Abstract
Practice based interprofessional education opportunities are proposed as a mechanism for health professionals to learn teamwork skills and gain an understanding of the roles of others. Primary care is an area of practice that offers a promising option for interprofessional student learning. In this study, we investigated what and how students from differing professions learn together. Our findings inform the design of future interprofessional education initiatives. Using activity theory, we conducted an ethnographic investigation of interprofessional education in primary care. During a 5 months period, we observed 14 clinic sessions involving mixed discipline student teams who interviewed people with chronic disease. Teams were comprised of senior medicine, nursing, occupational therapy, pharmacy and physiotherapy entry level students. Semi-structured interviews were also conducted with seven clinical educators. Data were analysed to ascertain the objectives, tools, rules and division of labour. Two integrated activity systems were identified: (1) student teams gathering information to determine patients’ health care needs and (2) patients either as health consumers or student educators. Unwritten rules regarding ‘shared contribution’, ‘patient as key information source’ and ‘time constraints’ were identified. Both the significance of software literacy on team leadership, and a pre-determined structure of enquiry, highlighted the importance of careful consideration of the tools used in interprofessional education, and the way they can influence practice. The systems of practice identified provide evidence of differing priorities and values, and multiple perspectives of how to manage health. The work reinforced the value of the patients’ voice in clinical and education processes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
The health system faces challenges with the number of Australians aged 65 or over projected to more than double by 2055, with corresponding increases in the incidence of age-related disability and disease (Australian Government Productivity Commission 2011; The Commonwealth of Australia 2015). Health spending is expected to rise with increased demand for services. Current discipline specific models of care may not meet future health service needs. A re-configuration of both workforce and education programs is required to develop more efficient health and social models of care to maintain and evolve a sustainable and equitable health system (Frenk et al. 2010; Health Workforce Australia 2011). Greater focus on health promotion and injury prevention for ‘active ageing’ may be achieved by collaborative teams who understand the roles of different professions in the efficient delivery of primary care services.
Interprofessional education (IPE) has been proposed as one strategy to promote the development of a collaborative workforce with efficient team practices across domains and disciplines (World Health Organisation 2010). In Australia, the call to embed IPE in entry level health programs is gaining momentum, with the Australian Medical Council and the national Office for Teaching and Learning reports both asserting the importance of IPE experiences in the curriculum of entry level health students (Australian Medical Council 2010; The Interprofessional Curriculum Renewal Consortium 2014). The discourse of interprofessional collaboration has been considered from the perspectives of knowledge and power (Haddara and Lingard 2013) but the value of IPE rests on the premise that the patient lies at the centre of the discourse about their own health.
Despite growing implementation (Barr 2015), the potential impact of entry level IPE activities on student learning and subsequent professional practice remains unclear (Reeves et al. 2013). Teamwork skills and knowledge of the roles of other health service providers may be developed through shared learning opportunities in primary care, however the impact on patient outcomes is less clear (Kent and Keating 2015). The significant effort and additional costs incurred in delivering IPE (compared to single discipline) initiatives should also be considered in light of evidence of its effects (Haines et al. 2014). In studies to date, the primary measurements of student learning resulting from IPE have been responses to self-rating questionnaires (Hammick et al. 2007). Pre and post measurements of students’ attitudes to collaborative practice (Leucht et al. 1990) and readiness for interprofessional learning (Parsell and Bligh 1999) are frequently reported. Such measures do not directly address the effectiveness of the intervention when controlled for the effects of time and the maturation that would be expected of learners over a period of entry level education. Self-assessment of one’s ability to work with others and knowledge of other discipline roles is flawed by the limitations of self-assessment in the novice learner (Colthart et al. 2008). Self-rating questionnaires also fall short of providing education designers with useful information regarding when, what and how students learn within IPE programs.
One model of IPE involves establishing clinics where volunteer students from medicine, nursing and allied health work together to assess patient needs, in clinics set up in response to gaps in community health care (Holmqvist et al. 2012; Kent and Keating 2015). In the study reported here, this model was adapted to develop interprofessional clinics in both a general practice and residential aged care setting in the context of providing services to people with complex and chronic conditions.
