Abstract
Based on plastically compressed cell-seeded collagen gels, we fabricated a small-diameter tubular construct that withstands arterial pressure without prolonged culture in vitro. Specifically, to mimic the microstructure of vascular media, the cell-seeded collagen gel was uniaxially stretched prior to plastic compression to align collagen fibers and hence cells in the gel. The resulting gel sheet was then wrapped around a custom-made multi-layered braided tube to form aligned tubular constructs whereas the gel sheet prepared similarly but without uniaxial stretching formed control constructs. With the braided tube, fluid in the gel construct was further removed by vacuum suction aiming to consolidate the concentric layers of the construct. The construct was finally treated with transglutaminase. Both SEM and histology confirmed the absence of gaps in the wall of the construct. Particularly, cells in the wall of the aligned tubular construct were circumferentially aligned. The enzyme-mediated crosslinking increased burst pressure of both the constructs significantly; the extent of the increase of burst pressure for the aligned tubular construct was greater than that for the control counterpart. Increasing crosslinking left the compliance of the aligned tubular construct unchanged but reduced that of the control construct. Cells remained viable in transglutaminase-treated plastically compressed gels after 6 days in culture. This study demonstrated that by combining stretch-induced fiber alignment, plastic compression, and enzyme-mediated crosslinking, a cell-seeded collagen gel-based tubular construct with potential to be used as vascular media can be made within 3 days.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cell-seeded collagen gels, which have been identified as a promising starting material for engineering tissues,3,4,22,41 were first employed by Weinberg and Bell46 to construct a blood vessel model. The use of cell-seeded collagen gels alleviated the difficulty of homogeneous cell seeding associated with a typical tissue engineering approach. It was required, however, that a Dacron mesh be incorporated into each gel layer of the blood vessel model due to the poor mechanical strength of collagen gels.46
Many efforts have been devoted to improving the structural integrity of cell-seeded collagen gel-based tubular constructs since the seminal work of Weinberg and Bell.46 L’Heureux et al. 29 developed a tubular collagen gel construct over a central mandrel and found that at least 1 week of culture is necessary to obtain massive cell reorientation. To achieve circumferential alignment of collagen fibrils in a media-equivalent, Tranquillo et al. 44 applied a strong magnetic field during collagen fibrillogenesis when the media-equivalent was created. The mandrel compaction was later found to be necessary to keep the circumferential alignment induced by magnetic prealignment.2 Seliktar et al. 40 identified that dynamic mechanical conditioning enhances the mechanical strength and histological organization of cell-seeded collagen gel tubular constructs. Isenberg and Tranquillo24 found that at least 5 weeks of cyclic distention in culture are required for a collagen-based media-equivalent to note significant increases in both stiffness and strength. Tissue-engineered tubular constructs fabricated based on cell-seeded collagen gels generally need a significant amount of culture time before they become stable and usable.
It remains challenging to enhance the mechanical strength of cell-seeded collagen gels without prolonged culture in vitro. Chemical crosslinking can improve the mechanical strength of natural polymer-based scaffolds but commonly used reagents such as glutaraldehyde and carbodiimide are cytotoxic and cannot be used with cells. Enzyme-mediated crosslinking using transglutaminase (TGase)27,36 or lysyl oxidase10 have been shown to improve mechanical properties of cell-seeded collagen gels without compromising cell viability but it is not as effective as using the reagents. Orban et al. 36 mixed cell-suspended collagen solution with TGase to prepare a tubular construct and found that after 7 days of culture, the burst pressure of the construct is increased reaching 71 ± 4 mmHg, which is still below arterial pressure.
Plastic compression, originally defined as the irreversible expulsion of excessive fluid in collagen gels using mechanical compression,6 has been employed to rapidly enhance the mechanical strength of collagen gels for tissue engineering applications.1,6,33 Collagen gels are essentially composed of highly entangled collagen fibers and a large amount of fluid. The fluid is the result of gel casting and does not return to the network when removed. Plastically compressed gels, in a generalized sense, can be obtained by a variety of other methods including blotting, centrifugation, and osmotic pressure.8 The process is generally simple and fast and the collagen density of the resulting gel can reach those of native tissues.1,6 Specifically, Micol et al. 33 created a plastically compressed collagen gel tube by gelling cell-suspended collagen solution in a cylindrical mold and subsequently folding blotting papers around the gel tube to absorb excessive fluid. The resulting gel tube had a burst pressure of only 18.4 mmHg. Nevertheless, it took 3 weeks of culture for a non-compressed cell-seeded gel tube to reach mechanical properties comparable to a tube undergoing plastic compression.33
In this study, we fabricated a small-diameter tubular construct using plastically compressed smooth muscle cell-seeded collagen gels. Specifically, to mimic the microstructure of vascular media, the cell-seeded collagen gels were uniaxially stretched prior to plastic compression to align collagen fibers and hence cells in the gels. The plastically compressed cell-seeded gel containing aligned fibers was wrapped around a custom-made multi-layered braided tube to form the tubular construct. With the braided tube, fluid in the gel construct was further removed by vacuum suction aiming to consolidate the concentric layers of the construct. The braided tube was then removed and the tubular construct was crosslinked by TGase treatment. The effectiveness of the TGase treatment on improving the mechanical strength of the plastically compressed cell-seeded tubular construct was examined.
Materials and Methods
Materials
Collagen type I was extracted from rat tail tendons. Briefly, after dissection, rat tail tendons were dissolved in 0.5 M acetic acid solution. The solution was then centrifuged at 8000×g for 1 h at 4 °C to remove undissolved residue. NaCl was added to the supernatant bringing the solution to 1 M. After incubating overnight at 4 °C, the precipitate of the solution was collected by centrifugation and dissolved in 0.01 N HCl. The solution was then dialyzed against 0.01 N HCl solution to obtain a sterile collagen solution at 8.6 mg/mL.
