Abstract
Purpose
To verify, by use of data collected by the Japan Glaucoma Society Survey of Bleb-related Infection (JGSSBI), that bleb morphology changes within 12 months of the development of bleb-related infection.
Methods
JGSSBI data from 57 eyes of 57 patients with primary open-angle glaucoma and normal tension glaucoma who developed a bleb-related infection were analyzed. Morphological features of the blebs were graded by use of a predetermined grading system. Multiple logistic regression analysis was conducted to identify factors relating to bleb morphology which were associated with poor outcome.
Results
Bleb sizes, including both circumferential and tangential lengths, were significantly smaller for stage IIIa/IIIb infections than for stage I/II bleb infections (P = 0.009 and P = 0.026 for the circumferential and tangential lengths, respectively; Fisher’s direct probability test). The bleb wall also became significantly thicker during stage IIIa/IIIb infections (P = 0.003). After infection, intraocular pressure (IOP) increased significantly for all cases but was no different in the three subgroups (i.e. stage I, stage II, and stage IIIa/IIIb bleb infections). Multiple logistic regression analysis revealed that a stage III infection was significantly associated with a poor outcome for the bleb.
Conclusions
This study revealed that the filtering bleb became smaller, both tangentially and circumferentially, and thicker, after stage III infections than after stage I or II infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bleb-related infection is a condition requiring immediate care for glaucoma patients with a history of filtering surgery [1–5]. It rapidly progresses to more advanced stages and often causes severe visual disturbance. It may also negatively affect intraocular pressure (IOP) [6, 7]. The causes of IOP elevation are variable, and can include degeneration of the trabecular meshwork, formation of peripheral anterior synechiae, and other causes. Dysfunction of the filtering bleb, however, is suspected to contribute to uncontrolled IOP in most cases, because inflammatory reactions at the bleb site cause vasodilation, production of inflammatory cytokines, and other problems, resulting in fibrosis at and around the filtering bleb [8, 9]. It is well known that bleb morphology is highly correlated with IOP control [10, 11], and that bleb size and intra-bleb reflectivity have predictive value for IOP after filtering surgery.
The Japan Glaucoma Society conducted a 5-year-long, multicenter survey on bleb-related infection [12–14]. The Japan Glaucoma Society Survey of Bleb-related Infection (JGSSBI) found that stage III bleb-related infection, i.e. infections with vitreous involvement, caused significant visual loss and elevation of IOP within 12 months of development. Because IOP control depends on the function of a filtering bleb, bleb morphology may have changed after resolution of infections with vitreous involvement. In this study we used the JGSSBI data to analyze changes in bleb morphology for open-angle glaucoma.
Materials and methods
The data used in this study were obtained from the JGSSBI. The details of the JGSSBI are described elsewhere [12, 13]. Briefly, this prospective study was conducted during a surveillance period of 5 years in which all patients with bleb-related infection from 82 medical centers in Japan were consecutively registered, and clinical and microbial data were collected. Management of the bleb-related infection was at the discretion of local investigators. Institutional review board approval was obtained at 46 centers. The Ethics Review Board of Gifu University Hospital approved the study protocol for the other 36 centers, for which there was no governing institutional review board, on the condition that the study would be conducted under the guidance of Gifu University Hospital. All patients gave written informed consent after receiving a thorough explanation of the study, and each gave permission for use of their individual data for scientific research on the condition of anonymity. The Japan Glaucoma Society approved our use of the data for this study and provided the anonymized data.
Each infection was classified into one of three stages in the JGSSBI [15, 16]: stage I denotes infections confined to the bleb site with a mild cell reaction in the anterior chamber; stage II denotes infections in which the anterior chamber is the main locus and the vitreous is not involved; stage III denotes infections involving the vitreous. Stage III is subdivided into two stages: IIIa denotes mild involvement of the vitreous and IIIb denotes more advanced involvement [17, 18].
