Abstract
Purpose
To determine the prevalence of and risk factors for myopia in primary school children in Chaoyang District, Beijing.
Methods
This cross-sectional prevalence survey was conducted in September to October 2011 in 4 schools randomly chosen from among the 126 primary schools in Chaoyang District. Students were assessed with autorefractometry under cycloplegia and checked with retinoscopy for accuracy. Questionnaires were completed by the students’ parents.
Results
Myopia was present in 36.7 ± 0.7 % of 4249 students aged 5–14 years old. The prevalence of myopia in girls (38.6 ± 1.1 %) was significantly higher than in boys (35.0 ± 1.0 %) (p = 0.015) and increased with age (p < 0.001), with the highest prevalence observed in children aged ≥11 years (67.5 ± 1.8 %). After adjustment, having a myopic parent (aOR 3.10; 95 % CI 2.49–3.86), incorrect reading posture (aOR 2.09; 95 % CI 1.75–2.50), reading a book at a distance of <20 cm (aOR 1.60; 95 % CI 1.16–2.21), studying at home for >3 h daily (aOR 1.50; 95 % CI 1.12–2.01), studying for >1 h continuously (aOR 1.21; 95 % CI 1.02–1.45), and reading extracurricular books that utilize a font larger than that used in textbooks (aOR 0.74; 95 % CI 0.59–0.94) were all significantly associated with myopia.
Conclusions
The prevalence of myopia among primary school children in Beijing increased with age, and was significantly higher in girls ≥10 years old. Myopia was significantly associated with parental myopia, reading posture, distance between the eyes and the book being read, font size used in extracurricular reading material, time spent studying at home, and the duration of continuous study time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myopia is not only one of the most common visual impairments in both children and adults, but also a leading cause of preventable blindness in developing countries [1]. The rate of myopia is increasing globally, especially in East and Southeast Asian countries. For example, in the United States, the prevalence of myopia was reported to be 28 % in 12 year olds in 1993 [2], and increased significantly in children aged 12–17 from 12 % in 1971–1972 to 31.2 % in 1999–2004 [3]. In Japan, the prevalence of myopia among those 7 years of age or older increased considerably from 39 % in 1984 to 59 % in 1996 [4]. In Hong Kong, the rate of myopia in a local school was reported to be 87.2 % in 2001, 25 % higher than the rate reported in 1991 [5]. In China, a nationwide survey of myopia in school children conducted during 2008–2009 showed that the prevalence of myopia was 13.7 % in primary school children, 42.9 % in junior high-school children, and 69.7 % in senior high-school children, and that the prevalence of myopia among children in developed regions was higher than that in children in less-developed regions [6]. In a Chinese metropolitan city, myopia (a spherical equivalent of at least −0.50 D in either eye) diagnosed by retinoscopy affected 73.1 % of children aged 15, or 78.4 % when diagnosed with autorefraction [7]. A review by He et al. reported that, in China, school children in urban settings exhibited a higher prevalence of myopia compared with those in rural settings, which may suggest environmental effects, given that the genetic background among people living in the urban and rural areas was similar [8].
Myopia is a complex condition and its progression may be impacted by both genetic and environmental components. It is reported that a parental history of myopia [9, 10], higher socioeconomic status [11], reduced outdoor activity [12], near work [13], and low light levels [14] may increase the likelihood of developing myopia. However, the associations between these factors and myopia have not been observed in other studies [15, 16]. As such, the impact of genetic and environmental factors on the development of myopia remains controversial; this may be partly due to the small sample sizes that have been employed in studies in this field, the assessment of myopia without using accurate diagnostic tools such as cycloplegic retinoscopy, or a lack of measurements of the exact intensities of the risk factors for myopia, such as near work or outside activities.
