Abstract
Object
The goal of the study was to determine blood T 1 and T 2 values as functions of oxygen saturation (Y), temperature (Temp) and hematocrit (Hct) at an ultrahigh MR field (11.7 T) and explore their impacts on physiological measurements, including cerebral blood flow (CBF), blood volume (CBV) and oxygenation determination.
Materials and methods
T 1 and T 2 were simultaneously measured. Temperature was adjusted from 25 to 40°C to determine Temp dependence; Hct of 0.17–0.51 to evaluate Hct dependence at 25 and 37°C; and Y of 40–100% to evaluate Y dependence at 25 and 37°C. Comparisons were made with published data obtained at different magnetic field strengths (B 0).
Results
T 1 was positively correlated with Temp, independent of Y, and negatively correlated with Hct. T 2 was negatively correlated with Temp and Hct, but positively correlated with Y, in a non-linear fashion. T 1 increased linearly with B 0, whereas T 2 decreased exponentially with B0.
Conclusion
This study reported blood T 1 and T 2 measurements at 11.7 T for the first time. These blood relaxation data could have implications in numerous functional and physiological MRI studies at 11.7 T.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The longitudinal relaxation time (T 1) and transverse relaxation time (T 2) of blood are important for a number of quantitative physiological and functional MRI measurements. For example, blood T 1 is used to quantify cerebral blood flow (CBF) using arterial spin labeling (ASL) techniques [1, 2]. The accuracy of blood T 1 is crucial for cerebral blood volume (CBV) determination using the vascular space occupancy (VASO) method [3]. Blood T 2 is important in differentiating between the extravascular and intravascular blood oxygenation level dependent (BOLD) contributions [4]. Blood T 2 has also been used for calibration in determining tissue oxygen extraction fractions (OEF) and the cerebral metabolic rate of oxygen (CMRO2), including the T2-relaxation-under-spin-tagging (TRUST) techniques [5–8].
T 1 and T 2 values of blood are dependent on hematocrit content (Hct), oxygenation level (Y) and temperature (Temp). These relationships have been extensively studied at different magnetic field strengths from 1.5 to 7 T [1, 9–11]. With the rapid growth of functional studies on high field MRI scanners (>7 T) with animal models (especially with rodents), similar measurements are necessary for those high field systems in order to accurately determine CBF, CBV, OEF, and optimize BOLD contrast under various physiological conditions. To our knowledge, only blood T 1 and T 2 dependence on Y has been reported up to 9.4 T [12, 13]. The goal of the present study was to determine blood T 1 and T 2 values as functions of Hct, Y and Temp, and explore their impacts on CBF, CBV, OEF and BOLD measurements at 11.7 T. Comparisons were also made with published data at different magnetic field strengths.
Materials and methods
Blood sample preparation
Fresh blood samples were taken from male Sprague–Dawley rats. Five rats (500–650 g body weight) were used for the study. Rats were anesthetized for surgical preparation with 4.0% isoflurane for induction, and maintained at a 2.0% isoflurane and air mixture using a face mask. Body temperature was kept at 37°C via a heating pad. PE-50 catheters were placed into the femoral artery and vein. For each measurement, a vial of 1.0 ml blood (with heparin) was taken from the rat (from either artery or vein, see details below). Blood gases, Y, total hemoglobin and temperature were measured with a blood gas analyzer (Radiometer ABL5, Copenhagen). Vials were then sealed. To minimize the error due to red blood cell precipitation, the samples were agitated immediately before measurement and the study time (preparation + scan) was accomplished within 30 min. In the middle of the experiment, blood samples were also taken out and agitated again to minimize settling. Blood oxygenation was also measured after the experiment.