The investigation of learning in teams is complex. Learning in complex and dynamic environments requires consideration of behaviors beyond those of individual health professionals (Bleakley et al. 2011). A number of theories have been proposed to explain the process and context for IPE including sociology, complexity theory, general systems theory and activity theory (Barr 2013). To explore learning in complex systems, socio-cultural theories have been described as more powerful than those oriented to individual cognition (Bleakley et al. 2011). Informed by the limitations of student self-assessment of learning, and the need to analyse the actions of a group, an ethnographic investigation of student learning was conducted using activity theory.
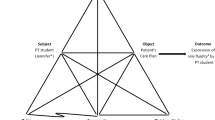
Activity theory is a psychological theory based on documenting and analysing the patterns of behaviour of an entire team or system. It has been used previously to describe the complexity of teamwork within healthcare settings (Lingard et al. 2012a; Reeves and Lewin 2004). The system includes consideration of the subjects (participants), objects (tasks), mediating artefacts (tools, instruments), rules (explicit or assumed), community (larger social group) and division of labour (task divisions) (Engestrom 2008). In an activity theory analysis of team processes in managing chronically ill children in Helsinki, subjects included the general practitioner, physician and parents, the object was movement of children between primary care and the hospital, tools included clinical pathways and relationships, rules were based on cost-effectiveness, and the division of labour was how tasks were divided between professions (Engeström 2001). Tensions within and between elements in activity systems have been described as ‘contradictions’ (Engeström 2001). Previous analyses of healthcare teams have described a process of ‘knotworking,’ with a tendency for individuals to improvise collaborative practice, drawing together an otherwise loosely connected team as required (Varpio et al. 2008). A key outcome of activity systems analysis is a diagrammatic representation that captures how the work of a group is influenced by the rules of practice, tools and divisions of labour and emergent contradictions.
In our work to date we have reported logistics of setting up student clinics and students perceived learning (Kent et al. 2014), cost of operations (Haines et al. 2014) and patient outcomes (Kent and Keating 2013; Lai et al. 2015). A natural extension of this work was to investigate how a group of students from different disciplines work and learn together. The specific research question was:
How do students from different discipline groups work together in an interprofessional clinic?
Methods
Setting
The interprofessional clinics under analysis took place in two settings: an outer metropolitan general practice and residential care setting. The clinics ran one half day per week, for 5 months.
Participants
There were three groups of participants (or subjects). The first were people being treated for chronic disease at the general practice or residential care setting, who were invited by the practice nurse to attend a student team consultation for a discussion of their perceived health issues. Participants were informed that the project was a ‘teaching and research’ clinic, where they would discuss their health with a team of students under the supervision of a qualified health professional. The dual goals of health screening and interprofessional student education were explicitly stated.
The second group of participants were fourth or final year entry level students from medicine, nursing, occupational therapy, pharmacy and physiotherapy, who volunteered to participate in one or two half day clinic sessions. Senior students were exclusively invited because it has been argued that IPE activities become meaningful when they occur in the later years of study, when students have developed the knowledge base and a sense of their own professional identity and role (Interprofessional Curriculum Renewal Consortium 2014). Students were notified of the project and invited to participate via electronic learning platforms.
The third group of participants were the educators who came from general practice medicine, nursing, community based pharmacy, physiotherapy and occupational therapy. The majority of the educators were primarily clinicians; two supervising educators had clinical practice experience but were recruited from the university. The researchers responsible for collecting observational data had practice backgrounds in physiotherapy and occupational therapy and experience in education and qualitative research.
