and more inclusive conversations. These groups showed Jennifer using the tool to foster conversations that broadened her role. While there is no certainty that students will choose to use tools collaboratively, by setting up learning environments and tools to promote collaboration, educators may provide some infrastructural scaffolding to support fluidity. The material components of learning environments are critical and this study shows the effect tangible tools have directly on the environment (Gruppen et al. 2019). The notion that ‘more is better’ in terms of access to technology or standardized templates breaks down when it pigeonholes students into professional-role-driven, task-driven experiences as they each work with tools on ‘their part’ of a task. As Kent found in her observations of IP student teams, checklist tools for patient interviews led to dependency on having to follow the tool (Kent et al. 2016). There could be value in creating spaces that push collaborative learning, such as offering more collaborative learning tools such as whiteboards or asking student groups to create their own checklist or template. Through careful construction of collaborative spaces, we might help role fluidity thrive.
Our findings suggest that the dynamic ability of learners to flow across professional boundaries could have noticeable changes in construction of comprehensive care plans. While some tasks can be completed by a single IP group member, (i.e., pharmacist investigating drug dosing), more holistic patient care issues, such as considering someone’s psychosocial needs, might benefit from diverse IP group member engagement through role fluidity. Intentionally designing IP activities to support role fluidity, along with role clarity, can open new opportunities for creative thinking and task completion from all IP group members that more accurately represents optimal teamwork in clinical practice (Lingard et al. 2017; Salas et al. 2005). Design changes, though, could also lead to increased team role conflict. As noted by Paradis and Whitehead, power and conflict within IPE is rarely studied, though present in teams (Paradis and Whitehead 2018). We feel that observing role fluidity could provide a framework for investigations into how roles impact conflict within teams. Future work could investigate how changes to the rules, division of labor, and tools of an IP team alter both role fluidity/clarity and the power dynamics, within IP teams.
We also note that while we argue that role fluidity is a necessary part of IPE, that our students were towards the end of their training and had firm foundations related to roles and responsibilities as developed by their prior IPE curricula and clinical care experiences. We would advocate that when constructing an IPE curriculum, that educators introduce role fluidity when describing IP team roles so that students understand there are opportunities for crossing sharp role boundaries. However, role fluidity is a skill best fostered and practiced in IPE activities designed for advanced students nearing the end of their training. In those settings, students can explore the possibilities of where to apply and engage in role fluidity over strict role clarity. Much like how a medical student must learn physiology before pathophysiology, IPE can promote foundations of role identity and clarity prior to creating variations in the learning environment that foster role fluidity. Future research could investigate what point in IP training would be best suited for students exploring role fluidity as well as how IP facilitators can identify that students are prepared to expand and broaden their roles.
Given our interest in factors impacting role fluidity, our collective instrumental case study approach in an IP nursing home environment allowed for the depth we needed to discern important and consistent interactions and tensions leading to student role fluidity in IP groups. This approach and setting, does, however, have limitations. Focusing on a single student limits our ability to disentangle individual characteristics (personality, clinical skills) and situational factors in our analysis of role fluidity. Nonetheless, our approach provided an in-depth look at both how a single student’s role fluidity changed across three unique groups—where the elements of the group (situational factors) are likely to change more than the student’s individual characteristics. We also acknowledge there are factors intrinsic to all student groups that are neither captured by activity system analysis, nor modifiable by external sources. Interpersonal dynamics, prior clinical and IP experiences, and attitudes toward IPE often impact the learning environment and can hinder a group’s ability to function, despite the best efforts in constructing a conducive learning climate (Channon et al. 2017; Gruppen et al. 2019; Nordquist et al. 2019; Rhee et al. 2013). However, by identifying key interactions and tensions organically affecting role fluidity, we hope that educators will be able to recognize and minimize potentially disruptive group dynamics that can inhibit role exploration. An additional potential limitation lies in the translatability of our findings beyond the nursing home learning environment. The nursing home setting, though, has a long history of IP practice and affords many opportunities for authentic IP patient care that may not exist in other settings, providing an authentic environment in which to observe role fluidity in clinical practice (Annear et al. 2016; Hilton and Morris 2001; Kent et al. 2016).
Concluding comments
Our work provides insights, and future directions for research, into the elements within IP learning systems affecting role fluidity. The learning opportunities offered by role fluidity suggest that we, as IP educators, need to think beyond, and build upon, narrow conceptualization of IPE competencies focusing on role definition and clarity for advanced students in IPE. Explicitly encouraging role fluidity for IP teams could improve the clinical care setting by fostering dynamic broadening of role inclusion, which could thus broaden holistic contributions to patient care. With ongoing interest in healthcare towards improving efficient patient care, future work could take insights from our study and further investigate how role fluidity impacts the efficiency, and quality, of patient care within IP teams (Frenk et al. 2010). Within IP education, further research into the ability of educators to craft role fluidity by manipulating IP learner tool use, rules, and division of labor, could help clarify the broader utility of trying to influence role fluidity.
