Abstract
Background
We occasionally encounter malignant pleural mesothelioma (MPM) of no apparent tumor or pleural thickening that is radiological early MPM. This study aimed to examine the clinicopathological outcomes of radiological early MPM.
Methods
Patients with MPM treated with neoadjuvant chemotherapy and planned surgery at the time of diagnosis between July 2004 and December 2019 were retrospectively examined. Pretreatment maximal pleural thickness of all patients was measured on chest computed tomography. We extracted and investigated the patients who exhibited a lack of pleural thickening or visible tumor, which was defined as radiological early MPM. Survival was analyzed by the Kaplan–Meier method.
Results
Of 296treated patients, 16 (5.4%) exhibited radiological early MPM. Fourteen (87.5%) of these patients underwent pleurectomy/decortication and 2 (12.5%) underwent extrapleural pneumonectomy. Pathological stage T1 disease was diagnosed in 14 (87.5%) patients; 2 (12.5%) exhibited pulmonary parenchymal invasion (pathological stage T2). Lymphatic invasion was detected in only 1 patient. Lymph node metastases and vascular invasion were not detected. Median follow-up was 42 months. Median progression-free survival and median overall survival were 40.7 and 56.1 months, respectively. The 3-year progression-free survival and overall survival rates were 84.8% and 83.6%, respectively.
Conclusions
Radiological early MPM occurs in approximately 1 of every 20 patients treated with neoadjuvant chemotherapy and surgery planned at the time of diagnosis in an experienced center. Radiological early MPM was associated with early pathological stage and long-term survival.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The current TNM staging system for malignant pleural mesothelioma (MPM) utilizes only anatomical descriptors of disease extent and invasion [1]. Preoperative clinical staging is challenging because MPM commonly has the unusual and unique growth pattern of pleural rind formation rather than development from a concentrically enlarging primary lesion, as seen in most other malignancies [1, 2].
Pleural thickness has recently been considered a novel prognostic factor in MPM [1, 3]. Measuring pleural thickness is useful and easy to perform without specific software or additional cost [3]. A recent analysis from the International Association for the Study of Lung Cancer (IASLC) database demonstrated the potential impact of pleural thickness on survival in a large cohort of MPM patients, suggesting further examination with regard to incorporation into future staging [1]. We previously reported that preoperative pleural thickness was an independent prognostic factor in patients who underwent multimodal treatment [3]. In contrast, MPM patients with no apparent tumor or pleural thickening other than pleural effusion on chest computed tomography (CT) are occasionally encountered. Hasegawa et al. proposed this type of MPM as radiological early MPM or radiological T0 MPM [4]. To our knowledge, no study has examined outcomes associated with this type of MPM. In clinical practice, radiological early MPM or radiological T0 MPM belongs to clinical T1 disease.
Based on our experience, we hypothesized that radiological early MPM has favorable clinicopathological outcomes. Early intervention may play a key role in improving prognosis of MPM, similar to other malignancies [4]. Therefore, this study aimed to examine clinicopathological outcomes of radiological early MPM.
Materials and methods
Study design
We reviewed the medical records of patients who registered in the prospective MPM database of our hospital surgery program between July 2004 and December 2019. Database eligibility criteria were as follows: non-sarcomatoid histological subtype on pleural biopsy, clinical stage T1-3N0-1M0 (International Mesothelioma Interest Group (IMIG) and IASLC staging system, 8th edition [1, 5]), Eastern Cooperative Oncology Group performance status (PS) 0 or 1, and no major comorbidity. We excluded patients with missing radiological data.
Treatment protocol
All patients received neoadjuvant chemotherapy (NAC) with platinum plus pemetrexed for a total of three cycles. Tumor response was assessed after NAC using a modified version of the Response Evaluation Criteria in Solid Tumors [6]. Curative-intent surgery was planned for patients who achieved a tumor response assessed as stable disease or better within 2 months after completion of NAC. In our hospital, extrapleural pneumonectomy (EPP) was performed before September 2012. Pleurectomy/decortication (P/D) was introduced in September 2012 and has been the main operative treatment for MPM since. Adjuvant chemotherapy was performed within 12 weeks of P/D. Completion of adjuvant chemotherapy was defined as having completed two or more cycles. Adjuvant high-dose hemithoracic irradiation using intensity-modulated radiotherapy was performed within 12 weeks of EPP. A total dose of 54 Gy was delivered in 30 fractions at 1.8 Gy/day. The above treatment plans were performed as per previous reports [3, 7, 8].