MRI experiments and data analysis
Experiments were performed on an 11.7 T BioSpec MR scanner (Bruker, Billerica, MA, USA). A quadrature volume coil (72 mm in diameter) was used for both RF transmission and reception. T 1 and T 2 were simultaneously measured using a RAREVTR sequence (RARE with variable repetition time TR) sequence. The sequence used a saturation scheme (i.e., varied TR) to acquire T 1 and used a multi-echo CPMG scheme (i.e., varied TE) to acquire T 2. In the study, six TR values (208, 400, 800, 1,500, 3,000 and 3,500 ms) and five TE values (14, 42, 70, 98, and 126 ms) were used. A single slice centered on the blood sample was chosen. The region of interest (ROI) was chosen to cover the blood sample area on the slice. Other imaging parameters were as follows: field-of-view (FOV) = 40 × 40 mm, slice thickness = 1.0 mm, matrix size = 128 × 128 and rare factor = 4. The total scan time was 3 min 46 s.
To evaluate temperature dependence, measurements were made on arterial blood samples (Hct = 0.43 and Y = 98–99%) with temperature adjusted from 25 to 40°C via a circulating water bath and monitored in real time by a temperature controller (Thermo Electron Co., Karlsruhe, Germany). This was done with a home-made acrylic tube (20 mm in diameter and 92 mm long) with a thermometer placed in the chamber but away from the imaging slice. To evaluate Hct dependence, plasma was added to arterial blood to achieve a Hct level of 0.17–0.51 with Y = 99% at room temperature (25°C) and body temperature (37°C). Hct was determined by a high-speed micro-hematocrit centrifuge (Model MB, International Equipment Company, MA, USA). To evaluate blood oxygenation dependence, oxygen concentration of the gas mixture that the animals inhaled was modulated to achieve Y = 40–100%. Measurements were also made at 25 and 37°C.
T 1 fitting was done with first echo (TE = 14 ms) and all the TRs; T 2 fitting was done with the 5th repetition time (TR = 3,000 ms) and all the echoes. T 1 was calculated by fitting M(t) = M 0 [1−c × exp (−TR/T 1)] and T 2 was calculated by fitting M(t) = M 0 exp (−TE/T 2) using ParaVision 5.0 software (Bruker) by fitting the absolute signals to a three-parameter model where M(t) is the signal intensity at a particular TR or TE, M 0 is the equilibrium signal and C is a factor to account for incomplete inversion.
Results
Study 1: Temperature (Temp) dependency
Figure 1 shows the plot of arterial blood T 1 and T 2 as a function of temperature (Hct = 0.43 and Y = 99%). T 1 was positively correlated with temperature (r = 0.99, P < 0.001). T 2 was negatively correlated with temperature in a non-linear fashion (r = −0.95, P < 0.001).
Study 2: Hematocrit level (Hct) dependency
A plot of arterial blood T 1 and T 2 (Y = 99% and Temp = 25 and 37°C) as a function of Hct is shown in Fig. 2. T 1 was negatively, and non-linearly, correlated with Hct at both temperature (r = −0.99, P < 0.001 at 25°C; r = −0.94, P < 0.005 at 37°C). Similar results were reported with bovine blood at 3 and 4.7 T [1, 9]. T 2 was also negatively correlated with Hct at the two temperatures (r = −0.93, P < 0.001, non-linearly, at 25°C; r = −1.00, P < 0.0005, linearly, at 37°C), consistent with that reported at 3 T [14].
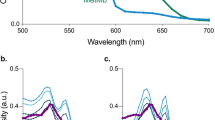
Study 3: Oxygenation level (Y) dependency
Figure 3 shows the plot of T 1 and T 2 versus Y with a normal hematocrit level (Hct = 0.43, Temp = 25°C and 37°C). T 1 was not significantly correlated with Y (r = 0.04, P > 0.5 at 25°C; r = 0.02, P > 0.5 at 37°C). This finding is consistent with those measured at lower fields [3, 12, 15, 16]. T 2 was positively, and non-linearly, correlated with Y (r = 0.95, P < 0.005 at 25°C; r = 0.97; P < 0.001 at 37°C). Arterial blood T 2 (Y = 99–100%) was significantly longer than that of venous blood (Y = 40–60%) at both temperatures (Table 1), in good agreement with literature [10, 13]. These findings indicate that there are strong T 2 dependencies over the physiological Y ranges.