References
Ambrose-Miller, W., & Ashcroft, R. (2016). Challenges faced by social workers as members of interprofessional collaborative health care teams. Health and Social Work, 41(2), 101–109.
Annear, M. J., Goldberg, L. R., Lo, A., & Robinson, A. (2016). Interprofessional curriculum development achieves results: Initial evidence from a dementia-care protocol. Journal of Interprofessional Care, 30(3), 391–393. https://doi.org/10.3109/13561820.2015.1117061.
Barrow, M., McKimm, J., Gasquoine, S., & Rowe, D. (2015). Collaborating in healthcare delivery: Exploring conceptual differences at the “bedside”. Journal of Interprofessional Care, 29(2), 119–124. https://doi.org/10.3109/13561820.2014.955911.
Battista, A. (2015). Activity theory and analyzing learning in simulations. Simulation and Gaming, 46(2), 187–196. https://doi.org/10.1177/1046878115598481.
Bittner, C. (2018). The importance of role clarity for development of interprofessional teams. The Journal of Continuing Education in Nursing, 49(8), 345–347.
Bleakley, A. (2006). Broadening conceptions of learning in medical education: The message from teamworking. Medical Education, 40, 150–157.
Bleakley, A., Bligh, J., & Browne, J. (2011). Socio-cultural learning theories. In A. Bleakley, J. Bligh, & J. Browne (Eds.), Medical education for the future: Identity, power and location (pp. 43–60). Springer Netherlands. https://doi.org/10.1007/978-90-481-9692-0_4.
Bridges, D., Davidson, R. A., Odegard, P. S., Maki, I. V., & Tomkowiak, J. (2011). Interprofessional collaboration: Three best practice models of interprofessional education. Medical Education Online, 16(1), 6035. https://doi.org/10.3402/meo.v16i0.6035.
Brown, B., Crawford, P., & Darongkamas, J. (2000). Blurred roles and permeable boundaries: The experience of multidisciplinary working in community mental health. Health and Social Care in the Community, 8(6), 425–435.
Channon, S. B., Davis, R. C., Goode, N. T., & May, S. A. (2017). What makes a “good group”? Exploring the characteristics and performance of undergraduate student groups. Advances in Health Sciences Education: Theory and Practice, 22(1), 17–41. https://doi.org/10.1007/s10459-016-9680-y.
Cheek, C., Hays, R., Smith, J., & Allen, P. (2017). Improving case study research in medical education: A systematised review. Medical Education. https://doi.org/10.1111/medu.13469.
Ching, S. S. Y., Cheung, K., Hegney, D., & Rees, C. S. (2020). Stressors and coping of nursing students in clinical placement: A qualitative study contextualizing their resilience and burnout. Nurse Education in Practice, 42, 102690. https://doi.org/10.1016/j.nepr.2019.102690.
Engeström, Y. (2001). Expansive learning at work: Toward an activity theoretical reconceptualization. Journal of Education and Work, 14(1), 133–156. https://doi.org/10.1080/13639080020028747.
Engeström, Y. (2015). Learning by expanding: An activity-theoretical approach to developmental research (2nd ed.). Cambridge: Cambridge University Press.
Frenk, J., Chen, L., Bhutta, Z. A., Cohen, J., Crisp, N., Evans, T., et al. (2010). Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet, 376(9756), 1923–1958. https://doi.org/10.1016/S0140-6736(10)61854-5.
Furr, S., Lane, S. H., Martin, D., & Brackney, D. E. (2020). Understanding roles in health care through interprofessional educational experiences. British Journal of Nursing, 29(6), 364–372. https://doi.org/10.12968/bjon.2020.29.6.364.
Galvin, J. E., Valois, L., & Zweig, Y. (2014). Collaborative transdisciplinary team approach for dementia care. Neurodegenerative Disease Management, 4(6), 455–469. https://doi.org/10.2217/nmt.14.47.
Gilbert, J. H. V., Yan, J., & Hoffman, S. J. (2010). A WHO report: Framework for action on interprofessional education and collaborative practice. Journal of Allied Health, 39(Suppl 1), 196–197.
