Abstract
Aim
To investigate the association between smoking, environmental tobacco smoke (ETS), and lung cancer risk.
Methods
This case–control study included 1622 newly diagnosed cases of lung cancer and 1622 healthy frequency-, age-, and gender-matched control participants. Epidemiological data were collected by in-person interviews using a standard questionnaire.
Results
Smoking was a risk factor for lung cancer in men (odds ratio (OR) = 4.486, 95% confidence interval (95%CI) 3.586–5.611). In addition, decreased starting age, increased number of cigarettes smoked per day, duration of smoking, pack–years, and depth of inhalation were all risk factors that met the dose–response relationship (P < 0.001). The risk of lung cancer was lower among men who had quit smoking for more than 10 years compared to current smokers. Additionally, male smokers with lung squamous cell carcinoma were at a higher risk of lung cancer than male smokers with lung adenocarcinoma. Workplace ETS increased the risk for lung cancer for male nonsmokers (OR = 2.452, 95%CI 1.534–3.920). In contrast, household ETS increased the risk for lung cancer for female nonsmokers (OR = 2.224, 95%CI 1.644–3.009). Approximately 65.93% cases of lung cancer in men could be attributed to smoking, whereas approximately 31.03% cases of lung cancer among nonsmokers could be attributed to ETS.
Conclusions
Smoking is the main risk factor for lung cancer. Workplace ETS is associated with increased lung cancer risk in male nonsmokers, while household ETS is associated with increased lung cancer risk in nonsmoking women. Thus, smoking and ETS increase the risk of lung cancer and are major public health concerns.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the most common cancer worldwide. Global cancer statistics (GLOBOCAN 2020) released by the International Agency for Research on Cancer in 2020 revealed that of the newly confirmed cases of cancer, lung cancer contributed to the second ratio (11.4%) and ranked first (18.0%) among malignant tumor-related deaths (Sung et al. 2021). In China, the rate of morbidity associated with lung cancer is increasing annually (Chen et al. 2016) and also currently ranks first among malignant tumors (Feng et al. 2019). According to the 2020 China Cancer Registration Annual Report, there are approximately 800,000 new cases of lung cancers and 1800,000 related deaths annually, and the burden of disease has increased in severity. A similar trend has been observed in the Fujian Province of China (Cao et al. 2020). In particular, in the Fujian Province, lung cancer is the most common cause of malignant cancers in males, and lung cancer and its associated mortality has drastically increased to the highest among all malignant cancers for females (Xiao et al. 2015).
Lung cancer is a multistage, complex disease with a multifactorial etiology, among which smoking remains a primary risk factor (Kim et al. 2014a; López-Campos et al. 2018; Wang et al. 2015b). The Chinese population has a high smoking rate and a low smoking–quitting rate. The male and female smoking rates are 68% and 3.2%, respectively, while the general smoking–quitting rate is <10% (Chen et al. 2015); therefore, the smoking control status does not appear promising. In particular, the indoor smoking rate in China is approximately 70%. Nearly 740,000,000 people are exposed to environmental tobacco smoke (ETS), which is one of the major risk factors for lung cancer (WHO. 2015). The strength of association between smoking and different pathological patterns of lung cancer differ. For instance, smoking is closely related to lung squamous cell carcinoma but is not as strongly associated with lung adenocarcinoma (Houston et al. 2014). In recent years, the pathological pattern of patients with lung cancer has changed. The rate of lung adenocarcinoma has increased, while the rate of lung squamous cell carcinoma has declined annually. These differences could possibly be related to the change in the types of cigarettes smoked. While the smoking rate among Chinese women has declined (Chen et al. 2015), the morbidity and mortality rates of women with lung cancer remain high, which may be closely related to ETS.
Currently, very little research exists regarding the association between smoking, ETS, population attributable risk, and changes in the pathological pattern of lung cancer. We used a hospital-based case–control study and took stratification quantitative analysis by gender and smoking status to investigate the relationship between smoking, passive smoking, and lung cancer in the Fujian population. Moreover, this study provides a scientific basis for carrying out targeted lung cancer prevention work and population smoking cessation, with important public health significance.