Microbial TGase was isolated from Activa® TG-K (Ajinomoto, Kawasaki, Japan) as follows. The powder of Activa® TG-K (0.8 g) was dissolved in a buffer (30 mL) containing 20 mM Tris/HCl, pH 7.5, and 300 mM NaCl. Insoluble materials were removed by centrifugation at 20,000×g for 15 min at 4 °C. After centrifugation, the protein sample was concentrated and loaded onto a Sephadex S200 gel filtration column (1.6 cm × 60 cm, GE Healthcare, United Kingdom). The purified target protein (i.e., TGase) was collected and concentrated to 5 mg/mL using ultrafiltration centrifugal filters (Amicon Ultra 10 K, Merck Millipore, Germany). The final yield of pure TGase was about 4 mg from 0.8 g of the powder of Activa® TG-K.
Preparation of Cell-Seeded Collagen Gels
A smooth muscle cell line (A10, ATCC CRL-1476) was used in this study. The cells were cultured in Dulbecco’s Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum, 1% penicillin/streptomycin, and 1% gentamicin. Confluent cells were detached by 0.05% trypsin–EDTA, counted, and resuspended in culture medium at 2.78 × 105 cells/mL to be incorporated into collagen gels. Cell-suspended collagen solution was prepared according to an established method.21 Briefly, 1.2 mL of reconstituted buffer (10×) was mixed with 2.4 mL of DMEM solution (5×) and 3.74 mL of collagen solution (8.6 mg/mL), mixed thoroughly, and then neutralized by ∼ 0.35 mL of 0.1 N NaOH before adding 4.31 mL of the cell suspension. The final density of cells and of collagen were 1 × 105 cells/mL and 2.68 mg/mL, respectively. The preparation was carried out on ice to avoid premature gelation. Dumbbell-shaped cell-seeded collagen gels were formed by pouring the cell-suspended collagen solution in a mold consisting of a silicone gasket placed within a 190 × 40 (diameter × height, mm) glass Petri dish and allowing to gel at 37 °C in a humidified CO2 incubator (Fig. 1). Specifically, porous polyethylene bars (Small Parts, Miramar, FL) were positioned at both ends of the mold before adding the collagen solution so that the resulting gel can be stretched uniaxially. The silicone gasket was removed upon gel formation and the gel was cultured in 100 mL of culture media within an incubator prior to further processing.
Preparation of Cell-Seeded Collagen Gel Sheets Containing Aligned Fibers
Plastic compression was performed similarly to a previously reported method.6 Briefly, the gel to be plastically compressed was placed on a stack of layers including, from top to bottom, a non-stick polyethylene terephthalate (PET) mesh, a stainless steel mesh, and some blotting paper, covered with another PET mesh, and loaded with a glass slide for 5 min (Fig. 1). To prepare gel sheets containing aligned fibers, the gel was cultured for 1 day, then subjected to uniaxial stretching (λ = 1.2; approximately the elastic limit of the gel within which collagen fibers can be aligned by deformation), cultured under stretching for another 1 day, and finally underwent plastic compression when the gel remained stretched (Fig. 1 and Supplemental Fig. 1). The initial one-day culture strengthened the gel so that it can be stretched whereas the additional one-day culture was to allow cells in the gel to attach and spread along the fibers. To prepare gel sheets containing randomly oriented fibers, the gel simply underwent plastic compression 3 h after gelation to avoid excessive gel contraction.
Fabrication of a Cell-Seeded Collagen Gel-Based Tubular Construct
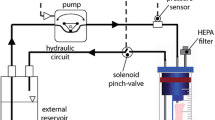
The plastically compressed gel with the porous bars removed was cut into a rectangular (40 mm × 50 mm) sheet. The gel sheet was then wrapped around a custom-made multi-layered braided tube (Fig. 1; the braided tube was fabricated by a 16-spindle braiding machine and comprised of two inner layers made of stainless steel and three outer layers of non-stick polyester. Its inner and outer diameters were 3.5 and 4.0 mm, respectively.) The fluid in the tubular construct was further removed by withdrawing air from the braided tube using a vacuum pump (Rocker 610, Rocker Scientific, Taiwan) for 1 min. Due to the mechanical support of the braided tube, the tubular construct remained intact during vacuum suction. Tubular constructs with circumferentially aligned fibers (henceforth called aligned tubular constructs) were prepared with one gel sheet containing aligned fibers whereas control constructs were prepared with one gel sheet containing randomly oriented fibers. To minimize variations due to manual fabrication, all the tubular constructs in this study were prepared by the same experienced person.
After the removal of the braided tube (it was removed by pulling its ends, thus reducing its diameter), both the tubular constructs were crosslinked by incubating in DMEM solution containing 0.05 or 0.1% w/v TGase for 1 or 2 h. The tubular construct was washed and cultured statically for 1 day before being tested for mechanical properties or processed for histology and immunohistochemistry. To compare the effects of TGase treatment with cell-mediated matrix remodeling, non-crosslinked aligned and control tubular constructs were prepared and cultured statically for 1, 3, or 6 days (n = 5 for each type of constructs and each culture duration).
Before and after removal of fluid by vacuum suction, the thickness of the tubular construct was measured using high-frequency ultrasound (lateral/axial resolution = 180/42 µm) and its volume was calculated. The collagen density was determined by dividing the dry weight of the construct by its volume. Assuming that cells had negligible weight, the dry weight of the construct was equal to the weight of collagen molecules, which was calculated based on the concentration and the volume of initial collagen solution.