Measurement of pretreatment pleural thickness
Pretreatment maximal pleural thickness of all patients was measured by two thoracic surgeons using thin-section contrast-enhanced (CE) chest CT as described in the IASLC mesothelioma staging project and our previous report [1, 3]. First, the hemithorax was divided into three zones (upper, middle, and lower) using axial thin sections. Zones were defined as follows: the upper zone extended from the apex of the lung to the inferior margin of the aortic arch; the middle zone included the pleura between the upper and lower zones; the lower zone included the first image on which the left atrium was seen and extended inferiorly. The preoperative maximum pleural thickness perpendicular to the chest wall or mediastinum was measured at each of the three levels (Fig. 1).
Measurement of pretreatment pleural thickness. The thoracic cavity was divided into 3 levels (upper, middle, and lower) (a). Pleural thickness was measured perpendicular to the chest wall or mediastinum at each of the 3 levels on axial computed tomography images; the double-headed arrow indicates the measurement of pleural thickness (b). A case of MPM unaccompanied by pleural thickening or tumor in any of the 3 levels, classified as radiological early MPM (c). MPM, malignant pleural mesothelioma
Definition of radiological early MPM, outcome evaluation
We extracted the patients who exhibited no pleural thickening or tumor in any of the three zones on pretreatment CECT from the MPM database; these patients were defined as radiological early MPM.
Clinical data, including patient characteristics, operative reports, radiological findings, histopathology, and survival, were collected by chart review. Patients were followed up every 1 to 3 months after multimodality treatment using CT or fluorodeoxy-d-glucose positron emission tomography (FDG-PET)/CT. Disease relapse was treated appropriately according to patient condition and PS. Overall survival (OS) was calculated from the date of pathological diagnosis to the date of most recent follow-up or death. Progression-free survival (PFS) was calculated from the date of pathological diagnosis to the date of most recent follow-up or development of progressive disease.
Statistical analysis
Analysis was based on data updated as of March 31, 2020. Survival analysis was performed using the Kaplan–Meier method. All analyses were performed using JMP 14 software (SAS Institute Inc., Cary, NC, USA).
Ethics
The institutional review board of the Hyogo College of Medicine (No. 3537) approved the study on May 23, 2020, and written informed consent was obtained from all patients.
Results
Patient characteristics
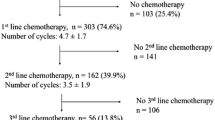
Figure 2 shows the flowchart of the study. Three hundred consecutive MPM patients were eligible for multimodality treatment. We excluded four because of missing data; thus, the sample size was 296. Of 296 patients, 16 patients (5.4%) exhibited no pleural thickening or tumor on pretreatment chest CT, which was classified as radiological early MPM. All patients underwent NAC followed by curative-intent surgery.
Flowchart of the study. Among the 300 eligible patients, 4 were excluded because of missing data. Sixteen patients exhibited unaccompanied by pretreatment pleural thickening or tumor on chest computed tomography, classifying as radiological early MPM. Of these, all patients completed neoadjuvant chemotherapy followed by curative-intent surgery. MCR, macroscopic complete resection; MPM, malignant pleural mesothelioma
Triggers initiating diagnostic procedures are summarized in Fig. 3. Among the 16 patients with radiological early MPM, seven patients exhibited some symptoms: 5 patients presented with dyspnea and 2 with chest pain. Of the nine patients who did not present with any symptoms, six patients exhibited abnormal chest shadow by medical checkup and three patients were found to have pleural nodules incidentally during lung cancer resections. Except for these three patients, 13 patients exhibited pleural effusion and underwent thoracentesis for analysis using the cell block technique, leading to the diagnosis of MPM. Finally, 15 patients underwent thoracoscopic pleural biopsy. One patients completed NAC without pleural biopsy at a previous hospital.