Procedure
On any clinic day, at either the general practice or aged care facility, the activity began with group introductions and orientation to the task. Students were then divided into mixed discipline teams of two or three students, with the two teams working concurrently in different rooms. Student grouping was opportunistic based on patient need as indicated by their general practitioner and student attendance, and students were frequently not known to one another prior to arrival at the clinic. 1 h of preparation time was assigned, during which each team would initially gather around the computer to review an electronic medical history. Students then planned and conducted patient interviews in teams to explore the patients’ perceived health concerns, guided by a general health screening prompt sheet with a list of areas for enquiry: patient perceived issues, medications, mobility, falls, function, continence, cognition, communication, nutrition, social status and foot care. Patient consultations were limited to 60 min. Educators from participating disciplines supervised the consultations from a corner of the room and intervened as required. Each student team conducted two patient consultations on any clinic day. On the completion of two patient interviews, student teams wrote a summary of their findings to the patient’s general practitioner and presented each case to the larger student group for reflection and discussion.
Data
An ethnographic approach to analysis was informed by activity theory (Engeström 2001). Data were collected through direct student observation and educator interviews. Observations were conducted by one of two researchers, who predominately maintained a position as silent observers of interprofessional teams, in the corner of consultation rooms. However, if required, a marginal participant role was adopted to interact with students if they sought clarification about the required task. Hand written, non-identifying notes were taken on how the teams operated. Notes were taken under three vertical columns titled subjects, activities and tools, to document systematically who was completing what task and with what tools.
Data analysis
At the completion of the 5 months study period, two researchers reviewed the observational data. Using an activity theory framework, they individually conducted open coding of the raw observational data of seven observation sessions that represented all combinations of participating student disciplines. The researchers came together to establish consensus on the activity systems observed, with disagreements resolved through re-analysis of the raw observational data and discussion.
In addition, all educators involved in supervising students in the clinic were invited to attend a 20 min semi-structured interview to describe their observations of students’ learning. Interviews were conducted by a research assistant and senior member of the research team, recorded and transcribed by a transcription service, and checked for errors. Transcripts were independently reviewed and coded by two researchers; agreement on themes was established by discussion. Cross case analysis was conducted to investigate areas of variability in responses by discipline and to investigate the stability of the findings (Miles and Huberman 1994). Quotations and sections of text were extracted to show examples of data that led to the development of themes. Themes were then considered within the framework of the activity systems identified through the observational data.
Ethics
All participating patients, students and educators provided informed consent and ethics approval was obtained from Monash University (Approval Number: CF14/509-2014000163).
Results
The results present the activity systems that emerged from analysis: the subjects, objectives, objects, tools, rules, community, divisions of labour and how they interacted. The contradictions within the systems are described. The discussion relates the findings to the interprofessional literature.
During the 5 months study period, observations were conducted on 14 clinic sessions involving n = 48 students from medicine (Med = 20), nursing (NS = 6), occupational therapy (OT = 4), pharmacy (Phar = 13) and physiotherapy (PT = 5). Some students attended on more than one occasion. Seven of the nine participating educators consented to interview, representing medicine (4), nursing (1), pharmacy (1) and physiotherapy (1).
Two activity systems were identified across the studies: students gathering health information to determine the health care needs of the patient and patients adopting either a health consumer or student educator role (Fig. 1). The purpose of the consultations informed the student objectives, which was to gather sufficient information to identify unmet patient healthcare needs. To achieve this objective, student teams focused on the information in the electronic medical file and provided by the patient, and on the knowledge needed to understand the issues.
Observational data suggested that patient objectives varied from educating students on a consumer’s perspective of living with and managing chronic disease, to seeking information to maximise their own health and independence. Some patient objectives were achieved when patients were able to describe their experience of living with chronic disease and how modifications to their daily activities allowed them to maximise function, despite their health limitations. Other patient (and student) objectives were achieved when patients gained new health promotion information from the student teams.
The software used to document and store patients’ medical health records was a key tool used by student teams to determine current health issues. Several medical students were familiar with navigating the software due to previous exposure on general practice rotations but regardless of experience, the role of navigating the program, and managing the paperwork tended to be adopted by the medical student. Additional tools were at times utilised to gain supplementary information such as a medication reference text (EBSCO 2014) by pharmacy students and online search engines to check the meaning of unfamiliar terms.