Cell Viability Assay
To evaluate if the viability of cells in collagen gels was affected by plastic compression or, in particular, TGase crosslinking, the methyl thiazolyl tetrazolium (MTT) assay was performed (n = 3). Two hours after plastic compression, the cell-seeded gel was incubated in 0.05% w/v MTT in PBS solution at 37 °C for 2 h and digested in 0.1% w/v collagenase in PBS solution at 37 °C for 30 min. The solution was centrifuged, resulting in a pellet. The pellet was dissolved in dimethyl sulfoxide (DMSO). The absorbance of the DMSO solution was measured at 570 nm and normalized by that of a non-compressed control gel seeded with cells of the same batch. The viability of cells in the plastically compressed collagen gel 1 or 6 days after TGase crosslinking (0.1% for 2 h) was examined in a similar way and normalized by a non-compressed, non-crosslinked control gel seeded with cells of the same batch. All tests were performed in triplicate.
Scanning Electron Microscopy and Analysis of Distribution of Fiber Orientations
Scanning electron microscopy (SEM) was employed to examine the ultrastructure of specimens. The specimen was rinsed with PBS buffer, fixed in 2.5% glutaraldehyde solution for 1 h, rinsed again with deionized water, and then dehydrated with series alcohols. Dried specimens were sputter-coated with platinum (Sputter E-1045, Hitachi, Japan) and viewed using a scanning electron microscope (S-4100, Hitachi, Japan). To quantify the fiber orientations, images of 256 × 256 were cropped from the SEM images and analyzed by a MATLAB routine based on a fast Fourier transform algorithm for the distribution of fiber orientations.21
Histology and Immunohistochemistry
The tubular construct was fixed in 4% paraformaldehyde overnight. After standard processing, five-micron sections were cut. The sections were stained with H&E for general morphology, picrosirius red (PSR) for collagen fibers, or immunostained for N ε-(γ-glutamyl)-lysine isopeptide bonds. Specifically for immunostaining, the sections were subjected to microwave radiation in 10 mM citrate buffer, pH = 6, for antigen retrieval. After incubation with primary antibody (dilution rate: 1:50; 81D1C2, abcam, UK) for 1 h, the sections were incubated with biotinylated secondary antibody for 30 min, followed by an avidin–biotin peroxidase complex for 30 min. The sections were then incubated with DAB substrate for 3–5 min. Images were acquired by a polarized microscope (DM2500P, Leica, Germany). PSR-stained sections were imaged with either normal light or linearly polarized light.
Mechanical Testing for Tubular Constructs
The mechanical properties of the tubular construct were evaluated by conventional pressure–diameter tests23 using a custom-made mechanical tester.20 The outer diameter of the construct was recorded at the unloaded configuration (luminal pressure = ~0 mmHg and axial load = ~0 mN) and denoted as D 0. Cyclic loading and unloading pressurization was performed by infusing and withdrawing water using a syringe pump at a flow rate of 0.2 mL/min. To ensure that pressure–diameter behavior of the construct was within its elastic limit, the construct was subjected to a sequence of cyclic pressurization (bottom pressure–top pressure–bottom pressure) with an incremental increase in top pressure until either plastic deformation or failure occurred. The data from the loading portion of the pressure–diameter curve was analyzed to shed light on the mechanical properties of the construct.
The compliance of the construct was calculated using
where P 2 and D 2 are the systemic pressure and the corresponding outer diameter of the construct, respectively, and P 1 and D 1 are the diastolic pressure and the corresponding outer diameter of the construct, respectively. Herein the compliance was calculated between 30 and 70 mmHg; the 70 mmHg was chosen to ensure that the compliance of all the constructs could be calculated for comparison as the burst pressure varied among groups. The pressure–diameter curves were, in general, fairly linear before 150 mmHg; e.g., for a construct that sustained at 120 mmHg, the compliance calculated using P 2 = 120 mmHg had little difference from that calculated using P 2 = 70 mmHg.
The burst pressure and the suture retention strength of the tubular construct were examined using the same mechanical tester45 except that a 100-psi pressure transducer (Model 80A, 0–100 psi, Sensormate, Taiwan) and a 50-N load cell (MOB-10, Transducer Technique, Temecula, CA) were used because larger maximum pressure and force were expected. After the pressure–diameter testing, the burst pressure of the tubular construct was measured at an infusion rate of 0.2 mL/min. Suture retention test was performed on 20-mm long segments. A 6-O polypropylene suture connected to the load cell was placed 2 mm from one end of the segment. The other end was fixed by cannulation. The segment was stretched at an extension rate of 0.25 mm/s until the suture pulled through the tubular construct.
Statistical Analysis
Data were presented as mean ± standard deviation. Student’s t tests were used to compare the viability of cells between two groups. Differences in compliance, burst pressure, and suture retention strength between aligned and control tubular constructs subjected to different TGase treatments were examined by three-way repeated measures ANOVA with Tukey post hoc procedure. Significant levels were set at 0.05.
Results
The volume of the gel decreased from ~ 2 mL to 22.90 ± 0.33 µL (n = 3) after plastic compression. Further removal of fluid by vacuum suction reduced the volume to 17.04 ± 0.19 µL. Assuming that only fluid but not collagen molecules was removed during each process, plastic compression increased the collagen density from 2.68 to 234.36 ± 6.6 mg/mL and the density further reached 314.52 ± 6.95 mg/mL after vacuum suction.
The viability of cells in gels was slightly reduced after plastic compression (90.85 ± 3.05% relative to cells in control gels). The viability of cells in plastically compressed gels 1 day after the TGase treatment was 90.19 ± 4.23% with respect to cells in control gels; there were no significant differences between the two groups, indicating the TGase treatment caused no further damage to cells (Supplemental Fig. 2). After 6 days of culture, the viability of cells in TGase-treated plastically compressed gels was 168.10 ± 14.47% relative to cells in control gels, suggesting that cell number was significantly increased in culture.
