Abstract
The aim of this study was to evaluate internal and marginal adaptation of high-viscosity bulk-fill composites to enamel and dentin with a self-etch (SE) and an etch-and-rinse adhesive (ER) without and with artificial aging. 128 MOD cavities in extracted human molars were prepared, randomly assigned to 8 groups (n = 16), bonded with either OptiBond FL (OFL, ER) or Xeno V+ (X, SE), and restored in 4 mm horizontal bulk layers with SonicFill (SF), Tetric EvoCeram Bulk fill (TEC), and x-tra fil (XF). Incremental layering technique with Premise (P) served as control. Half of the specimens each (n = 8) were subjected either to water storage (1 day, 37 °C) or prolonged storage (180 days) and thereafter thermocycling. Replicas were analyzed for marginal gap formation. After sectioning, interfacial adhesive defects were assessed. Results were statistical analyzed. (1) Internal adaptation: Except for TEC/OFL at enamel without artificial aging, no significant differences between bulk-fill composites and the control were observed. All groups at dentin with OFL showed less internal adhesive defects than that with X (p < 0.05). (2) Marginal adaptation: No significant differences were observed between bulk-fill composites and control except for P after artificial aging (p > 0.05). All other composites, regardless of artificial aging, formed significantly more marginal gaps at enamel with X compared to with OFL (p ≤ 0.05). Simplified restorations with high-viscosity bulk-fill composite showed comparable internal and marginal adaptation to incrementally placed fillings. A superiority of the 3-step ER approach was seen compared to the 1-step SE adhesive irrespective of the bulk-fill composite used.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Nowadays, composite is the primary choice for direct restorations and clinical studies reported high clinical performance on and good longevity [1,2,3,4]. However, the inevitable polymerization shrinkage and the resulting shrinkage stress are still relevant triggers for restoration failures due to breakdown of the adhesive bonding, which can, in turn, result in restoration loss [5]. Many clinical methods have been suggested such as incremental layering techniques or modifications of the light-activation protocol such as soft-start or pulse-delayed light curing to reduce polymerization shrinkage stress [6, 7]. These application techniques have demonstrated positive effects on clinical outcome and meanwhile, dentists started to use composite materials routinely also in large posterior cavities. However, the application is still time-consuming and technically demanding with inherent risks like contamination or application errors leading to debonding with potential clinical signs like post-operative sensitivity, marginal discoloration, or caries adjacent to the restoration [8].
Parallel to these variations in application, the drawbacks of polymerization shrinkage were addressed by the developments of new restorative materials. The ‘elastic cavity wall’ concept recommended the use of an intermediate elastic layer with resins of low elastic modulus [9]. Stress absorption could be achieved by thicker adhesive bonding layers or flowable composite [10, 11], but the reduction in filler content also results in a higher resin matrix ratio with an overall increase of polymerization shrinkage. Bulk-fill composites claim to address the time-consuming incremental filling procedure by allowing thicker horizontal increments up to 5 mm without a reduction in light-induced conversion rate and without an increase in shrinkage stresses. Deeper light polymerization could be achieved by increased light transmission due to filler modification or reduced filler content as well as by more efficient photoinitiators [12]. Before the establishment of the elastic modulus, the polymerization shrinkage stress development could be affected by viscoelastic flow behavior [13] and reaction kinetics [14]. The chemical composition of flowable bulk-fill composites is very similar to the conventional flowable composites with the exception of the first marketed flowable bulk-fill composite SDR (Dentsply Sirona) that is modified by a stress-relieving additive in the monomer matrix [15, 16]. The simplified procedure makes bulk filling popular with clinicians, and the lower polymerization stress reduces cusp deflection and improves the self-levelling ability compared to the conventional flowable composites [17]. However, flowable bulk-fill composites show inferior mechanical properties compared to the conventional composites and, therefore, require the placement of a capping layer made of a high-viscosity composite [18]. Manufacturers developed as a new stage high-viscosity bulk-fill composites to optimize the mechanical properties of the bulk-fill materials making coverage with a second highly viscous material unnecessary. There is, however, little knowledge about the internal as well as marginal adaptation of these high-viscosity bulk-fill composites. As the pulpal floor interface seems to be a weak spot for the effects of polymerization shrinkage stress on adhesive restoration adaptation [19], additional research is needed to evaluate the impact of bulk application of these materials on cavity seal. Furthermore, the influence of different adhesive systems might have an effect on the quality of the interfacial adhesive bond between bulk-fill composite resins luted to the tooth substrates. In the literature, it is widely accepted that especially large differences in adhesive performance are reported for etch and rinse (ER)—compared to 1-step self-echt (SE) adhesives [20]. However, it is questionable whether this weaker adhesive performance of 1-SE adhesives could be compensated by a potential reduction of polymerization stress of bulk-fill composites.