Methods
Study participants
This is a hospital-based, case–control study conducted across three hospitals in Fujian Province, China. Between January 2006 and July 2015, patients from the Department of Thoracic Surgery and Respiratory Medicine of the First Affiliated Hospital of Fujian Medical University, Affiliated Union Hospital of Fujian Medical University, and Fujian General Hospital of Nanjing Military Region who had been newly diagnosed with primary lung cancer, as confirmed by a fiber bronchoscope or histology, were recruited to the study. Patients with lung inflammation, benign lesion, secondary lung cancer, and critical illness, and who were incapable of clearly answering questions were excluded from the study. Based on gender and age (± 2), patients were subjected to frequency matching. At the same time, healthy people who visit patients in non-cancer departments of the hospital, as well as individuals from the general community population, were selected for the control group. Patients who had chronic respiratory disease were excluded from participation. A total of 1622 cases of lung cancer and 1622 healthy control participants were used in this study. This study protocol was approved by the Ethics Committee of Fujian Medical University, and all participants signed informed consent before the start of the survey (Code: [2014] (98)).
Survey content and variable definition
All research participants were surveyed using a structural questionnaire, and interviews were conducted by trained investigators. The survey was used to collect information including general condition, smoking history, passive smoking history, alcohol drinking history, tea drinking history, pulmonary disease history, occupational exposure to hazardous substances, and family history of cancer.
Body mass index (BMI) was calculated by dividing body weight (kg) by the square of the body height (m). The Chinese standard for BMI was used: very low weight: < 18.5 kg/m2; normal weight: 18.5–24.0 kg/m2; and overweight or obese: ≥ 24.0 kg/m2. Smoking was defined if participants reported to have smoked a total of at least 100 cigarettes in their lifetime. The packs–year of cigarettes smoked was calculated as the number of cigarette pieces smoked every day/20 × smoking years. Individuals were considered to have quit smoking if they were currently not smoking and had stopped smoking for over three months. ETS was defined as a nonsmoker who inhaled smoke generated by either a burning cigarette or exhaled by another smoker for at least one day (for more than 15 min/day) per week. Passive smoking index was defined as the passive smoking dose in a household (the number of years of ETS exposure from each smoking family member) + passive smoking dose in the workplace (years from which the participant was exposed to ambient ETS from smokers when engaging in work). Drinking alcohol was defined as drinking any type of alcoholic drink at least once per week for at least six months, excluding drinking on holidays and festivals. Drinking tea was defined as drinking at least one cup of tea per week for at least six months. A family history of cancer was considered when any genetically related individuals such as parents, siblings, children, grandparents, maternal grandparents, uncles, and aunts, had suffered from malignant tumors. The occupational hazardous substance included any kinds of physical, chemical, and biological factors.
Statistical analysis
Equilibrium of the case and control groups was tested by the χ2 test. Odds ratio (OR), 95% confidence interval (95%CI), and the population attributable risk proportion (PAR%) of each research variable were calculated by applying stratification analysis using binary or multi-classification unconditional logistic regression model after adjusting for possible confounding factors. PAR% = (Pe (OR–1))/(Pe (OR–1) + 1) × 100%. PAR% reflects the influence of exposure on population incidence and shows the ratio of incidence of a certain disease caused by certain exposure, and it is the ratio reduced in the disease incidence when assuming this exposure is removed. Multiplicative and additive interaction analysis and joint action analysis were used in the current study. The relative excess risk of interaction (RERI), attributable proportion of interaction (API), synergy index (S), and their 95%CI were used to evaluate the additive interaction. Because this was a case–control study, OR was replaced for risk ratio (RR). RERI=OR11–OR01–OR10 + 1, API = RERI/OR11 and S = (OR11–1)/ [(OR01–1) + (OR10–1)]. If there is no additive interaction between the two factors, the CI of the RERI and AP contains 0 and the CI of S should contain 1.
Analyses were carried out using SPSS 22.0 software. All P values were based on a two-sided test; and the α level was set at 0.05.