Poor vision as a result of uncorrected refractive error has been identified as a priority area by the World Health Organization’s global initiative for the elimination of avoidable blindness by the year 2020 [17]. The high prevalence of myopia among children in large cities in China has also reached a level that demands closer attention. In order to introduce effective preventive measures to curb the progression of myopia, it is necessary to investigate the current prevalence of myopia and its contextual factors so that appropriate interventions can be provided. Relatively few studies have been conducted in children in China using comprehensive or ophthalmic assessments of vision. In this study, we used cycloplegic refraction to accurately identify myopia among primary school children along with a detailed questionnaire on both genetic and environmental risk factors.
Materials and methods
Study population and sampling
A cross-sectional prevalence survey of myopia in primary school children was conducted in Chaoyang District, Beijing from September 2011 to October 2011. The sampling frame was based on 126 primary schools throughout Chaoyang District excluding international schools and special schools for the disabled. The study population was primary school children aged 5–14, grades 1–6. We randomly selected 4 primary schools from this district. The school principals were informed of the study objectives and procedures and all agreed that their schools would participate in the study. All children in the selected schools were invited to take part in the study. Written consent forms were sent to their parents before the ophthalmic examinations. All students had eye examinations and their parents completed a questionnaire. Those diagnosed with eye diseases such as keratoleukoma, cataract, glaucoma, and retinopathy were excluded from the study. We also excluded students who had received an ortho-K treatment. Approval for the study was granted by the Ethics Committee of the Capital Institute of Pediatrics.
Questionnaire and eye examinations
We designed a questionnaire using evidence from the literature to identify factors that might be associated with myopia. We then obtained advice on the questionnaire from experts engaged in research into refractive diseases and epidemiology and made revisions as necessary. The revised version was pilot tested on 60 parents from a primary school that was not one of the 4 schools included in this study. The parents were asked to give feedback on how easy the questionnaire was to understand and complete. The questionnaire was then finalized according to the parents’ input.
The questionnaire included questions on demographics, such as gender, date of birth, and school grade; family history of myopia, including parents, grandparents, and siblings; visual behavior, the child’s living environment, and intensity of visual activities. Visual behavior examined included correct reading posture, reading distance, font size of extracurricular books compared with the standard textbook according to textbook regulations (GB/T 18358-2009), sleep time, and light environment while studying. To assess correct reading posture, the questionnaire included a picture of the correct posture according to “The primary and middle school students myopia prevention and control work plan” issued by the Ministry of Education in 2008. The description accompanying the picture was as follows: “Sit in a chair that permits both feet to rest flat on the floor. Make sure your upper back and neck are straight, but still in a comfortable position. The distance between your eye and the book should be kept at about 30 cm. A fist should fit between your chest and table”. Any reading position not consistent with this description was considered to be incorrect. General requirements for page size and type area for primary and secondary school textbooks can be found in the standard GB/T 18358-2009. For students in grades 1 and 2, textbooks contain Chinese characters with a font size of 2 (equal to English characters with a font size of 22 points) to 3 points (equal to English characters with a font size of 16 points). Students in grades 2–4 use textbooks in Chinese characters with a font size of 4 points (equal to English characters with a font size of 14 points), and students in grade 5 or above use textbooks in Chinese characters with a font size of small 4 points (equal to English characters with a font size of 12 points). Parents were asked to compare the usual font employed in their child’s extracurricular reading books to their textbooks and report whether it was smaller, the same size, or larger.
Intensity of visual activities included how many extracurricular classes children attended per week, and how many hours per day the child spent performing the following activities outside school : (1) studying for school assignments; (2) reading books while lying down or lying prone; (3) reading books while on a bus or walking; (4) using palmtop electronic products; (5) watching television each weekday and on the weekend; (6) playing video/computer games each weekday and on the weekend or studying on the computer each weekday and on the weekend; (7) engaging in outside activities each weekday and on the weekend; (8) studying without a break or with a break of less than 10 min; and (9) studying using computer without a break or with a break of less than 10 min.