The current study was, therefore, set up to test the internal as well as the marginal adaptation of high-viscosity bulk-fill composites to enamel and dentin in class II cavities. An incrementally layered conventional hybrid composite served as a control. The null hypothesis tested was that no differences between incremental layering and bulk-fill technique could be observed. It was hypothesized that the ER adhesive would perform more effectively than the 1-SE adhesive and that artificial aging has a detrimental effect on the interface integrity. Furthermore, it was expected that quantitative internal and marginal adaptation would correspond to each other.
Materials and methods
This randomized-controlled in vitro study blinded for examiner and data analyst was performed with three high-viscosity bulk-fill composites and two different adhesive systems (Table 1). These groups were compared to a layered nanofilled hybrid composite (control, Table 1) with regard to internal adhesive defects and marginal gap formation. 128 intact, non-carious, unrestored human molars were selected out of a pool of collected teeth.
Restoration procedure
The teeth were stored in an aqueous solution of 0.5% Chloramine-T hydrate at 4 °C for up to 6 months after extraction. After debridement with a scaler (S204SD9, Hu-Friedy, Leimen, Germany), the teeth were assigned to 8 groups of 16 specimens each following simple randomization by a list computerized random numbers prepared by a person not involved in the conduct of the study.
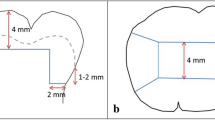
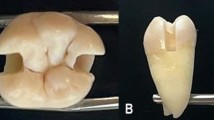
Standardized Class II cavities were prepared with a coarse cylindrical diamond bur (80 µm APS, Intensiv SA, Grancia, Switzerland) and refined in dentine with a cylindrical diamond finisher (25 µm, 16,000 min−1; APS) providing the following parameters: occlusal: 4 mm bucco-lingual width, 4 mm depth; mesial box: 1–2 mm above the cemento–enamel junction, 2 mm mesio-distal dimension at the bottom, 5 mm bucco-lingual width, 5 ± 1 mm below the peak of protuberance, distal box: 1–2 mm below the cemento–enamel junction, 2 mm mesio-distal dimension at the bottom, 5 mm bucco-lingual width were performed (Fig. 1). The margins were not beveled and all inner angles slightly rounded. The cavities were rinsed with water and stored in a climate chamber at a maximum of 1 h. All cavities were prepared by one operator.
The four resin-based composites, each combined with one of the two adhesives (etch-and-rinse, ER; self-etch adhesive system, SE) were applied to the prepared cavities. Table 1 shows the properties and composition of the materials used and supplementary Table 1 summarizes the procedure of application.
After restoration, overhangs were initially removed with a scaler (S204SD9, Hu-Friedy). The margins were finished proximal with a bud-shaped diamond finisher (15 µm, 20,000 min−1; APS) and occlusal with a grenade-shaped diamond finisher (9 µm, 20,000 min−1, APS) as well as polished (4000 min−1; Politip-F grey, Ivoclar Vivadent AG). All cavities were restored by the same previously trained operator. Afterwards, all specimens were extensively rinsed and stored in water for 24 h (distilled water ASTM III, 37 °C; Micromed 6, TKA; Niederelbert, Germany).
Artificial aging
Half of the specimens (n = 8) of each group were separated. Impressions of the proximal surfaces of these specimens were taken (Coltène PRESIDENT putty soft and plus light body, Coltène/Whaledent AG, Altstätten, Switzerland). The specimens were stored in distilled water at 37 °C for 180 days (water change 2× per week). After storage, the specimens were subjected to an alternating thermal cycle of + 5 °C and + 55 °C for 2500 cycles (Willytec Thermocycler V2.8, Feldkirchen-Westerham, Germany, exposure time 20 s each, and transfer time 5 s). The water temperature was checked continuously to produce a reliable thermocycling effect.