Results
Baseline characteristics
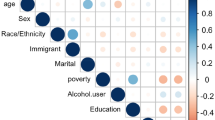
We included 1622 cases and 1622 controls in the present study. The average ages of the case and control groups were 59.14 ± 10.61 and 59.11 ± 10.56 years (t = 0.075; P = 0.940), respectively. The distribution of age, gender, nationality, and marital status did not significantly differ between the case and control groups (P > 0.05). However, educational background, BMI, history of drinking alcohol, drinking tea, pulmonary disease, occupational exposure to hazardous substances, and family history of cancer significantly differed between the two groups (P < 0.05) (Table 1).
Relationship between smoking and lung cancer risk
The average smoking rate of the research participants was 50.4%. There was a significant difference in smoking rate between males and females: 71.3% and 1.6% for men and women, respectively. There was no significant difference in smoking rate among females between the case and control groups (P > 0.05). Due to the low smoking rate among females, only ten cases and six controls female smokers were included in this study. To avoid the potential influence of gender on the relationship between smoking and the risk of lung cancer, we specifically analyzed the correlation between male smoking and lung cancer. Among the pathological patterns of lung cancers among males, adenocarcinoma ranked first with 472 cases (41.5%), followed by squamous carcinoma with 386 cases (34.0%), and small cell carcinoma with 109 cases (9.6%) (Table 2). Altogether, these three cancers accounted for 85.1% of lung cancer in the male patients. Supplementary Table 1 presents details regarding the association between smoking and lung cancer by gender.
Smoking was the most important risk factor for lung cancer in males. A history of smoking and current smoking increased the risk of different pathological patterns of lung cancer. The results revealed that there was a strong association between smoking and lung cancer (OR = 4.486, 95%CI 3.586–5.611). Our data further showed that there was a higher correlation between smoking and small cell lung cancer (OR = 15.081, 95%CI 5.997–37.924) and lung squamous cell carcinoma (OR = 7.243, 95%CI 4.838–10.844) compared to smoking and lung adenocarcinoma (OR = 3.037, 95%CI 2.297–4.014). Quitting smoking reduced the morbidity risk of lung cancer (OR = 0.804, 95%CI 0.648–0.999), as observed when comparing smokers with nonsmokers who had quit for at least 10 years. Quitting smoking did not significantly reduce the morbidity of lung adenocarcinoma (P > 0.05); however, among individuals who had quit for over 10 years, the risk of lung squamous cell carcinoma was reduced by 51.5% (OR = 0.485, 95%CI 0.318–0.740) and the risk of small cell lung cancer was reduced by 52.1% (OR = 0.479, 95%CI 0.237–0.969).
Lower smoking start age, longer smoking duration, higher daily number of cigarettes, and smoking pack–years were associated with an increased risk of lung adenocarcinoma, lung squamous cell carcinoma, small cell lung cancer, and lung cancer. Moreover, we observed a dose–response relationship (P < 0.001), with the highest risk being small cell lung cancer followed by lung squamous cell carcinoma. The correlation between different smoking depths and pathological patterns of lung cancer was statistically significant (P < 0.05). The risk of lung cancer when the smoker fully inhaled cigarette smoke was higher compared to when the smoker inhaled only into the mouth cavity and throat, and in these cases the risk of small cell lung cancer was the highest (OR = 21.405, 95%CI 8.461–54.151). Different cigarette types also increased the risk of different pathological patterns of lung cancer (P < 0.05). For instance, the risk of lung cancer existed when smoking filter-tipped cigarettes compared to compare to never smokers (OR = 3.780, 95%CI 3.007–4.751). However, relative to other types of cigarettes, smoking filter-tipped cigarettes is less at risk for lung adenocarcinoma, squamous cell carcinoma, and small cell cancer. See details in Table 2.
