Abstract
Patient-specific biomechanical properties of the human cornea are rarely used with finite elements analysis. In order for that to be possible, a proper formulation for biomechanical properties that is based on patient-specific measurable values must be used. In this study, we propose a formula that simulates hyperelastic stress–strain curves based on non-invasive clinical measurements that can be acquired in vivo. These consist of, but are not limited to, center corneal thickness and center corneal curvature as well as corneal resistance factor and applanation diameter that are measured during non-contact tonometry. The presented formulation was demonstrated and validated through several computer simulations. First, mean values that were reported in literature were inputted into the formula to simulate a curve that represents a healthy case. This case was compared to two independent in vitro studies. Then, a sensitivity analysis was carried to identify inputs that have the most dominant effect. Finally, a finite element analysis simulating elevations in intraocular pressure was conducted; the corneal model comprised of patient-specific corneal geometry that was measured in vivo in our clinic as well as the current formulation for patient-specific corneal biomechanics. “Strong” and “weak” corneal tissue cases were simulated and deformations as well as instantaneous curvature optical maps were derived. Results for the simulated healthy curve showed good agreement with the in vitro studies. The sensitivity analysis found the corneal resistance factor and applanation diameter to have the most dominant influence. The finite element analysis of strong and weak biomechanical properties resulted in corneal deformations and instantaneous curvature optical maps that are common for healthy and pathological conditions respectively. In conclusion, the presented modeling technique can be used to assess corneal biomechanics in vivo and therefor may enhance follow-up on the effectiveness of clinical treatments, rehabilitation of vision and perhaps improve the diagnosis of pathologies that are related to corneal biomechanics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The human eyeball is an imperfect sphere, with the cornea forming the transparent outer covering of the visible colored portion of the eyeball. Patient-specific morphology of the cornea can be captured using medical devices such as standard pachymeters, corneal topographers and tomographers. In general, healthy corneas are commonly characterized by a radius of curvature of 7.86 mm ± 0.26 mm (mean ± standard deviation) and 0.52 mm ± 0.04 mm thickness in the center region.34
Patient-specific finite element models (FEM) that rely on in vivo geometrical data of the cornea have been previously published.8,36 These aid tremendously in shedding light on the underlying mechanisms of corneal pathologies however, they do not account for patient-specific biomechanical properties. This would require a FEM-compatible formulation that is based on patient-specific in vivo measurable values.
A useful method for evaluating patient-specific corneal rigidity in vivo was introduced with the Reichert’s Ocular response analyzer (ORA; Reichert Ophthalmic Instruments, Buffalo, NY). This commercially available clinical instrument has been proposed to characterize corneal biomechanical responses using the noncontact tonometry process. The corneal resistance factor (CRF) value is proposed for representing the cumulative effects of both the viscous and elastic resistance of the cornea during applanation tonometry.25,28
The CRF alone gives a limited insight into patient-specific corneal biomechanics. In particular soft biological tissues such as the cornea typically exhibit highly nonlinear-elastic behavior under large deformations, due to rearrangements in the microstructure.32 Accurate simulations of these nonlinear large-strain effects hence require the use of constitutive models formulated within the framework of hyperelasticity.15,20,32,41
This study combines the CRF with several additional patient-specific non-invasive in vivo measurements in a mathematical formulation that produces FEM-compatible hyperelastic stress–strain curves.4,39 Connected to other studies in our group which aimed at pushing biomechanical modeling out of the research laboratories and into the clinics, the formulation is then integrated into a patient-specific case FEM to produce simulated optical power maps in response to increased IOP.35
Methods
The theoretical framework assumes a linear relationship between the cornea’s elasticity (C) and IOP (Eq. (1a))6,27,31 which essentially follows the assumption of hyperelastic mechanical behavior (otherwise known as a strain-stiffening behavior) for the corneal tissue.
where m is the proportionality factor. Since Eq. (1a) intersects at zero modulus—zero pressure, it must become increasingly inaccurate as the IOP decreases. This is because the cornea is expected to demonstrate a mechanical behavior of an elastic solid, at least to some extent, regardless of the applied pressure (i.e., its elasticity, a material property, cannot approach zero).6 Thus, the coefficient, E 0, which denotes a baseline modulus of elasticity for near-zero IOP was added to the right hand-side of Eq. (1a). The resulting Eq. (1b) has been previously experimentally validated by closely fitting results of in vitro inflation tests.10
We start by deriving a mathematical expression for a hyperelastic stress–strain curve based on Eq. (1b). Consecutively, analytical formulations for the scalars m and E 0 will be developed.
Hyperelastic Stress–Strain Relationship
A relationship between uniform internal pressure that is applied on the inner surface of a sphere and the resulting meridional stress could be derived by computing the equilibrium of forces.23,43
where S m(MPa) is the meridional stress component of the 2nd Piola Kirhoff stress tensor and IOP(mmHg) is converted to units of MPa by factoring 7501(MPa/mmHg). CCT(mm) and CCR(mm) are the center corneal thickness and center corneal radius respectively. The equation holds for \(\frac{\text{CCR}}{\text{CCT}} > 10\).