The screening interview prompt sheet largely dictated the content of the patient interview. This screening tool was distributed prior to attending the clinic and prompted students to consider areas beyond the remit of their usual discipline specific interview. The content of the prompt sheet informed the way the students conducted the interviews. Commonly, student teams negotiated how the aspects of the interview should be divided based on areas listed on the screening tool and their specific knowledge and confidence with those areas. This is illustrated in the field notes below.
NS | [says to Med, Phar student team] I am very happy to do a. to d., how about you pick up from the cognition bit |
Observation notes general practice (September) | |
PT, OT | Discussion—who will talk about what. Prompted by screening tool |
PT, OT, Med | Discussion about division of roles and sequence of interview. Screening tool-prompting topics |
Observation notes general practice (May) | |
Multiple rules were identified. Student team behaviour was influenced by the unspoken rule that everyone should contribute in getting the job done. For example, a student might invite another student for their perspective, if they had not been contributing to the discussion. To enact this rule, students frequently held discussions when they first came together to explore the roles and skills of others as captured in the following field notes:
NS | [asks OT] so what do OT’s do? |
OT | Description of role |
… | |
Med | Adopts some leadership [asks Phar] From a pharmacy perspective, what would you like to know? |
Observation notes residential care (July) | |
Med | [asks Phar] do you educate the patients? |
Observation notes general practice (June) | |
Students frequently used each other as a source of information and clarification; a shared understanding of the clinical case evolved through discussion. Students frequently declared areas of uncertainty. When asked, medical students commonly explained unfamiliar terms and pharmacy students frequently explained the purpose and side effects of medications as captured in the field note below.
PT, OT, Med | Discussion about past history—clarification of terms |
PT | Explains emphysema to OT |
Med | Explains lupus… |
OT | Questions…[asks] How does it affect someone? |
Observation notes session general practice (May) | |
Med | [comments to group] Had a grand mal! |
Phar | [asks]What’s a grand mal seizure? |
Med | [explains grand mal seizure to Phar student] |
Phar | looks up some medication side effects |
Med | [comments]I wonder what this drug is? |
Phar | [answers] It’s an antinflam |
Observation notes general practice (June) | |
The team presentations at the completion of each clinic session reinforced the extent of collaboration, with individuals supporting one another in the recall of details when required. In one case, collaborative work was less apparent with one medical student completing an excessive proportion of tasks, which resulted in a final case presentation lacking comprehensive analysis.
A common finding in the observational data and the educator interviews was the perception that exploring chronic disease was challenging and consultation time was limited. On occasions, students found addressing the complexity of the health issues challenging within the available time. By contrast, the complexity of the cases was considered a strength of the learning experience by the educators.
…you don’t have that long to discern the relevant information and act on it
Interview 5
…the advantage of having multiple disciplines is, particularly with students…see that looking at a complex medical problem requires a lot of complex interactions between different areas of allied health
Interview 1
A final rule was the priority held by students that the patients’ perspective was a key source of information. Patients disclosed both the complexity of their health history and the strategies they adopted to manage their needs and limitations.
Med | Describes what [the team] thought when they read [the history] were |
nothing like her problems | |
Observation notes general practice (June) | |
Patient | Explains how she manages with bathroom overnight and gardening…has exercise sheets from when did [exercise] class, self directed goals e.g. walk around lake…role of rehab that gave her strategies to cope with SOB [shortness of breath], ADL [activities of daily living] |
Observation notes general practice (May) | |
In the division of labour, leadership of the student teams was assumed, rather than negotiated, and was most likely informed by discipline, personality and confidence of student participants. The tendency for medical students to navigate the patient medical information via the software reinforced their leadership role.
The medical students were probably more common leaders, but certainly not always the case…I saw pharmacy students leading and I saw physio students leading. I didn’t at any point see a nursing student lead a session, but looking at how those sessions panned out, this was very much about personality. It was around confidence, and sometimes it was around knowledge
Interview 5
The wider community contribution to the activity systems was extensive. The family members, practice nurse, health network, health care system, aged care providers and general practice reception staff all contributed in a variety of ways. This was not a focus of analysis in this study.