Relationship between ETS and risk of lung cancer among nonsmokers
There were 1608 nonsmokers in this study. Of these, 623 were in the case group and 985 in the control group. The nationality, marital status, and pulmonary disease history did not significantly differ between the two groups (P > 0.05), but age, gender, education, BMI, drinking alcohol, drinking tea, prior occupational exposure to hazardous substances, and family history of lung cancer significantly differed between the groups (P < 0.05) (Supplementary Table 2). In the 1608 cases, 728 individuals had been exposed to ETS, and the passive smoking rate was 45.3% (36.8% for males and 51.0% for females). There were 623 nonsmoking patients with lung cancer, and the top two pathological patterns were adenocarcinoma (434 cases, 69.7%) and squamous carcinoma (72 cases, 11.6%), which accounted for 81.3% of the total cases of nonsmokers with lung cancer. Therefore, this research focused on analyzing the correlation between ETS and these two pathological patterns of lung cancer.
Our data show that ETS is a risk factor for lung adenocarcinoma (OR = 2.206, 95%CI 1.711–2.845), lung squamous cell carcinoma (OR = 2.715, 95%CI 1.626–4.533), and lung cancer (OR = 2.229, 95%CI 1.780–2.793) among nonsmokers. We found that the OR value is more closely related to lung squamous cell carcinoma. Particularly, people exposed to workplace and household ETS were at greater risk of developing lung squamous cell carcinoma (OR = 3.154, 95%CI 1.270–7.834). The accumulated exposure of individual ETS was reflected by the passive smoking index. When the passive smoking index increased, the risk of lung adenocarcinoma and lung squamous cell carcinoma also increased, exhibiting a dose–response relationship (Ptrend < 0.001). The association strength of the passive smoking index with lung squamous cell carcinoma was larger compared to lung adenocarcinoma.
Regardless of gender, ETS was a risk factor for different pathological patterns of lung cancer among nonsmokers, and the association strength between males and lung squamous cell carcinoma was larger compared to the association between females and the same type of cancer. Workplace ETS was the important risk factor for male nonsmokers suffering from lung cancer; meanwhile, patients exposed to workplace and household ETS were at a greater risk of lung cancer (OR = 3.155, 95%CI 1.511–6.588). For females, household ETS was the important risk factor for lung cancer (OR = 2.224, 95%CI 1.644–3.009). In males, household ETS was more likely than workplace ETS to cause lung adenocarcinoma, while workplace ETS increased the risk of lung adenocarcinoma and lung squamous cell carcinoma, and both household and workplace ETS exposure increased the onset risk of lung squamous cell carcinoma. In females, household ETS exposure was the important risk factor for lung adenocarcinoma and lung squamous cell carcinoma, while the association strength among workplace ETS and lung adenocarcinoma and lung squamous cell carcinoma was not statistically significant (Table 3).
Interaction between smoking, ETS, and lung cancer
Combined effect analysis showed that female nonsmokers were at a greater risk than male nonsmokers for developing lung cancer (OR = 2.671, 95%CI 2.047–3.484), and female smokers had an even greater risk of developing lung cancer (OR = 5.256, 95%CI 1.694–16.309). Females who were not exposed to ETS were at a greater risk of developing lung cancer compared to males who were not exposed to ETS (OR = 2.882, 95%CI 2.030–4.089), and females exposed to ETS had an even greater risk of developing lung cancer (OR = 5.736, 95%CI 4.024–8.177). Additionally, we found neither additive interactions nor multiple interactions between smoking and gender or ETS and gender (Table 4).
Population attributable risk proportion of smoking and ETS
The PAR%’s for male smokers were 65.93% for lung cancer, 53.06% for lung adenocarcinoma, 77.60% for lung squamous cell carcinoma, and 88.66% for small cell lung cancer. Furthermore, among nonsmokers, the PAR% for ETS exposure was 31.03% for lung cancer, 33.14% for male lung cancer, 32.02% for female lung cancer, 30.62% for lung adenocarcinoma, and 38.56% for lung squamous cell carcinoma (Table 5).