Substituting Eq. (2) into Eq. (1b) gives:
where C m represents the meridional elasticity component of the elasticity tensor and a is a non-dimensional patient-specific property determined by the scalar m and the individual’s corneal geometry. Recall that for a hyperelastic material, there exists a strain energy density function U so that for the meridional strain component of the Green–Lagrange strain tensor E m, \(C_{m} = \frac{{\partial^{2} U}}{{\partial E_{m}^{2} }}\) and \(S_{m} = \frac{\partial U}{{\partial E_{m} }}\) we can obtain:
Considering \(S\left( {E = 0} \right) = \frac{\partial U}{\partial E}\left( {E = 0} \right) = 0\) as a boundary condition (see Appendix for a non-zero boundary condition) and solving the above differential equation provides the explicit form of U which could be used to obtain Eq. (5).
Many commercially available non-invasive medical devices can measure the cornea’s geometrical properties directly (e.g., standard pachymeters, corneal topographers and tomographers) by implementing a quick and simple procedure.3,33,42 This facilitates acquiring the CCT, CCR and patient-specific corneal topography, however, this is not the case for the scalars m and E 0 and to the authors’ current knowledge they cannot be measured directly with any existing device. Therefore, mathematical relationships between each of these parameters and current clinically-available measurements were derived.
Analytical Formulation for the Proportionality Factor
Adjustments are made to the Orssengo and Pye’s formulation (Eq. (6.1)) for the corneal modulus of elasticity.31
where E(MPa) is the linear-elastic modulus of elasticity, IOPG(mmHg) is the IOP measured with a Goldmann’s tonometer, IOPT(mmHg) is the true IOP and α and β are dimensionless constants that are defined by CCT(mm), CCR(mm), v (Poisson’s ratio) and the applanation area during tonometry (an explicit presentation of α and β is provided in the Appendix).
Rewrite Eq. (6.1) to obtain the difference equation:
The proportionality factor m is defined as:
Replacing the numerator (in Eq. (7.1)) with the derived expression for ΔE (Eq. (6.2)) and defining \(\tau \equiv \frac{{\Delta {\text{IOPG}}}}{{\Delta {\text{IOPT}}}}\) for simplicity results in:
A proposed procedure for acquiring a patient-specific τ value might be to measure the true IOP as well as the Goldmann’s IOP while using IOP regulating medicine for continuously lowering the IOP. However, two major drawbacks are identified for such a process. The first is that the Goldmann’s tonometer suffers from relatively large measuring errors. The second drawback is that as a matter of fact that the most valid method to measure the true IOP is by using an invasive manometer, which involves connecting a cannula inserted into the anterior chamber of the eye to a column of fluid.11,24 Perhaps a patient-specific τ could be obtained during surgical procedures that involve inserting a cannula and following the procedure proposed above. However, in the reasonable case that an invasive maneuver is undesirable, we propose a generalized m value that is physiological and can be used within this modeling. For that matter, let us make an observation that τ represents the correlation between the Goldmann’s IOP and the true IOP. This correlation between applanation tonometry and direct intracameral IOP readings was previously measured in vivo and is equal to τ = 0.78.11 Due to the fact that the CCT and CCR were not reported in the referenced study we use a set of nominal geometry values termed as the “calibration values” of human CCT (0.52 mm) and CCR (7.8 mm) 9 to go with the reported τ when assessing the value of m. These values are not to be confused with the patient-specific CCT and CCR and are merely used herein to represent the values of those whom participated in the referenced study. It is common to refer to the corneal tissue as a nearly incompressible material and therefore the Poisson’s ratio was set here to ν = 0.49.5,27 The applanation surface was set to the Goldmann’s tonometer surface area \(({\text{Area}} = 7.35\;{\text{mm}}^{2} )\).31 Resulting m = 0.0115 MPa/mmHg will be used throughout this study.
The implications of using a constant value for m for achieving a non-invasive evaluation of the individual’s corneal tissue stiffness will be discussed later. It is also noteworthy that though m is assessed in the linear-elastic region, it is a scalar that may be inputted into the large deformation stress–strain Eq. (5) to define the value of a.
Analytical Formulation for the Baseline Elastic Modulus
Assuming again that \(\frac{\text{CCR}}{\text{CCT}} > 10\) and that deformations due to edge supports or membrane stress remote from the loading are disregarded, the central deflection of the cornea due to external loading can be calculated as follows27,31,43:
where F is the acting load, \(\delta ({\text{mm}})\) is the deflection under the area where the load is applied and E is the elastic modulus of the corneal tissue. A(μ) is an approximated geometrical coefficient (for further details please see the Appendix).
Rearranging the formula for the elastic modulus E and writing F in terms of pressure P (mmHg) acting on an area gives:
Equation (9) infers that if a known pressure is applied on the center of the cornea over a known applanation area and the corneal deflection is assessed or measured as well, it is possible to calculate the elastic modulus of the cornea.
A diversity of indirect IOP measurements can be obtained using various devices, the gold standard being the Goldmann’s applanation tonometry. These measurements all share the property of being inaccurate to some extent due to the transcorneal measurement.7 Therefore, a non-invasive exact value of the true IOP is not available and the absolute pressure P that represents the fraction of the total pressure that is needed in order to oppose the elastic resistance during applanation, cannot be calculated using a true IOP. The CRF(mmHg) is a measurement of the cumulative effects of both the viscous and elastic resistance encountered by the air jet while deforming the corneal surface and importantly, is minimally correlated with IOP.25,28 It therefor provides a good assessment of the absolute pressure P that is needed in order to oppose the elastic resistance during applanation.
