Abstract
Purpose
To examine the prevalence of myopia in primary school children in Hong Kong, and the risk factors for myopia development.
Study design
A cross-sectional study.
Methods
Subjective refraction and axial length were measured in all participants. Structured questionnaire was completed by the parents to assess risk factors of myopia.
Results
A total of 1396 children (491 boys) from Grade 1 to Grade 6 from 4 primary schools in Sham Shui Po district of Hong Kong participated. All participants underwent non-cycloplegic refraction. The overall prevalence of myopia (spherical equivalent, SE ≤ -0.5 diopter [D]) was 37.7%, which significantly increased with age, from 13.3% at grade 1 to 54.7% at grade 6. The prevalence of moderate myopia (-3.0D < SE < -6.0D) increased from 1.6% at grade 1 to 18.2% at grade 6 and the prevalence of high myopia (SE < = -6.0 D and/or AL ≥ 26.5 mm) increased from 0.94% (7/747) in grade 1-3 students to 1.85% (12/649) in grade 4-6 students. Among the students with myopia, only 23.6% of the parents knew their children had refractive errors and only 19.8% of the children wore glasses. Multivariate logistic regression analysis showed myopia development was significantly associated with older age (OR = 1.36, P = 0.008), better academic ranking in class in the preceding semester (OR = 1.01, P = 0.02) and absence of routine eye check (OR = 2.70, P = 0.001).
Conclusion
The prevalence of myopia in primary school students in Hong Kong is high. There is a low level of awareness of refractive errors among parents, and high proportion of under-correction, resulting in suboptimal vision.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The prevalence of myopia is high in Hong Kong [1]. The largest series published, involving 2651 children aged 6-12 found that myopia (less than -0.50 diopter [D]) was 18.3% for the 6-year-old group and 61.5% for the 12-year-old group. Prevalence of high myopia of less than -6.00D increased from 0.7% at the age of 6 to 3.8% at the age of 12 [2]. Among adults in the developed countries of East and Southeast Asia, the prevalence of myopia is as high as 90%, in contrast to the much lower prevalence of less than 5–10% in developing countries [3]. For most of the myopic population, refractive errors tend to stabilize beyond adulthood. However, a significant portion of myopic individuals develop pathologic myopia, defined as myopia of less than -6D with progressive increase in axial length, resulting in various vision-threatening ocular pathologies. The incidence of myopia and pathologic myopia is particularly high in urban Asian communities, including Hong Kong. A study in Hong Kong shows that in adolescents with less than -6D myopia, 94/120 were found to have retinal changes of which 0.8% were sight-threatening [4].
Risk factors for myopia progression include younger age, higher myopic spherical equivalent at baseline and having 2 myopic parents. Regression analysis shows that the risk of myopia progression was 40% lower with each year of increased age, and 43% lower for every 1.0 D less in myopia at baseline [5]. Life style including decrease in outdoor activity, increase in time doing near work, and increase in urbanization were also found to be associated with myopia development [6].
Studies show myopia progresses at the fastest rate at 6-7 years old, and tends to slow down after 11-12 years of age [7, 8]. Hence the population most at risk would be in primary school. It is important to understand the rate of prevalence in recent years and risk factors in students so that policy makers and health care providers can implement strategies to halt the development of this disease. Because of the paucity of local data of myopia in Hong Kong, we conducted this study to examine the prevalence of myopia in primary school students, and managed to identify the risk factors for developing myopia in these students.
Methods
This was a school-based cross-sectional study. Four public primary schools in the Sham Shui Po District of Hong Kong were invited to join the study from March 2017 to May 2018. We did not exclude any students from participating, unless they declined to join. The study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (HKU/HA HKW IRB) and adhered to the tenets of the Declaration of Helsinki. All primary school students, from Grade 1 to Grade 6, in the 4 schools were invited to join the study. All parents were requested to sign an informed consent after we explained the study purpose and procedures.
Study parameters
-
1.
Ophthalmic assessment
Basic eye examinations included visual acuity (VA), and refraction OU. VA was tested on a logarithm of the minimum angle of resolution (logMAR) number chart (Lighthouse International) at 4 m OU. Best-corrected VA (BCVA) was measured with the best possible correction obtained with non-cylcoplegic auto-refraction, followed by subjective refraction by an optometrist. The spherical and cylindrical measurements, and the axis were documented. A logMAR VA higher than 0.2 was considered to have failed the VA test.