Giuliante, M. M., Greenberg, S. A., McDonald, M. V., Squires, A., Moore, R., & Cortes, T. A. (2018). Geriatric interdisciplinary team training 2.0: A collaborative team-based approach to delivering care. Journal of Interprofessional Care. https://doi.org/10.1080/13561820.2018.1457630.
Gruppen, L. D., Irby, D. M., Durning, S. J., & Maggio, L. A. (2019). Conceptualizing learning environments in the health professions. Academic Medicine: Journal of the Association of American Medical Colleges, 94(7), 969–974. https://doi.org/10.1097/ACM.0000000000002702.
Gunaldo, T. P., Andrieu, S. C., Garbee, D., Giovingo, L. K., Mercante, D. E., Tortu, S., et al. (2015). Student perceptions about interprofessional education after an elective course. Journal of Interprofessional Care, 29(4), 370–371. https://doi.org/10.3109/13561820.2014.969836.
Harrod, M., Weston, L. E., Robinson, C., Tremblay, A., Greenstone, C. L., & Forman, J. (2016). It goes beyond good camaraderie”: A qualitative study of the process of becoming an interprofessional healthcare “teamlet. Journal of Interprofessional Care, 30(3), 295–300. https://doi.org/10.3109/13561820.2015.1130028.
Hean, S., Green, C., Anderson, E., Morris, D., John, C., Pitt, R., & O’Halloran, C. (2018). The contribution of theory to the design, delivery, and evaluation of interprofessional curricula: BEME Guide No. 49. Medical Teacher. https://doi.org/10.1080/0142159X.2018.1432851.
Hilton, R., & Morris, J. (2001). Student placements—Is there evidence supporting team skill development in clinical practice settings? Journal of Interprofessional Care, 15(2), 171–183.
Hudson, C. C., Gauvin, S., Tabanfar, R., Poffenroth, A. M., Lee, J. S., & O’Riordan, A. L. (2017). Promotion of role clarification in the health care team challenge. Journal of Interprofessional Care, 31(3), 401–403. https://doi.org/10.1080/13561820.2016.1258393.
Interprofessional Education Collaborative. (2016). Core competencies for interprofessional collaborative practice: 2016 update. Washington, DC: Interprofessional Education Collaborative.
Jakobsen, F., Musaeus, P., Kirkeby, L., Hansen, T. B., & Mørcke, A. M. (2018). Emotions and clinical learning in an interprofessional outpatient clinic: A focused ethnographic study. Journal of Interprofessional Care. https://doi.org/10.1080/13561820.2018.1514372.
Jessee, M. A. (2016). Influences of sociocultural factors within the clinical learning environment on students’ perceptions of learning: An integrative review. Journal of Professional Nursing: Official Journal of the American Association of Colleges of Nursing, 32(6), 463–486. https://doi.org/10.1016/j.profnurs.2016.03.006.
Johnston, J., & Dornan, T. (2015). Activity theory: Mediating research in medical education. In Researching medical education (pp. 93–103). Wiley.
Kent, F., Francis-Cracknell, A., McDonald, R., Newton, J. M., Keating, J. L., & Dodic, M. (2016a). How do interprofessional student teams interact in a primary care clinic? A qualitative analysis using activity theory. Advances in Health Sciences Education: Theory and Practice. https://doi.org/10.1007/s10459-015-9663-4.
Kent, F., Lai, F., Beovich, B., & Dodic, M. (2016b). Interprofessional student teams augmenting service provision in residential aged care. Australasian Journal on Ageing. https://doi.org/10.1111/ajag.12288.
Lingard, L., Espin, S., Evans, C., & Hawryluck, L. (2004). The rules of the game: Interprofessional collaboration on the intensive care unit team. Critical Care, 8(6), R403–R408. https://doi.org/10.1186/cc2958.
Lingard, L., McDougall, A., Levstik, M., Chandok, N., Spafford, M. M., & Schryer, C. (2012). Representing complexity well: A story about teamwork, with implications for how we teach collaboration. Medical Education, 46(9), 869–877. https://doi.org/10.1111/j.1365-2923.2012.04339.x.
Lingard, L., Sue-Chue-Lam, C., Tait, G. R., Bates, J., Shadd, J., Schulz, V., & Heart Failure/Palliative Care Teamwork Research Group. (2017). Pulling together and pulling apart: Influences of convergence and divergence on distributed healthcare teams. Advances in Health Sciences Education: Theory and Practice, 22(5), 1085–1099. https://doi.org/10.1007/s10459-016-9741-2.
MacNaughton, K., Chreim, S., & Bourgeault, I. L. (2013). Role construction and boundaries in interprofessional primary health care teams: A qualitative study. BMC Health Services Research, 13, 486. https://doi.org/10.1186/1472-6963-13-486.