Discussion
In the current study, a case–control study design was used to collect the relevant exposure information of the participants through epidemiological investigation. Although the quality control was emphasized in the design, implementation, and analysis stages, some of the exposure information was mainly based on the self-report from the participants. It was difficult to avoid the recall bias completely and reporting bias. The sample size of this study is large, but some factors with low exposure rate remain small for analyzing. We verified that smoking is the most important risk factor for developing lung cancer, and we found associations between smoking and small cell lung cancer, lung squamous cell carcinoma, and lung adenocarcinoma. We found dose-dependent associations between lower smoking start age, longer smoking duration, higher daily number of cigarettes, and smoking pack–years, respectively, with increased risks of lung adenocarcinoma, lung squamous cell carcinoma, and small cell lung cancer. Small cell lung cancer had the greatest dose–response relationship, followed by lung squamous cell carcinoma, and then lung adenocarcinoma. Smoking filter-tipped cigarettes was associated with a lower risk of lung adenocarcinoma, lung squamous cell carcinoma, and small cell lung cancer, which is consistent with the results of several previous studies (Cozen et al. 2017; Houston et al. 2014). However, the popularization of filter-tipped cigarettes has enabled smokers to obtain more nicotine per cigarette, which has possibly allowed smokers to inhale deeper when smoking in order to meet the smoker’s desire for nicotine. As a result, lung tissues furthest from the bronchi are more likely to come into contact with carcinogenic substances (Chang et al. 2016; Ramström 2017), which may be the causative factor for the rising proportion of lung adenocarcinoma and the declining proportion of lung squamous cell carcinoma in the pathological pattern of lung cancer in recent years. Compared with smokers who never quit, smoking–quitting does not significantly reduce the risk of lung adenocarcinoma, but smoking–quitting for ≥10 years was associated with a reduced risk of lung squamous cell carcinoma (51.5%) and small cell lung cancer (52.1%). Therefore, smoking-quitting is positively correlated with preventing and controlling lung cancer.
We used the passive smoking index to quantify the accumulated exposure of passive smoking. We found that ETS exposure is a risk factor for lung cancer among nonsmokers. Both household and workplace ETS exposure increased the risk of lung cancer among nonsmokers, which is consistent with the higher association between ETS and lung squamous cell carcinoma compared to ETS and lung adenocarcinoma. Workplace ETS exposure is the important risk factor of lung cancer among male nonsmokers. Specifically, workplace ETS increased the risk of onset of lung adenocarcinoma and lung squamous cell carcinoma and may be related to the harm suffered by males exposed to secondhand smoking in the workplace. Our study also found that household ETS exposure increased the risk of lung adenocarcinoma and lung squamous cell carcinoma among females, while workplace ETS exposure was not significantly associated with lung adenocarcinoma and lung squamous cell carcinoma among females. This may be attributed to the higher rate of male Chinese smokers, which may result in potentially higher ETS exposure for female spousal nonsmokers. This result is consistent with previous studies (Avino et al. 2018; Becher et al. 2018; Hori et al. 2016; Kim et al. 2014b; Li et al. 2018; Ni et al. 2018; Okazaki et al. 2016; Wang et al. 2015a).
There are over 6000 chemical substances in cigarette smoke, and of these approximately 69 are known carcinogens. Nicotine is an important component of tobacco that affects the central nervous system (Sharp and Chen 2019), it is responsible for smoking addiction, and various randomized trials found that reducing the tobacco nicotine lowers smoking rates (Donny et al. 2015; Higgins et al. 2017). The most significant carcinogens in lung cancer are benzopyrene, nitrate, and 4-(methylnitroso)-1-(3-pyridyl)-1-butanone (NNK), all of which are polycyclic aromatic hydrocarbons. Sidestream smoke (80%) that is released by tobacco burning and mainstream smoke exhalation from smokers contribute to ETS (Du et al. 2020). Several chemical reactions take place in the environmental smoke, and the smoke particles become smaller after a few hours. Compared to mainstream smoke, which is inhaled by the smokers, sidestream smoke inhaled by passive smokers contains higher levels of toxic substances and carcinogenic compounds such as nitrosamine, 4-aminobiphenyl, and benzopyrene (Behera et al. 2014). Additionally, ETS exposure for a longer time and without protective factors of active smoking, for example, the filter and more complete combustion occur (Ngu and McEvoy 2017). After the carcinogens enter the human body, the occurrence of lung cancer may be caused in one of the following ways (Clark and Molloy 2017; Kocyigit et al. 2011; Kubo et al. 2005):
-
(1)
Smoking can cause free radical oxidation. Cigarette smoke contains a large number of reactive oxygen species, and when inhaled can exhaust or decompensate the antioxidant substances and anti-oxidases in the human body resulting in consequent injury to biomacromolecules (such as DNA, RNA, protein, and fat). This sets favorable conditions for the initiation and development of malignant tumors.