Consider that for normal physiological IOP where linear elasticity applies, E is approximately E 0 6 and let CRF represent the pressure needed to oppose both the viscous and elastic resistance Eq. (9) becomes:
where E 0 is the elastic modulus for IOP ≌ 0 mmHg. The effects of the viscous element of the CRF in this formulation will be discussed later on.
Corneal deflection was calculated analytically using Eq. (11) which is based on a Pythagorean derivation.31 Novel emerging tonometers, such as the Corvis (Corvis ST, Oculus, Wetziar, Germany) can measure the patient-specific AD as well as δ during tonometry.
It is noteworthy that though E 0 is assessed in the linear-elastic region, like m it too is a scalar that may be inputted into the large deformation stress–strain Eq. (5).
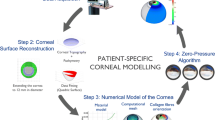
Protocol of Simulations
The presented formulation was demonstrated and validated through computer simulations using MATLAB (2013a, The MathWorks) and FEbio (Ver. 1.5.1, University of Utah). First, mean values that were reported in literature were inputted into the formula to produce a curve which represents a healthy case. This case was compared to in vitro results from two independent studies. Then, a sensitivity analysis was carried to identify inputs that have the most dominant effect. Finally, a finite elements analysis (FEA) simulating elevations in intraocular pressure was conducted. In this analysis the corneal model comprised of patient-specific corneal geometry as well as the current formulation for patient-specific corneal biomechanics. Healthy and pathological corneal biomechanics were simulated and deformations as well as instantaneous curvature optical maps were derived. The following sections describe in detail the methods that were used.
Healthy-Simulated Curve
A simulated curve representing a healthy case was plotted using the calibration values of human \({\text{CCT}} (0.52\;{\text{mm)}}\) and CCR \((7.8\; {\text{mm)}}\) 9 along with the Goldmann’s AD (\(3.06\;{\text{mm}}\)) and reported mean CRF value (\(10.46\; {\text{mmHg}}\)) for normal corneas.24
To confirm the resulting curve with respect to experimental data, the resulted curve was plotted along with a scatter with margins plot which was recreated from empirical data that were published in two independent in vitro studies.40,44
This curve was used as a reference curve during the sensitivity analysis and therefore is termed as the “reference simulation” in the following.
Sensitivity Analysis and Keratoconus-Simulated Curve
Sensitivity analysis was carried by varying one parameter at a time (from the set CCT, CCR, AD and CRF) while holding the other three constant. The ranges of all values were defined to include the scope of healthy and pathological values. The range of values for CCT and CCR was set to be \(\pm 10\%\) of the calibration values and the range of values for AP was 0.5–3.4 mm. CRF values ranged between 6 mmHg and 15 mmHg.24
A curve simulating keratoconus (a pathology that is thought to be related to degradation in corneal biomechanics) was plotted using values that are in range with reported keratoconus cases21,37,38 and are often measured by the clinician co-authors in patients with keratoconus (CCT = 0.45 mm, CCR = 8.6 mm, AP = 3.4 mm and CRF = 5 mmHg).
Finite Element Analysis
The data acquisition was approved by the Institutional Ethics Committee at the Tel Aviv Sourasky Medical Center (approval no. 0266-10-TLV) and the chosen subject was a healthy 30 year old male.
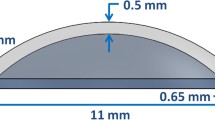
The patient-specific geometry was optically scanned in vivo using the GALILEI™ Dual Scheimpflug Analyzer (Ziemer Group; Port, Switzerland). The geometrical data was imported into Matlab from two separate files, each containing one surface of the cornea on an 8 mm diameter domain. The sampled points from both surfaces were assembled together and anatomically extrapolated to produce a point cloud file of the cornea-sclera on a 14 mm diameter domain. This was done by controlling the pachymetry to a maximum of 1 mm thickness and bounding the angle of extrapolation to a 2.4 mm maximal height.8 The result was converted into STL format using ADINA (ADINA Inc., Watertown, MA, USA) and loaded as such into the Simpleware finite element suit (Simpleware Ltd, Ver. 2012, Exeter, UK). The STL data was sampled with a 20 μm spaced grid and the resulting mask was partitioned into two separate parts; the cornea on 11.89 mm domain (patient-specific white to white—WTW) and the sclera completing the domain up to 14 mm (Fig. 1).
Schematic representation of the BCs and loads working on the patient-specific cornea. The WTW domain is 11.89 mm (colored in blue) and the sclera (colored in grey) completes the domain up to 14 mm. The model was clamped at the scleral circumference and the anterior surface of the sclera was constrained to sliding. IOP varied between 5 and 20 mmHg and was applied on the posterior surface
Mesh density was set based on the implementation of the instantaneous curvature algorithm on the nodes of the anterior surface of the cornea post-deformation (as explained later on). The mesh was generated semi-automatically, eventually comprising of 1646875 4-node tetrahedron elements. In terms of numerical convergence or accuracy, using greater mesh densities did not provide any benefit (resulted in less than 1% difference in strain data for denser meshes in preliminary analysis).
