Abstract
This article reviews the quantitative evidence on the behavioural effects of copayment within the health area across a wide range of countries. The review distinguishes itself from previous similar reviews by having a high degree of transparency for the search strategy used to identify the studies included in the review as well as the criteria for inclusion and by including the most recent literature. Empirical studies were identified by performing searches in EconLit. The literature search identified a total of 47 studies of the behavioural effects of copayment. Considering the demand effects, the majority of the reviewed studies found that copayment reduces the use of prescription medicine, consultations with general practitioners and specialists, and ambulatory care, respectively. The literature found no significant effects of copayment on the prevalence of hospitalisations. The empirical evidence on whether copayment for some services, but not for others, causes substitution from the services that are subject to copayment to the ‘free’ services rather than lower total use is sparse and mixed. Likewise, the health effects of copayment have only been analysed empirically in a limited number of studies, of which half did not find any significant effects in the short term. Finally, the empirical evidence on the distributional consequences of copayment indicates that individuals with low income and in particular need of care generally reduce their use relatively more than the remaining population in consequence of copayment. Hence, it is clear that copayment involves some important economic and political trade-offs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction and background
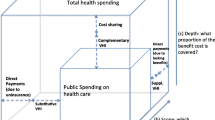
Copayment is frequently brought up as a possible solution to the steadily increasing cost pressure faced by many universal health care systems [1]. Economic theory predicts that copayment may under some circumstances reduce the individual demand for health care services by increasing the price paid by the consumer at the time of consumption, while at the same time contribute to the financing. However, it may also give rise to adverse health effects and distributional consequences.
The use of copayment within the health area varies considerably between countries and largely reflects political choice as well as historical circumstances [2]. The empirical literature on the effects of copayment for health care services has previously been reviewed in a number of studies with different areas of focus and using different methods and delimitations. One group of studies have focussed exclusively on the effects of copayment for prescription medicine [3–6]. Others have reviewed the literature on the effects of copayment for various types of health care services [7–9], one of which restricted the review to consider effects among the elderly [10]. While the reviews focussing on the use of prescription medicine are explicit about their search strategy and criteria for inclusion, this is not the case for the reviews including various types of health care services and entire populations. Hence, this review distinguishes itself from these reviews by having a high degree of transparency about the search strategy used to identify the studies included in the review as well as the criteria for inclusion. Moreover, given that new studies of the behavioural effects of copayment appear on a frequent basis, an updated review is justified alone by including the most recent literature.
This article reviews the quantitative evidence on the behavioural effects of copayment within the health area across a wide range of countries. The specific aims are to provide a systematic overview of the extent to which copayment (1) reduces the individual demand for the services on which it is imposed, (2) has adverse health effects or shifts the use to services that are not subject to copayment rather than reduce total use and finally (3) gives rise to distributional consequences.Footnote 1 Hereby the review contributes not only to the academic literature, but it also has a policy purpose as national decision makers in many European countries are faced with decisions about whether to introduce copayment for new types of services or expand, restructure or phase out existing copayment schemes.
Within the health area, the copayment debate often takes its point of departure in the RAND health insurance experiment (HIE). This section proceeds by summarising the results of the RAND HIE and briefly outlining the theoretical framework for the analysis of the behavioural effects of copayment. The remainder of the article is organised as follows: the “Methods” section describes the search strategy used to identify the empirical literature included in the review and the criteria for inclusion. The “Results” section reviews the results of the identified studies. Finally, the “Conclusions and perspectives” section concludes and discusses the findings in a broader perspective.
The RAND health insurance experiment
The RAND HIE enjoys special status as one of the most comprehensive social experiments ever with respect to both the number of involved individuals and costs. The experiment was launched by the US government with the purpose of investigating mainly how copayment affects the use of health care services. The experiment ran from November 1974 to February 1977 and involved around 6,000 individuals, who were randomly distributed into five different health insurance plans with varying levels of copayment. The insurance plans varied with respect to both the deductible, copayment share and maximum annual copayment. Overall, the RAND HIE finds that copayment reduces the use of all types of health care services. The average price elasticity of the individual demand for health care services is estimated to be -0.20 across the different types of health care services included in the experiment [11].
More specific results from the RAND HIE found that:
-
Copayment reduces the number of visits but not the intensity of the treatment received. This indicates that the effect of copayment is limited once the individual has contacted the relevant health care provider [12].
-
Copayment reduces the effect of effective and ineffective treatments to the same extent, and it does not prevent the occurrence of inappropriate hospitalisations [13, 14].
-
The effects of copayment vary for different population groups. Copayment reduces the demand for health care services more for low income groups, and it is particularly effective in reducing the use of health care services among low income children [12].
-
For the average participant in the experiment copayment does not affect health as measured by a number of indicators. However, there are negative health effects of copayment for individuals with high blood pressure and low income as well as individuals with poor sight [15].
There are a number of reasons in favour of not basing the current debate about copayment in the European health care systems on the RAND results alone. First, the RAND HIE is conducted within an institutional setting differing markedly from the universal health care systems found in most European countries. Second, the copayment schemes that exist alongside universal health care systems are usually more complex than those implemented in the RAND HIE. Third, the RAND HIE does not include the elderly, who account for a large share of the health expenditures in most countries. Finally, the experiment was conducted more than 3 decades ago. Since then, the incidence of a number of lifestyle illnesses has developed, just as the diagnosis and treatment options have changed for many illnesses.
Brief outline of the theoretical framework
The theoretical framework for the analysis of the behavioural effects of copayment takes it point of departure from the demand side. This requires that the use of the services on which copayment is imposed is demand driven. For several services within the health care area, it may be argued that use is also determined by the supply side. It is thus important to keep in mind that copayment is only one among several instruments with potential to lower the use of services and the corresponding expenditure within the health area. Visitation and waiting lists as well as mechanisms seeking to affect the suppliers are also capable of lowering the use of health care services. It may, however, be argued that use in most cases requires the presence of some sort of demand. An important point in this regard is that copayment should not be viewed as a substitute for the alternative rationing mechanisms, but rather as a supplement [16]. Hence, when we refer to the demand for health care services in the following, this is done assuming all else equal, i.e. that potential supply-side initiatives as well as prioritisation through visitation and waiting lists are kept constant.