Characteristics of the 16 patients with radiological early MPM are shown in Table 1. Median age was 67 years (range 51–79). Ten were men (62.5%) and most had PS 0 (93.8%). The tumor involved the left pleura in 10 patients (62.5%). The median maximum standardized uptake value on FDG-PET/CT was 0 (range 0–7.2). There was no evidence of FDG accumulation in nine patients. Two patients had a history of preoperative pleurodesis (Talc), and FDG-PET/CT revealed FDG accumulation (SUV max, 7) in the talcoma. There was mild FDG accumulation in five patients (SUV max, 1–3). All patients were clinical stage 1A. P/D was performed in 14 patients (87.5%); 2 patients (12.5%) underwent EPP. Macroscopic complete resection was achieved in all patients. Pericardium and diaphragm patch reconstructions were performed in 2 (12.5%) and 4 (25.0%) patients, respectively. Median postoperative hospital stay was 29 days (range 15–63). Although one patient required reoperation for empyema, both 30- and 90-day mortality rates were 0%. Twelve patients (75.0%) completed adjuvant treatment. Of the 14 patients who underwent P/D, 10 patients completed adjuvant chemotherapy, whereas 4 did not undergo adjuvant chemotherapy because of patient refusal (n = 3) and postoperative complication (interstitial pneumonia, n = 1). Two patients who underwent EPP completed adjuvant radiotherapy.
Pathological findings
Table 2 summarizes the pathological findings of the 16 radiological early MPM patients. The pathological findings were based on surgically resected pleura. There were no patients with localized MPM, and all the patients were diagnosed with diffuse MPM. All patients exhibited epithelioid-type MPM. The most common histologic subtype was tubulopapillary (n=10, 62.5%), followed by trabecular (n=6, 37.5%). No patient exhibited micropapillary, solid, or pleomorphic subtype. Two patients (12.5%) exhibited pulmonary parenchymal invasion (pathological T2 stage). Fourteen patients (87.5%) exhibited pathological T1 stage; 3 of these tumors were limited to the ipsilateral parietal pleura. No lymph node metastases were seen. In this regard, 14 patients (87.5%) were stage IA and 2 (12.5%) were stage IB. Lymphatic invasion was detected in only 1 patient (6.3%). There was no case of vascular invasion. Port site infiltration occurred in7 patients (43.8%). Median p53 and MIB-1 labeling indices were6.5 (range 0–80) and 3 (range 1–16), respectively.
Survival and progression-free survival
Among the 16radiological early MPM patients, median follow-up was 42 months (range 8–77). Seven patients (43.8%) experienced recurrence. Recurrence was local in 4 patients (57.1%), distant in 2 (28.6%), and both local and distant in 1 (14.3%). The most common pattern of local recurrence (n=5) was pleural thickening (n=4), followed by chest wall mass (n=1). In contrast, the most common pattern of distant recurrence (n= 3) was peritoneal dissemination (n=2), followed by contralateral intrapulmonary metastasis (n=1). Of the 6 patients who died, 1 died without evidence of tumor recurrence. Kaplan–Meier curves for OS and PFS are shown in Fig. 4. The 2- and 3-year OS rates were 92.9% and 83.6%, respectively (median OS, 56.1 months). Both2- and 3-year PFS rates were 84.8% (median PFS, 40.7 months).
Triggers initiating diagnostic procedures. Of the 16 patients with radiological early MPM, 7 presented with some symptoms. Six patients exhibited abnormal chest shadow by medical checkup, and three patients were found to have pleural nodules incidentally during lung cancer resection. Thirteen patients exhibited pleural effusion and underwent thoracentesis for further analysis using the cell block technique, leading to the diagnosis of MPM. Finally, 15 patients underwent thoracoscopic pleural biopsy. One patient had completed NAC without pleural biopsy at a previous hospital. MPM, malignant pleural mesothelioma
Representative radiological early MPM patient
A representative study patient is described here to highlight the potential clinical importance of radiological early MPM. A 61-year old man was diagnosed with left epithelioid-type MPM on thoracoscopic pleural biopsy. No apparent tumor was macroscopically visible at thoracoscopy (Fig. 5a). On preoperative CECT, the patient exhibited only a left pleural effusion unaccompanied by pleural thickening or visible tumor (Fig. 5b). P/D was performed and the patient’s postoperative course was uneventful. The resected specimen showed normal pleural thickening of the parietal and visceral pleura (Fig. 5c). Histopathological examination showed epithelioid-type MPM limited to the ipsilateral pleura (Fig. 5d); no evidence of lymph node metastasis was seen and lymphatic invasion and vascular invasion were not detected. The p53 and MIB-1 labeling indices were 3 and 7, respectively. The patient has remained recurrence-free for 3 years after diagnosis.