Using our formulation, two stress–strain curves were simulated to represent “strong” and “weak” cases of corneal tissue; the values that were used in each case are provided in Table 1. The CCT (0.58 mm), CCR (8 mm) and IOP (13 mmHg) values were measured patient-specifically in the clinic while the AD and CRF values were varied to signify the strong and weak corneal tissue cases.
Both curves were evaluated as uniaxial stretch test data using Abaqus (Simulia Inc, Providence, RI) to calculate the constants of a third-order Ogden strain energy function. The sclera was modeled as a linear elastic material with a modulus of elasticity of 2.35 MPa.21
The boundary conditions (BC) were set as fixed along the rim of the sclera and only sliding was allowed on the anterior surface of the sclera. Elevations in IOP (5, 10, 15 and 20 mmHg) were prescribed by setting an acting pressure on the posterior surface of the cornea and sclera (Fig. 1).
The FE simulations were all set up and pre-processed using PreView (Ver. 1.8), analyzed using the Pardiso linear solver of FEBio in structural mechanics mode, and post-processed using PostView (Ver. 1.4).29 The runtime of each case was approximately one hour using a 64-bit Windows 7-based workstation with a CPU comprising Intel Xeon E5645 2.4 GHz (2 processors), and 32 Gb of RAM.
A file was created recording the nodal displacements per each step in the analysis until the full extent of deformation was achieved for each elevation in IOP. These were used in order to present deformations by means of instantaneous curvature maps that are commonly used by ophthalmologists for identifying and describing corneal pathologies. In order to do so, the file with the nodal displacements was loaded into Matlab. The nodes, represented by Cartesian coordinates were first transformed into cylindrical coordinates. Then, all nodes were sorted and quantized into 360°. Multiple range values for single domain points were averaged, resulting in unique values along a given radius. Finally, for each degree, the values along the radii were interpolated along a 0.1 mm spaced line domain. The instantaneous curvature was calculated along each radius using Eq. (12). The algorithm was tested successfully by inputting a known 7 mm radius hemisphere, resulting in a maximal deviation of ±1 μm. In addition, the instantaneous curvature map that was exported from the GALILEI was compared to the zero pressure maps that were created using this algorithm resulting in variations of several microns at maximum.
Results
Analysis of Formulation
The simulated stress–strain curve for the healthy case is presented in Fig. 2 by a solid line along with a scatter with margins plot of the in vitro experimental data. The simulated stress–strain curve for the keratoconus case is also presented in this figure by a dashed line.
The stress–strain curve for the reference simulation is presented by a solid line along with a scatter with margins plot that was recreated using empirical data that were published in two independent in vitro studies.40,44 The stress–strain curve for the keratoconus simulation is marked by a dashed line and is significantly more compliant than the reference curve
The solid curve is well within the boundaries of the experimental data for up to roughly 35% strains. Increased stiffening (elevation in the rate of change in slope), relative to the experimental data, is noticeable at approximately 30% strains. It is clear that for the keratoconus simulation the stiffness is reduced considerably in the entire domain.
The CCT and CCR were varied separately between 0.45–0.6 (mm) and 7–8.6 (mm) respectively while the remaining parameters were held as same as in the reference simulation. Comparing to the reference simulation up to approximately 25% strains, changes in both CCT and CCR had a minor effect (less than a 1% maximal change) on the resulting stress–strain curve. For larger strains, elevations in CCT resulted in mild stiffening while in contrast decreasing the CCR resulted in mild weakening. The latter having a least dominant effect on the simulated curves.
The AD was varied between 0.5 and 3.4 mm while the remaining parameters were held as in the reference simulation (Fig. 3). It is evident that a shorter AD (dotted line) results in stiffer curves.
The CRF was varied between 6 and 15 mmHg24 while the remaining parameters were held as same as in the reference simulation (Fig. 4). It is evident that low values of CRF (dotted line) result in a more compliant curve.
Unlike the minor influence the geometrical parameters exhibited, changes in both AD and CRF resulted in a noticeable linear change across the entire strain domain. The latter having a more dominant effect on the simulated curves.
Finite Element Analysis
The total displacements for the set of “strong” biomechanical properties under 10 mmHg are presented in Fig. 5. As expected, because the cornea is thinnest at its center and thickens towards the limbus and sclera in a relatively symmetrical fashion, a relative symmetry in deformations is observed. It is obvious that small asymmetrical changes are barely, if at all, noticeable in such presentation.
The maximal tissue displacement for both strong and weak biomechanical properties is presented in Fig. 6. The strong case presents a 15 μm elevation per 5 mmHg. The origin and slop of the weak case are higher than those observed for the strong case. For increasing elevations in IOP a growing difference between both cases is evident. At 20 mmHg the weak case suggests a 42% increase relative to the strong case in terms of maximal tissue displacement of the cornea.