Demand effects
Economic theory predicts that copayment may under some circumstances reduce the individual demand for health care services by increasing the price paid by the consumer at the time of consumption [17, 18]. The magnitude of this effect depends on the price elasticity of demand. Imposed on health care services for which the demand is largely price inelastic, copayment shifts the burden of financing from the public coffers to the users rather than lower the use.Footnote 2 Imposed on health care services for which the demand is price elastic, copayment may be shown to reduce the demand, thereby potentially also lowering the total health care costs.
Health effects and substitution
Even when copayment reduces use of the relevant services, it does not necessarily lower the total health care costs. First, it is possible that copayment for some services within a given area, but not for others, causes substitution from services that are subject to copayment to services that are free or subject to less copayment rather than lower the total use. Second, the introduction of copayment for services, for which the individual demand is price elastic, may lead to a deterioration in public health, if the copayment causes citizens to drop effective and necessary care and treatment. Besides this being inconvenient for the affected individuals, it implies that savings brought along by copayment in one area may be fully or partly cancelled out by increases in the use of other types of services. However, it is also possible that copayment for one type of health care service reduces the use of complementary services.Footnote 3
Distributional effects
Finally, economic theory suggests that copayment may have distributional consequences [16]. First, it is expected that low income individuals reduce their use of health care services more than the remaining population in consequence of copayment for two reasons. One reason, which is especially expected to affect the use of services accounting for a large share of the budget, is that low income individuals have smaller consumption possibility sets. The other reason is that subject to the standard assumption of decreasing marginal utility of income, the marginal utility of income is higher for low income individuals. This implies that the utility loss associated with copayment is higher for low income individuals, all else equal, and they are therefore expected to reduce their use of the services that are subject to more copayment. Second, individuals with a high demand for services on which copayment is imposed are hit particularly hard when part of the burden of payment is distributed according to use rather than income. Even when the demand is inelastic for low income groups and use is not affected by copayment, there are still distributional consequences because copayment lowers the income left for remaining consumption disproportionally more for low income individuals.
Considering the distributional consequences of copayment, an important point is that the group of individuals with a high demand in the reference point with no copayment is likely to be heterogeneous with regards to the need for health care services as well as the corresponding price elasticity of demand. Some individuals have a limited need for the service in question and in consequence of this their demand is very price sensitive. This group is expected to reduce their use notably in consequence of copayment, which was the exact point of introducing copayment. Another group of individuals have a regular need for the service in question and are thus not expected to reduce their use notably in consequence of copayment. This group, typically made up of chronic patients, is hit particularly hard by the copayment, which may be considered undesirable from an equity point of view. In either case, the distributional consequences of copayment may be mitigated by making the copayment income dependent, exempting groups in particular need of the service in question, or put a ceiling on the annual copayment, after which additional use is paid in full by the public coffers.
Methods
Inclusion criteria
The literature review includes quantitative studies of the behavioural effects of user charges for health care services. Studies published as articles in peer-reviewed journals and as working papers, scientific dissertations,Footnote 4 books and book chapters in English, Danish or Swedish are included. In order to ensure some degree of overall homogeneity across the health care systems and institutional settings considered, we include only studies based on data from high income countries cf. the World Bank [19]. Only original studies, i.e. studies that perform an independent analysis of existing data or data collected specifically for the purpose, are considered. Timewise, the review is restricted to include studies published from 1990 and up until December 2011. Moreover, the focus of the review is on direct copayment, which may take the form of a fixed rate per unit of service, a share of the costs of providing the service or a deductible (i.e. the user pays the full costs of providing the service up until a given threshold) [5], as opposed to indirect copayment in the form of reference or tiered pricing, which is mainly used within the pharmaceutical area.Footnote 5
Finally, studies that have identified the effect of copayment by using variation in the copayment rate between individuals who have purchased private health insurance on a voluntary basis are not included in the present review.Footnote 6 The main reason for this limitation is that the voluntary element in these schemes implies a selection, which is tricky to handle empirically. The level of copayment an individual is facing in such a setting may to a large extent be expected to depend on unobservable individual characteristics, such as risk preferences and expected use of the health care services that are subject to copayment. The methodological challenges associated with handling such selection are judged to necessitate a thorough quality assessment of the identified studies, which is outside the scope of this review.
Search strategy and identification of relevant studies
The reviewed studies were identified by performing electronic searches in the bibliographic database EconLit. The search was restricted to words included in the title, abstract and keywords. The search terms used were [payment* OR copayment* OR co-payment* OR user fee* OR user charge* OR co-finance OR user pays OR cost sharing OR out-of-pocket OR private payment* OR finance OR financing OR funding] AND [health* OR medical OR somatic OR doctor* OR dental OR medicine OR drug* OR primary care OR general practice OR specialist OR physio* OR rehabilitation OR hospital OR ambulatory].Footnote 7 The identification of the relevant studies among the studies identified by the search was based on title and abstract or summary. In case of doubt, the decision was based on a reading of the entire study. The relevance of the studies was assessed based on the inclusion criteria outlined in the previous section and whether they answered at least one of the research questions outlined in the introduction. Subsequently, the reference lists of the studies identified as being relevant were searched for additional literature.Footnote 8
Results
The initial search in EconLit resulted in 3,289 hits. A screening of the many hits resulted in 37 studies being identified as relevant.Footnote 9 Next, the reference lists of the selected studies were searched for additional literature, resulting in 10 additional studies. Hence, the search strategy identified 47 studies of the behavioural effects of copayment in total. It is ensured that the same study is not included more than once, e.g. both in the form of working paper and journal article.
Table 1 provides key information about the reviewed studies, the majority of which are published within the recent decade. The reviewed studies are described with respect to the data, methods, focus of analysis and type of publication.
It is seen from Table 1 that the vast majority of the reviewed studies identify the effects of copayment in a national context. The health care system in Canada provides the background for most of the studies, although these are often restricted to consider individual states, but also Belgium, Denmark, Ireland, Italy, Spain, Sweden, the USA, Czech Republic and Germany are represented in several studies. Hence, a wide selection of countries is represented. While most of the studies are restricted to consider a single country, the distributional consequences of copayment are analysed across several countries in four studies [26, 50, 63, 64]. Moreover, a few studies use variation in the general copayment levels between countries to identify the effect of copayment through cross-country comparisons [43, 44, 49].