Specimen preparation and analysis of internal and marginal adaptation
After artificial aging, impressions of the same specimens were taken. Epoxy resin replicas from the impressions (before and after artificial aging) were produced (Stycast 1266 Part A + B, Emerson and Cumming, Westerlo, Belgium). For the analysis of marginal adaptation, the replicas (before and after artificial aging) were sputter-coated (Edwards Sputter Coater S150B, BOC Edwards, Irvine, Great Britain). The marginal gap formation was assessed by scanning electron microscopy (SEM; 200×; Phenom G2 Pro Phenom-World BV, Eindhoven, The Netherlands). The length of the gap formation at enamel and dentin were related to the total length of these margins and expressed as a percentage of total enamel or dentinal margin length, respectively.
For the analysis of internal adaptation, all specimens with/without artificial aging were rinsed (15 s, 20 °C) and stored in 5% glutaric di-aldehyde in 0.1 M sodium phosphate buffer (pH 7.2; 24 h, 4 °C). After rinsing again three times with 0.1 M sodium phosphate buffer (pH 7.2; 1× per h, 20 °C), the specimens were embedded in epoxy resin (Stycast 1266 Part A + B, Emerson & Cuming, Westerlo, Belgium) and sectioned longitudinally (5 slices per specimen, 200 µm) using a microtome (Leitz 1600 sawing-microtome, Ernst Leitz Wetzlar GmbH, Wetzlar, Germany). The second and the forth slice per specimens were selected as representative slices within restoration for the direct illustration of internal adaptation. The slices were etched with HCl (2%, 10 s, 20 °C) and NaOCl (10%, 30 s, 20 °C) and rinsed with distilled water (60 s, 20 °C) after every step. Furthermore, they were dehydrated (afferent alcohol chain: 30–50–70–80–90–95–100–100–100%, 5 min each), stored in hexamethyldisilazane (10 min, 20 °C, HMDS, Carl Roth GmbH, Karlsruhe, Germany) and gently air dried. Each slice was mounted on an aluminum specimen stub (12.5 mm Ø, Plano GmbH, Wetzlar, Germany) and gold-coated (5 nm).
The internal adaptation at enamel or dentin as relation of adhesive defect length to total length of the interface was scored using an SEM (2000×; Phenom G2 Pro) [21,22,23,24]:
-
score 1: 0–25%;
-
score 2: > 25–50%;
-
score 3: > 50–75%;
-
score 4: > 75–100%.
Statistical analysis
Assuming a power 70% sample size calculation (G*Power 3.1.9.2, free, Heinrich-Heine-University Düsseldorf) resulted in n = 7 specimens per group for adhesive defects and marginal gaps. In each group, n = 8 specimens were used. While the operator applying the restorations was aware of the allocation to the adhesive materials, the examiner and the data analyst were kept blinded to the allocation. The endpoints of analysis were the lengths with and without interfacial adhesive defects as well as lengths of marginal gaps before and after artificial aging. SPSS 20.0 for Windows (SPSS Inc., Chicago, USA) was used to analyze the data using Kruskal–Wallis and Mann–Whitney U test or Friedman and Wilcoxon test for comparison of the groups (α = 0.05). Due to the exploratory nature of this research, raw p values are reported and we refrained from correction for multiple testing.
Results
Internal adhesive defects at enamel–composite interface (Table 2)
TEC/OFL without artificial aging showed significantly less adhesive defects than P/OFL (p ≤ 0.05). While SF/X with artificial aging showed significantly less adhesive defects than TEC/X und XF/X (p ≤ 0.05), no differences to the P/X were observed (p > 0.05). Except for SF with artificial aging (p > 0.05) and P without artificial aging (p > 0.05), all composites showed more adhesive defects at the enamel–composite interface with X compared to OFL. XF/OFL and P/OFL showed less adhesive defects after artificial aging compared to no aging (p ≤ 0.05), whereas all the other groups showed no significant difference (p > 0.05) (Fig. 2).