This is accommodated by increased change in the instantaneous curvature power maps as could be observed in Fig. 7. Compared to the instantaneous curvature that is associated with the time of measurement it is evident that under elevations in IOP both the strong and the weak cases show elevations in diopters. Under 10 mmHg and 20 mmHg increases in IOP, the weak case shows a substantial increase in diopters compared to the strong case. The highest diopter values are observed in the inferior part of the cornea. The maximal dioptric power [D] for both strong and weak cases is presented in Fig. 8. The origin and slop of the weak case are higher than those observed in the strong case and a growing difference between both cases is evident under elevations in IOP. Values are summarized in Table 2.
Instantaneous curvature maps for strong and weak biomechanical properties under a 10 and 20 mmHg increase in IOP were produced post analysis using the anterior surface of the cornea FEM. The orientation is noted by the Nasal–Temporal and Superior–Inferior directions. Warm colors depict high dioptric values. Higher values of optical power were observed with the weak case compared to the strong one
The strong case remains under a 1 diopter elevation even for a 20 mmHg increase in IOP while the weak case passes this value after a little less than a 10 mmHg increase in IOP.
Discussion
The present formulation is suitable for implementation in medical devices (e.g., corneal topographers or applanation tomographers) so that it can be used directly in the clinic for evaluating patients. Most importantly, the biomechanical formulation can be integrated with FEM to show the patient-specific response to an increase in IOP in terms of deformations and optical power. Ultimately, our modeling can be used for quick follow-ups of changes in the cornea’s biomechanical properties by clinicians (since it weighs the multiple parameters measured by their different medical devices into a single graph with a functional meaning), and thus, it can aid in the prognosis of corneal diseases and responses to preventative and rehabilitating treatments.
The reference simulation curve (Fig. 2) demonstrates important properties that are expected from a hyperelastic material in general, and from the cornea in particular. First, a gradual increase in slope (i.e., tangential modulus of elasticity) relates to the stiffening effect that occurs when the cornea is subjected to increasing strains. Second, the curve resembles linear elasticity (R 2 = 0.98) for up to 2–3% strains however, it is clear that our formulation can account for large strains which complies with the current convention.10,32,36
The healthy biomechanics curve was compared with two in vitro experimental results; the first recreated dataset was up to 14% strains40 while the second dataset completed the strain domain for up to 40% strains.44 An excessive magnitude of change for the maximum/minimum value of a changed variable can indicate that the model is oversensitive to that parameter. During the sensitivity analysis, when the input variables (CCT, CCR, AD and CRF) were modified, the resulting curves remained inside the ranges of the error margins of the experimental data. In particular, the reference curve nearly passes through the mean values up to 30% strains and then rises gradually until passing above the upper error margin at around 35% strains. This gradual stiffening compared to the in vitro data could be explained by the high strain rate that is applied when measuring the CRF.28 Nevertheless, very high strains have little biological relevance, because they represent stresses that are much greater than naturally seen.5 Therefore, our formulation very nicely agrees with published empirical data within the entire domain of physiologically-relevant corneal strains, including large strains.
The simulated keratoconus curve (Fig. 2) resulted in a severe decrease in stiffness. This is in agreement with the known decrease in stiffness that characterizes keratoconus.16 The result shows that the keratoconic cornea allows very large deformations for relatively low stress values, which supports the notion that these cases are more susceptible to a peak increase in IOP. For example, eye rubbing is associated with peaks in IOP and is a risk factor that is recognized by clinicians and explained by them to keratoconus patients. Patients are encouraged to avoid eye rubbing, assuming this could delay or arrest progression of the disease.22
The sensitivity analysis points at only a minor contribution of the CCT and CCR to simulated curves whereas AD and CRF were shown to have a more dominant effect. A stiffer cornea would be more resistant to the applied force and therefore would deform less during applanation than a more compliant one. Accordingly, smaller values for the inputted AD resulted in a stiffer curve whereas a large diameter gave a more compliant curve (Fig. 3). It has been previously shown that low CRF values correspond with a lower viscoelastic resistance of the corneal tissue to the air pulse during non-contact tonometry.25,28 An air pulse of increasing force is directed onto the eye, lasting approximately 20 ms and causing progressive corneal deformation through two applanation phases; an inward applanation state to indentation followed by an outward applanation as the cornea returns to its original shape. The air pulse force is noted at the two points of corneal flattening and is later used to calculate the aforementioned CRF. This value represents the cumulative effects of both the viscous and elastic resistance encountered by the air jet while deforming the corneal surface.25,28 In accordance, low CRF values resulted in a more compliant curve, while high values resulted in a stiffer curve (Fig. 4). The fact that the CRF is minimally correlated with IOP implies that changes in IOP will have a minimal effect on the measured CRF. To the authors’ knowledge the CRF has yet been compared with traditional mechanical variables; our formulation for calculating E 0 provides a useful and practical method for integrating the CRF in biomechanical analysis and so forth harnesses its in vivo indication of corneal rigidity.
The strong case in Fig. 6 presents a 15 μm elevation per 5 mmHg which agrees with previously published results that indicate that an IOP change of 1 mmHg causes an elevation of 3 μm to the center of the cornea.26 From both Figs. 6 and 8 it is clear that the weak case exhibits more maximal tissue displacement and maximal dioptric power with respect to the strong case. Figure 7 shows the results as they might be presented in a clinical environment; as instantaneous curvature maps. Based on these results clinicians may decide to prescribe IOP lowering medications to a patient with maps such as those that were obtained in the weak case which clearly demonstrates a pathological dioptric map. The importance of using the instantaneous curvature maps is emphasized by Fig. 5; deformations alone cannot depict the small changes that occur in the corneal topography though these have severe implications on vision as demonstrated with the instantaneous curvature maps.