Contradictions within the activity systems occurred, noted by the lightening-shaped arrows in Fig. 1. Contradictions were identified within and between the patient and student team activity systems. The outcome of these combined student/patient objectives was at times differing priorities and values, and multiple perspectives of how best to manage health.
The student activity system was not successful when student teams remained focused on their area of expertise and were unable to structure the interview to identify patient priorities. This may have occurred when the patient’s issue was beyond the participating student teams’ interest, knowledge or skill or not identified because it was beyond the content of the screening prompt tool. In the event that students remained focused on their discipline perspective, rather than the patient’s priority, the activity systems of the students and patients did not successfully result in both objectives being met.
…the major deficiency in what the students have is the ability to have a perspective of what is really required to prioritise the patient’s management, because when you’ve got these different disciplines, they tend to focus on their discipline. That creates a problem, because that’s not always what the patient is mainly concerned about
Interview 1
Contradictions occurred when patients were less effective in student education in circumstances where their health condition did not require engagement with a particular discipline perspective (Fig. 1). For example a patient on minimal medications was a less effective teaching case for a pharmacy student, or a physically active patient engaged in a community exercise program was a less effective source of learning for a physiotherapy student. Differing perspectives about best practice in health management based on either the students’ perspectives or a patient preference occasionally occurred as illustrated in the observation note below:
Med | [asks patient] have you had your fats in the blood tested? |
Patient | deny need to test it |
Observation notes general practice (June) | |
As these results illustrate, learning can be a reciprocal relationship not only between student teams, but also between students and patients. A system approach for analysis reveals the tensions arising from these perspectives.
Discussion
IPE has been proposed as a useful mechanism to educate students about the roles of other health disciplines with whom they will work (World Health Organisation 2010). Two areas of growing need for collaboration are primary care and aged care, where chronic disease management is central to effective health services. Although complex in both education design and evaluation, investigation of how collaboration and effective teamwork can be taught is required (Frenk et al. 2010).
In this study, an analysis of interprofessional student teams at work provides useful information for education designers about the interactions and learning processes that occur. Learning was socially constructed through dialogue between students, patients and educators and facilitated through legitimate participation in a useful yet challenging task. The observation of interprofessional teams in primary care revealed that students brought their discipline focus, yet the patients’ perspective remained central to the health discourse and recommended management. Activity theory usefully assisted in the analysis of this system, through the identification of contradictions and areas for further consideration and development.
Real patients offer real life complexity, and therefore rich learning opportunities (Bleakley et al. 2011). Effective chronic disease management requires the integration of a range of health discipline perspectives. Co-locating students from different professions in primary care, with a shared patient case, provides opportunity for organisation and practice of collaborative service delivery. Through direct questioning of one another and observation, students were exposed to the areas of knowledge (and knowledge gap) of others, and areas of discipline knowledge and practice overlap. Within each clinic session, the task of ‘getting the job done’ was delivered to the team, rather than to any individual, and this required that students distribute the workload. Student participants tended to organise their teams to ensure tasks could be completed within the limited time, and shared the load.
In the absence of a ‘usual’ way for students from different disciplines to conduct a shared consultation, the tasks and tools provided strongly influenced behaviour. Although not the intention, the screening prompt sheet was at times used like a checklist. A positive result was the breadth of content covered; a negative result was the risk that the tool directed the interview rather than enabling students to explore the patients’ perceived issues as they arose. Previous authors have also described the importance of the tools in the analysis of interprofessional practice (Varpio et al. 2008). In this study, leadership was intentionally not delegated, yet familiarity with the patient history software appeared to contribute to the adoption of leadership by medical students. Equal access to patient information or training on software use prior to participation would be preferred in future iterations of this work. New models of ‘leader as expert collaborator’ rather than traditional models of leadership have recently been described (Bleakley et al. 2011) although collaborative leadership appears to be difficult to achieve in practice (Lingard et al. 2012b).