Considering the data and methods of the remaining studies, it is seen from Table 1 that the vast majority are based on individual or household level data, while a few studies use aggregate data in which individual and household-specific characteristics cannot be identified. The studies are distributed evenly across survey and register data. The distributional consequences of copayment are analysed in a handful of studies by estimating various concentration and inequity indices [36, 63, 64, 68]. A large group of studies use panel data combined with natural experiments to identify the effect of copayment through difference-in-difference estimation [23, 24, 34, 48, 53, 54, 56, 66, 67], while two studies implement a difference-in-difference estimator using data from natural experiments and repeated cross-sections [30, 41]. Other studies analyse data from natural experiments using instrument variables [31, 42] or discontinuity [59] or kink [58] regression designs to overcome selection problems. Another large group of studies identifies the effects of copayment by estimating various other types of regressions [22, 25, 27, 46, 51, 61, 62, 65] or performing descriptive comparisons [37, 40, 52] based on panel or time series data combined with natural experiments. Three studies analyse data from actual experiments by descriptive comparisons [28, 29, 47], while the remainder identify effects using observational data and various types of regressions [26, 32, 33, 38, 39, 45, 55, 57, 58, 60].
As regards publication type, about one-fourth of the studies are published in the form of working papers at universities or other research institutions, while the rest are published as articles in peer-reviewed journals.Footnote 10
The results of the empirical studies are accounted for by topic as follows: The first section reviews the evidence on the presence of demand effects. The next section accounts for the evidence regarding the prevalence of health and substitution effects. The evidence on the distributional consequences of copayment is reviewed in the final section. Significance refers to a 5 % level if nothing else is mentioned. The order of magnitude of the effects are not summarised systematically across the reviewed studies for two reasons. First, the effects are not measured uniformly across the studies. Second, a number of studies do not identify the effect of a specific copayment but consider differences in copayment levels described in general terms.Footnote 11
Demand effects
Table 2 summarises the results of the identified studies of how copayment affects the use of health care services by type of service. For all types of health care services except hospitalisations, the majority of the reviewed studies find a negative effect of copayment. This indicates that a higher level of copayment generally reduces the use of health care services, while a lower level increases use.
Table 3 summarises the results of the studies that have estimated price elasticities of the demand for different types of health care services. The estimated price elasticities are all negative and numerically less than one, which means that the individual demand drops by less than 1 % following a 1 % increase in the price paid by the consumer at the time of consumption. Other aspects of the studies included in Table 3 are discussed in the relevant subsections, which are organised by type of health care service.
General practice
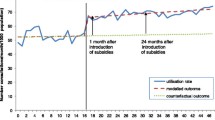
The three studies that use variation in the general copayment levels between countries to identify the effect of copayment through cross-country comparisons all find a negative association between the copayment level and the use of general practice [43, 44, 49], as do the studies using observational data and regression [26, 33, 55]. However, one of these studies finds that the effect tails off about 2.5 years after the introduction of copayment [55]. Moreover, it is found that the tendency to refrain from seeking medical help due to copayment is more pronounced among younger people [33, 55]. One study was based on a cross-country comparison [49] and two of the studies used observational data and regression to measure changes in the use of general practice as perceived by the individual (as opposed to actual use) [33, 55].
The majority of the reviewed studies use natural experiments combined with panel [24, 48, 54, 56, 62, 66, 67], repeated cross-section [27, 30, 41] or time series [37, 40] data to identify the effect of copayment for general practice on the use. The results of these studies are mixed: the majority find evidence of a negative demand effect of copayment [27, 30, 37, 40, 41, 48, 62, 66], some find no effect [24, 41, 56, 67], while one study finds that copayment leads to an increase in use [54]. The one study that finds an increase in the number of doctor visits following the introduction of copayment notes that this is most likely due to some structural circumstances related to the payment of suppliers [54].Footnote 12 The two studies using aggregate data and descriptive comparisons to identify the effect of an increase in copayment caused by a reform both find evidence of a negative association between the level of copayment and the use of general practice [37, 40]. Moreover, the effect is found to be relatively larger for home visits [40].
Likewise, the two studies that identify the effect of copayment using a sizeable increase in the copayment for office visits to general practitioners and specialists as well as medical home visits in Belgium both find a negative effect of copayment on the average number of all types of visits per year, but disagree on the order of magnitude cf. Table 3 [30, 62].Footnote 13 While one of these studies argues that the price elasticity of demand cannot be estimated for the upper income groups based on the observed change in copayment and limits itself to report elasticity estimates for the lower income groups [30], the other reports elasticity estimates for the total population [62]. Along a similar line, two studies analyse the effect of copayment for general practice based on natural experiments within the setting of the Irish health care system [41, 48]. One study exploits variation in the level of copayment that occurs because individuals with income below a certain threshold are exempted from copayment and find that this shift in the level of copayment affects the use of general practice significantly [48]. Moreover, this study finds that the negative effect of being charged copayment due to an increase in income is larger than the positive effect of being exempted due to low income. The other study uses exogenous variation stemming from the fact that individuals aged 70 and above are exempted from copayment regardless of their income and finds that while this increases the probability of having at least one annual GP visit significantly, it does not affect the frequency of visits [41].Footnote 14
On the contrary, two studies based on a natural experiment within the setting of the German health care system find no significant effect of introducing a small copayment for visits to general practitioners on neither the probability of having at least one visit nor the number of visits within a 3-month period [24, 56]. Both of these studies use a control group of privately insured, for whom no copayment is charged.
Finally, two studies use the fact that general practice visits often result in prescriptions [66, 67]. One of these studies finds that exempting children for copayment for general practice does not affect use approximated by number of prescriptions [67]. The other study finds that a sharp increase in copayment for prescription medicine curbs the demand for general practice and argues that this may be explained by the fact that the increased copayment for prescription medicine increases the average total costs associated with visits to the doctor [66].