Figure 2 illustrates the ultrastructure of acellular collagen gels, cell-seeded collagen gels before and after uniaxial stretching, and plastically compressed aligned gels. Quantification of fiber orientations within the squares in Figs. 2g and 2f are shown in Figs. 2i and 2j, respectively. The uniaxial stretching aligned effectively collagen fibers and hence cells in the gel (comparing Figs. 2e and 2f with Figs. 2c and 2d). Plastic compression condensed the gel and left the stretch-induced fiber alignment unchanged (comparing Figs. 2g and 2h with Figs. 2e and 2f). Figure 3 shows that gaps in the wall of the tubular construct were successfully removed after vacuum suction. Figure 4 illustrates the ultrastructure of the cross-sections of aligned tubular constructs before and after the TGase treatment. It appeared that collagen fibers became thicker after the TGase treatment. Particularly, the sheet-like structure between collagen fibers was observed in TGase-treated constructs but not in non-crosslinked counterparts.
Representative SEM images of acellular collagen gels (a, b); cell-seeded collagen gels (c, d); and uniaxially stretched cell-seeded collagen gels before (e, f) and after (g, h) plastic compression, and analysis of fiber orientation distribution (i, j) in the square of (g) and (f), respectively. Double arrows indicate the direction of uniaxial stretching; (b, d, f, h) show part of (a, c, e, g) in higher magnification, respectively.
Representative SEM images of cross-sections of non-crosslinked aligned tubular constructs (a, b), and cross-sections of aligned tubular constructs treated with 0.1% TGase for 2 h (c, d). Thickened fibers and sheet-like structure (arrowheads) were found in the TGase-treated construct; (b, d) show part of (a, c) in higher magnification, respectively.
Figure 5 shows the histology of aligned tubular constructs and control constructs. For both aligned and control tubular constructs, the smooth muscle cells were evenly distributed in the wall of the construct. We found that, in particular, most cell nuclei in cross-sections of aligned tubular constructs showed an elongated, bipolar shape, aligning to the circumferential direction (Fig. 5a) whereas those of control constructs showed no specific pattern (Fig. 5c). That is, cells appeared to circumferentially orient in aligned tubular constructs whereas they were more randomly oriented in control constructs. The circumferential alignment of collagen fibers in aligned tubular constructs was best demonstrated by imaging PSR-stained cross-sections under linearly polarized light. Whereas the intensity of birefringence was independent on section orientation for control constructs, the average intensity of birefringence reached the maximum when the wall of aligned tubular constructs was in parallel or perpendicular to the plane of linearly polarized light. That is, collagen fibers in aligned tubular constructs were highly aligned in the circumferential direction whereas they showed no specific orientation in control constructs. Similar to the finding of SEM, there were no obvious gaps in the wall of both aligned and control tubular constructs.
Representative H&E staining (a, d) and PSR staining (b, c, e, f) of cross-sections of aligned tubular constructs (a–c) and those of control constructs (d–f). Under linearly polarized light, the sections of both aligned and control tubular constructs were rotated on the microscope stage for the strongest (b, e) and the weakest (c, f) average intensity of birefringence. Note that the intensity was essentially independent on the section orientation for control constructs. Insets in (b) and (e) are corresponding images taken under normal light. Scale bar = 100 µm.
Figure 6 illustrates the immunohistochemistry of N ε-(γ-glutamyl)-lysine isopeptide bonds for different TGase-treated groups. The staining intensity in the wall of aligned tubular constructs was proportional to TGase concentration and reaction time.
We found that there was hysteresis between loading and unloading curves for all the tubular constructs, indicating the presence of viscous effects on the mechanical behavior. In the sequence of cyclic pressurization with incrementally increasing top pressure, each loading portion of the pressure–diameter curves consistently overlapped before the burst pressure was reached (Supplemental Fig. 3). That is, all the tubular constructs remained elastic within the burst pressure. The mean pressure–diameter curves (loading portion) of tubular constructs are illustrated in Fig. 7 (n = 5 for each group). For aligned tubular constructs, pressure–diameter curves of the TGase-treated groups showed no significant difference (Fig. 7a). For control constructs, however, pressure–diameter curves shifted noticeably to the left with increasing TGase concentration or reaction time (Fig. 7b). The compliance of control constructs was greater than that of aligned tubular constructs for each combination of TGase concentration and reaction time except for the group treated with 0.1% TGase for 2 h (Fig. 7c).
Figure 8 shows comparisons of burst pressure and suture retention strength between aligned and control tubular constructs subjected to different TGase treatments (n = 5 for each group). Upon the same treatment, the burst pressure of aligned tubular constructs was significantly greater than that of control constructs except for those treated with 0.05% TGase for 1 h. Regardless of fiber orientations, tubular constructs treated with 0.1% TGase for 2 h had significantly greater burst pressure than those subjected to other treatments. In contrast, the suture retention strength of aligned tubular constructs was significantly lower than that of control constructs. Note, however, that in suture retention testing of aligned tubular constructs, the suture did not cut through the wall of the construct. Instead, a ring-like segment always split from the construct as the construct failed. The mode of failure is likely due to the intense circumferential alignment of collagen fibers in the construct. Similarly, regardless of fiber orientations, the groups treated with 0.1% TGase for 2 h had significantly greater suture retention strength.
Non-crosslinked aligned and control tubular constructs were cultured statically for 3 and 6 days to compare with their TGase-treated counterparts. For both the non-crosslinked constructs, burst pressure and suture retention strength were increased with increasing culture duration (Fig. 9). The increases of both properties might be attributed to cell-mediated matrix remodeling as the two properties of accellular tubular constructs were found unchanged after 6 days in culture (data not shown). Similar to the findings of TGase-treated counterparts, pressure–diameter curves of non-crosslinked control constructs shifted to the left with increasing culture duration whereas no significant difference was found in pressure–diameter curves between non-crosslinked aligned tubular constructs cultured for 3 and 6 days (Fig. 9).