The goal of collaborative care is to establish a partnership between a team of health providers and a patient in a participatory, collaborative and coordinated approach to shared decision-making around health and social issues (CIHC 2010). Through participation in student consultations, patients attending these clinics had the opportunity to both discuss their health condition and contribute meaningfully to student education. With recent calls to increase the ‘voice’ of the patient in medical education (Towle et al. 2010), interprofessional primary care student consultations, such as undertaken in this study, offer one potential avenue for useful patient engagement.
A limitation in the study was the imbalance of participants by discipline. Medical and pharmacy students were represented in most clinic consultations, but physiotherapy, nursing and occupational therapy presence was less common. More observational data on the behaviour of the less well represented disciplines would be useful to inform future educational design. Another limitation was that the primary researcher was involved in the design, observation and analysis of the interprofessional program. To minimise bias, secondary analysis of all data was conducted by another researcher without involvement in the design or observation of the IPE consultations.
This work indicates the potential value for patients and learners in the interprofessional student clinic model. Given the current momentum toward IPE implementation, further research into the learning processes and outcomes involved in complex real world interprofessional initiatives is warranted. Importantly, the role of tools such as protocols, IT systems and paperwork processes on collaborative practice requires further investigation, in both pre and postgraduate settings.
Conclusion
Primary care settings offer a promising site for interprofessional student learning. We identified two adjacent activity systems through observation of consultations. Students worked together to gather health information to determine the health care needs of the patient and patients adopted either a health consumer or student educator role. The outcome of the interspersed systems was evidence of differing priorities and values and multiple perspectives of how to manage health. Careful attention to the selection of tools that support student activities is required to maximise collaborative practice and develop opportunities for distributed leadership. The willingness of patients to engage in the education of undergraduate students suggests further active patient engagement in IPE should be considered.
References
Australian Government Productivity Commission. (2011). Caring for older Australians: Overview, report no. 53. Canberra. Retrieved December 10, 2014, from http://www.pc.gov.au/inquiries/completed/aged-care/report/aged-care-overview-booklet.pdf
Australian Medical Council. (2010). Assessment and accreditation of medical schools: Standards and procedures, 2011. Australia.
Barr, H. (2013). Toward a theoretical framework for interprofessional education. Journal of Interprofessional Care, 27(1), 4–9.
Barr (2015). Interprofessional education: The genesis of a global movement. CAIPE. Retrieved November 20, 2015, from http://caipe.org.uk/silo/files/global-ipe-2015-corrected-hb-sept–2015pdf.pdf
Bleakley, A., Bligh, J., & Browne, J. (2011). In S. Hamstra (Ed.), Medical education for the future: Identity, power and location, Advances in Medical Education series (Vol. 1). New York: Springer.
CIHC. (2010). A national interprofessional competency framework. Retrieved December 10, 2014, from http://www.cihc.ca/files/CIHC_IPCompetencies_Feb1210.pdf
Colthart, I., Bagnall, G., Evans, A., Allbutt, H., Haig, A., Illing, J., & McKinstry, B. (2008). The effectiveness of self-assessment on the identification of learner needs, learner activity, and impact on clinical practice: BEME guide no. 10. Medical Teacher, 30(2), 124–145.
EBSCO Publishing. (2014). MIMS abbreviated. NSW: St Leonards.
Engestrom, Y. (2008). From teams to knots: Activity-theoretical studies of collaboration and learning at work. Cambridge: Cambridge University Press.
Engeström, Y. (2001). Expansive learning at work: Toward an activity theoretical reconceptualization. Journal of Education and Work, 14, 133–156.
Frenk, J., Chen, L., Bhutta, Z. A., Cohen, J., Crisp, N., Evans, T., & Zurayk, H. (2010). Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. The Lancet, 376(9756), 1923–1958.
Haddara, W., & Lingard, L. (2013). Are we all on the same page? A discourse analysis of interprofessional collaboration. Academic Medicine, 88(10), 1509–1515.
Haines, T. P., Kent, F., & Keating, J. L. (2014). Interprofessional student clinics: An economic evaluation of collaborative clinical placement education. Journal of Interprofessional Care, 28(4), 292–298.