Ophthalmic investigations included OPD-Scan lll (Nidek) to assess the keratometry (KM), central corneal thickness (CCT), and white-to-white (WTW) distance; the anterior chamber depth (ACD) and axial length (AL) were measured by AL-scan (Nidek).
- 2.
Demographic data
Age, gender, and ethnicity were noted.
- 3.
Questionnaire to assess associated risk factors of myopia
After signing the consent form, the parents of the subjects were invited to complete a structured questionnaire. The questionnaire consisted of information about the subjects, mainly sociodemographic data, and habits. The questionnaire was designed in both Chinese for Chinese subjects, and English for non-Chinese subjects.
The questionnaire included:
Schooling
School attending, overall results for last term, and overall position in last term.
Household condition
District of residence, type of residence (Public rental housing, Housing Society Flat for Sale Scheme flats, Private residential flats, Other permanent housing (including hotels, hostels and dormitories), Temporary housing (including rooftop structures, mobile dwellings, wooden houses and non-domestic purpose areas, or institutions), area of the living quarters, number of households in the quarters, number of domestic helpers, and average monthly household income, source of income (Employment salary / wages, Comprehensive Social Security Assistance/ Other social Security Scheme, Family’s financial support, Investment, or No income).
Parents (Father and mother)
Highest education level of the parents, presence of refractive error in the parents’ eyes, and degrees of refractive errors.
Medical history
Presence of chronic diseases, eye diseases, whether the child was on treatment for any ocular conditions, presence of refractive errors and age of onset, whether the child was wearing spectacles, the age when spectacles were first prescribed, and whether the child had regular eye checks by an ophthalmologist/optometrist.
Daily activities/habits
Average daily outdoor activities’ time per day during weekdays and weekends, age at which child started having regular exposure to electronic screen products, average duration of using these products each day, purpose of using electronic screen products – for education, entertainment and/or social function, and eye problems related to the use of electronic screen products.
Spherical equivalent (SE) was calculated as the combination of sphere power and ½ cylinder power. The worse eye was defined as the eye with larger absolute value of SE refractive error. Myopia, mild myopia, moderate myopia and high myopia were defined as SE ≤ −0.5D, -3.0D ≤ SE ≤ -0.5D, -6.0D < SE < -3.0D and SE ≤ -6.0 D and/or AL ≥ 26.5mm, respectively. Hyperopia was defined as SE > 0.5D and moderate hyperopia was defined as SE ≥ 2D [9]. Astigmatism was defined as cylinder of -1.00 D or less. Parental myopia was defined whenever either right eye or left eye of mother or father had myopia.
Data analysis
The data were presented in the form of percentage or mean and standard deviation (SD). Data were analysed using SPSS software (version 19.0) and the figures were generated using SPSS software and Prism Graphpad (version 6). A two-tailed P-value of less than 0.05 was considered to be statistically significant.
Pearson correlation was conducted to investigate the correlation of eye examination values between right and left eyes, the association of SE between the children and parents, as well as the association between SE in the children and age of onset. Spearman analysis was conducted to investigate the association of ocular examination values and grades. Independent sample t test was used to compare difference of values between the two groups; R by C chi-square test was used to investigate the difference of sampling distribution from different grades. Univariate and multivariate logistic regression was used to evaluate the risk factors for developing myopia. Odds ratios (OR) and 95% confidence intervals (CIs) were presented.
Results
Demographic characteristics
One thousand four hundred and fifteen children from 4 public primary schools were invited to join this study, 19 of which declined to join. Therefore, data from 1396 children (491 boys), with a mean age of 8.8 years (ranged from 6 to 13 years), were analysed. Boys accounted for 35.2% and Chinese ethnicity accounted for 73.5%. The distribution of subjects enrolled in each school was as follow: Pak Tin Catholic Primary School (234 subjects, 125 boys [53.4%]); S.K.H. Kei Oi Primary School (444 subjects, 171 boys [38.5%]), St. Francis of Assisi’s Caritas School (429 subjects, 110 boys [25.6%]) and Li Cheng Uk Government Primary School (289 subjects, 85 boys [29.4%]). The details of demographic and ocular examination data in different grades of students were shown in Table 1.