Among the CRF are additional in vivo methods that can indicate changes in corneal biomechanics. Examples are dynamic corneal imaging and ultrasonic spectroscopy. The latter can measure an aggregated modulus and the former can be used to measure values such as flexing curve or when used with ultra high-speed Scheimpflug imaging can measure changes in deformations that have been shown to correlate with corneal stiffness.2,17,19 All of these parameters share two common attributes; the first is that they offer measures that although have a correlation with corneal biomechanics they cannot be directly used in a classic mechanical analysis and therefore require additional research in order to implement with FEM. The second is that they give an indication of corneal biomechanics at the time of measurement alone and refer to the cornea as a linear elastic material. In oppose to these methods our current modeling characterizes the corneal biomechanics as hyperelastic, promotes integration with FEM and ultimately also allows simulations in silico such as increases in IOP which were presented herein.
Simplifications and analytical and numerical approximations that were made during the development of this formulation should be considered. Although the cornea is not a perfect symmetrical sphere, the equations that were used represent one. The cornea is non-homogenous, is not isotropic and does not have constant pachymetry but is treated as such in our formulation for practicality and ease of implementation and interpretation.1,18,20,32 True IOP measurements are not mandatory thanks to the mathematical maneuver presented for obtaining m. The fact that the calculated value agrees nicely with the experimental results is encouraging. In addition, other parameters that were varied produced significant changes in stiffness that agreed with the experimental data. Nonetheless, further investigation into the relationship between IOPT and IOPG is required in order to establish if the proposed calculated value for m can be fixed for clinical use. The formulation holds in both cases, whether a fixed value is chosen or not. The patient-specific values that are used with this formulation represent the entire cornea however they are measured only in the center of the cornea. However, this may be beneficial considering that in pathological cases such as keratoconus, the center region of the cornea is where these variables remain accurate during in vivo measurements. The term A(μ) imposes limitations on the range of values of CCT, CCR and AD that can be inserted into the formulation. However, the range of inputs that are permitted include severe pathological conditions and therefore this does not impose any clinical limitations (for the analysis and values please see the appendix).12–14,30,38
Further improvements to this model may include adding orthotropic characteristics of the cornea in order to provide a more complete representation of corneal biomechanics. In the present framework it would be straight forward to do so by adding fiber elements in reinforced directions. These mainly consist of a gradual increase in circumferential fibers towards the limbus and reinforcing fibers along the superior–inferior and nasal–temporal meridians with a sinusoidal fashioned density distribution as reported in literature [8, 11]. The present modeling, if adapted to account for orthotropic reinforcement, may also be valuable for anticipating the patient-specific biomechanical limits of safe rehabilitating refractive surgery, in order to avoid unexpected iatrogenic keratoectatic catastrophic results.
To conclude, this paper provides a formulation for acquiring patient-specific corneal biomehcanics. The present mathematical formulation can be implemented and used in ophthalmological devices as well as for educational purposes. It can further be coupled with structural computational and particularly FEA, and should be useful for quick follow-ups of changes in the cornea’s biomechanical properties, rendering it extremely useful for physicians to illustrate how degenerative changes affect corneal stiffness. The large range of potential applications provides clinicians, researchers, medical educators and students a novel tool for representing and studying patient-specific corneal biomechanics.
References
Aghamohammadzadeh, H., R. H. Newton, and K. M. Meek. X-ray scattering used to map the preferred collagen orientation in the human cornea and limbus. Structure 12:249–256, 2004.
Ambrósio, Jr., R., I. Ramos, A. Luz, F. C. Faria, A. Steinmueller, M. Krug, M. W. Belin, and C. J. Roberts. Dynamic ultra high speed Scheimpflug imaging for assessing corneal biomechanical properties. Rev. Bras. Oftalmol. 72:99–102, 2013.
Aramberri, J., L. Araiz, A. Garcia, I. Illarramendi, J. Olmos, I. Oyanarte, A. Romay, and I. Vigara. Dual versus single Scheimpflug camera for anterior segment analysis: Precision and agreement. J. Cataract Refract. Surg. 38:1934–1949, 2012.
Asher, R., A. Gefen, and D. Varssano. In: Patient-Specific Modeling in Tomorrow’s Medicine, edited by A. Gefen. Berlin: Springer, 2012, Vol. 09, pp. 461–483.
Buzard, K. Introduction to biomechanics of the cornea. Refract. Corneal Surg. 8:127, 1992.
Chihara, E. Major review. Surv. Ophthalmol. 53:203–218, 2008.
Cook, J. A., A. P. Botello, A. Elders, A. Fathi Ali, A. Azuara-Blanco, C. Fraser, K. McCormack, and J. Margaret Burr. Systematic review of the agreement of tonometers with Goldmann applanation tonometry. Ophthalmology 119:1552–1557, 2012.
Deenadayalu, C., B. Mobasher, S. D. Rajan, and G. W. Hall. Refractive change induced by the LASIK flap in a biomechanical finite element model. J. Refract. Surg. 22:286, 2006.