The eyes analyzed in this study were selected from a total of 146 eyes of 146 patients for whom 6 and/or 12-month follow-up data were available after bleb-related infection [13]. Six-month data were available for 134 eyes and 12-month data for 112 eyes. The selection criteria were:
-
primary open-angle glaucoma (POAG) and normal tension glaucoma (NTG); and
-
availability of bleb morphology grading pre and post-infection on the basis of a predetermined grading system (Table 1).
We investigated changes in bleb morphology after infection and compared the morphology from pre-infection to the last follow-up. In this study, we assigned bleb infections to two subgroups (stage I/II infections and stage IIIa/IIIb infections) to determine whether infectious propagation into the vitreous cavity affected bleb morphology. The morphological features included size (both circumferential and tangential), height, border, wall thickness, avascularity, and leakage of the bleb. If 12-month follow-up data were available, they were also analyzed in this study; if not, only the 6-month data were analyzed.
To determine which factors are associated with poor outcomes of filtering blebs, we conducted multiple logistic regression analysis. A poor outcome was regarded as having occurred when the bleb size (circumferentially or tangentially) was smaller, or the bleb wall was thicker, after infection. Age, gender, being stage III, type of conjunctival incision, type of glaucoma surgery, and pre-infection IOP were considered as potentially associated factors. Independent factors were regarded as significant at values of <0.05 when forward stepwise variable selection was used.
Statistical analysis was conducted by use of IBM SPSS statistics software version 20.0 (IBM Japan, Tokyo, Japan). P values <0.05 were regarded as statistically significant.
Results
On the basis of the selection criteria we included in this study a total of 57 eyes of 57 patients. Reasons for exclusion were glaucoma subtypes other than POAG and NTG for 72 eyes and incomplete availability of bleb morphology grading pre and post-infection for 17 eyes. Of the 57 eyes, 6-month data were available for 56 eyes and 12-month data for 49 eyes. Thus, 12-month follow-up data were analyzed for 49 eyes and 6-month data were analyzed for the other 8 eyes. Relevant background data for the subjects are shown in Table 2. All eyes were intensively treated with antibiotic therapy and surgery when indicated. Vitreous surgery was performed on 15 eyes.
IOP increased significantly from 10.0 ± 3.7 mmHg pre-infection (mean ± standard deviation (SD)) to 11.2 ± 4.6 mmHg after infection for all cases (Table 3). However, IOP was not significantly different in the 3 subgroups (i.e. stage I, stage II, and stage IIIa/IIIb bleb infections). After resolution of the bleb-related infection, twenty eyes (35.1 %) required ocular hypotensive drugs and 9 (15.8 %) needed revision of their trabeculectomy bleb (Table 4).
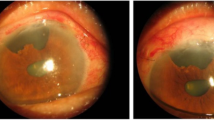
Bleb morphology changes are listed in Table 5. Bleb sizes, both circumferential and tangential lengths, were significantly smaller in stage IIIa/IIIb infections than in stage I/II infections (P = 0.009 and P = 0.026 for circumferential length and tangential length, respectively; Fisher’s direct probability test). The bleb wall also became significantly thicker in stage IIIa/IIIb infections (P = 0.003; Fisher’s direct probability test). Bleb height, bleb border, and surface vascularity did not change significantly (P = 0.161, P = 0.214, and P = 0.614, respectively; Fisher’s direct probability test). In the eyes in which bleb leakage had been observed before infection, the rate of leakage after infection did not change significantly (P = 0.194; Fisher’s direct probability test).