SEM images (×1000 magnification). a P/OFL, b SF/OFL, c TEC/OFL, d P/X and e TEC/X at enamel–composite interface, f P/OFL, g SF/OFL, h XF/OFL, i P/X, j TEC/X at dentin–composite interface: no gap between enamel and OptiBond FL is present, while adhesive defects (white arrows) are visible between Xeno V+ and enamel. With OptiBond FL, the groups at dentin showed distinct resin tags distribution with deep penetration and lateral branches in dentin. Hybrid layers were observed. With Xeno V+, the groups showed adhesive defects (white arrows) within the hybrid layers. Tags of resin sporadically penetrating into dentinal tubule were observed. C composite, E enamel, D dentin
Internal adhesive defects at dentin–composite interface (Table 2)
No significant differences were observed between composites (Fig. 2). All composites with X, regardless of the artificial aging, showed significantly more adhesive defects than those with OFL (p ≤ 0.01). No significant differences were seen comparing data from groups subjected to aging and not subjected to aging (p > 0.05).
Marginal gap formation (Table 3)
At the enamel margins, the composite material did not show a significant influence (p > 0.05) on marginal gap formation. Except for P after artificial aging (p > 0.05), all other composites, regardless of the artificial aging, formed significantly more marginal gaps with X compared to OFL (p ≤ 0.05).
At dentin margins, no significant difference was observed between bulk-fill composites and the control (p > 0.05). SF/OFL showed significantly more marginal gaps compared to SF/X regardless of the artificial aging (p ≤ 0.05). After artificial aging, XF/OFL showed more gaps compared to XF/X (p ≤ 0.01) as did P/OFL compared to P/X (p ≤ 0.05).
Discussion
Where TEC/OFL at enamel demonstrates significantly less internal adhesive defects than control, all other bulk-fill groups showed no significant difference in internal adhesive defects to enamel and dentin compared to the control for both adhesive systems used. Moreover, no significant differences were observed between bulk-fill composites and control in marginal gap formation at enamel and dentin. Additionally, conform results of internal and marginal adaptation were seen.
The null hypothesis of this study cannot be completely rejected as the bulk-fill technique with appropriate composite materials could obtain similar adaptation to the cavity than an incremental filling with a conventional composite. Internal and marginal adaptation of resin composite restorations is closely related to forces induced by polymerization shrinkage stress [25] which is significantly affected by the factors such as volumetric polymerization shrinkage, elastic modulus, and rate of conversion [26]. Bulk-fill materials show similar volumetric polymerization shrinkage compared to the conventional composites [16]. As all composites investigated in this study contain similar amounts of filler (81–86 wt%) and have a similar degree of conversion of 69.4–71.6% at 4 mm depth for bulk-fill composites and 72.8% at 2 mm depth for Premise [27, 28], it could be assumed that volumetric polymerization shrinkage of both investigated composite groups is similar. Several research groups reported that there is no statistical difference of shrinkage values between high-viscosity conventional composites and high-viscosity bulk-fill composites [16, 29, 30]. Even so not measured by the same method, manufacturers’ data approve this for the materials under study. Shrinkage values of SF, TEC, XF, and P range between 1.6 and 1.9%, respectively, clarify that not the pure shrinkage but the polymerization kinetic of bulk-fill materials is the key feature behind stress absorption [17]. This is illustrated in this study by the absence of significant differences in bond failure between the incremental and bulk-fill approach. However, in addition to this fundamental finding, there are still differences between bulk-fill materials. TEC, for instance, showed significantly enhanced marginal sealing and more perfect margins at the enamel than the conventional composites [31], which is comparable with the results of the current study with regard to internal adaptation. The reason for this might be the lower modulus of elasticity of TEC compared to that of other composites which results in lower polymerization shrinkage stress. Despite similar amounts of filler in all the composites investigated in this study, the modulus of elasticity of TEC is significantly lower than that of other composites [32], because TEC contains pre-polymerized fillers, which are included in the total filler amount. Consequently, TEC has a lower fraction of inorganic filler, which is the main contributor to a higher modulus of elasticity [33].