To measure uncorrected visual acuity, we used a light box type “E” word standard logarithmic visual chart at a distance of 5 m from each subject. Visual acuity measurements were performed by ophthalmic nurses. Evaluation of binocular motor function, examination of the anterior segment, automated refraction, and media and fundus examinations were done by the study team’s ophthalmologists. Poor vision was defined as an uncorrected visual acuity of <1.0. Students with poor vision were then examined using rapid cycloplegic refraction performed with cycloplegic autorefraction and a retinoscope or subjective refraction, provided their parents gave written consent. Automated refraction was performed with an autorefractometer (Canon rk-f1, Tokyo, Japan) after completion of the drug regime. Cycloplegic refraction was measured 30 min after the last instillation of 3 drops of 1 % tropicamide at 5-min intervals. All values of refractive status were rechecked with a retinoscope by senior ophthalmologists. We used the values of refraction measured by retinoscopy to define refractive status, including myopia, hypermetropia, and astigmatism.
Definitions
Spherical equivalent refraction (SER) was calculated as the numerical sum of the sphere and half of the cylinder. The negative cylinder method was used. Emmetropia was defined as a mean SER of between −0.50 D and +2.00 D (including uncorrected visual acuity ≥1.0). Myopia was defined as SER of −0.50 D or worse in one or both eyes. Hypermetropia was defined as SER of +2.00 D or more. Astigmatism was defined as cylinder ≥1.00 D (absolute value).
Data analysis
Clinical examination and questionnaire data were reviewed for accuracy and completeness before computer data entry. Data ranges, frequency distributions, and consistency among related measurements were checked with data cleaning programs. The chi-square test was used to analyze prevalence of myopia among the children according to the various characteristics measured. The Cochran–Armitage trend test was used to test the linear trends in the prevalence of myopia in different age groups. To identify risk factors associated with myopia, odds ratios and 95 % confidence intervals (CI) were calculated using univariate logistic regression analysis. Multivariate logistic regression analysis was used to determine independent risk factors. All of the factors associated with myopia as identified by univariate analysis were included in the multivariate analysis. Comparison of the spherical equivalents between autorefraction and retinoscopy was conducted using Student’s paired t-test and correlation was assessed using Pearson’s correlation analysis. All statistical tests were two-sided at p < 0.05 and were performed using R 2.15 (http://www.r-project.org). All prevalence data are presented as the mean ± standard error.
Results
Of the 4321 children invited, 4249 (98 %) participated in the study, 2048 of which were girls (48.2 %) and 2201 were boys (51.8 %) aged 5–14 years old. The mean age of the children was 8.9 ± 1.7 [standard deviation (SD)] years old. Table 1 shows the demographic characteristics of the study participants. More than half of the children’s parents had myopia.
Prevalence of myopia and other refractive errors
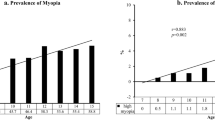
The prevalence of myopia, emmetropia, hypermetropia, and astigmatism in the school children examined are shown in Table 2. Myopia was the most common type of refractive error. The overall prevalence of myopia in this sample was significantly higher in girls than in boys (p = 0.015) and increased with respect to age in both boys and girls (p < 0.001). Compared with other age groups, the prevalence of myopia was greatest (at 67.5 ± 1.8 %) in children aged ≥11 years. The prevalence of myopia increased from 8.7 % in boys younger than 7 years old to 63.0 % in boys older than 11 years, and from 6.3 % in girls younger than 7 years to 72.0 % in girls older than 11 years. According to age group, boys younger than 7 years had a higher prevalence of myopia than girls younger than 7 years. But in the groups aged 7 and older, girls had a higher prevalence of myopia than boys. The differences between boys and girls were significant for children aged 10 and older (p < 0.05) (Fig. 1).
Astigmatism was the second most common refractive error. Boys had a higher prevalence of astigmatism than girls, but the difference was not significant (p > 0.05). The prevalence of astigmatism increased significantly with age (p < 0.001). The prevalence of hypermetropia overall was 2.4 ± 0.2 % and was higher for boys compared with girls, but the difference was insignificant (p > 0.05). The prevalence of hypermetropia decreased significantly with age (p < 0.001). The prevalence of emmetropia was significantly higher for boys than girls (p = 0.024).