Ehlers, N., T. Bramsen, and S. Sperling. Applanation tonometry and central corneal thickness. Acta Ophthalmol. Suppl. 53:34–43, 1975.
Elsheikh, A., D. Wang, and D. Pye. Determination of the modulus of elasticity of the human cornea. J. Refract. Surg. (Thorofare, NJ: 1995), 23:808, 2007.
Feltgen, N., D. Leifert, and J. Funk. Correlation between central corneal thickness, applanation tonometry, and direct intracameral IOP readings. Br. J. Ophthalmol. 85:85–87, 2001.
Fontes, B. M., R. Ambrósio, D. Jardim, G. C. Velarde, and W. Nosé. Corneal biomechanical metrics and anterior segment parameters in mild keratoconus. Ophthalmology 117:673–679, 2010.
Franco, S., and M. Lira. Biomechanical properties of the cornea measured by the Ocular Response Analyzer and their association with intraocular pressure and the central corneal curvature. Clin. Exp. Optom. 92:469–475, 2009.
Galletti, J., T. Pförtner, and F. Bonthoux. Improved keratoconus detection by ocular response analyzer testing after consideration of corneal thickness as a confounding factor. J. Refract. Surg. (Thorofare, NJ: 1995), 28:202–208, 2012.
Gasser, T. C., R. W. Ogden, and G. A. Holzapfel. Hyperelastic modelling of arterial layers with distributed collagen fibre orientations. J. R. Soc. Interface 3:15–35, 2006.
Gefen, A., R. Shalom, D. Elad, and Y. Mandel. Biomechanical analysis of the keratoconic cornea. J. Mech. Behav. Biomed. Mater. 2:224–236, 2009.
Grabner, G., R. Eilmsteiner, C. Steindl, J. Ruckhofer, R. Mattioli, and W. Husinsky. Dynamic corneal imaging. J. Cataract Refract. Surg. 31:163–174, 2005.
Grytz, R., and G. Meschke. A computational remodeling approach to predict the physiological architecture of the collagen fibril network in corneo-scleral shells. Biomech. Model. Mechanobiol. 9:225–235, 2010.
He, X., and J. Liu. A quantitative ultrasonic spectroscopy method for noninvasive determination of corneal biomechanical properties. Invest. Ophthalmol. Vis. Sci. 50:5148–5154, 2009.
Holzapfel, G. A., T. C. Gasser, and R. W. Ogden. A new constitutive framework for arterial wall mechanics and a comparative study of material models. J. Elast. 61:1–48, 2000.
Jordan, C. A., A. Zamri, C. Wheeldon, D. V. Patel, R. Johnson, and C. N. McGhee. Computerized corneal tomography and associated features in a large New Zealand keratoconic population. J. Cataract Refract. Surg. 37:1493–1501, 2011.
Karseras, A. G., and M. Ruben. Aetiology of keratoconus. Brit. J. Ophthalmol. 60:522–525, 1976.
Kling, S., L. Remon, A. Pérez-Escudero, J. Merayo-Lloves, and S. Marcos. Corneal biomechanical changes after collagen cross-linking from porcine eye inflation experiments. Invest. Ophthalmol. Vis. Sci. 51:3961–3968, 2010.
Kniestedt, C., O. Punjabi, S. Lin, and R. L. Stamper. Tonometry through the ages. Surv. Ophthalmol. 53:568–591, 2008.
Lau, W., and D. Pye. A clinical description of Ocular Response Analyzer measurements. Invest. Ophthalmol. Vis. Sci. 52:2911–2916, 2011.
Leonardi, M., P. Leuenberger, D. Bertrand, A. Bertsch, and P. Renaud. First steps toward noninvasive intraocular pressure monitoring with a sensing contact lens. Invest. Ophthalmol. Vis. Sci. 45:3113–3117, 2004.
Liu, J., and C. J. Roberts. Influence of corneal biomechanical properties on intraocular pressure measurement: quantitative analysis. J. Cataract Refract. Surg. 31:146–155, 2005.
Luce, D. A. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J. Cataract Refract. Surg. 31:156–162, 2005.
Maas, S. A., B. J. Ellis, G. A. Ateshian, and J. A. Weiss. FEBio: finite elements for biomechanics. J. Biomech. Eng. 134, 2012.
Miháltz, K., I. Kovács, Á. Takács, and Z. Z. Nagy. Evaluation of keratometric, pachymetric, and elevation parameters of keratoconic corneas with pentacam. Cornea 28:976, 2009.
Orssengo, G. J., and D. C. Pye. Determination of the true intraocular pressure and modulus of elasticity of the human cornea in vivo. Bull. Math. Biol. 61:551–572, 1999.
Pandolfi, A., and F. Manganiello. A model for the human cornea: constitutive formulation and numerical analysis. Biomech. Model. Mechanobiol. 5:237–246, 2006.
Park, S.-H., S.-K. Choi, D. Lee, E.-J. Jun, and J.-H. Kim. Corneal thickness measurement using orbscan, pentacam, galilei, and ultrasound in normal and post-femtosecond laser in situ keratomileusis eyes. Cornea 31:978–982, 2012.
Pinsky, P. M., and D. V. Datye. A microstructurally-based finite element model of the incised human cornea. J. Biomech. 24:907–922, 1991.