Ocular dimensions among grades, gender and ethnicity
Since there was a high correlation in SE, AL, CCT, ACD, KM, WTW between the right and left eyes (all r Pearson ≥ 0.80, P < 0.0001), only the OD data was used to analyse yearly trends of AL, CCT, ACD, KM and WTW. SE was negatively correlated with the grades while the ACD and AL were positively correlated with grades (Fig. 1a, c & g, all P < 0.0001). The AL, ACD and WTW in boys was higher than in girls, while the vertical and horizontal KM in boys were lower than in girls (Fig. 1a, c, d, e & f, all P < 0.0001). We also compared data of Chinese (n = 1026) and non-Chinese (n = 330) students. The difference in ocular dimensions between these 2 groups is shown in Table 2. Chinese children had a statistically significant thinner CCT, shallower ACD and shorter WTW distance. However, no difference was found in SE between the two groups.
Mean annual measures of ocular parameters. Mean annual measures of axial length (a), CCT (b); vertical keratometry (c); horizontal keratometry (d); ACD (e); WTW (f) and spherical equivalent (g); with gender-specific sub-analyses; CCT, central corneal thickness; ACD, anterior chamber depth; WTW, white to white; #, P < 0.1; *, P < 0.05; **, P < 0.01;***, P < 0.001; &, P < 0.0001
Prevalence of refractive errors
Myopia
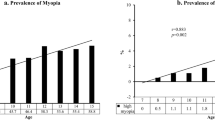
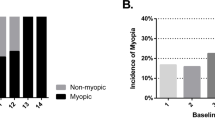
The overall prevalence of myopia in primary school students in Hong Kong was 37.7% (526/1396, 95%CI, [35.1%-40.2%]) based on the worse eye SE. The prevalence of myopia increased significantly with grades. It was 13.3% (34/255, 95%CI, [9.1%-17.5%]), 30.0%(71/237, 95%CI, [24.1%-35.8%]), 42.7%(109/255, 95%CI, [36.6%-48.9%]), 38.1%(93/244, 95%CI, [32.0%-44.3%]), 53.6%(120/224, 95%CI, [47.0%-60.2%]) and 54.7% (99/181, 95%CI, [47.4%-62.0%]) in Grade 1, 2, 3, 4, 5 and 6 respectively (Table 3, Fig 2). There was no statistically significant difference between the prevalence of myopia in boys and girls (39.5%, 194/491, 95%CI, [35.2%-43.9%]) vs 36.7%, 332/905,95%CI, [33.5%-39.8%]), P = 0.30).
The overall prevalence of moderate myopia was 8.4% (117/1396, 95%CI, [6.9%-9.8%]), which increased significantly with years, from 1.6%(4/255, 95%CI, [0.4%-4.0%]) at Grade 1 to 18.2% (33/181, 95%CI, [12.6%-23.9%]) at Grade 6 (Table 3). The overall prevalence of high myopia in primary school students was 1.4%(19/1396, 95%CI[0.8%-2.0%]), which increased from 0.94% (7/747, 95%CI[0.2%-1.6%]) in lower grade students (Grade 1 to Grade 3) to 1.85% (12/649, 95%CI[0.8%-2.9]) in higher grade students (Grade 4 to Grade 6) (Data from students from different grades were grouped for analysis because of the small number if analysed individually).
Awareness of refractive errors
The overall prevalence of refractive error (myopia or hyperopia) was 54.4% (759/1396, 95%CI [51.8%-57.0%]) among which only 35.7% (271/759, 95%CI, [32.3%-39.1%]) of the parents were aware and 32.5% (247/759, 95%CI, [29.2%-35.9%]) of the children wore glasses. Among the students with myopia, only 40.3% (216/526, 95%CI, [36.1%-44.5%]) of the parents knew their children had myopia and only 39.0% (205/526, 95%CI, [34.8%-43.2%]) of the children wore glasses. As shown in Table 4, low myopic students had lowest awareness of their myopia, only 34.4% (134/390), while in moderately myopic children 59.8% and in high myopic children 63.2% were aware of their myopia. As shown in table 1, only around 50% children passed the VA test (logMAR VA less than 0.2) with their current vision (with current spectacles if they had been prescribed one), while around 85% children passed the VA test after all refractive errors were corrected. At Grade 6, 97% of the children has BCVA <0.2 LogMAR, but only around 60% passed the VA test with uncorrected vision.