Furthermore, it has been partially confirmed that the adhesive system (ER vs. SE) influences adhesive defects at the tooth composite interface. Almost all groups with ER (OFL) at enamel, as well as dentin, showed less adhesive defects than groups with SE (X). The inferior margin quality of SE compared to ER is probably associated with the less distinct micro-retention of the adhesive layer at the enamel surface. The previous studies reported that ER has mostly better adhesive performance especially than 1-SE [34, 35], which is in line with the results of the current study. This statement is, however, strongly dependent on the sub-classification of the adhesive systems. Peumans et al. [36] summarized in their meta-analysis that 2-step SE adhesives achieve similar performance as 3-step ER adhesives, while van Meerbeek et al. [37] concluded that 1-step SE adhesives have shortcomings such as low immediate bond strength and low long-term effectiveness. In the current study, a 3-step ER (OptiBond FL) and a 1-step SE (Xeno V+) were used. A significant difference between ER and most SE adhesives can be noted not only at enamel but also at dentin especially for 1-step systems like Xeno V+. These adhesives generally lack of a second layer for hydrophobic coating and Xeno V additionally does not contain effective functional monomers like MDP, that is known for its chemical bond to dentin [38, 39]. A possible and obvious assumption that bulk-fill materials with reduced polymerization shrinkage stress might positively affect adaptation of simplified and clinically less effective adhesive systems could not be confirmed. This finding is a special feature of this study and expands the findings of Roggendorf et al. [40] and Heintze et al. [41] that saw a better performance of ER adhesives in adhesive–composite combinations of the same manufacturer.
The hypothesis of the detrimental effect of artificial aging on the adhesive interface cannot be generally accepted. With respect to the adhesive system, it was expected that the 1-SE groups would show more adhesive defects with water storage and artificial aging due to hydrolysis of the more hydrophilic resin [42] and lower stability to degradation, in general [43]. The current study showed only partially significant influence of artificial aging, it seems plausible that this can be attributed to the short-term character of this study with storage below 1 year [35, 44] and a moderate amount of thermocycles with regard to the variance in the literature [41, 45, 46].
Limitations of the current study are related to this experimental setup. As an invasive method was used for the evaluation of internal adhesive defects, the adhesive quality was measured on two slices obtained by cross-sectioning. The three-dimensional geometry of the internal interfaces is, therefore, only partially represented by the prepared sections. While only a few significant differences were observed, it could be argued that a greater sample size would result in more discrimination. However, the chosen sample size allowed an initial material comparison in vitro as a basis for further clinical testing. A clear advantage of this setup is the combined evaluation of internal and marginal adaption, which allows a more complete assessment of the complex adhesive interface in a cavity design comparable to the clinical situation [47, 48].
At the moment, it remains unclear, whether the initial compensation of thicker composite layers due to reduced polymerization stress is a sustainable parameter for the clinical success of this simplified composite application. In addition, one could well ask whether the potential to reduce polymerization stress could lead to a relevant decrease in adhesive defects if this advantage would not be influenced by the counteracting increase of the layer thickness. Although Flury et al. [49] reported no detrimental effect of different increment thicknesses on shear bond strength of bulk-fill materials, the three-dimensional cavity configuration will add significant complexity to the force distribution induced by polymerization shrinkage.
Conclusion
The current study shows that simplified restorations with high-viscosity bulk-fill composites achieve an internal and a marginal adaptation comparable to incremental layering techniques with a conventional composite. The bulk-fill composites evaluated in this study can, therefore, be applied without detriment to the quality of posterior restorations. However, more importantly, a well-performing adhesive is the key element for achieving good bonding quality of restorations regardless of the composites used.
Change history
04 February 2019
In the original publication of the article the paragraph “The four resin-based composites…” appearing below the “Materials and methods” section is incomplete. The correct paragraph is provided in this correction below.
References
Opdam NJM, van de Sande FH, Bronkhorst E, Cenci MS, Bottenberg P, Pallesen U, Gaengler P, Lindberg A, Huysmans MCDNJM, van Dijken JW. Longevity of posterior composite restorations: a systematic review and meta-analysis. J Dent Res. 2014;93:943–9. https://doi.org/10.1177/0022034514544217.
van Dijken JW. Direct resin composite inlays/onlays: an 11 year follow-up. J Dent. 2000;28:299–306.