Ambulatory care and hospitalisations
The four studies that analyse the effect of copayment on the use of ambulatory care and hospitalisations, respectively, find that while copayment reduces the use of ambulatory care [38–40], hospitalisations are less affected [39, 40, 43]. One study uses an increase in the general copayment level caused by a reform to identify the effect of copayment on the use of a broad selection of health care services [40]. This study finds that hospitalisations are the health care service that is the least affected by copayment, while the use of ambulatory care in the form of visits to accident and emergency departments is reduced. Another study uses aggregate data from Japan’s 47 prefectures, which differ in terms of copayment levels [39]. This study finds that while copayment reduces the use of both hospital (inpatient) care and ambulatory (outpatient) care, the use of ambulatory care is most sensitive to the copayment rate [39]. The study conducted within the setting of the South Korean health care system finds that while the individual demand for ambulatory care drops in consequence of increasing copayment, the demand for ambulatory care provided in a hospital setting is less price sensitive than the corresponding demand for ambulatory care at clinics [38]. Moreover, this study also finds that low income patients reduce their use of ambulatory care provided in hospitals as well as clinics relatively more than high income patients in consequence of copayment, cf. Table 3.
Prescription medicine
About one-third of the studies considering the effect of copayment on the use of prescription medicine estimate effects for the entire adult population [22, 34, 40, 45, 46, 58, 60]. With the exception of [22], these studies all find that copayment has a negative effect on use [34, 40, 45, 46, 58, 60]. One study considers hypothetical changes in the use of prescription medicine as perceived by the individual [45], while the remaining studies are based on data on actual use.
Another third of the studies exploit a shift in the level of copayment for prescription medicine at the transition from adult to elderly to identify demand effects of copayment [32, 35, 53, 61]. These studies unambiguously find that the drop in copayment levels around the age of retirement brings along an increase in the use of prescription medicine. One study also estimates demand effects for welfare recipients and finds that they reduce their use of prescription medicine relatively more than the elderly in consequence of copayment [35, 61].
The final third of the reviewed studies have estimated effects for various groups with a documented need for medicine due to illness. The results of this group of studies are mixed: some find no effect [51, 52], other find clear evidence of a negative demand effect of copayment [31, 42, 59], and yet other find that effects vary across different groups of patients and medicine types [23, 25]. Considering first the two studies that find no effect of copayment, one analyses the effect of a small copayment for prescriptions on the use of prescription medicine used to treat hypertension and anxiety, respectively, among the elderly users of these two types of medicine [52]. The other study focusses on the probability of complying with medical advice on medication for elderly who had a coronary [51]. Among the group of studies that find clear evidence of a negative demand effect of copayment for prescription medicine, one analyses the use of prescription medicine for elderly patients with rheumatoid arthritis [42], another considers a broader group of elderly chronic patients [31], while the most recent study analyses the use of insulin used to treat diabetes and penicillin mainly used to treat non-chronic illness [59]. In addition to a negative demand effect of copayment, the study of insulin users also finds that this patient group reacts to the price change by stockpiling medicine immediately before the rise in the copayment level [59]. The remaining two studies find varying effects across different groups of patients and medicine types. One study of hypertension patients treated with ACE-inhibitors finds that an abolition of copayment for prescriptions brings along an increase in compliance with medical advice on medication for the group of patients who do not take enough medicine to begin with, while the behaviour of the remaining patients is unaffected [23]. Another study of adult welfare recipients finds that an increase in the copayment level causes a significant drop in the use of inhaled corticosteroids used to treat asthma, while the use of neuroleptics used to treat schizophrenia and anticonvulsants used to treat epilepsy is not significantly affected [25]. Along a similar line, some studies find that copayment reduces the use of non-essential medicine relatively more than the use of essential medicine prescribed to specific diagnosis groups with the purpose of preventing deterioration in health and prolonging life [35, 46, 58, 61].
Overall, the empirical evidence thus indicates that the extent to which copayment affects the use of prescription medicine depends on the type of medicine as well as the part of the population in focus.
Prevention
The three studies based on controlled randomised experiments all find that copayment decreases the use of preventive health care services. One of these studies analyses the probability of getting a flu vaccination [47], while the other two consider prevention in the form of screening for ischaemic heart disease [28, 29].
Health effects and substitution
Table 4 summarises the results of the sparse literature that investigates whether copayment leads to deterioration in the public health and the extent to which copayment for some services within a given area, but not for others, causes substitution from the services that are subject to copayment to the ‘free’ services.
Prescription medicine
All studies included in Table 4 focus on the consequences of copayment for prescription medicine. Overall, the studies that tend to find negative effects of copayment on the use of prescription medicine find a positive effect of copayment on mortality and substitution to other types of health care services.Footnote 15
The majority of the reviewed studies consider the consequences of copayment for prescription medicine specific groups of elderly Canadians. Two of these studies find no evidence of either health effects or substitution for elderly who had a coronary [51] and users of antidepressants [65], respectively. The other two studies find evidence of substitution from medicine to other types of health care services for elderly patients with rheumatoid arthritis [42] and to some extent also for elderly welfare recipients [61]. More specifically, for elderly welfare recipients it is found that a relatively modest drop in the use of essential medicine following an increase in copayment leads to an increase in mortality as well as the use of accident and emergency departments, hospitalisations and long-term care, while a larger drop in the use of non-essential medicine does not affect any of these outcomes [61].
The two remaining studies are based on data from Italy and Spain, respectively. One study of Italian patients with hypertension finds that the probability of complying with medical advice on medication increases in the absence of copayment for the group of patients who do not take enough medicine to begin with and that this brings along a drop in mortality and hospitalisations [23]. The other study finds that exempting the elderly in Spain for copayment for prescription medicine does not reduce the number of hospitalisations significantly [53].
Distributional effects
The empirical literature takes two different approaches in investigating the distributional consequences of copayment.