Mean pressure–diameter data of non-crosslinked aligned tubular constructs statically cultured for 3 or 6 days (a) and non-crosslinked control constructs statically cultured for 3 or 6 days (b). Comparisons of burst pressure (c) and suture retention strength (d) among static culture groups (n = 5). Note that both aligned tubular constructs and control constructs that were cultured statically for 1 day were too fragile for the suture retention test. * denotes p < 0.05 and ** denotes p < 0.001. Data are presented as mean ± SD.
Discussion
Natural polymers such as collagen and fibrin have been intensively used for developing tissue-engineered vascular grafts. Their initial poor mechanical strength, in general, requires a significant amount of culture time for them to mature and become usable.
Plastic compression can rapidly boost the mechanical strength of collagen gels and creates many new opportunities for collagen gel-based tissue-engineered constructs. Nevertheless, the existence of gaps at the contact interface between plastically compressed collagen gels was identified as a problem for their applications.6,15 Vacuum suction along with the use of the braided tube appeared to consolidate the original layered structure successfully. The subsequent TGase treatment could thus crosslink collagen fibers more effectively throughout the thickness of the wall. Although we did not characterize the interface integration caused by vacuum section, the tubular constructs actually could not hold pressure in mechanical testing if they were not subjected to vacuum suction prior to the TGase treatment (data not shown), indicating the significant role of the vacuum suction in the successful fabrication of the tubular construct.
To the best of our knowledge, currently all plastically compressed collagen gels are structurally and mechanically isotropic, which certainly limits their applications. In this study, structurally anisotropic gel sheets were prepared according to our previous findings.21 The gel sheet was wrapped to form a tubular construct that has circumferentially oriented microstructure. The anisotropic gel sheets can potentially be utilized to create other desired microstructure of tissue-engineered constructs. Note that dynamic mechanical stimulation was employed in preparing structurally and mechanically anisotropic engineered tissues.11,13,28,35 For example, Gauvin et al. 13 used a self-assembly approach (i.e., with no scaffolding) to produce engineered tissue sheets and demonstrated that dynamic mechanical stimulation led to the establishment of anisotropy of the sheet.
Given the circumferentially oriented microstructure, the consolidated wall, and the significantly increased collagen density, it was surprising that the burst pressure of non-crosslinked aligned tubular constructs was not significantly improved. The poor burst pressure of non-crosslinked aligned tubular constructs was consistent with the findings of Micol et al. 33 The TGase treatment was therefore attempted aiming to form chemical bonds among the condensed collagen fibers. Indeed, with proper TGase treatment, the burst pressure increased significantly to up to 380 mmHg. The results emphasized the important role of chemical crosslinking in the mechanical enhancement of plastically compressed collagen gels. Mi et al. 32 combined plastic compression and photochemical crosslinking to enhance the mechanical strength of acellular collagen gels. Note that their plastically compressed gels were not strong enough for suturing until photochemical crosslinking.
While previous research reported that TGase treatment increases the mechanical strength of collagen gels, TGase in these studies was, in fact, mixed with collagen solution prior to gelation.18,27,36 In this study, the TGase treatment was performed separately after gel formation and plastic compression. In our pilot study, we found surprisingly that if the TGase treatment was applied to a non-compressed collagen gel, the mechanical strength of the gel would not be significantly enhanced. The improved mechanical behaviors of plastically compressed tubular constructs due to the TGase treatment might be attributed to the chemical crosslinking of a large amount of fiber-to-fiber interlocking resulted from plastic compression.
It seemed that the TGase treatment affected the compliance of aligned and control tubular constructs to different extents, suggesting a combined effect of fiber alignment and crosslinking on the stiffness of the gel (see Supplemental Fig. 4 for an illustrating example). For specimens containing randomly oriented fibers, the fibers tend to re-orient upon uniaxial stretching. If these specimens have more crosslinks (red dots in Supplemental Fig. 4), they would undergo less extension than those with fewer crosslinks when subjected to the same stress because the crosslinks restrict fiber re-orientation. For specimens containing aligned fibers, however, there is less fiber re-orientation during deformation; recall that these specimens are stiffer in nature. Specifically, because of intrinsically fewer fiber interactions in this case, the stiffness of the specimens may be less influenced by the number of crosslinks.
The viability of cells in collagen gels after plastic compression was about 90% relative to the control, which is consistent with a previous study.6 Plastic compression reduces the water content of collagen gels, which increases matrix stiffness and ligand density of the gel. Although we did not investigate other cellular changes caused by plastic compression, numerous studies showed that matrix stiffness affected cell phenotype,7,17,37 proliferation,5,16 and mobility.17,30 It seemed that the TGase treatment did not to affect the viability of cells in plastically compressed collagen gels. TGase catalyzes the formation of covalent bonds that increase proteolytic and mechanical stability of collagen gels. The tubular constructs, after crosslinking, were washed thoroughly to remove/dilute any residual TGase within the gel. TGase crosslinking was found to be benign to cells12,36; note, again, that in these studies TGase was added to cell-suspended collagen solution prior to gelation. More importantly, MTT results of gels cultured statically for 6 days demonstrated that the combination of plastic compression and TGase crosslinking did not affect cell proliferation in the gels.
Many studies have reported that plastic compression improved significantly both stiffness and mechanical strength of collagen gels.1,6,14,33 In the tensile testing of these studies, however, gels were stretched to failure and elastic characteristics of the gel were seldom evaluated. That is, the extent to which the gel remains elastic was not determined. Even though physical bonds between collagen fibers are increased after plastic compression, these bonds are essentially non-covalent. When overstretched, plastically compressed collagen gels may exhibit significant plastic behavior similar to conventional collagen gels.22 In this study, we employed cyclic pressurization to examine the mechanical properties of tubular constructs; in particular, the top pressure in cyclic pressurization was gradually increased to ensure that the tubular construct returned to the original shape upon unloading; i.e., underwent elastic (reversible) deformation.