Univariate and multivariable logistic regression
Use of univariate logistic regression determined that the following factors were associated with myopia: sex, age, parental history of myopia, reading position, distance between eyes and books, time spent lying down or lying prone while reading a book, sleep time, font size of extracurricular reading books versus textbooks, learning time at home, extracurricular lessons, continuous learning time, time spent performing outdoor activities from Monday to Friday, time spent performing outdoor activities at the weekend, and continuous use of a computer (Table 3).
The significant risk factors identified in the univariate logistic regression were used to identify independent risk factors for myopia in a multivariate logistic regression (Table 3). We found that boys were less likely to have myopia than girls. There was also a relationship between increasing age and myopia such that the adjusted odds ratio increased from 2.33 (95 % CI 1.59–3.44) at 7 years old to 26.71 (95 % CI 17.88–39.92) for children 11 or older compared with children less than 7 years old. Compared with the reference group (children with no myopic parents), the risk of myopia was higher for participants where either parent or both parents had myopia. We observed an approximate twofold increase in the risk of myopia among participants with an incorrect reading position. We also observed an increased risk of myopia in participants who maintained a distance of less than 20 cm between their eyes and a book, who studied for more than 3 h a day outside of school, or who studied continuously for more than 1 h. Participants who read extracurricular books where the font size was larger than that used in school textbooks were less likely to have myopia.
Comparison of the spherical equivalents between autorefraction and retinoscopy
A total of 1156 students with poor vision had an eye examination performed using rapid cycloplegia. Measures of cycloplegic refraction were obtained using both autorefraction and retinoscopy. The mean refractive error measured by autorefraction and retinoscopy in the students’ right eyes was −1.02 ± 1.83 and −1.12 ± 1.75 diopters, respectively, and in their left eyes it was −0.94 ± 1.84 and −1.07 ± 1.75 diopters, respectively. The differences in refractive error measured by the two methods were found to be statistically significant (p < 0.0001). For students younger than 11 years, the spherical equivalents measured by autorefraction were significantly higher than those measured using retinoscopy for both eyes (p < 0.05). For students aged 11 years or older, there was no significant difference in spherical equivalent in either eye as measured by the two methods (see Table 4). The differences in refractive error between autorefraction and retinoscopy were significantly associated with age (p < 0.0001 each for right and left eyes). The refractive error measured by cycloplegic autorefraction was highly correlated with the cycloplegic retinoscopy results (r = 0.99, p < 0.0001 for both eyes). The autorefraction results indicated that 67.3 % of students had myopia, while the retinoscopy results indicated that 69.2 % of students had myopia. The kappa value was 0.93 and the observed agreement was 96.8 %.
Discussion
This study indicates that the overall prevalence of myopia (−0.50 D or less) in either eye as measured by cycloplegic retinoscopy is 36.7 % in primary school children in the Chaoyang District, a densely populated metropolitan area. This prevalence is higher than that reported in a study conducted in 2003 for metropolitan Guangzhou, which was supported by the U.S. National Eye Institute and the World Health Organization [7]. However, the prevalence is similar to the level of myopia among school children with a mean age of 9 years noted in Hong Kong, which was found to be 36.7 % in a study conducted with cycloplegic autorefractometry from 1998 to 2000 [18]. Although it is difficult to compare the prevalence of myopia across studies because of differences in study design, refractive error measurement methods, study population, and nonuniform definitions [19], our present study provides comparative data on the prevalence of myopia in primary school children using the same definition of myopia, school-based prevalence survey design with randomly selected primary schools, and more accurate refractive error measurement techniques. As such, our data indicate that the prevalence of myopia among primary school children in this urban area of Beijing is high.