Demarco FF, Corrêa MB, Cenci MS, Moraes RR, Opdam NJM. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater. 2012;28:87–101. https://doi.org/10.1016/j.dental.2011.09.003.
el-Mowafy OM, Lewis DW, Benmergui C, Levinton C. Meta-analysis on long-term clinical performance of posterior composite restorations. J Dent. 1994;22:33–43.
Cardoso MV, Almeida Neves A de, Mine A, Coutinho E, van Landuyt K, Munck J de, van Meerbeek B. Current aspects on bonding effectiveness and stability in adhesive dentistry. Aust Dent J. 2011;56(Suppl 1):31–44. https://doi.org/10.1111/j.1834-7819.2011.01294.x.
Ferracane JL. Developing a more complete understanding of stresses produced in dental composites during polymerization. Dent Mater. 2005;21:36–42. https://doi.org/10.1016/j.dental.2004.10.004.
Park J, Chang J, Ferracane J, Lee IB. How should composite be layered to reduce shrinkage stress: incremental or bulk filling? Dent Mater. 2008;24:1501–5. https://doi.org/10.1016/j.dental.2008.03.013.
Abbas G, Fleming GJP, Harrington E, Shortall ACC, Burke FJT. Cuspal movement and microleakage in premolar teeth restored with a packable composite cured in bulk or in increments. J Dent. 2003;31:437–44.
Kemp-Scholte CM, Davidson CL. Complete marginal seal of Class V resin composite restorations effected by increased flexibility. J Dent Res. 1990;69:1240–3.
Oliveira LCA, Duarte S, Araujo CA, Abrahão A. Effect of low-elastic modulus liner and base as stress-absorbing layer in composite resin restorations. Dent Mater. 2010;26:e159-69. https://doi.org/10.1016/j.dental.2009.11.076.
Haak R, Wicht MJ, Noack MJ. Marginal and internal adaptation of extended class I restorations lined with flowable composites. J Dent. 2003;31:231–9.
Menees TS, Lin CP, Kojic DD, Burgess JO, Lawson NC. Depth of cure of bulk fill composites with monowave and polywave curing lights. Am J Dent. 2015;28:357–61.
Vaidyanathan J, Vaidyanathan TK. Flexural creep deformation and recovery in dental composites. J Dent. 2001;29:545–51.
Braga RR, Ferracane JL. Contraction stress related to degree of conversion and reaction kinetics. J Dent Res. 2002;81:114–8.
Garcia D, Yaman P, Dennison J, Neiva G. Polymerization shrinkage and depth of cure of bulk fill flowable composite resins. Oper Dent. 2014;39:441–8. https://doi.org/10.2341/12-484-L.
Jang J-H, Park S-H, Hwang I-N. Polymerization shrinkage and depth of cure of bulk-fill resin composites and highly filled flowable resin. Oper Dent. 2015;40:172–80. https://doi.org/10.2341/13-307-L.
Kwon Y, Ferracane J, Lee I-B. Effect of layering methods, composite type, and flowable liner on the polymerization shrinkage stress of light cured composites. Dent Mater. 2012;28:801–9. https://doi.org/10.1016/j.dental.2012.04.028.
Ilie N, Kessler A, Durner J. Influence of various irradiation processes on the mechanical properties and polymerisation kinetics of bulk-fill resin based composites. J Dent. 2013;41:695–702. https://doi.org/10.1016/j.jdent.2013.05.008.
Furness A, Tadros MY, Looney SW, Rueggeberg FA. Effect of bulk/incremental fill on internal gap formation of bulk-fill composites. J Dent. 2014;42:439–49. https://doi.org/10.1016/j.jdent.2014.01.005.
Heintze SD. Systematic reviews: I. The correlation between laboratory tests on marginal quality and bond strength. II. The correlation between marginal quality and clinical outcome. J Adhes Dent. 2007;9(Suppl 1):77–106.
Park K-J, Schneider H, Haak R. Assessment of interfacial defects at composite restorations by swept source optical coherence tomography. J Biomed Opt. 2013;18:76018. https://doi.org/10.1117/1.JBO.18.7.076018.