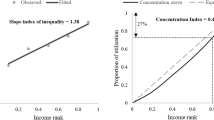
The first approach involves estimating various concentration and inequity indices of the financing and use of health care services and decomposing the total degree of inequity into various factors. The two studies considering the financing side both find that individuals in the lower end of the income distribution pay a relatively large share of their income in the form of copayment in all of the countries considered, i.e. the financing of health care services through copayment is regressive [63, 64]. Likewise, the two studies of use both find evidence that copayment brings about horizontal inequity in the use of health care services. One study finds that while the use of health care services is generally not associated with income, there is horizontal inequity in favour of high income individuals in the use of dental services and prescription medicine in a setting where both of these services are characterised by a high level of copayment [36]. The other study investigates the distributional consequences of copayment by comparing the degree of inequity in the use of prescription medicine over a number of years with varying copayment levels. Horizontal inequity indices indicate that while the degree of inequity is generally lower among the elderly (who are facing a lower copayment level than the remaining population), it increases when the elderly are charged higher copayments [68]. Finally, Or et al. [50] analyse the effect of various characteristics of the health care system on social inequities in the use of health care services across a number of European countries and find that copayment as a share of the total health expenditures has a small but statistically significant effect on the degree of social inequity in the use of general practice and specialist consultations.
The second approach is to compare the effect of copayment across different population groups in order to reveal whether vulnerable population groups reduce their use of health care services more than the general population in consequence of copayment. Approximately one-third of the demand studies summarised in Table 2 have taken this approach and extended their analyses to also consider the distributional consequences of copayment. Table 5 summarises the results of these studies with regard to the association between the price sensitivity of demand and various measures of vulnerability. A positive association between the price sensitivity of demand and low income, education level, social status or bad health, respectively, means that individuals with these characteristics reduce their use of health care services relatively more in consequence of copayment. Social status is defined by occupation and health is measured by self-perceived health and the prevalence of chronic conditions in the reviewed studies.
General practice
The majority of the reviewed studies find that vulnerable population groups reduce their use of general practice more than the general population in consequence of copayment [33, 43, 44, 49, 55, 57]. Two of the studies that do not find any differences in use between different population groups [24, 56] are characterised by not finding any demand effects of copayment for either the general population or vulnerable subgroups. The third study [27] considered a population of state government and higher education employees, a group that enjoys moderate incomes, and therefore does not provide any information on individuals with very low incomes.
Prescription medicine
A similar pattern applies to the studies of prescription medicine, where the majority of the reviewed studies also find that copayment leads to a larger reduction in the use of prescription medicine for vulnerable population groups than for the general population [42, 45, 58, 59]. Two studies do not find any demand effects of copayment neither for a population of elderly users of various types of prescription medicine nor for vulnerable subgroups [51, 52]. Finally, a single study finds the use of prescription medicine to be less price sensitive for low income individuals and individuals in bad health than for the remaining population [31]. This result runs counter to the results of the remaining empirical literature.
Ambulatory care and hospitalisations
The study of ambulatory care conducted within the setting of the South Korean health care system finds that low income patients reduce their use of ambulatory care provided in hospitals as well as clinics relatively more than high income patients in consequence of copayment [38]. Another study based on aggregate data from Japan finds that low income patients reduce their use of hospital (inpatient) care more than the remaining population in consequence of copayment, while there are no systematic differences for ambulatory (outpatient) care [39].
Conclusions and perspectives
This article reviews the quantitative evidence on the behavioural effects of copayment for different types of health care services across a wide range of countries. The present review distinguishes itself from previous reviews, also including studies of various types of health care services and entire populations, by having a high degree of transparency about the search strategy used to identify the studies included in the review as well as the criteria for inclusion, and by including the most recent literature.
The main results of the review can be summarised and discussed as follows: Considering the demand effects, the majority of the reviewed studies find that copayment reduces the use of prescription medicine, consultations with general practitioners and specialists, and ambulatory care, respectively, thereby potentially lowering the total health care costs. In general the literature finds no significant effects of copayment on the prevalence of hospitalisations, which implies that copayment for this type of treatment mainly shifts the burden of financing from the public coffers to the users rather than reduces demand. One of several reasons why the demand for consultations with general practitioners reacts more to copayment than hospitalisations could be due to differences in accessibility. For example, the finding that the demand for hospital care is largely price inelastic probably has something to do with the fact that access is usually restricted by some sort of visitation, either through general practice or on site. This implies that hospital patients have a regular need for care and therefore do not reduce their use notably in consequence of copayment. Along a similar line, another explanatory factor is that contacts to general practitioners are usually initiated by the patient, whereas hospitalisations to some extent may be argued to be a provider-initiated service, over which the patient has far less control [69].
The empirical evidence on whether copayment for some services, but not for others, causes substitution from the services that are subject to copayment to the ‘free’ services rather than lower total use is sparse and mixed. Likewise, the health effects of copayment have only been analysed empirically in a limited number of studies, of which half did not find any significant effects in the short term. This result is, however, restricted by the fact that the reviewed studies primarily consider effects on mortality, which is a rather coarse measure of health. It can thus not be ruled out that copayment affects health as measured by more nuanced indicators. As regards copayment for prescription medicine, one study finds that copayment reduces the use of non-essential medicine relatively more than the use of essential medicine [61]. However, most studies are unable to say anything about whether the eliminated use is necessary from a medical point of view. Moreover, none of the data sets used in the empirical literature spans a sufficient sequence of years to be able to make inference about the long-term consequences.
Finally, the empirical literature confirms almost unambiguously that distributional consequences are a real matter of concern and not just a theoretical construct. On the financing side, the reviewed studies find that copayment represents an unequal type of financing vertically as well as horizontally. The empirical evidence likewise indicates that vulnerable groups, including individuals with low income and in particular need of care, reduce their use relatively more than the remaining population in consequence of copayment. This highlights the need for protecting particularly vulnerable groups from the consequences of copayment, e.g. by making the copayment income dependent or exempting groups in particular need of the services in question. The strategy of exempting certain groups from copayment suffers from the weakness that it may result in rather arbitrary dividing lines [69]. Moreover, exempting vulnerable groups from copayment implies that the burden of financing primarily falls on the working population, who already contribute considerably to the health system through their tax payment. If the tax on labour is held constant and only the working population is required to copay, this group will experience an increase in their total payment towards the health system, which may over time reduce their support for the public system. Another possibility is to encourage people to purchase supplementary private health insurance policies that cover the copayment. This, however, only benefits those who can afford to pay the insurance premium. Moreover, economic theory predicts that supplementary private health insurance counteracts any demand effects of copayment that may occur by lowering the price paid by the consumer.