Our results suggest that independent risk factors for myopia include female gender, increasing age, parental history of myopia, incorrect reading posture, reading at a distance of less than 20 cm between the eyes and the book, reading extracurricular books with a smaller font than that used in textbooks, spending more than 3 h per day studying, and studying outside school for more than 1 h at a time without a break. The fact that increasing age is the strongest risk factor for myopia is not surprising. Previous studies have documented a positive relation between age and myopia [20, 21]. This relationship may be due to an increasing requirement for study that results in children spending more time on visually taxing activities and less time on outdoor activities [22]. Since the prevalence of myopia increases with age, special attention should be paid to students in higher grades. In children aged less than 9 years, there is no significant difference between boys and girls. The prevalence of myopia increases quickly with age and the difference in the prevalence of myopia between boys and girls becomes significant at 10 years old and above. One potential reason for the gender differences in the prevalence of myopia may be that in China girls are traditionally more studious than boys. However, there may be other factors related to the differences between the genders. A previous study in school children aged 6–14 years old in Singapore reported that boys and girls with earlier growth spurts experienced earlier peak spherical equivalent, axial length velocity, and onset of myopia [23]. It is generally accepted that girls reach puberty earlier than boys. It is possible that girls who reach puberty early are also more likely to be heavier and taller than boys of the same age and to develop myopia earlier, although further investigation of this possibility is required.
Previous studies indicate that children with myopia are more likely to have a family history of myopia [16, 24, 25]. Our study confirms these findings, as the aOR for myopia was 1.72 when the father was myopic, 1.91 when the mother was myopic, and 3.10 when both parents were myopic. This evidence of an additional genetic risk for myopia is similar to the observations made during a population-based study of the impact of parental myopia on children in Guangzhou, China [16]. However, this risk could also have an environmental component, as increasing educational levels, a higher individual income, and professional or office-related occupations have previously been shown to be significantly associated with higher rates of myopia [26]. As such, perhaps mothers and fathers with myopia, who may have a higher socioeconomic status and education level, have a different degree of enthusiasm for instilling disciplined study practices in their children than mothers and fathers without myopia, who may come from a different background. Further study of the interaction between hereditary and environmental factors is warranted in the future.
Our finding that reading posture is an independent risk factor for myopia and has a larger effect on boys is consistent with previous clinical experience. We also found that reading with the book less than 20 cm from the eyes and studying for more than 1 h without a break are independent risk factors for myopia. These findings are similar to those from the Sydney Myopia Study, which reported that near-work activities in general are a weak risk factor, but that children who read continuously or at a close distance are more likely to be myopic [22]. These findings emphasize that it is necessary to quantify not only the time spent on near work but also the intensity and distance involved. Results from our study show that studying at home for more than 3 h per day is associated with an increased risk of myopia among children. Spending a long time on near work, such as reading and writing, could be associated with myopia, but epidemiological support for this idea is not strong [27]. The increased risk may be also related to the definition of learning at home in the questionnaire. Some children may learn while playing, but this was not probed by the questionnaire. Also, the study times indicated on the questionnaire rely on parent recall and may not be accurate. We also found that reading extracurricular books with a bigger font size compared with the font size used in textbooks is associated with a decreased risk of myopia, which has not been identified in previous studies.
Many factors, such as the time spent lying down or prone while reading a book, sleep time, amount of extracurricular lessons taken every week, hours of outdoor activities performed from Monday to Friday, hours of outdoor activities performed at the weekend, and hours of continuous computer use every day, were identified in the univariate logistic model but not in the multivariate logistic model; however, some of these factors have been found to be associated with myopia in other studies [15, 28]. Since this was a cross-sectional study, it is possible that some children’s visual habits may have changed once a diagnosis of myopia was made, such that the child no longer exhibits behavior associated with myopia. As such, we cannot draw any conclusion regarding a causal relationship from this study. Another limitation was that we did not measure cycloplegic refraction in children with uncorrected visual acuity ≥1.0 D. Some hyperopic children with refraction ≥2.0 D may have been counted in the emmetropia group, which would cause the number of children with hyperopia to be underestimated. However, this possibility has a much smaller effect on the prevalence of myopia. As in our pilot study, among children with normal vision (uncorrected visual acuity ≥1.0) who received the rapid cycloplegic refraction examination with retinoscopy, the spherical equivalent refractions of most children (91.5 %) were between −0.25 D and +2.00 D. We also did not collect information on each child’s lifestyle and activities directly from the child but from an adult who lived with the child, which may lead to the underestimation of some factors. In the future, by prospectively following children without myopia using ophthalmologic examinations and lifestyle surveillance, we can assess risk factors in more detail and assess their specific effects on the onset of myopia.