Representative case of radiological early MPM. On thoracoscopy, no apparent tumor was macroscopically visible (a). Pretreatment contrast-enhanced computed tomography showed only a left pleural effusion unaccompanied by pleural thickening or visible tumor (b). The resected specimen after pleurectomy/decortication showed normal pleural thickening of the parietal and visceral pleura (c). Histopathologically, the tumor was epithelioid-type MPM and limited to the ipsilateral pleura (d). MPM, malignant pleural mesothelioma
Discussion
This study showed three important findings regarding radiological early MPM. First, radiological early MPM occurred in 16 of 296 patients (5.4%) treated with NAC and surgery that was planned at the time of diagnosis in an experienced center. Second, radiological early MPM was associated with early pathological stage: Among the 16 patients, 14 exhibited pathological T1 stage. Lymph node metastases and vascular invasion were not seen, and lymphatic invasion was detected in only one patient. Third, radiological early MPM stage was associated with good OS and PFS. To our knowledge, this is the first study to demonstrate clinicopathological outcomes for radiological early MPM.
MPM is an aggressive tumor that frequently recurs after treatment [9]. However, early diagnosis and intervention may provide a better prognosis. In fact, MPM patients who undergo multimodality treatment in the early stages of disease have improved survival [7, 8, 10,11,12]. Several previous reports have found that patients with radiologically undetectable MPM survive longer [13, 14]. Hasegawa et al. proposed that radiological early MPM or radiological T0MPMbe defined as MPM unaccompanied by pleural thickening or tumor visible on chest CT [4]. According to the IMIG/IASLC staging system, 8th edition, T0 indicates no evidence of primary tumor; however, the details are unclear [1, 5]. In clinical practice, radiological early MPM or radiological T0 MPM belongs to clinical T1 disease. We hypothesized that radiological early MPM has favorable outcomes and retrospectively examined the clinicopathological features of this disease.
The frequency of radiological early MPM is not well documented in the literature. A retrospective cohort study in Japan assessed the CT findings of 327 patients with MPM classified into four stages: no irregularity, mild irregularity, high irregularity, and mass formation. No irregularity indicated that no pleural thickening was found or that the thickening was ≤ 3 mm with no irregular surface. Of the 327 patients, only 7 (2.1%) were classified as no irregularity [15]. In contrast, another retrospective cohort study in Canada reviewed the CT findings of 92 patients with MPM; while all patients had pleural thickening, there was no case of radiological early MPM [16]. Based on these reports, there might be regional differences in frequency of radiological early MPM. We found a 5.4% frequency in a population of patients from Japan; however, unlike previous studies, our study included only patients with radiologically normal pleura who had curative-intent surgery planned at diagnosis.
Our results indicate that radiological early MPM was associated with early pathological stage. A previous retrospective cohort study at Memorial Sloan-Kettering Cancer Center (MSKCC) reported pathological findings of 232 patients with epithelioid MPM [17]:14patients (6%) were stage I, 54 (23%) were stage II, 130 (56%) were stage III, and 34 (15%) were stage IV (based on the 7th edition TNM staging system). The most common histologic subtype was solid (38%), followed by tubulopapillary (22%), trabecular (16%), pleomorphic (15%), and micropapillary (9%). Lymph node metastases were detected in 40% of patients, lymphatic invasion in 33%, and vascular invasion in 23%. The trabecular and tubulopapillary subtypes were associated with less lymphatic and vascular invasion. Taken together, early-stage (stage I–II) patients with trabecular and tubulopapillary subtypes had a significantly favorable median OS compared with pleomorphic and micropapillary subtypes (26.7 months and 33.7 months vs 14.7 months and 15.0 months, respectively) [17]. The histologic subtypes represented in our study were tubulopapillary (62.5%) or trabecular (37.5%), which have more favorable outcome; micropapillary, solid, and pleomorphic subtypes were not represented, in contrast to the MSKCC study. In addition, no patient in our study exhibited lymph node metastasis or vascular invasion, and lymphatic invasion was detected in only 1. Furthermore, most patients had low p53 and MIB-1 labeling indices. These results are consistent with the MSKCC study in that the trabecular and tubulopapillary subtypes were associated with less lymphatic and vascular invasion and earlier stage. Thus, radiological early MPM shows a tendency for earlier pathological stage.