McMurty, A., Shanta, R., & Kilgour, K. (2016). Socio-material perspectives on interprofessional team and collaborative learning. Medical Education, 50, 169–180. https://doi.org/10.1111/medu.12833.
Nordquist, J., Hall, J., Caverzagie, K., Snell, L., Chan, M.-K., Thoma, B., et al. (2019). The clinical learning environment. Medical Teacher, 41(4), 366–372. https://doi.org/10.1080/0142159X.2019.1566601.
O’Brien, B. C., Little, J. W., Wamsley, M., Cook, J. G., Yuan, P., Rivera, J., et al. (2017). Emergent is authentic: A sociomaterial perspective on simulation-enhanced interprofessional education. Teaching and Learning in Medicine, 29(4), 363–367. https://doi.org/10.1080/10401334.2017.1361326.
O’Keefe, M., & Ward, H. (2018). Implementing interprofessional learning curriculum: How problems might also be answers. BMC Medical Education, 18, 132. https://bmcmededuc-biomedcentral-com.liboff.ohsu.edu/articles/10.1186/s12909-018-1231-1.
O’Neill, B. J., & Wyness, M. A. (2005). Student voices on an interprofessional course. Medical Teacher, 27(5), 433–438. https://doi.org/10.1080/01421590500086680.
Papp, I., Markkanen, M., & von Bonsdorff, M. (2003). Clinical environment as a learning environment: Student nurses’ perceptions concerning clinical learning experiences. Nurse Education Today, 23(4), 262–268. https://doi.org/10.1016/S0260-6917(02)00185-5.
Paradis, E., & Whitehead, C. R. (2018). Beyond the lamppost: A proposal for a fourth wave of education for collaboration. Academic Medicine, 93(10), 1457–1463. https://doi.org/10.1097/ACM.0000000000002233.
Pype, P., Mertens, F., Helewaut, F., & Krystallidou, D. (2018). Healthcare teams as complex adaptive systems: Understanding team behaviour through team members’ perception of interpersonal interaction. BMC Health Services Research, 18(1), 570. https://doi.org/10.1186/s12913-018-3392-3.
Rhee, J., Parent, D., & Basu, A. (2013). The influence of personality and ability on undergraduate teamwork and team performance. SpringerPlus, 2(1), 16. https://doi.org/10.1186/2193-1801-2-16.
Salas, E., Sims, D. E., & Burke, C. S. (2005). Is there a “big five” in teamwork? Small Group Research, 36(5), 555–599. https://doi.org/10.1177/1046496405277134.
Stake, R. E. (1995). The art of case study research. Thousand Oaks: SAGE.
Suter, E., Arndt, J., Arthur, N., Parboosingh, J., Taylor, E., & Deutschlander, S. (2009). Role understanding and effective communication as core competencies for collaborative practice. Journal of Interprofessional Care, 23(1), 41–51. https://doi.org/10.1080/13561820802338579.
Thomas, G., & Myers, K. (2018). The anatomy of the case study. https://doi.org/10.4135/9781473920156.
Varpio, L., Hall, P., Lingard, L., & Schryer, C. F. (2008). Interprofessional communication and medical error: A reframing of research questions and approaches. Academic Medicine: Journal of the Association of American Medical Colleges, 83(10 Suppl), S76–S81. https://doi.org/10.1097/ACM.0b013e318183e67b.
Yamagata-Lynch, L. C. (2010). Activity systems analysis methods: Understanding complex learning environments. New York: Springer.
Yamagata-Lynch, L. C., & Haudenschild, M. T. (2009). Using activity systems analysis to identify inner contradictions in teacher professional development. Teaching and Teacher Education, 25(3), 507–517. https://doi.org/10.1016/j.tate.2008.09.014.
Yamagata-Lynch, L. C., & Smaldino, S. (2007). Using activity theory to evaluate and improve K-12 school and university partnerships. Evaluation and Program Planning, 30(4), 364–380. https://doi.org/10.1016/j.evalprogplan.2007.08.003.
Acknowledgements
We thank Dr. Judith Bowen for her expert critique and review of this manuscript. We also thank Rachel Campbell, PharmD and Jessica Larson, DPT for their assistance in student care plans review as well as their support as student preceptors.
Funding
This project was funded in part by a 2016 AAMC Western Group on Educational Affairs Mini-Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Byerly, L.K., Floren, L.C., Yukawa, M. et al. Getting outside the box: exploring role fluidity in interprofessional student groups through the lens of activity theory. Adv in Health Sci Educ 26, 253–275 (2021). https://doi.org/10.1007/s10459-020-09983-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10459-020-09983-w