Study 4: Field strength (B 0) dependency
We compared our T 1 and T 2 results at 11.7 T to published data at other field strengths [3, 9–13, 15, 22, 23]. Figure 4a shows that both arterial and venous T 1 values (T 1(a) and T 1(v), respectively) are linearly dependent on Bo (T 1(a) = 133.98 T + 1,211.4, r = 0.99, P < 0.001, and T 1(v) = 133.27 T + 1,187.4, r = 1.0, P < 0.02). Both arterial and venous T 1 values are linearly dependent on B0. Figure 4b shows T 2(a) and T 2(v) decreased exponentially with B 0 (r = −0.99, P < 0.001 and r = −0.90, P < 0.005 for arterial and venous blood, respectively).
a T 1 values of arterial and venous blood were both linearly dependent on B0. For arterial blood, r = 0.99, P < 0.001; data citation: 1.5 T [3]; 3 T [9]; 4.7 T [12]; 7 T [12]; 9.4 T [12]; 11.7 T [present study]. For venous blood, r = 1.0, P < 0.02; data citation: 1.5 T [3]; 3 T [9]; 11.7 T [present study]. b T 2 values of arterial and venous blood as a function of magnetic field. For T 2(a): 1.5 T [23]; 3 T ([11], Hct = 0.44, Y = 0.99); 4.7 T ([15], Y = 0.9–1.0); 7 T [present study]; 9.4 T [13]; 11.7 T [present study]; for T 2(v): 1.5 T [23]; 3 T ([10], Hct = 0.44, Y = 0.44); 4.7 T ([15], Y = 0.4); 7 T [22]; 9.4 T [13]; 11.7 T [present study]
Discussion
Accurate blood T 1 is important for determining absolute CBF (with unit ml/g/min) with the following equation: CBF = λ/T1 [(SNL–SL)/(SL + (2α-1)SNL)] (SNL and SL are signal intensities of the non-labeled and labeled images, respectively. α is the labeling efficiency, λ is the water tissue-blood partition coefficient) [17]. Based on the equation, one can estimate that quantitative CBF varies from −6 to 19% (0.94–1.19 ml/g/min, respectively, with the assumed basal CBF of 1 ml/g/min at 37°C in rodents) across the four Temp points, and from −8 to 10% across the seven Hct levels at 37°C (assuming CBF baseline is Hct = 0.43).
VASO signal changes are acquired at blood null point (TInull), which is determined based on the blood T 1. VASO signals will have blood signal contamination with inaccurate T 1 values. Because changes in CBV are determined from VASO signal [3], slightly changes in VASO signal changes could result in dramatic difference in CBV changes. For example, VASO changes from −1.2 to −3.7% could result in CBV changes from 21 to 38%, respectively, based on the model presented in [3]. Because CBV change is an important parameter in determining cerebral CMRO2 via the fMRI BOLD biophysical model [18–20], accurate determination of CBV changes is important. A CBV change from 21 to 38% would cause an error in CMRO2 changes of 5–10%. Therefore, caution must be taken to determine VASO changes when applying blood T 1 values at various physiological conditions. Oxygenation level does not significantly affect blood T 1, suggesting that the utilization of arterial or venous blood T 1 should not cause significant differences for VASO determination.
Blood T 2 values, on the other hand, are highly dependent on oxygenation level. This makes T 2 particularly useful for quantitatively estimating Y. Several groups have used this T 2 MRI approach to determine quantitative OEF (=1−Y) and CMRO2 (=CBF × OEF × CaO2; where CaO2 is the oxygen content), including the TRUST techniques [5–8, 14]. MRI OEF and CMRO2 data have been shown to be consistent with those obtained by O-15 positron emission tomography (PET), which is considered the gold standard [21]. MRI OEF and CMRO2 will likely have widespread utility because they are totally non-invasive.