-
(2)
Smoking directly leads to mutation of proto-oncogenes or cancer suppressor genes (such as proto-oncogene RAS, MYC, and cancer suppressor gene p53).
-
(3)
Carcinogenic metabolic enzymes activated by exposure to smoke can cause DNA damage and gene mutation.
-
(4)
Imbalanced expression of lung injury and inflammatory cell factors following exposure to cigarette smoke promote lung cancer.
In recent years, the smoking rate has reduced remarkably in many developed countries, and the smoking–quitting rate has exceeded 50% (Giovino et al. 2012). Accordingly, the lung cancer morbidity and mortality rates have also declined (Mowls et al. 2015). However, in the Fujian Province of China, the male smoking rate is higher (76.1%) compared to that in the general Chinese population (68%). Interestingly, the female smoking rate is less (1.8%) than that in the general Chinese population (3.2%), and the rate of quitting is also less (11.5%) than that in to the general Chinese population (10%) (Chen et al. 2015; Lin et al. 2008). Moreover, China is also facing a rising trend of smoking among adolescents. The age of smokers in China, as well as the average age at which individuals start smoking, is decreasing. Based on a 2010 global adult tobacco survey, the passive smoking rate in the Chinese population is 72.4%, causing 38.0% of nonsmokers to be exposed to ETS daily. A survey of adult passive smoking in 11 provinces and counties of China revealed that 39.4% of nonsmokers are exposed to passive smoking. Furthermore, the passive smoking rate was higher among females than males (Xu et al. 2010).
The results from the current study indicate that if all male smokers quit smoking, the percentage of lung cancer, lung adenocarcinoma, lung squamous cell carcinoma, and small cell lung cancer among males could be reduced by approximately 66%, 53%, 78%, and 89%, respectively. The occurrence of nonsmoking lung cancer (31.03%), male nonsmoking lung cancer (33.14%), female nonsmoking lung cancer (32.02%), nonsmoking lung adenocarcinoma (30.62%), and nonsmoking lung squamous cell carcinoma (38.56%) was attributed to ETS exposure. The Tobacco Control Movement is concerned about the significance of smoking on public health. Smoking is closely related to lung cancer and the Chinese population has a high smoking rate; therefore, compared to other risk factors of lung cancer, such as inheritance and environmental pollution, adopting the precautionary measure of quitting smoking is more feasible and will have greater public health significance. Therefore, it is urgent to establish policy and/or systems approaches that support healthy behaviors for Chinese. Further developing the Tobacco Control Movement to include raising taxes on cigarettes, providing certain cessation treatment services, and implementing a smoke-free policy in public places is needed. Additionally, it is vital to better educate the Chinese population on the harms of tobacco use as well as enhance awareness of self-care.