Although the differences in spherical equivalents measured by cycloplegic autorefraction and retinoscopy were found to be statistically significantly different, the detection of myopia by these two methods was highly consistent. The spherical equivalents measured by cycloplegic autorefraction were higher than those measured using retinoscopy and the differences in spherical equivalent were correlated with age, findings which are similar to those previously published [29]. Cycloplegic retinoscopy cannot be replaced by cycloplegic autorefraction, especially for younger children. However, the refractive error measured by autorefraction can be used as a reference point; based on this reference point, we can then perform retinoscopy to get a more accurate measurement of refractive error.
In conclusion, this study shows that the prevalence of myopia among primary school children in a central business district in Beijing was higher than that reported in a previous study conducted in Guangzhou, another metropolitan area in mainland China, but similar to the prevalence of myopia observed in Hong Kong 10 years ago. Myopia was associated with higher age, female gender, parental myopia, incorrect reading posture, smaller distance between the eyes and the book, smaller font size used in extracurricular reading books, longer time spent studying at home, and longer continuous study time.
References
Congdon NG, Friedman DS, Lietman T. Important causes of visual impairment in the world today. JAMA. 2003;290:2057–60.
Zadnik K. The Glenn A. Fry Award Lecture (1995): Myopia development in childhood. Optom Vis Sci. 1995;1997(74):603–8.
Vitale S, Sperduto RD, Ferris FL III. Increased prevalence of myopia in the United States between 1971–1972 and 1999–2004. Arch Ophthalmol. 2009;127:1632–9.
Matsumura H, Hirai H. Prevalence of myopia and refractive changes in students from 3 to 17 years of age. Surv Ophthalmol. 1999;44(Suppl 1):S109–15.
Lam CS, Goldschmidt E, Edwards MH. Prevalence of myopia in local and international schools in Hong Kong. Optom Vis Sci. 2004;81:317–22.
Xie HL, Xie ZK, Ye J, Yang XJ, Qu J. Analysis of correlative factors and prevalence on China’s youth myopia. Zhonghua Yi Xue Za Zhi. 2010;90:439–42.
He M, Zeng J, Liu Y, Xu J, Pokharel GP, Ellwein LB. Refractive error and visual impairment in urban children in southern China. Invest Ophthalmol Vis Sci. 2004;45:793–9.
He M, Zheng Y, Xiang F. Prevalence of myopia in urban and rural children in mainland China. Optom Vis Sci. 2009;86:40–4.
Lim LT, Gong Y, Ah-Kee EY, Xiao G, Zhang X, Yu S. Impact of parental history of myopia on the development of myopia in mainland China school-aged children. Ophthalmol Eye Dis. 2014;6:31–5.
Mutti DO, Mitchell GL, Moeschberger ML, Jones LA, Zadnik K. Parental myopia, near work, school achievement, and children’s refractive error. Invest Ophthalmol Vis Sci. 2002;43:3633–40.
You QS, Wu LJ, Duan JL, Luo YX, Liu LJ, Li X, et al. Factors associated with myopia in school children in China: the Beijing childhood eye study. PLoS One. 2012;7:e52668.
Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379:1739–48.
Saw SM, Zhang MZ, Hong RZ, Fu ZF, Pang MH, Tan DT. Near-work activity, night-lights, and myopia in the Singapore–China study. Arch Ophthalmol. 2002;120:620–7.
Donovan L, Sankaridurg P, Ho A, Chen X, Lin Z, Thomas V, et al. Myopia progression in Chinese children is slower in summer than in winter. Optom Vis Sci. 2012;89:1196–202.