IOP was 10.7 ± 5.2 mmHg (mean ± SD) for eyes for which bleb circumferential length was shorter after infection and 11.4 ± 4.5 mmHg (mean ± SD) for eyes with either unchanged or longer blebs, but the difference between the two groups was not significant (P = 0.450, Mann–Whitney U test). IOP was 12.3 ± 6.9 mmHg (mean ± SD) for eyes for which bleb tangential length that was shorter after infection and 11.0 ± 4.1 mmHg (mean ± SD) for those for which it was either unchanged or longer, but the difference between the two groups was not significant (P = 0.570, Mann–Whitney U test). IOP was 10.7 ± 6.7 mmHg (mean ± SD) for eyes with a bleb wall thickness that was thicker and 11.3 ± 4.4 mmHg (mean ± SD) for eyes that were either unchanged or thinner, but this difference was not significant (P = 0.730, Mann–Whitney U test). The IOP of eyes for which bleb leakage had been observed before infection was not significantly different after infection, irrespective of whether the leakage persisted or was resolved. (9.9 ± 3.8 and 10.6 ± 3.3 mmHg, respectively; P = 0.837, Mann–Whitney U test). In addition, IOP was 13.1 ± 5.9 mmHg for those treated with vitrectomy and 10.6 ± 4.0 mmHg for those left untreated (P = 0.076, Mann–Whitney U test).
Multiple logistic regression analysis revealed that stage III infection was significantly associated with a poor outcome of the bleb (Table 6). Bleb size (both circumferentially and tangentially) tended to be smaller and the bleb wall tended to be thicker for stage III eyes after infection.
Discussion
We performed a sample-size calculation before this study. We hypothesized that bleb-related infection significantly affects bleb morphology in stage III infections but has little effect in stages I or II. In the JGSSBI report the ratio of stages I or II to stage III infections was 100:46 [13]. On the basis of our estimate that bleb morphology would be changed in 50 % of eyes with stage III infections within 1 year, but would change in only 5 % of eyes with stage I or II infections, we calculated a minimum sample size of 36 eyes in total (24 eyes for stage I or II and 12 eyes for stage III) to provide a two-sided significance level of 0.05 and a power of 0.8 in a chi-squared test. In our previous study [19] we observed poor IOP control of more than 21 mmHg in 4.6 % of cases with stage I or II infections and uncontrolled IOP in 36.4 % of cases with stage III infections. Because IOP control depends upon the function of a filtering bleb, we set values of 50 % and 5 % in this study. However, the actual number of eyes analyzed was 57 (45 eyes for stage I or II and 12 eyes for stage III), which exceeded the estimated minimum sample size.
This study revealed that the filtering bleb became smaller, both tangentially and circumferentially, and thicker after stage III infections than after stage I or II infections, i.e. stage III bleb-related infections resulted in the most significant changes in bleb morphology. This finding is in good agreement with increases in IOP in stage III bleb-related infections reported by the JGSSBI [13]. The IOP increased significantly in all the cases in this study, all of which were selected from the JGSSBI cases, whereas significantly different IOP was not observed in the subgroups. Further, IOP after infection was no different in eyes with morphological changes in the bleb and in those without. Bleb-related infections are reported to develop in 2.2 % of cases within 5 years after trabeculectomy or trabeculectomy combined with cataract surgery with adjunctive mitomycin C [18]. Because stage III infection is a more severe form of bleb-related infection, it may cause more profound inflammation which can result in more significant visual deterioration and IOP elevation.
The bleb classification system we used here is unique. It was adopted for description of bleb morphology in the two independent prospective studies on bleb-related infection conducted by the Japan Glaucoma Society (JGSSBI) [12, 13] and by the Collaborative Bleb Infection Incidence and Treatment Study (CBIITS) [18, 19]. Several bleb-grading systems are used internationally, for example the Moorfields Bleb Grading System [20, 21], the Indiana Bleb Appearance Grading System [21, 22], and the Wuerzburg bleb classification score [23]. Each of these systems regards bleb morphology as closely related to the outcome of filtering surgery; the system we used focuses on the circumferential and tangential length of the bleb.