Association between myopia degree and degree of parental refractive error
The association between the degree of myopia (SE in worse eye) of the children and their parents, as well as its association with the age of students and the age of onset of myopia were analyzed. The degree of myopia in the worse eye was negatively associated with age (Fig. 3a, r = -0.13, P = 0.003, n = 486), suggesting that the younger the student is, the less degree of myopia. The degree of myopia was positively associated with the age at which myopia was initially diagnosed (Fig. 3b, r = 0.18, P = 0.013, n = 186), indicating that with a younger age of onset, one would develop a higher degree of myopia. However, the degree of myopia in the worse eye of the students was not associated with the degree of refractive error in the fathers (r = 0.05, P = 0.51, n = 178) or mothers (r = -0.03, P = 0.70, n = 180). We further investigated whether there was any correlation between the degree of myopia and parental myopia. With neither of the parents having myopia, 21.30% of the students had moderate or high myopia, whereas 30.77% of those having moderate or high myopia, had at least one of their parents having myopia. The difference is statistically significant (χ2 = 5.25, P = 0.02). Among the 19 children with high myopia, 3 failed to report any refractive errors, 6 parents (mother or father or both) had myopia higher than -5D, 4 parents had moderate myopia and 6 parents had no refractive errors.
Risk factors for the development of myopia
The risk factors for the presence of myopia are shown in Table 5. In a univariate model, older children (OR, 1.42; P = 0.000), better academic ranking in class in the preceding semester (OR,1.02 [1/0.98]; P = 0.007), absence of routine eye checks (OR, 1.92[1/0.52]; P = 0.004), younger age of exposure to electronic devices (P = 0.004), longer duration of using electronic screen products each day (P = 0.005), using electronic devices for social purpose (OR, 1.59 [1/0.63]; P = 0.01) and having eye problems related to the use of electronic screen products (OR, 3.23[1/0.31]; P = 0.000) were associated with presence of myopia. In multivariate logistic regression analysis, parameters with p value less than 0.05 in univariate analysis were put in multivariate logistic regression as covariates. After adjusting the covariates, myopia was only significantly associated with older age (OR,1.36; P=0.01), better academic ranking in class in the preceding semester (OR, 1
.01[1/0.99]; P=0.03) and absence of routine eye check (OR, 2.63 [1/0.38]; P=0.001).
Hyperopia
The overall prevalence of hyperopia based on the worse eye was 16.7% (233/1396, 95%CI [14.8%-18.7%]) and the overall prevalence of moderate hyperopia was 1.0%(14/1396, 95% CI, [0.5%-1.5%]). The prevalence of hyperopia decreased with school grades, from 27.5% (70/255, 95%CI, [21.9%-33.0%]) in grade 1 to 9.4%(17/181, 95%CI, [5.1%-13.7%]) in grade 6 (P=0.00, Table 3).
Astigmatism
The overall prevalence of astigmatism based on the worse eye was 28.8%. There was no difference in the prevalence of astigmatism among different grades (P>0.05, Table 3).
Discussion
Prevalence of myopia in Hong Kong
Hong Kong is one of the regions with the highest prevalence of myopia in the world [2, 3]. The reported overall prevalence of myopia in primary school students in Hong Kong was 36.71% in 1998-2000[10] and 47.5% in 2005-2010 [2].
Ours was the largest cross-sectional study in the recent 10 years and it demonstrates the prevalence of myopia in primary school students in Hong Kong. The overall prevalence of myopia reported at the four primary schools surveyed was 37.7%, similar to a study conducted in 1998-2000 [10] but appeared to be lower than the later study in 2005-2010 [2]. This suggests that, although the prevalence of myopia remains high, there is a possible trend of decline. Another study in 1991-1996 [11] followed up children from the age of 7 (equivalent to Grade 2), until 12 years old (equivalent to just beyond Grade 6), to evaluate the development and progression of myopia. That study demonstrates a higher prevalence of myopia, although the sample size was relatively small, 123 subjects at baseline only, thus rendering a possibility of selection bias. A comparison of the different studies conducted in Hong Kong on the prevalence of myopia in primary school students is summarized in Table 6.