In addition to Y, blood T 2 values are also dependent on Temp and Hct. It is interesting to see from Table 1 that venous blood T 2 has a much lower T 2 at higher temperatures, opposite to the trend of blood T 1, and is more negatively correlated with temperature than is arterial blood T 2 (Table 1). The Hct-dependent T 2 is an important factor for calibrating OEF measurement since Hct could vary slightly across individuals. All three parameters (Y, Temp and Hct) are thus crucial for OEF and CMRO2 determinations.
Blood T 2 also can be used to dissect the BOLD signal contributions. The BOLD signal consists of and intravascular (IV) and an extravascular (EV) component. The IV BOLD component exists because blood deoxyhemoglobin content strongly influences blood T 2, as well as the susceptibility-induced frequency difference between blood and surrounding tissue. At the same field strength (B 0), as demonstrated in the study, the IV contribution to BOLD signal should increase as Y increases, and decrease as Hct and Temp increase. At different B 0, T 2 decreases as B 0 increases. One can expect, therefore, that the IV contribution to the BOLD signal decreases with the increase of B 0. However, it is clear from previous and present studies that T 2 did not decrease as steeply at high fields (>7 T) [4, 13, 22]. This has strong implications in BOLD fMRI. Signals can be improved at high fields by using spin-echo acquisition because the intravascular venous signal is not visible at high field values [4]. Our finding suggests that going to higher field values may not result in further reduction of the intravascular venous signal per se, although BOLD contrast also increases overall.
Conclusion
This study analyzed the T 1 and T 2 values as a function of Y, Temp, and Hct of rat blood at 11.7 T. Over the ranges of physiological conditions investigated, change of arterial blood T 1 was negatively correlated with Hct (−883.7 ms per unit of Hct change), but positively correlated with temperature (51.8 ms/°C). T 2 change was negatively correlated with temperature (arterial T 2, −0.36 ms/°C), and was non-linearly correlated with Y and Hct. These results could have implications in many physiological studies at 11.7 T [24–26], including CBF using ASL, CBV using VASO, OEF using TRUST, and high spatial specificity BOLD fMRI [4, 22].
References
Silvennoinen MJ, Kettunen MI, Kauppinen RA (2003) Effects of hematocrit and oxygen saturation level on blood spin-lattice relaxation. Magn Reson Med 49:568–571
Wang J, Aguirre GK, Kimberg DY et al (2003) Arterial spin labeling perfusion fMRI with very low task frequency. Magn Reson Med 49:796–802
Lu H, Golay X, Pekar JJ et al (2003) Functional magnetic resonance imaging based on changes in vascular space occupancy. Magn Reson Med 50:263–274
Duong TQ, Yacoub E, Adriany G et al (2003) Microvascular BOLD contribution at 4 and 7 T in the human brain: gradient-echo and spin-echo fMRI with suppression of blood effects. Magn Reson Med 49:1019–1027
Golay X, Silvennoinen MJ, Zhou J et al (2001) Measurement of tissue oxygen extraction ratios from venous blood T(2): increased precision and validation of principle. Magn Reson Med 46:282–291
Lu H, Ge Y (2008) Quantitative evaluation of oxygenation in venous vessels using T2-relaxation-under-spin-tagging MRI. Magn Reson Med 60:357–363
Xu F, Ge Y, Lu H (2009) Noninvasive quantification of whole-brain cerebral metabolic rate of oxygen (CMRO2) by MRI. Magn Reson Med 62:141–148
Oja JM, Gillen JS, Kauppinen RA et al (1999) Determination of oxygen extraction ratios by magnetic resonance imaging. J Cereb Blood Flow Metab 19:1289–1295