Our findings showed that after resolution of bleb-related infection, changes in bleb size and wall thickness were different for the milder (stages I and II) and more severe (stages IIIa and IIIb) stages whereas other features, for example bleb height, bleb border appearance, and degree of avascularity, were not. Although we cannot fully explain why bleb height and border appearance did not change whereas size and thickness did change, it is nevertheless likely that in most cases the changes in these features may be correlated. On the basis of our findings we speculate that bleb size and bleb wall thickness are indicative of a failing bleb. Ultrasound biomicroscopy and anterior segment optical coherence tomography have shown that bleb size, intra-bleb structure, and intra-bleb reflectivity are closely associated with bleb function [10, 11].
This study has several limitations. First, we adopted a new bleb classification system that was unfamiliar to some of the JGSSBI researchers and so may have been a source of variation in grading. Although the reproducibility of this bleb classification has yet to be reported, it would show a better agreement because of a simpler bleb grading system than others and high reproducibility reported on other bleb grading systems [20–23]. However, we did expect this challenge and it was addressed during researcher meetings both before and annually during the JGSSBI study period. Second, some researchers did not report bleb morphology; data were missing for 23 % (17/74) of POAG and NTG. Lack of a predetermined treatment protocol and the missing data might have weakened our conclusions, as pointed out previously [13]. Third, medical and surgical intervention after the development of bleb-related endophthalmitis, including vitrectomy and different ocular hypotensive therapy, were not taken as potential associated factors in the multiple logistic regression analysis. Such intervention may affect bleb morphology. In this study no absolute definite therapeutic procedure was adopted after settling endophthalmitis with regard to which anti-glaucoma agents were prescribed and whether surgical intervention was performed. Despite these limitations we believe our central findings remain relevant because of the prospective nature of the JGSSBI data, the relatively large number of cases, and the strict enrollment criteria, enrollment being restricted to POAG and NTG cases only.
This study showed that, after resolution of bleb-related infections, bleb morphology worsens more often during stage III infection than during milder cases. Bleb-related infection with vitreous involvement is not only undesirable from the perspective of visual outcome, it also negatively affects IOP control. Early detection of bleb-related infection, and prompt intervention, is clearly important.
References
Leng T, Miller D, Flynn HW Jr, Jacobs DJ, Gedde SJ. Delayed-onset bleb-associated endophthalmitis (1996–2008): causative organisms and visual acuity outcomes. Retina. 2011;31:344–52.
Ciulla TA, Beck AD, Topping TM, Baker AS. Blebitis, early endophthalmitis and late endophthalmitis after glaucoma-filtering surgery. Ophthalmology. 1997;104:986–95.
Kangas TA, Greenfield DS, Flynn HW, Parrish RK, Palmberg P. Delayed-onset endophthalmitis associated with conjunctival filtering blebs. Ophthalmology. 1997;104:746–52.
Higginbotham EJ, Stevens RK, Musch DC, Karp KO, Lichter PR, Bergstrom TJ, et al. Bleb-related endophthalmitis after trabeculectomy with mitomycin C. Ophthalmology. 1996;103:650–6.
Bayraktar Z, Kapran Z, Bayraktar S, Acar N, Unver YB, Gök K. Delayed-onset streptococcus pyogenes endophthalmitis following Ahmed glaucoma valve implantation. Jpn J Ophthalmol. 2005;49:315–7.
Greenfield DS, Suñer IJ, Miller MP, Kangas TA, Palmberg PF, Flynn HW Jr. Endophthalmitis after filtering surgery with mitomycin. Arch Ophthalmol. 1996;114:943–9.
Song A, Scott IU, Flynn HW, Budenz DL. Delayed-onset bleb-associated endophthalmitis: clinical features and visual acuity outcomes. Ophthalmology. 2002;109:985–91.
Engel LA, Muether PS, Fauser S, Hueber A. The effect of previous surgery and topical eye drops for primary open-angle glaucoma on cytokine expression in aqueous humor. Graefes Arch Clin Exp Ophthalmol. 2014;252:791–9.