The prevalence of moderate myopia in our study was less than that in 1998-2000 (8.6% vs 9.5%) but the prevalence of high myopia remains nearly the same as in previous studies (1.4% in our study vs 1.19% in 1998-2000 [2] and 1.8% in 2005-2010 [2, 10]). Evidence from meta analysis has demonstrated that Orthokeratology (OK lenses) and atropine are effective in slowing the progression of axial elongation [12, 13]. Previously, OK lenses had been the most popular method of myopia control in Hong Kong [14, 15]. Nowadays, after preservative-free 0.01% atropine has become available, that method gained popularity because it is free from the potential sight-threatening complications of OK lenses, infective keratitis in particular. Although environmental conditions have not changed, there has been an increase in the use of myopia controlling measures, low-dose atropine eye drops in particular, to which the decrease in myopia over the past ten years can be attributed. Yet, the prevalence of myopia among primary school students in Hong Kong is stil high. More than 1 in 3 primary school students have myopia; 13% of Grade 1 students already had developed myopia by the time they entered school, and in Grade 6, more than half of the students have myopia. This is significantly higher than that reported in major cities in China, like Beijing and Shanghai. The prevalence of myopia in Shanghai in 2016 was 3.4%, 6.0%, and 12.7% in children aged 6, 7 and 8 year olds respectively [16]. In Urban Beijing, myopia in children aged 7 to 11 years was 11.7%, 14.6%, 31%, 37%, 46.7% respectively (data published in 2014) [17]. It is shown that the earlier the onset of myopia, the faster the progression and the higher the chance that pathologic myopia would develop [7, 18, 20]. The development of high myopia was also more rapid in the period of secondary school at the age of around 13-18 years old [21]. If more than half of the students already had myopia by the end of primary school, it is likely that a high proportion of them will develop high myopia. Pathologic myopia is associated with sight-threatening conditions, including atrophic maculopathy, choroidal neovascularization, and retinal detachment. Higher SE, longer AL and older age were found to be risk factors of pathologic myopia [22, 23]. If almost 4% of myopic primary school children already have high myopia at a young age, we can foresee a high chance of them developing sight threatening complications later in life. Early intervention of myopia control in this group of children should be promoted, particularly in those with myopia onset at a younger age.
Awareness of refractive errors
WHO estimates that 12.8 million children aged 5–15 years are visually impaired from uncorrected or inadequately corrected refractive errors worldwide [24] In Hong Kong, it is also worrying that a significant proportion of the children who ought to be wearing spectacles, are not doing so. Only around 50% children passed the VA test without correction, whereas, with proper correction, 85% did pass the VA test. Hence, given sufficient spectacle correction 35% of the students could have improved vision. Globally, the main factors for non-correction of refractive errors include lack of awareness, non-availability and/or non-affordability of ocular examination, non-affordability of corrective lenses as well as cultural issues [24]. In Hong Kong, optometrists and opticians are readily available and the price of corrective lenses is affordable. Therefore, lack of awareness of the need for refrective correction may be the major contributing factors. Our results show that among children with myopia, only 19.4 % of the parents knew their children had refractive errors and only 17.7% of the children wore glasses. There is also a misconception by parents that, once the children start wearing glasses, the degree of myopia would progress more rapidly. Therefore, even if they are told their children need glasses, many of the parents are reluctant to have their children wear glasses. This is especially a problem with children below the age of 8 years, because of the chance of amblyopia if they are not provided with proper glasses. Moreover, undercorrection of myopia might affect the academic performance of the students, since they may not be able to see the blackboard or screen clearly. They may not be able to focus and tend to be distracted from the teaching. Parents’ education should emphasize that the importance of optimal correction of their children’s vision, especially before the age when amblyopia may develop. In addition, the children, especially those in lower grades, might not be able to inform the grown ups of their difficulties. Parents need to have their children get regular eye checks to screen for any refractive errors, and to correct them in time. Amblyopia is potentially reversible if detected early, but the number of cases will only increase if there will be no improvement in the current situation.
Age and parental factors’ influence on myopia prevalence
The degree of myopia in the worse eye was positively associated with age at which myopia was initially diagnosed, indicating that the younger the age of onset, the higher the degree of myopia [18, 19, 20]. This was in line with our regression analysis that the prevalence of myopia is significantly associated with older age. Hence, treatment would start at as young an age as possible so that the development of myopia can be arrested at its inception.
It is believed that myopia is caused by a combination of genetic and environmental factors. However, there are also suggestions that the hereditary factors transmitted from parents to children affect ocular dimensions, such as AL, corneal radius, ACD, rather than refraction [25]. Whether parental myopia is associated with myopia in children remains controversial. Some studies demonstrate that parental myopia was linked to myopia in their children [26, 27], while others did not identify any association. Similar to some previous studies [25, 28], our study shows that the degree of parental refractive error is not associated with myopia degree in the children. However, as the information of parental refractive error was by self-reported questionnaire, there was possibly some discrepany between their exact refractive error compared to that reported. Although 1180 parents reported a refractive status, only 180 parents reported the exact degree of their refractive error.