Hammick, M., Freeth, D., Koppel, I., Reeves, S., & Barr, H. (2007). A best evidence systematic review of interprofessional education: BEME guide no. 9. Medical Teacher, 29, 735–751.
Health Workforce Australia. (2011). National health workforce Innovation and reform strategic framework for action 2011–2015. Retrieved December 10, 2014, from http://www.hwa.gov.au/sites/uploads/hwa-wir-strategic-framework-for-action-201110.pdf
Holmqvist, M., Courtney, C., Meilli, R., & Dick, A. (2012). Student-run clinics: Opportunities for interprofessional education and increasing social accountability. Journal of Research in Interprofessional Practice and Education, 2, 264–277.
Kent, F., Drysdale, P., Martin, N., & Keating, J. L. (2014). The mixed discipline aged care student clinic: An authentic interprofessional learning initiative. Journal of Allied Health, 43(1), 51–56.
Kent, F., & Keating, J. (2013). Patient outcomes from a student-led interprofessional clinic in primary care. Journal of Interprofessional Care, 27(4), 336–338.
Kent, F., & Keating, J. L. (2015). Interprofessional education in primary care for entry level students—A systematic literature review. Nurse Education Today, 35(12), 1221–1231.
Lai, F., Kent, F., & Dodic, M. (2015). Student-led interprofessional clinics may improve health management in patients with chronic disease. Medical Journal Australia, 203(10), 402.
Leucht, R., Madsen, M., Taugher, M., & Petterson, B. (1990). Interprofessional education perception scale. Journal of Allied Health, 19(2), 181–191.
Lingard, L., McDougall, A., Levstik, M., Chandok, N., Spafford, M. M., & Schryer, C. (2012a). Representing compexity well: A story about teamwork, with implications for how we teach collaboration. Medical Education, 46, 869–877.
Lingard, L., Vanstone, M., Durrant, M., Fleming-Carroll, B., Lowe, M., Rashotte, J., & Tallett, S. (2012b). Conflicting messages: Examining the dynamics of leadership on interprofessional teams. Academic Medicine, 87(12), 1762–1767.
Miles, M., & Huberman, A. M. (1994). Qualitative data analysis: An expanded sourcebook (2nd ed.). Thousand Oaks: Sage Publications.
Parsell, G., & Bligh, J. (1999). The development of a questionnaire to assess the readiness of health care students for interprofessional learning (ripls). Medical Education, 33(2), 95–100.
Reeves, S., & Lewin, S. (2004). Interprofessional collaboration in the hospital: Strategies and meanings. Journal of Health Services & Research Policy, 9(4), 218–225.
Reeves, S., Perrier, L., Goldman, J., Freeth, D., & Zwarenstein, M. (2013). Interprofessional education: Effects on professional practice and healthcare outcomes (update) (review). Cochrane Database of Systematic Reviews, 3.
The Commonwealth of Australia. (2015). 2015 Intergenerational report Australia in 2055.
The Interprofessional Curriculum Renewal Consortium. (2014). Curriculum renewal for interprofessional education in health. Australia: Commonwealth of Australia, Office for Learning and Teaching.
Towle, A., Bainbridge, L., Godolphin, W., Katz, A., Kline, C., Lown, B., & Thistlethwaite, J. (2010). Active patient involvement in the education of health professionals. Medical Education, 44(1), 64–74.
Varpio, L., Hall, P., Lingard, L., & Schryer, C. F. (2008). Interprofessional communication and medical error: A reframing of research questions and approaches. Academic Medicine, 83(10 Suppl), S76–S81.
World Health Organisation. (2010). Framework for action on interprofessional education and collaborative practice. Geneva.
Acknowledgments
This project received funding from the Australian Government and the Department of Health, Victoria.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kent, F., Francis-Cracknell, A., McDonald, R. et al. How do interprofessional student teams interact in a primary care clinic? A qualitative analysis using activity theory. Adv in Health Sci Educ 21, 749–760 (2016). https://doi.org/10.1007/s10459-015-9663-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10459-015-9663-4