Lu H, Clingman C, Golay X et al (2004) Determining the longitudinal relaxation time (T1) of blood at 3.0 Tesla. Magn Reson Med 52:679–682
Silvennoinen MJ, Clingman CS, Golay X et al (2003) Comparison of the dependence of blood R2 and R2* on oxygen saturation at 1.5 and 4.7 Tesla. Magn Reson Med 49:47–60
Zhao JM, Clingman CS, Narvainen MJ et al (2007) Oxygenation and hematocrit dependence of transverse relaxation rates of blood at 3T. Magn Reson Med 58:592–597
Dobre MC, Ugurbil K, Marjanska M (2007) Determination of blood longitudinal relaxation time (T1) at high magnetic field strengths. Magn Reson Imaging 25:733–735
Lee SP, Silva AC, Ugurbil K et al (1999) Diffusion-weighted spin-echo fMRI at 9.4 T: microvascular/tissue contribution to BOLD signal changes. Magn Reson Med 42:919–928
Qin Q, Grgac K, van Zijl PC (2011) Determination of whole-brain oxygen extraction fractions by fast measurement of blood T(2) in the jugular vein. Magn Reson Med 65:471–479
Atalay MK, Reeder SB, Zerhouni EA et al (1995) Blood oxygenation dependence of T1 and T2 in the isolated, perfused rabbit heart at 4.7T. Magn Reson Med 34:623–627
Brooks RA, Di Chiro G (1987) Magnetic resonance imaging of stationary blood: a review. Med Phys 14:903–913
Muir ER, Shen Q, Duong TQ (2008) Cerebral blood flow MRI in mice using the cardiac-spin-labeling technique. Magn Reson Med 60:744–748
Davis TL, Kwong KK, Weisskoff RM et al (1998) Calibrated functional MRI: mapping the dynamics of oxidative metabolism. Proc Natl Acad Sci USA 95:1834–1839
Lu H, Golay X, Pekar JJ et al (2004) Sustained poststimulus elevation in cerebral oxygen utilization after vascular recovery. J Cereb Blood Flow Metab 24:764–770
Lin AL, Fox PT, Yang Y et al (2008) Evaluation of MRI models in the measurement of CMRO2 and its relationship with CBF. Magn Reson Med 60:380–389
Mintun MA, Raichle ME, Martin WR et al (1984) Brain oxygen utilization measured with O-15 radiotracers and positron emission tomography. J Nucl Med 25:177–187
Yacoub E, Duong TQ, Van De Moortele PF et al (2003) Spin-echo fMRI in humans using high spatial resolutions and high magnetic fields. Magn Reson Med 49:655–664
Barth M, Moser E (1997) Proton NMR relaxation times of human blood samples at 1.5 T and implications for functional MRI. Cell Mol Biol (Noisy-le-grand) 43:783–791
Silva AC, Koretsky AP (2002) Laminar specificity of functional MRI onset times during somatosensory stimulation in rat. Proc Natl Acad Sci USA 99(23):15182–15187
Kalthoff D, Seehafer JU, Po C, Wiedermann D, Hoehn M (2011) Functional connectivity in the rat at 11.7 T: impact of physiological noise in resting state fMRI. Neuroimage 54(4):2828–2839
De La Garza BH, Li G, Muir E, Shih YY, Duong TQ (2011) BOLD fMRI of visual stimulation in the rat retina at 11.7 tesla. NMR in Biomed 24:188–193
Acknowledgments
We thank Hsiao-Ying Wey of the Research Imaging Institute and Saaussan Madi of Bruker Biospin for technical support. This work was supported by in part by the NIH (R01EY014211, R01EY018855) and VA MERIT. We are also grateful for the resources and support from NIH/NCRR (S10 RR023038), from the Defense Advanced Research Projects Agency (Comprehensive Facility for Animal Imaging Research (CFAIR), HR0011-07-C-0027), and the Texas Emerging Technology Fund from the Office of the Governor of Texas.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, AL., Qin, Q., Zhao, X. et al. Blood longitudinal (T 1) and transverse (T 2) relaxation time constants at 11.7 Tesla. Magn Reson Mater Phy 25, 245–249 (2012). https://doi.org/10.1007/s10334-011-0287-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10334-011-0287-2