Nonetheless, we identified a higher proportion of moderate or high myopia in children with parental myopia, suggesting that children with parental myopia were more likely to develop moderate or high myopia. In the 16 children with high myopia who reported their degree of myopia, 6 had at least one parent with high myopia.
Risk factors for the presence of myopia
Use of electronic devices by children
The use of electronic devices is common among primary school students. Apart from social reasons, many require electronic devices for school work. The effect of near work on myopia development has been extensively studied for years. However, the results are inconsistent. Some studies suggest longer time of near work increases the risk of myopia development or progression [29, 30], while others do not. A study of 835 myopic children reports that near work including studying, watching TV, using computers or playing games did not increase the risk of myopia progression [31]. Results from the Sydney Myopia Study on 1781 year-7 children do not suggest a correlation between near work and myopia progression [32]. In Lin et al’s study, although myopic children were found to spend more time on near work, the results from multiple logistic regression do not suggest any correlation between near work and myopia [33]. In our study, univariate analysis showed age of exposure to electronic devices had an additional 19%, and average duration of using electronic screen products each day a 13% risk of myopia development. On the other hand, not using electronic devices for social purpose and absence of eye problems related to the use of electronic screen have 37% (P = 0.06) and 69% risk reduction in myopia development. However, these parameters were not associated with the myopia development after adjustment for confounding variables in the multiple logistic regression, suggesting that they were not independent risk factors for myopia development. Most of the students reported a daily use of electronic devices of less than 2 hours. If the schools are to advocate the use of electronic devices for teaching and assignments, the children will likely need to use the devices for more than 2 hours a day. Whether long use of electronic devices might impose a negative impact on ocular health will require further evaluation.
Outdoor activities
Most recent studies demonstrate that outdoor activity time helps prevent myopia onset and progression [34, 35]. This was not observed in our study. However, in the original questionnaire, 97 children reported that their average daily outdoor activity time on weekdays is > 4 hours (some even up to more than 8 hours) and 103 children reported that their average daily outdoor activity time on weekends is > 6 hours. This is probably due to a misunderstanding on the children’s part as, considering the education system in Hong Kong, it is impossible for a child to spend these long hours outdoors. We suspect that some children confused the daily outdoor activity time with total outdoor activity time per week. We have excluded the data of > 4 hours (n = 97) of daily outdoor activities on weekdays and > 6 hours (n = 103) on weekends from the analysis. After excluding the unlikely data, univariate analysis showed that weekday outdoor activity time, OR 1.10 (P = 0.14) and weekend outdoor activity time, OR 0.97 (P = 0.50), were not associated with presence of myopia.
Older age, absence of routine eye check and better academic ranking in class in the preceding semester were independent risk factors for the presence of myopia in Hong Kong
In this study, multivariate analysis showed the independent risk factors for the myopia onset to be older age, lack of routine eye check and better academic ranking in class in the preceding semester. As in previous studies [7, 36, 37] children of older age had a higher risk of myopia development. In addition, our study was the first to report that routine eye checks are associated with a lower risk of myopia development in 63% of cases. This might be because parents with higher awareness to children’s eye health would be more interested in taking the necessary steps to prevent myopia development. In addition, early intervention, such as wearing appropriate corrective eyewear, using orthokeratology lenses or 0.01% atropine, would be helpful in halting myopia development and progression [38, 39]. In addition, this study also suggests that better academic ranking in class during the preceding semester was associated with a higher risk of myopia development (P = 0.03). Children with better academic performance in general devote more time to revision and studying, which involves near work. This can result in myopia progression. However, we had not explored in this study whether near work was associated with myopia development. In addition, since the OR was only 1.01(1/0.99) (95% CI [1.00-1.03(1/0.97)]), although there is a statistical significance, whether this result indicates any clinical values should be verified by future work.
Limitations of this study
The limitations of our study include a possibility of sampling error as the data were collected from 4 public primary students in Sham Shui Po district. Traditionally, there is a higher proportion of residents from lower socioeconomic classes in this district. Myopia was found to be related to the socioeconomic status [40], so this particular population may not be representative of the entire Hong Kong population. However, this serves as a pilot study, and we can extend it by collecting data from primary schools from different districts in Hong Kong. In addition, the refractive error was determined based on non-cycloplegic refraction. Therefore, the myopia prevalence and the myopia degree might be overestimated in this study. Furthermore, the questionnaires depend on self-reporting from parents. There are some missing data, and the information they provide might not be completely accurate. In future studies, the refractive status of the parents can also be measured, which would likely give more reliable results.