Hence, the results of the empirical literature indicate that introducing copayment for new types of health care services or extending existing schemes involves some important economic and political trade-offs. It is thus important for the responsible policymakers to be clear about what they wish to obtain by introducing copayment and how to counter the possible side effects.
Considering the welfare consequences of copayment, economic theory predicts that under perfect competition individuals who are charged the full cost consume until the point where the marginal cost of producing the service equals their willingness to pay given preferences and income. Based on this line of reasoning, it may be argued that copayment brings the level of use closer to the socially optimal level than tax funding. This argument, however, presupposes that individuals are able to value the benefits and disadvantages of use, which is often not the case for health care services. Moreover, market solutions are not always optimal within the health area, where the possible presence of information problems, externalities and myopic preferences may well mean that the optimal use for the individual does not equal the optimal use for society as a whole. Adding further complications is the fact that the need for and thus also the individual demand for health care services is characterised by uncertainty, which is an important reason why these services were financed through taxes and social insurance systems in the first place [17]. Hence, the case of full copayment should not necessarily be used as benchmark for efficiency within the health area. Another issue that should also be taken into account in an overall assessment of the distributional consequences of copayment is that the alternative to copayment, i.e. funding through taxes or social insurance systems, has been shown theoretically as well as empirically to redistribute income from high to low income groups [70, 71].
Other considerations than equity and efficiency also apply to general health policy [16]. For one thing, the cost and feasibility of administering a given copayment scheme is an important consideration. In this regard it is worth noting that the complexity and costs of administration are likely to increase if efforts are made to preserve equity by exempting vulnerable populations from payment. Another issue that may constitute an important constraint on implementing and changing copayment arrangements is the question of public acceptability. A survey of public attitudes in several countries indicates that copayment is a hotly debated political issue and illustrates a range of contrasting public attitudes [16].
Finally, it is important to keep in mind that copayment is only one of several instruments with potential to lower the use of services and the corresponding expenditure within the health area. Visitation and waiting lists as well as mechanisms seeking to affect the suppliers, such as reimbursement schemes, are also capable of lowering the use of health care services, which often involves a complex interaction of factors [16, 69]. This means that politicians contemplating copayment as a means to curb the increasing health expenditures also need to consider the incentives facing, e.g. the pharmaceutical industry, hospitals, general practitioners, specialists, nursing homes and so on, given that these actors also have a share in the responsibility for decision making on accessibility, use and expenditures related to the health system. In an overall reform perspective, it is thus of crucial importance that copayment is seen in connection with other possible steering instruments.
Notes
Given that demand is approximated by actual use in all of the reviewed studies, the terms demand and use are applied interchangeably throughout the article.
Examples of health care services for which the price elasticity of demand is most likely limited are chemotherapy, bypass operations and other major interventions, which may be lifesaving but pose considerable health risks in themselves.
For example, it is possible that increased copayment for prescription medicine reduces the demand for general practice consultations, which often result in a prescription.
Master Theses are not systematically available from all institutes and faculties and are therefore not included.
A review of the empirical literature on the consequences of different types of copayment within the pharmaceutical area found that indirect copayment has the ability to shift use from expensive to cheaper types of medicine, although often with modest savings in consequence [5].
See Atherly [20] for a review of effect studies for the elderly in the US, for whom variation in the level of copayment is mainly cause by voluntary purchase of supplementary private health insurance and Kiil [21] for an overview of effect studies of voluntary private health insurance in universal health care systems.
* Indicates a truncated search, i.e. a search on the stem of the word as well as its different endings.
Relevant employees at a number of Danish research institutions, ministries and interest groups were also contacted in order to ensure that all relevant literature was included. However, this did not result in the identification of additional studies.
In consequence of the rather general search terms used, the main reason that many studies were classified as being irrelevant and discarded was that they dealt with something else than copayment. More specific groups of discarded studies include studies that investigate effects of supply-side payment systems, studies based on data collected prior to 1990, studies of indirect copayment, and studies that identified the effect of copayment by using variation in copayment rates between individuals who have voluntarily selected themselves into different schemes or purchased complementary private health insurance.
Some of the more recent working papers may reasonably be expected to be published in article format at a later point in time.
Specifically, while there is an upper limit for the total earnings of doctors, they are allowed to exceed the threshold with income stemming from copayment. This structure may unintentionally have created an incentive for the doctors to seek to increase the visit rate among the patients who are required to copay in order to increase total earnings.
Cockx and Brasseur [30] adjust the estimates reported in van de Voorde et al. [62] by taking into account that the increases in the relative copayments for the three types of doctor visits considered were not proportional and decomposing the demand effect into an income effect and a substitution effect.
The authors note that the fact that general practitioners receive a fixed fee for patients aged 70 and above creates an incentive for the general practitioners to seek to limit the number of visits for this patient group.
With the exception of Puig-Junoy et al. [53].