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Avino P, Scungio M, Stabile L, Cortellessa G, Buonanno G, Manigrasso M (2018) Second-hand aerosol from tobacco and electronic cigarettes: evaluation of the smoker emission rates and doses and lung cancer risk of passive smokers and vapers. Sci Total Environ 642:137–147. https://doi.org/10.1016/j.scitotenv.2018.06.059
Becher H, Belau M, Winkler V, Aigner A (2018) Estimating lung cancer mortality attributable to second hand smoke exposure in Germany. Int J Public Health 63:367–375. https://doi.org/10.1007/s00038-017-1022-1
Behera S, Xian H, Balasubramanian R (2014) Human health risk associated with exposure to toxic elements in mainstream and sidestream cigarette smoke. Sci Total Environ 472:947–956. https://doi.org/10.1016/j.scitotenv.2013.11.063
Cao M, Li H, Sun D, Chen W (2020) Cancer burden of major cancers in China: a need for sustainable actions. Cancer Commun (London, England) 40:205–210. https://doi.org/10.1002/cac2.12025
Chang CM, Edwards S, Arab A, Del Valle-Pinero A, Yang L, Hatsukami DK (2016) Biomarkers of Tobacco Exposure: Summary of an FDA-sponsored Public Workshop. Cancer Epidemiol Biomarkers Prev 26:291–302 https://doi.org/10.1158/1055-9965.EPI-16-0675
Chen Z et al (2015) Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet (London, England) 386:1447–1456. https://doi.org/10.1016/s0140-6736(15)00340-2
Chen W et al (2016) Cancer statistics in China, 2015 CA. Cancer J Clin 66:115–132. https://doi.org/10.3322/caac.21338
Clark S, Molloy P (2017) Smoke-induced changes to the epigenome provide fertile ground for oncogenic mutation. Cancer Cell 32:278–280. https://doi.org/10.1016/j.ccell.2017.08.016
Cozen et al. (2017) Case-control study of cumulative cigarette tar exposure and lung and upper aerodigestive tract cancers. Int J Cancer 140:2040–2050. https://doi.org/10.1002/ijc.30632
Donny E et al (2015) Randomized trial of reduced-nicotine standards for cigarettes. New England J Med 373:1340–1349. https://doi.org/10.1056/NEJMsa1502403
Du Y et al (2020) Lung cancer occurrence attributable to passive smoking among never smokers in China: a systematic review and meta-analysis. Trans Lung Cancer Res 9:204–217. https://doi.org/10.21037/tlcr.2020.02.11
Feng R, Zong Y, Cao S, Xu R (2019) Current cancer situation in China: good or bad news from the 2018 global Cancer statistics? Cancer Commun 39:22. https://doi.org/10.1186/s40880-019-0368-6
Giovino G et al (2012) Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys. Lancet 380:668–679. https://doi.org/10.1016/s0140-6736(12)61085-x
Higgins S et al (2017) addiction potential of cigarettes with reduced nicotine content in populations with psychiatric disorders and other vulnerabilities to tobacco addiction. JAMA Psychiat 74:1056–1064. https://doi.org/10.1001/jamapsychiatry.2017.2355
Hori M, Tanaka H, Wakai K, Sasazuki S, Katanoda K (2016) Secondhand smoke exposure and risk of lung cancer in Japan: a systematic review and meta-analysis of epidemiologic studies. Japanese J Clin Oncol 46:942–951. https://doi.org/10.1093/jjco/hyw091
Houston K, Henley S, Li J, White M, Richards T (2014) Patterns in lung cancer incidence rates and trends by histologic type in the United States, 2004-2009. Lung Cancer 86:22–28. https://doi.org/10.1016/j.lungcan.2014.08.001
Kim C et al (2014a) Smoky coal, tobacco smoking, and lung cancer risk in Xuanwei, China. Lung Cancer 84:31–35. https://doi.org/10.1016/j.lungcan.2014.01.004
Kim C et al (2014b) Exposure to secondhand tobacco smoke and lung cancer by histological type: a pooled analysis of the international lung cancer consortium (ILCCO). Int J Cancer 135:1918–1930. https://doi.org/10.1002/ijc.28835
Kocyigit A, Selek S, Celik H, Dikilitas M (2011) Mononuclear leukocyte DNA damage and oxidative stress: the association with smoking of hand-rolled and filter-cigarettes. Mutation Res 721:136–141. https://doi.org/10.1016/j.mrgentox.2011.01.013
Kubo S, Kobayashi M, Masunaga Y, Ishii H, Hirano Y, Takahashi K, Shimizu Y (2005) Cytokine and chemokine expression in cigarette smoke-induced lung injury in Guinea pigs. European Respiratory J 26:993–1001. https://doi.org/10.1183/09031936.05.00042405