Using a method similar to the present approach, Ghezzi et al. 14 fabricated tubular constructs with plastically compressed collagen gel sheets. The burst pressure and the suture retention strength of their tubular constructs exceeded 1000 mmHg and 100 g-f, respectively; both are significantly greater than those of our constructs. Ghezzi et al. 14 used ultimate tensile strength from a ring test to estimate burst pressure according to Laplace’s law; this approach may have resulted in an overestimation of burst pressure.25 Particularly, before the gel ring reached its ultimate tensile strength, the microstructure of the ring might have been damaged; the damaged microstructure, if occurred in tubular constructs, could have led to water leakage. The determination of suture retention strength, on the other hand, depends on parameters such as suture size, wall thickness, and extension rate,34,38 which may explain the discrepancy. In addition, NIH 3T3 fibroblasts used in their study are superior to A10 smooth muscle cells in terms of cell proliferation and matrix production. Note, however, that Micol et al. 33 used a different method to make plastically compressed collagen gel tubes and none of their high-density collagen gel tubes could sustain the tension of a suture thread.
The enhancement in burst pressure due to the circumferentially aligned fibers, unfortunately, came along with reduced compliance. That is, the circumferentially aligned fibers inevitably compromised the compliance of aligned tubular constructs. The almost straight collagen fibers found in most tubular constructs (data not shown) also intensified the poor compliance. Collagen fibers in the body are typically undulated or crimped in the unloaded configuration; the undulated fibers straighten upon loading acting as a shock damper. It has been shown that collagen fiber undulation in engineered tissues can be induced by cellular contraction19; therefore, the prolonged culture in vitro may still be required if the development of undulated collagen fibers is desired. Nevertheless, the lack of highly stretchable, elastic components such as elastin in the tubular construct inherently limited its distensibility and compliance. Note that at low pressure the passive elastic response of native arteries is determined by elastic fibers and that undulated collagen fibers are not loaded until higher pressure. This issue may be addressed by incorporating elastin or other elastin-like protein polymers (e.g., the one developed by Sallach et al. 39) into the tubular construct or replacing collagen gels with fibrin gels. Fibrin gels, instead of collagen gels, was found to support substantial elastogenesis by smooth muscle cells.31 The latter approach again requires prolonged culture in vitro. Although the compliance of aligned tubular constructs (2.86 ± 0.53%/100 mmHg; calculated for the whole group with n = 15) was significantly lower than that of the human internal mammary artery (11.5 ± 3.9%/100 mmHg25), it is close to the compliance of the human saphenous vein (3.4 ± 2.0%/100 mmHg42) and many other tissue-engineered vascular grafts.9,26,43
The poor suture retention strength of the tubular construct constitutes a major drawback of the current approach. The suture retention strength of either TGase-treated aligned tubular constructs or control constructs was less than 10 g-f, which is obviously insufficient for surgical procedures. Nevertheless, the way by which aligned tubular constructs failed in suture retention tests suggested an imbalance of its mechanical strength in the circumferential and the axial directions. In our previous study, a tubular construct comprising double helically arranged fiber pattern was successfully fabricated by wrapping axisymmetric electrospun membranes around a mandrel and both circumferential and axial stiffness of the tubular construct could be manipulated by varying the pitch angle of the helices.20 The suture retention strength of the tubular construct may be improved by enhancing its mechanical strength in the axial direction using the same idea. The lack of suture retention strength may also be resolved by adding a suturable outer layer surrounding the tubular construct42,47; the layer may as well act as a protective sheath to prevent over-dilation of the construct.
Conclusion
We started the construction of the tubular construct by wrapping plastically compressed cell-seeded collagen gels on the custom-made braided tube. Specifically, the cell-seeded collagen gel was stretched uniaxially before plastic compression so that the resulting tubular construct had circumferentially oriented microstructure. The use of the braided tube allowed vacuum suction to be applied to the construct, which not only further removed fluid in the construct but also consolidated the concentric layers of the construct. The burst pressure of the construct, however, was not greatly improved until the TGase treatment, which, when applied after plastic compression, appeared to form a significant number of irreversible, chemical bonds between fibers. Cells remained viable in transglutaminase-treated plastically compressed gels after 6 days in culture. By combining stretch-induced fiber alignment, plastic compression, and enzyme-mediated crosslinking, we successfully fabricated a cell-seeded collagen gel-based small-diameter tubular construct that withstands arterial pressure within 3 days. The tubular construct will prove useful in building a tissue-engineered vascular graft.
References
Abou Neel, E. A., U. Cheema, J. C. Knowles, R. A. Brown, and S. N. Nazhat. Use of multiple unconfined compression for control of collagen gel scaffold density and mechanical properties. Soft Matter 2:986–992, 2006.
Barocas, V. H., T. S. Girton, and R. T. Tranquillo. Engineered alignment in media equivalents: magnetic prealignment and Mandrel compaction. J. Biomech. Eng. Trans. ASME 120:660–666, 1998.
Bell, E., H. P. Ehrlich, D. J. Buttle, and T. Nakatsuji. Living tissue formed in vitro and accepted as skin-equivalent tissue of full thickness. Science 211:1052–1054, 1981.
Bell, E., B. Ivarsson, and C. Merrill. Production of a tissue-like structure by contraction of collagen lattices by human fibroblasts of different proliferative potential in vitro. Proc. Natl. Acad. Sci. U.S.A. 76:1274–1278, 1979.