Freedman J, Iserovich P. Pro-inflammatory cytokines in glaucomatous aqueous and encysted Molteno implant blebs and their relationship to pressure. Invest Ophthalmol Vis Sci. 2013;54:4851–5.
Yamamoto T, Sakuma T, Kitazawa Y. An ultrasound biomicroscopic study of filtering blebs following mitomycin trabeculectomy. Ophthalmology. 1995;102:1770–6.
Park HY, Ahn MD. Imaging of trabeculectomy blebs with Visante anterior segment optical coherence tomography after digital ocular compression. Jpn J Ophthalmol. 2012;56:38–45.
Yamamoto T, Kuwayama Y, Kano K, Sawada A, Shoji N, Study Group for the Japan Glaucoma Society Survey of Bleb-related Infection. Clinical features of bleb-related infection: a 5-year survey in Japan. Acta Ophthalmol. 2013;91:619–24.
Yamamoto T, Kuwayama Y, Nomura E, Tanihara H, Mori K, Study Group for the Japan Glaucoma Society Survey of Bleb-related Infection. Changes in visual acuity and intraocular pressure following bleb-related infection: the Japan Glaucoma Society Survey of Bleb-related Infection Report 2 [report online]. Acta Ophthalmol. 2013;91:e420–6.
Yamada H, Sawada A, Kuwayama Y, Yamamoto T. Blindness following bleb-related infection in open-angle glaucoma. Jpn J Ophthalmol. 2014;58:490–5.
Greenfield DS. Bleb-related ocular infection. J Glaucoma. 1998;7:132–6.
Azuara-Branco A, Katz LJ. Dysfunctional filtering blebs. Surv Ophthalmol. 1998;43:93–126.
Yamamoto T, Kuwayama Y. The Collaborative Bleb-related Infection Incidence and Treatment Study Group. Interim clinical outcomes in the collaborative bleb-related infection incidence and treatment study. Ophthalmology. 2011;118:453–8.
Yamamoto T, Sawada A, Mayama C, Araie M, Ohkubo S, Sugiyama K, et al. The Collaborative Bleb-related Infection Incidence and Treatment Study Group. The 5-year incidence of bleb-related infection and its risk factors following filtering surgeries with adjunctive mitomycin C. Collaborative bleb-related infection incidence and treatment study 2. Ophthalmology. 2014;121:1001–6.
Hori N, Mochizuki K, Ishida K, Yamamoto T, Mikamo H. Clinical characteristics and risk factors of glaucoma filtering bleb infections. Nihon Ganka Gakkai Zasshi. 2009;113:951–63 (in Japanese).
Wells AP, Crowston JG, Marks J, Kirwan JF, Smith G, Clarke JC, et al. A pilot study of a system for grading of drainage blebs after glaucoma surgery. J Glaucoma. 2004;13:454–60.
Wells AP, Ashraff NN, Hall RC, Purdie G. Comparison of two clinical bleb grading systems. Ophthalmology. 2006;113:77–83.
Cantor LB, Mantravadi A, WuDunn D, Swamynathan K, Cortes A. Morphologic classification of filtering blebs after glaucoma filtration surgery: the Indiana Bleb Appearance Grading Scale. J Glaucoma. 2003;12:266–71.
Furrer S, Menke MN, Funk J, Töteberg-Harms M. Evaluation of filtering blebs using the ‘Wuerzburg bleb classification score’ compared to clinical findings. BMC Ophthalmol. 2012;17(12):24.
Acknowledgments
The authors wish to express their deep appreciation to the Japan Glaucoma Society for the opportunity to conduct this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
A. Sawada, None; Y. Kuwayama, None; T. Yamamoto, None.
About this article
Cite this article
Sawada, A., Kuwayama, Y. & Yamamoto, T. Changes in filtering bleb morphology after bleb-related infection. Jpn J Ophthalmol 59, 312–317 (2015). https://doi.org/10.1007/s10384-015-0398-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-015-0398-9