In many solid malignancies, a smaller tumor predicts a more favorable postoperative prognosis [3]. Several studies have recently addressed the correlation between pleural thickness and clinical outcomes of MPM [3, 18]. de Perrot et al. reported that the sum of pleural thickness on 9 sectors of the chest wall, mediastinum, and diaphragm was an independent prognostic factor for both recurrence-free survival and OS [18]. We previously reported that pleural thickness after NAC is an independent prognostic factor and that lower post sum values (< 13 mm) reduced the risk of recurrence and death in MPM patients [3]. In the current study, radiological early MPM patients showed good long-term survival, with 2- and 3-year OS rates of 92.9% and 83.6%, respectively (median OS, 56.1 months). These findings are in line with previous studies. Furthermore, although comparisons between this study and the previous IASLC report should be carefully interpreted because of the different populations, the outcome of radiological early MPM in our study was more favorable than that of clinical T1 MPM in the IASLC report (median OS, 56.1 months vs 27.0 months; 2-year OS, 92.9% vs 58.0%).
The IASLC report described the problems of measuring pleural thickness [1]. First, the procedure of measurement may be subject to interobserver variability; absolute differences may be as great as ±2 mm even when a fixed outer measurement point is provided [19]. Second, previous pleurodesis is a potential confounder when measuring pleural thickness [1]. In this study, we defined radiological early MPM as lack of pleural thickening or visible tumor and did not have problems with interobserver variability or previous pleurodesis. Taken together, radiological early MPM could potentially be used to refine clinical TNM staging of MPM and may aid in determining the prognosis of multimodality treatment.
This study has several limitations. First, its single-center design may have introduced bias, so the results should be carefully interpreted. Second, Japanese centers operate earlier for patients with MPM compared with centers in the United States and Europe; for this reason, the frequency of radiological early MPM is probably lower in the USA and Europe than Japan. Future studies are needed to compare radiological early with the other clinical T stages.
Conclusion
In conclusion, our data suggest that radiological early MPM occurs in approximately 1 of every 20 patients (5.4%) treated with NAC and surgery planned at the time of diagnosis in an experienced center. Radiological early MPM was associated with early pathological stage and good long-term survival. Prospective nationwide studies are warranted to further evaluate radiological early MPM as a new T-component in the assessment of the prognosis of MPM.
Abbreviations
- MPM:
-
Malignant pleural mesothelioma
- IASLC:
-
International Association for the Study of Lung Cancer
- IMIG:
-
International Mesothelioma Interest Group
- CT:
-
Computed tomography
- PS:
-
Performance status
- NAC:
-
Neoadjuvant chemotherapy
- EPP:
-
Extrapleural pneumonectomy
- P/D:
-
Pleurectomy/decortication
- CE:
-
Contrast-enhanced
- FDG-PET:
-
Fluorodeoxy-d-glucose positron emission tomography
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- MSKCC:
-
Memorial Sloan–Kettering Cancer Center
References
A.K. Nowak, K. Chansky, D.C. Rice et al., The IASLC mesothelioma staging project: proposals for revisions of the T descriptors in the forthcoming eighth edition of the TNM classification for pleural mesothelioma. J Thorac Oncol 11, 2089–2099 (2016)
B.M. Burt, H.S. Lee, A.C. Raghuram et al., Preoperative prediction of unresectability in malignant pleural mesothelioma. J Thoracic Cardiovasc Surg 159, 2512–20 (2020)
M. Hashimoto, J. Takeuchi, T. Takuwa et al., Pleural thickness after neoadjuvant chemotherapy is a prognostic factor in malignant pleural mesothelioma. J Thorac Cardiovasc Surg 157, 404–13 (2019)