Li M, Liu X, Zhang L (2018) The relationship of indoor coal use and environmental tobacco smoke exposure with lung cancer in China: a meta-analysis. J Cancer Res Therapeutics 14:S7–S13. https://doi.org/10.4103/0973-1482.168965
Lin X, Zhong WL, Lin SG (2008) Epidemiological survey on smoking situation for adults in Fujian. Strait J Prevent Med 14:1–3
López-Campos J, Ruiz-Ramos M, Fernandez E, Soriano J (2018) Recent lung cancer mortality trends in Europe: effect of national smoke-free legislation strengthening. Eur J Cancer Prev 27:296–302. https://doi.org/10.1097/cej.0000000000000354
Mowls D, McCaffree D, Beebe L (2015) Trends in lung cancer incidence rates, Oklahoma 2005-2010. PLoS One 10:e0119251. https://doi.org/10.1371/journal.pone.0119251
Ngu N, McEvoy M (2017) Environmental tobacco smoke and peripheral arterial disease. A Rev Atherosclerosis 266:113–120. https://doi.org/10.1016/j.atherosclerosis.2017.09.024
Ni X, Xu N, Wang Q (2018) Meta-analysis and systematic review in environmental tobacco smoke risk of female lung cancer by research type. Int J Environ Res Public Health 15:1348. https://doi.org/10.3390/ijerph15071348
Okazaki I, Ishikawa S, Ando W, Sohara Y (2016) Lung adenocarcinoma in never smokers: problems of primary prevention from aspects of susceptible genes and carcinogens. Anticancer Res 36:6207–6224. https://doi.org/10.21873/anticanres.11215
Ramström L (2017) Insufficient knowledge about use of multiple tobacco/nicotine products. Addict Behav 76:384–385. https://doi.org/10.1016/j.addbeh.2017.01.027
Sharp B, Chen H (2019) Neurogenetic determinants and mechanisms of addiction to nicotine and smoked tobacco. Eur J Neurosci 50:2164–2179. https://doi.org/10.1111/ejn.14171
Sung H, Ferlay J, Siegel R, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. https://doi.org/10.3322/caac.21660
Wang A et al (2015a) Active and passive smoking in relation to lung cancer incidence in the Women’s health initiative observational study prospective cohort. Annals Oncol 26:221–230. https://doi.org/10.1093/annonc/mdu470
Wang G et al (2015b) Tobacco smoke induces production of chemokine CCL20 to promote lung cancer. Cancer Lett 363:60–70. https://doi.org/10.1016/j.canlet.2015.04.005
WHO (2015) Smoke-free policies in china–evidence of effectiveness and implications for action. https://iris.wpro.who.int/handle/10665.1/12047
Xiao J, Zhou Y, Jiang H, Lin Y, Ma J (2015) Analysis of cancer incidence and mortality from cancer registries of Fujian province in 2011 Zhonghua yu fang yi xue za zhi. Chin J Prevent Med 49:738–740
Xu T, Li W, Hu B (2010) Survey of smoking and passive smoking status among chinese adults in 11 provinces. Chin J Prevent Control Chronic Diseases 18:229–230
Acknowledgments
We thank all the staff from the Department of Thoracic Surgery, The First Affiliated Hospital of Fujian Medical University. We also would like to express our appreciation to the patients who participated in our study.
Funding
This study was supported by the National Natural Science Foundation of China [grant number 81402738].
Author information
Authors and Affiliations
Contributions
FH and LC conceived and designed the experiments; ZQL, QPX, and WMX did the survey; FH, ZQL, JMZ, and RDX analyzed the data; RDX and XL contributed materials; JMZ and RDX wrote the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Ethical Review Committee of Fujian Medical University (Fuzhou, China).
Consent to participate
All of the participants consented to complete the questionnaire.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 210 kb)
Rights and permissions
About this article
Cite this article
Zhuang, J., Liu, Z.q., Xiao, R. et al. Association between smoking and environmental tobacco smoke with lung cancer risk: a case–control study in the Fujian Chinese population. J Public Health (Berl.) 30, 2047–2057 (2022). https://doi.org/10.1007/s10389-021-01573-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-021-01573-3