References
Rovira, J., et al.: Comparing cost-sharing in European Union member states: a system-oriented framework. In: Leidl, R. (ed.) Health Care and Its Financing in the Single European Market, pp. 183–211. IOS Press, Amsterdam (1998)
Hansen, S.W., Houlberg, K.: Brugerbetaling på sundheds- og ældreområdet i komparativt perspektiv. AKF, Copenhagen (2012)
Gibson, T.B., Ozminkowski, R.J., Goetzel, R.Z.: The effects of prescription drug cost sharing: a review of the evidence. Am. J. Manag. Care 11, 730–740 (2005)
Goldman, D.P., Joyce, G.F., Zheng, Y.: Prescription drug cost sharing. Associations with medication and medical utilization and spending and health. J. Am. Med. Assoc. 298(1), 61–69 (2007)
Gemmill, M.C., Thomson, S., Mossialos, E.: What impact do prescription drug charges have on efficiency and equity? Evidence from high-income countries. Int. J. Equity Health 7(12), (2008)
Lexchin, J., Grootendorst, P.: Effects of prescription drug user fees on drug and health services use and on health status in vulnerable populations: a systematic review of the evidence. Int. J. Health Serv. 34(1), 101–122 (2004)
Carrieri, V.: The effects of cost-sharing in health care: what do we know from empirical evidence? Economia politica. J. Anal. Inst. Econ. 2, 351–374 (2010)
Holst, J.: Patient Cost Sharing—Reforms without Evidence, pp. 1–146. Social Science Research Centre, Berlin (2010)
Swartz, K.: Cost-sharing: effects on spending and outcomes. In: The Synthesis Project, pp. 1–36. Robert Wood Johnson Foundation (2010)
Rice, T., Matsuoka, K.Y.: The impact of cost-sharing on appropriate utilization and health status: a review of the literature on seniors. Med. Care Res. Rev. 61(4), 415–452 (2004)
Manning, W.G., et al.: Health insurance and the demand for medical care: evidence from a randomized experiment. Am. Econ. Rev. 77, 251–277 (1987)
Lohr, K.N., et al.: Use of medical care in the RAND health insurance experiment. Med. Care 24(9 Suppl), S1–S87 (1986)
Shapiro, M.F., Ware, J.E., Sherbourne, C.D.: Effects of cost sharing on seeking care for serious and minor symptoms. Results of a randomized controlled trial. Ann. Intern. Med. 104(2), 246–251 (1986)
Siu, A.L., et al.: Inappropriate use of hospitals in a randomized trial of health insurance plans. N. Engl. J. Med. 315, 1259–1266 (1986)
Brook, R.H., et al.: Does free care improve adults’ health? Results from a randomized controlled trial. N. Engl. J. Med. 309(23), 1426–1434 (1983)
Robinson, R.: User charges for health care. In: Mossialos, E., et al. (eds.) Funding Health Care: Options for Europe, pp. 161–183. Open University Press, London (2002)
Arrow, K.J.: Uncertainty and the welfare economics of medical care. Am. Econ. Rev. 53, 941–973 (1963)
Pauly, M.V.: The economics of moral hazard: comment. Am. Econ. Rev. 58, 531–537 (1968)
The World Bank: Country and Lending Groups. 2012 [cited 2012 27/2]. Available from: http://data.worldbank.org/about/country-classifications/country-and-lending-groups#High_income
Atherly, A.: Medicare’s accidental stepchild. Med. Care Res. Rev. 2, 131–161 (2001)
Kiil, A.: Does employment-based private health insurance increase the use of covered health care services? A matching estimator approach. Int. J. Health Care Financ. Econ. 12(1), 1–38 (2012)
Almarsdóttir, A.B., Morgall, J.M., Grimsson, A.: Cost containment of pharmaceutical use in Iceland: the impact of liberalisation and user charges. J. Health Serv. Res. Policy 5(2), 109–113 (2000)
Atella, V., et al.: Drug compliance, co-payment and health outcomes: evidence from a panel of Italian patients. Health Econ. 15, 875–892 (2006)
Augurzky, B., Bauer, T.K., Schaffner, S.: Copayments in the German Health System: Does It Work? in IZA Discussion Paper No. 2290 (2006)
Blais, L., et al.: Impact of a cost sharing drug insurance plan on drug utilization among individuals receiving social assistance. Health Policy 64, 163–172 (2003)
Bolin, K., et al.: Utilisation of physician services in the 50+ population. The relative importance of individual versus institutional factors in 10 European countries. Int. J. Health Care Financ. Econ. 9(1), 83–112 (2009)
Cherkin, D.C., Grothaus, L., Wagner, E.H.: Is magnitude of co-payment effect related to income? Using census data for health services research. Soc. Sci. Med. 43(1), 33–41 (1992)
Christensen, B.: Characteristics of attenders and non-attenders at health examinations for ischaemic heart disease in general practice. Scand. J. Prim. Health Care 13, 26–31 (1995)
Christensen, B.: Payment and attendance at general practice preventive health examinations. Fam. Med. 27(8), 531–534 (1995)
Cockx, B., Brasseur, C.: The demand for physician services. Evidence from a natural experiment. J. Health Econ. 22, 881–913 (2003)
Contoyannis, P., et al.: Estimating the price elasticity of expenditure for prescription drugs in the presence of non-linear price schedules: an illustration from Quebec. Can. Health Econ. 14, 909–923 (2005)
Costa-Font, J., Kanavos, P., Rovira, J.: Determinants of out-of-pocket pharmaceutical expenditure and access to drugs in Catalonia. Appl. Econ. 39(5), 541–551 (2007)
Elofsson, S., Undén, A.-L., Krakau, I.: Patient charges—a hindrance to financially and psychologically disadvantage groups seeking care. Soc. Sci. Med. 46(10), 1375–1380 (1998)
Fiorio, C.V., Siciliani, L.: Co-payments and the demand for pharmaceuticals: evidence from Italy. Econ. Model. 27, 835–841 (2010)
Grootendorst, P., Levine, M.: Do Drug Plans Matter? Effects of Drug Plan Eligibility on Drug Use Among the Elderly, Social Assistance Recipients and the General Population, in QSEP Research Report No. 372. McMaster University (2002)
Gundgaard, J.: Income-related inequality in utilization of health services in Denmark: evidence from Funen County. Scand. J. Public Health 34, 10 (2006)
Jordin, B., Engholm, G.: Besöksfrekvenser för unga och äldre efter införandet av avgiftsfrihet för patienter yngre än 20 år. Socialmedicinsk tidsskrift: Organ för sjuk- och hälsovård 1, 85–90 (2001)
Kim, J.Y., Ko, S.K., Yang, B.M.: The effects of patient cost sharing on ambulatory utilization in South Korea. Health Policy 72(3), 293–300 (2005)
Kupor, S.A., et al.: The effect of copayments and income on the utilization of medical care by subscribers to Japan’s National Health Insurance System. Int. J. Health Serv. 25(2), 295–312 (1995)