Lin Z, Vasudevan B, Jhanji V, Mao GY, Gao TY, Wang FH, et al. Near work, outdoor activity, and their association with refractive error. Optom Vis Sci. 2014;91:376–82.
Xiang F, He M, Morgan IG. The impact of parental myopia on myopia in Chinese children: population-based evidence. Optom Vis Sci. 2012;89:1487–96.
Pizzarello L, Abiose A, Ffytche T, Duerksen R, Thulasiraj R, Taylor H, et al. VISION 2020: the right to sight: a global initiative to eliminate avoidable blindness. Arch Ophthalmol. 2004;122:615–20.
Fan DS, Lam DS, Lam RF, Lau JT, Chong KS, Cheung EY, et al. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest Ophthalmol Vis Sci. 2004;45:1071–5.
Saw SM, Katz J, Schein OD, Chew SJ, Chan TK. Epidemiology of myopia. Epidemiol Rev. 1996;18:175–87.
He M, Huang W, Zheng Y, Huang L, Ellwein LB. Refractive error and visual impairment in school children in rural southern China. Ophthalmology. 2007;114:374–82.
Lim HT, Yoon JS, Hwang SS, Lee SY. Prevalence and associated sociodemographic factors of myopia in Korean children: the 2005 third Korea National Health and Nutrition Examination Survey (KNHANES III). Jpn J Ophthalmol. 2012;56:76–81.
Ip JM, Saw SM, Rose KA, Morgan IG, Kifley A, Wang JJ, et al. Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci. 2008;49:2903–10.
Yip VC, Pan CW, Lin XY, Lee YS, Gazzard G, Wong TY, et al. The relationship between growth spurts and myopia in Singapore children. Invest Ophthalmol Vis Sci. 2012;53:7961–6.
Jones LA, Sinnott LT, Mutti DO, Mitchell GL, Moeschberger ML, Zadnik K. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci. 2007;48:3524–32.
Saw SM, Nieto FJ, Katz J, Schein OD, Levy B, Chew SJ. Familial clustering and myopia progression in Singapore school children. Ophthalmic Epidemiol. 2001;8:227–36.
Wong TY, Foster PJ, Hee J, Ng TP, Tielsch JM, Chew SJ, et al. Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Invest Ophthalmol Vis Sci. 2000;41:2486–94.
Mutti DO, Zadnik K. Has near work’s star fallen? Optom Vis Sci. 2009;86:76–8.
Paudel P, Ramson P, Naduvilath T, Wilson D, Phuong HT, Ho SM, et al. Prevalence of vision impairment and refractive error in school children in Ba Ria—Vung Tau province, Vietnam. Clin Exp Ophthalmol. 2014;42:217–26.
Demirci G, Arslan B, Özsütçü M, Eliaçık M, Gulkilik G. Comparison of photorefraction, autorefractometry and retinoscopy in children. Int Ophthalmol. 2014;34:739–46.
Acknowledgments
This study was funded by the China Health and Medical Development Foundation. The authors would like to thank the members of this study team and the participating schools, pupils, and parents. The authors would also like to thank Zhenying Li from the Chaoyang Center for Disease Control and Prevention, Beijing, China, and Ping Zhang from the Chaoyang Health Care Institution for students in Middle and Primary School, Beijing, China, for their hard work in collecting data. Editorial assistance during the preparation of this article was provided by Dr. Ruth Warre.
Conflicts of interest
Y. Lyu, None; H. Zhang, None; Y. Gong, None; D. Wang, None; T. Chen, None; X. Guo, None; S. Yang, None; D. Liu, None; M. Kang, None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Lyu, Y., Zhang, H., Gong, Y. et al. Prevalence of and factors associated with myopia in primary school students in the Chaoyang District of Beijing, China. Jpn J Ophthalmol 59, 421–429 (2015). https://doi.org/10.1007/s10384-015-0409-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-015-0409-x