Bott, K., Z. Upton, K. Schrobback, M. Ehrbar, J. A. Hubbell, M. P. Lutolf, and S. C. Rizzi. The effect of matrix characteristics on fibroblast proliferation in 3D gels. Biomaterials 31:8454–8464, 2010.
Brown, R. A., M. Wiseman, C. B. Chuo, U. Cheema, and S. N. Nazhat. Ultrarapid engineering of biomimetic materials and tissues: fabrication of nano- and microstructures by plastic compression. Adv. Funct. Mater. 15:1762–1770, 2005.
Chaudhuri, O., S. T. Koshy, C. B. da Cunha, J. W. Shin, C. S. Verbeke, K. H. Allison, and D. J. Mooney. Extracellular matrix stiffness and composition jointly regulate the induction of malignant phenotypes in mammary epithelium. Nat. Mater. 13:970–978, 2014.
Cheema, U., and R. A. Brown. Rapid fabrication of living tissue models by collagen plastic compression: understanding three-dimensional cell matrix repair. Adv. Wound Care (New Rochelle) 2:176–184, 2013.
Dahl, S. L. M., C. Rhim, Y. C. Song, and L. E. Niklason. Mechanical properties and compositions of tissue engineered and native arteries. Ann. Biomed. Eng. 35:348–355, 2007.
Elbjeirami, W. M., E. O. Yonter, B. C. Starcher, and J. L. West. Enhancing mechanical properties of tissue-engineered constructs via lysyl oxidase crosslinking activity. J. Biomed. Mater. Res. A 66A:513–521, 2003.
Engelmayr, G. C., D. K. Hildebrand, F. W. H. Sutherland, J. E. Mayer, and M. S. Sacks. A novel bioreactor for the dynamic flexural stimulation of tissue engineered heart valve biomaterials. Biomaterials 24:2523–2532, 2003.
Garcia, Y., R. Collighan, M. Griffin, and A. Pandit. Assessment of cell viability in a three-dimensional enzymatically cross-linked collagen scaffold. J. Mater. Sci. Mater. Med. 18:1991–2001, 2007.
Gauvin, R., R. Parenteau-Bareil, D. Larouche, H. Marcoux, F. Bisson, A. Bonnet, F. A. Auger, S. Bolduc, and L. Germain. Dynamic mechanical stimulations induce anisotropy and improve the tensile properties of engineered tissues produced without exogenous scaffolding. Acta Biomater. 7:3294–3301, 2011.
Ghezzi, C. E., B. Marelli, N. Muja, and S. N. Nazhat. Immediate production of a tubular dense collagen construct with bioinspired mechanical properties. Acta Biomater. 8:1813–1825, 2012.
Hadjipanayi, E., R. A. Brown, and V. Mudera. Interface integration of layered cottagen scaffolds with defined matrix stiffness: implications for sheet-based tissue engineering. J. Tissue Eng Regen. Med. 3:230–241, 2009.
Hadjipanayi, E., V. Mudera, and R. A. Brown. Close dependence of fibroblast proliferation on collagen scaffold matrix stiffness. J. Tissue Eng Regen. Med. 3:77–84, 2009.
Hadjipanayi, E., V. Mudera, and R. A. Brown. Guiding cell migration in 3D: a collagen matrix with graded directional stiffness. Cell Motil. Cytoskelet. 66:121–128, 2009.
O’Halloran, D. M., J. C. Russell, M. Griffin, and A. S. Pandit. Characterization of a microbial transglutaminase cross-linked type II collagen scaffold. Tissue Eng. 12:1467–1474, 2006.
Herchenhan, A., N. S. Kalson, D. F. Holmes, P. Hill, K. E. Kadler, and L. Margetts. Tenocyte contraction induces crimp formation in tendon-like tissue. Biomech. Model. Mechanobiol. 11:449–459, 2012.
Hu, J. J., W. C. Chao, P. Y. Lee, and C. H. Huang. Construction and characterization of an electrospun tubular scaffold for small-diameter tissue-engineered vascular grafts: a scaffold membrane approach. J. Mech. Behav. Biomed. Mater. 13:140–155, 2012.
Hu, J. J., J. D. Humphrey, and A. T. Yeh. Characterization of engineered tissue development under biaxial stretch using nonlinear optical microscopy. Tissue Eng. A 15:1553–1564, 2009.
Huang, D., T. R. Chang, A. Aggarwal, R. C. Lee, and H. P. Ehrlich. Mechanisms and dynamics of mechanical strengthening in ligament-equivalent fibroblast-populated collagen matrices. Ann. Biomed. Eng. 21:289–305, 1993.
Humphrey, J. D. Cardiovascular solid mechanics: cells, tissues, and organs. New York: Springer, p. xvi, 2002; (757 p).
Isenberg, B. C., and R. T. Tranquillo. Long-term cyclic distention enhances the mechanical properties of collagen-based media-equivalents. Ann. Biomed. Eng. 31:937–949, 2003.
Konig, G., T. N. McAllister, N. Dusserre, S. A. Garrido, C. Iyican, A. Marini, A. Fiorillo, H. Avila, W. Wystrychowski, K. Zagalski, M. Maruszewski, A. L. Jones, L. Cierpka, L. M. de la Fuente, and N. L’Heureux. Mechanical properties of completely autologous human tissue engineered blood vessels compared to human saphenous vein and mammary artery. Biomaterials 30:1542–1550, 2009.
Kumar, V. A., J. M. Caves, C. A. Haller, E. B. Dai, L. Y. Liu, S. Grainger, and E. L. Chaikof. Acellular vascular grafts generated from collagen and elastin analogs. Acta Biomater. 9:8067–8074, 2013.
Lee, P. F., Y. Bai, R. L. Smith, K. J. Bayless, and A. T. Yeh. Angiogenic responses are enhanced in mechanically and microscopically characterized, microbial transglutaminase crosslinked collagen matrices with increased stiffness. Acta Biomater. 9:7178–7190, 2013.