Portnoy, S., N. Vuillerme, Y. Payan, and A. Gefen. Clinically oriented real-time monitoring of the individual’s risk for deep tissue injury. Med. Biol. Eng. Comput. 49:473–483, 2011.
Roy, A. S., and W. J. Dupps, Jr. Patient-specific modeling of corneal refractive surgery outcomes and inverse estimation of elastic property changes. J. Biomech. Eng. 133:011002, 2011.
Szalai, E., A. Berta, Z. Hassan, and L. Módis. Reliability and repeatability of swept-source Fourier-domain optical coherence tomography and Scheimpflug imaging in keratoconus. J. Cataract. Refract. Surg. 2012.
Uçakhan, Ö. Ö., V. Çetinkor, M. Özkan, and A. Kanpolat. Evaluation of Scheimpflug imaging parameters in subclinical keratoconus, keratoconus, and normal eyes. J. Cataract Refract. Surg. 37:1116–1124, 2011.
Varssano, D., R. Asher, and A. Gefen. Biomechanical modeling of the human eye with a focus on the cornea. In: Multi-Modality State-of-the-Art: Human Eye Imaging and Modeling, edited by E. Y. K. Ng. Boca Raton, FL: CRC Press. ISBN 9781439869932.
Wollensak, G., E. Spoerl, and T. Seiler. Stress-strain measurements of human and porcine corneas after riboflavin–ultraviolet-A-induced cross-linking. J. Cataract Refract. Surg. 29:1780–1785, 2003.
Woo, S.-Y., A. Kobayashi, W. Schlegel, and C. Lawrence. Nonlinear material properties of intact cornea and sclera. Exp. Eye Res. 14:29–39, 1972.
Yeter, V., B. Sönmez, and U. Beden. Comparison of central corneal thickness measurements by Galilei Dual-Scheimpflug analyzer® and ultrasound pachymeter in myopic eyes. Ophthalmic Surg. Lasers Imaging 43:128–134, 2012.
Young, W. C., and R. G. Budynas. Roark’s Formulas for Stress and Strain. New York: McGraw-Hill, 2002.
Zeng, Y., J. Yang, K. Huang, Z. Lee, and X. Lee. A comparison of biomechanical properties between human and porcine cornea. J. Biomech. 34:533–537, 2001.
Acknowledgments
This study was partially supported by a Grant from the Tel Aviv Sourasky Medical Center Research Foundation (A. G., D. V.).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Sigal Portnoy oversaw the review of this article.
Appendix
Appendix
Expansion of Eq. (4) to Include IOP0 (IOP at Time of Measurement)
Solving the differential Eq. (4) using non-homogenous boundary conditions results in:
Note that Eq. (13) becomes Eq. (5) by zeroing IOP0
Use Eq. (2) to give the residual stress for measured IOP0
An Explicit Definition of α and β
An Explicit Definition for A(μ)
A(μ) is a geometrical coefficient that was approximated using Taylor’s approximation as follows5,35:
(for 0 < μ < 1.4)
where \(\mu = \frac{AD}{2}\left[ {\frac{{12\left( {1 - \nu^{2} } \right)}}{{\left( {R - \frac{t}{2}} \right)^{2} \cdot t^{2} }}} \right]^{0.25}\) (AD is in our case the applanation diameter).
Limitations Imposed by A(μ)
Special attention was given to the Taylor’s approximation, in order to clarify the constraints it imposes on the model. For that matter, a simulation was carried in order to show the dependency of \(A(\mu )\) on the range of possible inputs (CCT, CCR and AD). In each analysis (Figs. 9a, 9b and 9c) the horizontal dashed lines depict where the approximation limits are. Passing these margins will add a growing approximation error to the results. The CCT, CCR and AD were varied between 0.34–0.65 mm, 6–9 mm and 0.5–4 mm respectively. These ranges were chosen in order to cover a very wide of possible inputs, including very extreme pathological conditions.12–14,30,38
In each simulation the horizontal dashed lines depict where the approximation limits are. Passing these margins will add a growing error to the results. The CCT, CCR and applanation diameter were varied between 0.34–0.65 mm, 6–9 mm and 0.5–4 mm respectively. These ranges were chosen in order to cover a very wide of possible inputs, including very extreme pathological conditions12–14,30,38
The asterisk in Fig. 9 marks the values of the reference simulation (Fig. 2). Low CCT and CCR values move the asterisk towards lower A(μ) values. In contrast, low AD values move the asterisk upwards towards higher A(μ) values. The resulting lower limit for the CCT (Fig. 9a) is 0.4 mm and there is no upper limit. The CCR (Fig. 9b) has a lower limit of 6.1 mm and no upper limit as well. A(μ) is inside the boundaries for applanation diameters that are up to 3.5 mm and has no lower limit (Fig. 9c).
Rights and permissions
About this article
Cite this article
Asher, R., Gefen, A., Moisseiev, E. et al. An Analytical Approach to Corneal Mechanics for Determining Practical, Clinically-Meaningful Patient-Specific Tissue Mechanical Properties in the Rehabilitation of Vision. Ann Biomed Eng 43, 274–286 (2015). https://doi.org/10.1007/s10439-014-1147-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-014-1147-9