To conclude, our results show that there was a high prevalence of myopia among primary school students, and the prevalence increased with age. Despite the accessibility of eye-care service across Hong Kong, around two-thirds of the children and their parents were not aware of the children’s refractive errors, and many of them could have had vision improved with appropriate corrective glasses. This highlights the importance of regular eye checks. At the same time, 3% of parents were reluctant to prescribe glasses for their children even if they were aware of them having refractive error. This indicates that more public education may be required to clear the misconception among the population.
References
Edwards MH, Lam CS. The epidemiology of myopia in Hong Kong. Ann Acad Med Singap. 2004;33:34–8.
Lam CS, Lam CH, Cheng SC, Chan LY. Prevalence of myopia among Hong Kong Chinese schoolchildren: changes over two decades. Ophthalmic Physiol Opt. 2012;32:17–24.
Morgan IG, French AN, Ashby RS, Guo X, Ding X, He M, et al. The epidemics of myopia: aetiology and prevention. Prog Retin Eye Res. 2018;62:134–49.
Cheng SC, Lam CS, Yap MK. Prevalence of myopia-related retinal changes among 12-18 year old Hong Kong Chinese high myopes. Ophthalmic Physiol Opt. 2013;33:652–60.
Loh KL, Lu Q, Tan D, Chia A. Risk factors for progressive myopia in the atropine therapy for myopia study. Am J Ophthalmol. 2015;159:945–9.
Pineles SL, Kraker RT, VanderVeen DK, Hutchinson AK, Galvin JA, Wilson LB, et al. Atropine for the prevention of myopia progression in children: a report by the American Academy of Ophthalmology. Ophthalmology. 2017;124:1857–66.
Hyman L, Gwiazda J, Hussein M, Norton TT, Wang Y, Marsh-Tootle W, et al. Relationship of age, sex, and ethnicity with myopia progression and axial elongation in the correction of myopia evaluation trial. Arch Ophthalmol. 2005;123:977–87.
Tan NW, Saw SM, Lam DS, Cheng HM, Rajan U, Chew SJ. Temporal variations in myopia progression in Singaporean children within an academic year. Optom Vis Sci. 2000;77:465–72.
Ip JM, Robaei D, Kifley A, Wang JJ, Rose KA, Mitchell P. Prevalence of hyperopia and associations with eye findings in 6- and 12-year-olds. Ophthalmology. 2008;115(678–85):e1.
Fan DS, Lam DS, Lam RF, Lau JT, Chong KS, Cheung EY, et al. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Investig Ophthalmol Vis Sci. 2004;45:1071–5.
Edwards MH. The development of myopia in Hong Kong children between the ages of 7 and 12 years: a five-year longitudinal study. Ophthalmic Physiol Opt. 1999;19:286–94.
Li SM, Kang MT, Wu SS, Liu LR, Li H, Chen Z, et al. Efficacy, safety and acceptability of orthokeratology on slowing axial elongation in myopic children by meta-analysis. Curr Eye Res. 2016;41:600–8.
Gong Q, Janowski M, Luo M, Wei H, Chen B, Yang G, et al. Efficacy and adverse effects of atropine in childhood myopia: a meta-analysis. JAMA Ophthalmol. 2017;135:624–30.
Charm J, Cho P. High myopia-partial reduction ortho-k: a 2-year randomized study. Optom Vis Sci. 2013;90:530–9.
Cho P, Tan Q. Myopia and orthokeratology for myopia control. Clin Exp Optom. 2018;102:364–77.
He X, Sankaridurg P, Xiong S, Li W, Zhang B, Weng R, et al. Shanghai time outside to reduce myopia trial: design and baseline data. Clin Exp Ophthalmol. 2019;47:171–8.
You QS, Wu LJ, Duan JL, Luo YX, Liu LJ, Li X, et al. Prevalence of myopia in school children in greater Beijing: the Beijing Childhood Eye Study. Acta Ophthalmol. 2014;92:e398–406.
Chua SY, Sabanayagam C, Cheung YB, Chia A, Valenzuela RK, Tan D, et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol Opt. 2016;36:388–94.
Parssinen O, Kauppinen M. Risk factors for high myopia: a 22-year follow-up study from childhood to adulthood. Acta Ophthalmol. 2018;97:510–8.