Park K-J, Schneider H, Haak R. Assessment of defects at tooth/self-adhering flowable composite interface using swept-source optical coherence tomography (SS-OCT). Dent Mater. 2015;31:534–41. https://doi.org/10.1016/j.dental.2015.02.005.
Haak R, Schmidt P, Park K-J, Häfer M, Krause F, Ziebolz D, Schneider H. OCT for early quality evaluation of tooth-composite bond in clinical trials. J Dent. 2018;76:46–51. https://doi.org/10.1016/j.jdent.2018.06.007.
Häfer M, Schneider H, Rupf S, Busch I, Fuchß A, Merte I, Jentsch H, Haak R, Merte K. Experimental and clinical evaluation of a self-etching and an etch-and-rinse adhesive system. J Adhes Dent. 2013;15:275–86. https://doi.org/10.3290/j.jad.a29633.
Kim HJ, Park SH. Measurement of the internal adaptation of resin composites using micro-CT and its correlation with polymerization shrinkage. Oper Dent. 2014;39:70. https://doi.org/10.2341/12-378-L.
Braga RR, Ballester RY, Ferracane JL. Factors involved in the development of polymerization shrinkage stress in resin-composites: a systematic review. Dent Mater. 2005;21:962–70. https://doi.org/10.1016/j.dental.2005.04.018.
Tarle Z, Attin T, Marovic D, Andermatt L, Ristic M, Taubock TT. Influence of irradiation time on subsurface degree of conversion and microhardness of high-viscosity bulk-fill resin composites. Clin Oral Investig. 2015;19:831–40. https://doi.org/10.1007/s00784-014-1302-6.
Magne P, Malta DAMP, Enciso R, Monteiro-Junior S. Heat treatment influences monomer conversion and bond strength of indirect composite resin restorations. J Adhes Dent. 2015;17:559–66. https://doi.org/10.3290/j.jad.a35258.
Kim RJ, Kim YJ, Choi NS, Lee IB. Polymerization shrinkage, modulus, and shrinkage stress related to tooth-restoration interfacial debonding in bulk-fill composites. J Dent. 2015;43:430–9. https://doi.org/10.1016/j.jdent.2015.02.002.
Zorzin J, Maier E, Harre S, Fey T, Belli R, Lohbauer U, Petschelt A, Taschner M. Bulk-fill resin composites: polymerization properties and extended light curing. Dent Mater. 2015;31:293–301. https://doi.org/10.1016/j.dental.2014.12.010.
Al-Harbi F, Kaisarly D, Bader D, El GM. Marginal integrity of bulk versus incremental fill class II composite restorations. Oper Dent. 2015. https://doi.org/10.2341/14-306-L.
Leprince JG, Palin WM, Vanacker J, Sabbagh J, Devaux J, Leloup G. Physico-mechanical characteristics of commercially available bulk-fill composites. J Dent. 2014;42:993–1000. https://doi.org/10.1016/j.jdent.2014.05.009.
Ilie N, Bucuta S, Draenert M. Bulk-fill resin-based composites: an in vitro assessment of their mechanical performance. Oper Dent. 2013;38:618–25. https://doi.org/10.2341/12-395-L.
Frankenberger R, Tay FR. Self-etch vs etch-and-rinse adhesives: effect of thermo-mechanical fatigue loading on marginal quality of bonded resin composite restorations. Dent Mater. 2005;21:397–412. https://doi.org/10.1016/j.dental.2004.07.005.
Häfer M, Jentsch H, Haak R, Schneider H. A three-year clinical evaluation of a one-step self-etch and a two-step etch-and-rinse adhesive in non-carious cervical lesions. J Dent. 2015;43:350–61. https://doi.org/10.1016/j.jdent.2014.12.009.
Peumans M, Munck J de, Mine A, van Meerbeek B. Clinical effectiveness of contemporary adhesives for the restoration of non-carious cervical lesions. A systematic review. Dent Mater. 2014;30:1089–103. https://doi.org/10.1016/j.dental.2014.07.007.
van Meerbeek B, Yoshihara K, Yoshida Y, Mine A, Munck J de, van Landuyt KL. State of the art of self-etch adhesives. Dent Mater. 2011;27:17–28. https://doi.org/10.1016/j.dental.2010.10.023.