Lee, E. J., J. W. Holmes, and K. D. Costa. Remodeling of engineered tissue anisotropy in response to altered loading conditions. Ann. Biomed. Eng. 36:1322–1334, 2008.
L’Heureux, N., L. Germain, R. Labbe, and F. A. Auger. In vitro construction of a human blood vessel from cultured vascular cells: a morphologic study. J. Vasc. Surg. 17:499–509, 1993.
Lo, C. M., H. B. Wang, M. Dembo, and Y. L. Wang. Cell movement is guided by the rigidity of the substrate. Biophys. J . 79:144–152, 2000.
Long, J. L., and R. T. Tranquillo. Elastic fiber production in cardiovascular tissue-equivalents. Matrix Biol. 22:339–350, 2003.
Mi, S. L., V. V. Khutoryanskiy, R. R. Jones, X. P. Zhu, I. W. Hamley, and C. J. Connon. Photochemical cross-linking of plastically compressed collagen gel produces an optimal scaffold for corneal tissue engineering. J. Biomed. Mater. Res. A 99:1–8, 2011.
Micol, L. A., M. Ananta, E. M. Engelhardt, V. C. Mudera, R. A. Brown, J. A. Hubbell, and P. Frey. High-density collagen gel tubes as a matrix for primary human bladder smooth muscle cells. Biomaterials 32:1543–1548, 2011.
Mohammadi, H., P. D. Arora, C. A. Simmons, P. A. Janmey, and C. A. McCulloch. Inelastic behaviour of collagen networks in cell-matrix interactions and mechanosensation. J. R. Soc. Interface 12:20141074, 2015.
Mol, A., N. J. B. Driessen, M. C. M. Rutten, S. P. Hoerstrup, C. V. C. Bouten, and F. P. T. Baaijens. Tissue engineering of human heart valve leaflets: a novel bioreactor for a strain-based conditioning approach. Ann. Biomed. Eng. 33:1778–1788, 2005.
Orban, J. M., L. B. Wilson, J. A. Kofroth, M. S. El-Kurdi, T. M. Maul, and D. A. Vorp. Crosslinking of collagen gels by transglutaminase. J. Biomed. Mater. Res. A 68:756–762, 2004.
Paszek, M. J., N. Zahir, K. R. Johnson, J. N. Lakins, G. I. Rozenberg, A. Gefen, C. A. Reinhart-King, S. S. Margulies, M. Dembo, D. Boettiger, D. A. Hammer, and V. M. Weaver. Tensional homeostasis and the malignant phenotype. Cancer Cell 8:241–254, 2005.
Roh, J. D., G. N. Nelson, M. P. Brennan, T. L. Mirensky, T. Yi, T. F. Hazlett, G. Tellides, A. J. Sinusas, J. S. Pober, W. M. Saltzman, T. R. Kyriakides, and C. K. Breuer. Small-diameter biodegradable scaffolds for functional vascular tissue engineering in the mouse model. Biomaterials 29:1454–1463, 2008.
Sallach, R. E., W. Cui, J. Wen, A. Martinez, V. P. Conticello, and E. L. Chaikof. Elastin-mimetic protein polymers capable of physical and chemical crosslinking. Biomaterials 30:409–422, 2009.
Seliktar, D., R. A. Black, R. P. Vito, and R. M. Nerem. Dynamic mechanical conditioning of collagen-gel blood vessel constructs induces remodeling in vitro. Ann. Biomed. Eng. 28:351–362, 2000.
Shi, Y. L., and I. Vesely. Fabrication of mitral valve chordae by directed collagen gel shrinkage. Tissue Eng. 9:1233–1242, 2003.
Soletti, L., Y. Hong, J. Guan, J. J. Stankus, M. S. El-Kurdi, W. R. Wagner, and D. A. Vorp. A bilayered elastomeric scaffold for tissue engineering of small diameter vascular grafts. Acta Biomater. 6:110–122, 2010.
Syedain, Z. H., L. A. Meier, J. W. Bjork, A. Lee, and R. T. Tranquillo. Implantable arterial grafts from human fibroblasts and fibrin using a multi-graft pulsed flow-stretch bioreactor with noninvasive strength monitoring. Biomaterials 32:714–722, 2011.
Tranquillo, R. T., T. S. Girton, B. A. Bromberek, T. G. Triebes, and D. L. Mooradian. Magnetically orientated tissue-equivalent tubes: application to a circumferentially orientated media-equivalent. Biomaterials 17:349–357, 1996.
Tuan-Mu, H. Y., C. H. Yu, and J. J. Hu. On the decellularization of fresh or frozen human umbilical arteries: implications for small-diameter tissue engineered vascular grafts. Ann. Biomed. Eng. 42:1305–1318, 2014.
Weinberg, C. B., and E. Bell. A blood-vessel model constructed from collagen and cultured vascular cells. Science 231:397–400, 1986.
Wu, W., R. A. Allen, and Y. D. Wang. Fast-degrading elastomer enables rapid remodeling of a cell-free synthetic graft into a neoartery. Nat. Med. 18:1148–1153, 2012.
Acknowledgment
Financial supports from the National Science Council (NSC102-2221-E-006-028) and the National Health Research Institute (NHRI-EX103-10217EC) in Taiwan are gratefully acknowledged.
Conflict of Interest
The author declares that he have no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Kent Leach oversaw the review of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tuan-Mu, HY., Lu, PC., Lee, PY. et al. Rapid Fabrication of a Cell-Seeded Collagen Gel-Based Tubular Construct that Withstands Arterial Pressure. Ann Biomed Eng 44, 3384–3397 (2016). https://doi.org/10.1007/s10439-016-1645-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-016-1645-z