S. Hasegawa, N. Kondo, S. Matsumoto et al., Practical approaches to diagnose and treat for T0 malignant pleural mesothelioma: a proposal for diagnostic total parietal pleurectomy. Int J Clin Oncol 17, 33–9 (2012)
V.W. Rusch, K. Chansky, H.L. Kindler et al., The IASLC mesothelioma staging project: proposals for the M descriptors and for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for mesothelioma. J Thorac Oncol 11, 2112–9 (2016)
M.J. Byrne, A.K. Nowak, Modified RECIST criteria for assessment of response in malignant pleural mesothelioma. Ann Oncol 15, 257–60 (2004)
S. Hasegawa, N. Kondo, S. Matsumoto et al., Surgical risk and survival associated with less invasive surgery for malignant pleural mesothelioma. Semin Thorac Cardiovasc Surg 31, 301–9 (2019)
A. Nakamura, T. Takuwa, M. Hashimoto et al., Clinical outcomes with recurrence after pleurectomy/decortication for malignant pleural mesothelioma. Ann Thorac Surg 109, 1537–43 (2020)
E.H. Baldini, W.G. Richards, R.R. Gill et al., Updated patterns of failure after multimodality therapy for malignant pleural mesothelioma. J Thorac Cardiovasc Surg 149, 1374–81 (2015)
R.M. Flores, H.I. Pass, V.E. Seshan, Extrapleural pneumonectomy versus pleurectomy/decortication in the surgical management of malignant pleural mesothelioma: results in 663 patients. J Thorac Cardiovasc Surg 135, 620–6 (2008)
J.S. Friedberg, C.B. Simone 2nd, M.J. Culligan et al., Extended pleurectomy-decortication-based treatment for advanced stage epithelial mesothelioma yielding a median survival of nearly three years. Ann Thorac Surg 103, 912–9 (2017)
M. de Perrot, R. Feld, B.C. Cho et al., Trimodality therapy with induction chemotherapy followed by extrapleural pneumonectomy and adjuvant high-dose hemithoracic radiation for malignant pleural mesothelioma. J Clin Oncol 27, 1413–8 (2009)
C. Boutin, F. Rey, J. Gouvernet et al., Thoracoscopy in pleural malignant mesothelioma: a prospective study of 188 consecutive patients. Part 2: prognosis and staging. Cancer 72, 394–404 (1993)
J. Scurry, M.A. Duggan, Malignant mesothelioma eight years after a diagnosis of atypical mesothelial hyperplasia. J Clin Pathol 52, 535–7 (1999)
K. Kato, K. Gemba, N. Fujimoto et al., Fatal pleural mesothelioma in Japan (2003–2008): evaluation of computed tomography findings. Jpn J Radiol 34, 432–8 (2016)
J.M. Seely, E.T. Nguyen, A.M. Churg et al., Malignant pleural mesothelioma: computed tomography and correlation with histology. Eur J Radiol 70, 485–91 (2009)
K. Kadota, K. Suzuki, C.S. Sima et al., Pleomorphic epithelioid diffuse malignant pleural mesothelioma: a clinicopathological review and conceptual proposal to reclassify as biphasic or sarcomatoid mesothelioma. J Thorac Oncol 6, 896–904 (2011)
M. de Perrot, Z. Dong, P. Bradbury et al., Impact of tumour thickness on survival after radical radiation and surgery in malignant pleural mesothelioma. Eur Respir J 49, 1601428 (2017)
S.G. Armato 3rd, G.R. Oxnard, H. MacMahon et al., Measurement of mesothelioma on thoracic CT scans: a comparison of manual and computer-assisted techniques. Med Phys 31, 1105–15 (2004)
Acknowledgement
The authors thank Drs. Teruhisa Takuwa, Seiji Matsumoto, Ayumi Kuroda, and Toru Nakamichi for their significant contribution to this study. The authors would also like to thank Enago (www.enago.jp) for the English language review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No author has any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Nakamura, A., Hashimoto, M., Kodama, H. et al. Clinicopathological features of radiological early malignant pleural mesothelioma with no apparent tumor or pleural thickening. Int J Clin Oncol 26, 95–103 (2021). https://doi.org/10.1007/s10147-020-01780-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-020-01780-0