Inoue S, Koshiro K, Yoshida Y, Munck J de, Nagakane K, Suzuki K, Sano H, van Meerbeek B. Hydrolytic stability of self-etch adhesives bonded to dentin. J Dent Res. 2005;84:1160–4. https://doi.org/10.1177/154405910508401213.
Munck J de, Mine A, Poitevin A, van Ende A, Cardoso MV, van Landuyt KL, Peumans M, van Meerbeek B. Meta-analytical review of parameters involved in dentin bonding. J Dent Res. 2012;91:351–7. https://doi.org/10.1177/0022034511431251.
Roggendorf MJ, Kramer N, Appelt A, Naumann M, Frankenberger R. Marginal quality of flowable 4-mm base vs. conventionally layered resin composite. J Dent. 2011;39:643–7. https://doi.org/10.1016/j.jdent.2011.07.004.
Heintze SD, Monreal D, Peschke A. Marginal quality of class II composite restorations placed in bulk compared to an incremental technique: evaluation with SEM and stereomicroscope. J Adhes Dent. 2015;17:147–54. https://doi.org/10.3290/j.jad.a33973.
Breschi L, Mazzoni A, Ruggeri A, Cadenaro M, Di Lenarda R, De Stefano Dorigo E. Dental adhesion review: aging and stability of the bonded interface. Dent Mater. 2008;24:90–101. https://doi.org/10.1016/j.dental.2007.02.009.
Shirai K, Munck J de, Yoshida Y, Inoue S, Lambrechts P, Suzuki K, Shintani H, van Meerbeek B. Effect of cavity configuration and aging on the bonding effectiveness of six adhesives to dentin. Dent Mater. 2005;21:110–24. https://doi.org/10.1016/j.dental.2004.01.003.
Hashimoto M, Ohno H, Kaga M, Endo K, Sano H, Oguchi H. In vivo degradation of resin-dentin bonds in humans over 1 to 3 years. J Dent Res. 2000;79:1385–91. https://doi.org/10.1177/00220345000790060601.
Campos EA, Ardu S, Lefever D, Jasse FF, Bortolotto T, Krejci I. Marginal adaptation of class II cavities restored with bulk-fill composites. J Dent. 2014;42:575–81. https://doi.org/10.1016/j.jdent.2014.02.007.
Bayraktar Y, Ercan E, Hamidi MM, Colak H. One-year clinical evaluation of different types of bulk-fill composites. J Investig Clin Dent. 2016. https://doi.org/10.1111/jicd.12210.
Shahidi C, Krejci I, Dietschi D. In vitro evaluation of marginal adaptation of direct class II composite restorations made of different “low-shrinkage”. Syst Oper Dent. 2017;42:273–83. https://doi.org/10.2341/15-217-L.
Garcia-Godoy F, Krämer N, Feilzer AJ, Frankenberger R. Long-term degradation of enamel and dentin bonds: 6-year results in vitro vs. in vivo. Dent Mater. 2010;26:1113–8. https://doi.org/10.1016/j.dental.2010.07.012.
Flury S, Peutzfeldt A, Lussi A. Influence of increment thickness on microhardness and dentin bond strength of bulk fill resin composites. Dent Mater. 2014;30:1104–12. https://doi.org/10.1016/j.dental.2014.07.001.
Acknowledgements
The intact, non-carious, unrestored human molars were selected out of a pool of collected teeth in accordance with an approved protocol of the Ethics Committee of the University Leipzig, Germany (no. 299-10-04102010).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The restoration materials were provided by Dentsply Sirona GmbH, Ivoclar Vivadent AG and Voco GmbH.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: In the original publication of the article the paragraph “The four resin-based composites…” appearing below the “Materials and methods” section is incomplete. The correct paragraph is provided in this correction below: The four resin-based composites were applied to the prepared cavities combined with each of the two adhesives (etch-and-rinse, ER; self-etch, SE). Table 1 shows the properties and composition of the materials used and supplementary table 1 summarizes the procedure of application.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Haak, R., Näke, T., Park, KJ. et al. Internal and marginal adaptation of high-viscosity bulk-fill composites in class II cavities placed with different adhesive strategies. Odontology 107, 374–382 (2019). https://doi.org/10.1007/s10266-018-0402-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-018-0402-1