Krutilová, V.: Impact of user fees in health care system on health care consumption. Rev. Econ. Perspect. 10(4), 113–132 (2010)
Layte, R., et al.: Do consultation charges deter general practitioner use among older people? Soc. Sci. Med. 68, 1432–1438 (2009)
Li, X., et al.: The impact of cost sharing of prescription drug expenditures on health care utilization by the elderly: own- and cross-price elasticities. Health Policy 82, 340–347 (2007)
Lostao, L., et al.: Patient cost sharing and social inequalities in access to health care in three western European countries. Soc. Sci. Med. 65, 367–376 (2007)
Lostao, L., et al.: Patient cost sharing and physician visits by socioeconomic position: findings in three Western European countries. J. Epidemiol. Community Health 61(5), 416–420 (2007)
Lundberg, L., et al.: Effects of user charges on the use of prescription medicines in different socio-economic groups. Health Policy 44, 123–134 (1998)
McManus, P., et al.: Prescription drug utilization following patient co-payment changes in Australia. Pharmacoepidemiol. Drug Saf. 5, 385–392 (1996)
Nexøe, J., Kragstrup, J., Rønne, T.: Impact of postal invitations and user fee on influenza vaccination rates among the elderly. Scand. J. Prim. Health Care 15, 109–112 (1997)
Nolan, A.: Evaluating the impact of eligibility for free care on the use of general practitioner (GP) services: a difference-in-difference matching approach. Soc. Sci. Med. 67, 1164–1172 (2008)
O’Reilly, D., et al.: Consultation charges in Ireland deter a large proportion of patients from seeing the GP: results of a cross-sectional survey. Eur. J. Gen. Pract. 13, 231–236 (2007)
Or, Z., Jusot, F., Yilmaz, E.: Impact of Health Care System on Socioeconomic Inequalities in Doctor Use, in IRDES Working Paper No. 17, Paris (2008)
Pilote, L., et al.: The effects of cost-sharing on essential drug prescriptions, utilization of medical care and outcomes after acute myocardial infarction in elderly patients. Can. Med. Assoc. J. 167(3), 246–252 (2002)
Poirier, S., et al.: The effect of a $2 co-payment on prescription refill rates of quebec elderly and its relationship to socio-economic status. Can. Pharm. J. 130(10), 30–34 (1998)
Puig-Junoy, J., García-Gómez, P., Casado-Marín, D.: Free Medicines Thanks to Retirement: Moral Hazard and Hospitalization Offsets in an NHS, in Tintenberg Institute Discussion Paper 108/3 (2011)
Rosen, B., et al.: When co-payments for physician visits can affect supply as well as demand: findings from a natural experiment in Israel’s national health insurance system. Int. J. Health Plan. Manag. 26, e68–e84 (2011)
Rückert, I.-M., Böcken, J., Mielck, A.: Are German patients burdened by the practice charge for physician visits (‘Praxisgebuehr’)? A cross sectional analysis of socio-economic and health related factors. BMC Health Serv. Res. 8(232), 2008
Schreyögg, J., Grabka, M.M.: Copayments for Ambulatory Care in Germany: A Natural Experiment Using a Difference-in-Difference Approach, in SOEP Papers on Multidisciplinary Panel Data Research. DIW, Berlin (2008)
Scott, K.M., Marwick, J.C., Crampton, P.R.: Utilization of general practitioner services in New Zealand and its relationship with income, ethnicity and government subsidy. Health Serv. Manag. Res. 16(1), 45–55 (2003)
Simonsen, M., Skipper, L., Skipper, N.: Price Sensitivity of Demand for Prescription Drugs: Exploiting a Regression Kink Design, in Economics Working Paper. School of Economics and Management, Aarhus University (2010)
Skipper, N.: On Utilization and Stockpiling of Prescription Drugs when Co-payments Increase: Heterogeneity Across Types of Drugs, in Economics Working Paper. School of Economics and Management, Aarhus University (2010)
Street, A., Jones, A., Furuta, A.: Cost-sharing and pharmaceutical utilisation and expenditure in Russia. J. Health Econ. 18, 459–472 (1999)
Tamblyn, R., et al.: Adverse events associated with prescription drug cost-sharing among poor and elderly persons. J. Am. Med. Assoc. 285(4), 421–429 (2001)
van de Voorde, C., van Doorslaer, E., Schokkaert, E.: Effects of cost sharing on physician utilization under favourable conditions for supplier-induced demand. Health Econ. 10, 457–471 (2001)
van Doorslaer, E., et al.: The redistributive effect of health care finance in twelve OECD countries. J. Health Econ. 18, 291–313 (1999)
Wagstaff, A., et al.: Equity in the finance of health care: some further international comparisons. J. Health Econ. 18, 263–290 (1999)
Wang, P.S., et al.: Impact of drug cost sharing on service use and adverse clinical outcomes in elderly receiving antidepressants. J. Mental Health Policy Econ. 13(1), 37–44 (2010)
Winkelmann, R.: Co-payments for prescription drugs and the demand for doctor visits—evidence from a natural experiment. Health Econ. 13, 1081–1089 (2004)
Zápal, J.: Doctor-visit co-payment exemption for children: first look at the data. Czech J. Econ. Financ. 60(1), 58–72 (2010)
Zhong, H.: Equity in pharmaceutical utilization in Ontario: a cross-section and over time analysis. Can. Public Policy 33(4), 487–507 (2007)
Louckx, F.: Patient cost sharing and access to health care. In: Mackenbach, J., Bakker, M. (eds.) Reducing Inequalities in Health. A European Perspective, pp. 188–198. Routledge, London (2002)
Paulus, A., Sutherland, H., Tsakloglou, P.: The distributional impact of in-kind public benefits in European countries. J. Policy Anal. Manag. 29, 243–266 (2010)
Aaberge, R., et al.: The Distributional Impact of Public Services when Needs Differ, in IZA Discussion Paper No. 4826. Institute for the study of Labor, Bonn (2010)
Acknowledgments
The authors would like to thank research librarian Lisa la Cour for providing valuable guidance on how to search for literature and helping us collect the relevant studies and two anonymous reviewers for their helpful comments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kiil, A., Houlberg, K. How does copayment for health care services affect demand, health and redistribution? A systematic review of the empirical evidence from 1990 to 2011. Eur J Health Econ 15, 813–828 (2014). https://doi.org/10.1007/s10198-013-0526-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-013-0526-8