Chen Y, Zhang J, Morgan IG, He M. Identifying children at risk of high myopia using population centile curves of refraction. PLoS One. 2016;11:e0167642.
Chen Y, Shi Y, Yang L. Tendency for evolution of high myopia in 308 Chinese school children from Xi’an city. Eye Sci. 2014;29:36–42.
Asakuma T, Yasuda M, Ninomiya T, Noda Y, Arakawa S, Hashimoto S, et al. Prevalence and risk factors for myopic retinopathy in a Japanese population: the Hisayama Study. Ophthalmology. 2012;119:1760–5.
Xiao O, Guo X, Wang D, Jong M, Lee PY, Chen L, et al. Distribution and severity of myopic maculopathy among highly myopic eyes. Investig Ophthalmol Vis Sci. 2018;59:4880–5.
Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008;86:63–70.
Goldschmidt E, Jacobsen N. Genetic and environmental effects on myopia development and progression. Eye (Lond). 2014;28:126–33.
Zhang X, Qu X, Zhou X. Association between parental myopia and the risk of myopia in a child. Exp Ther Med. 2015;9:2420–8.
Lim DH, Han J, Chung TY, Kang S, Yim HW. The high prevalence of myopia in Korean children with influence of parental refractive errors: the 2008–2012 Korean National Health and Nutrition Examination Survey. PLoS One. 2018;13:e0207690.
Guggenheim JA, Kirov G, Hodson SA. The heritability of high myopia: a reanalysis of Goldschmidt’s data. J Med Genet. 2000;37:227–31.
Saw SM, Zhang MZ, Hong RZ, Fu ZF, Pang MH, Tan DT. Near-work activity, night-lights, and myopia in the Singapore-China study. Arch Ophthalmol. 2002;120:620–7.
Huang HM, Chang DS, Wu PC. The association between near work activities and myopia in children-a systematic review and meta-analysis. PLoS One. 2015;10:e0140419.
Jones-Jordan LA, Sinnott LT, Cotter SA, Kleinstein RN, Manny RE, Mutti DO, et al. Time outdoors, visual activity, and myopia progression in juvenile-onset myopes. Investig Ophthalmol Vis Sci. 2012;53:7169–75.
Ip JM, Huynh SC, Robaei D, Rose KA, Morgan IG, Smith W, et al. Ethnic differences in the impact of parental myopia: findings from a population-based study of 12-year-old Australian children. Investig Ophthalmol Vis Sci. 2007;48:2520–8.
Lin Z, Gao TY, Vasudevan B, Ciuffreda KJ, Liang YB, Jhanji V, et al. Near work, outdoor activity, and myopia in children in rural China: the Handan offspring myopia study. BMC Ophthalmol. 2017;17:203.
Dirani M, Tong L, Gazzard G, Zhang X, Chia A, Young TL, et al. Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol. 2009;93:997–1000.
Wu PC, Tsai CL, Wu HL, Yang YH, Kuo HK. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology. 2013;120:1080–5.
Theophanous C, Modjtahedi BS, Batech M, Marlin DS, Luong TQ, Fong DS. Myopia prevalence and risk factors in children. Clin Ophthalmol. 2018;12:1581–7.
Guo Y, Liu LJ, Xu L, Lv YY, Tang P, Feng Y, et al. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology. 2013;120:277–83.
Sun Y, Xu F, Zhang T, Liu M, Wang D, Chen Y, et al. Orthokeratology to control myopia progression: a meta-analysis. PLoS One. 2015;10:e0124535.
Chia A, Lu QS, Tan D. Five-year clinical trial on atropine for the treatment of myopia 2: myopia control with atropine 0.01% eyedrops. Ophthalmology. 2016;123:391–9.
Wong TY, Foster PJ, Johnson GJ, Seah SK. Education, socioeconomic status, and ocular dimensions in Chinese adults: the Tanjong Pagar Survey. Br J Ophthalmol. 2002;86:963–8.
Acknowledgements
The study was partly supported by Eye Care Charitable Foundation
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
B.N.K.Choy, None; Q.You, None; M.M.Zhu, None; J.S.M.Lai, None; A.L.K.Ng, None; I.Y.H.Wong, None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Ian Yat Hin Wong
About this article
Cite this article
Choy, B.N.K., You, Q., Zhu, M.M. et al. Prevalence and associations of myopia in Hong Kong primary school students. Jpn J Ophthalmol 64, 437–449 (2020). https://doi.org/10.1007/s10384-020-00733-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-020-00733-4