Abstract
Purpose
The purpose of this study was to clarify the characteristic findings of mesothelioma at the time of diagnosis, and determine precautions and guidelines for diagnosing mesothelioma early in imaging studies.
Materials and methods
Overall, 327 patients with pleural mesothelioma were selected from 6030 patients who died of mesothelioma between 2003 and 2008 in Japan. Their imaging findings were examined retrospectively.
Results
Plaques were found in 35 % of computed tomography (CT) scans. Asbestosis, diffuse pleural thickening, and rounded atelectasis were found in only seven (2 %), five (2 %), and two cases (1 %), respectively. Pleural thickening findings on CT scans were classified into four stages: no irregularity, mild irregularity, high irregularity, and mass formation. Overall, 18 % of cases did not show a clear irregularity. Localized thickening was observed in the mediastinal (77 %) and basal (76 %) pleura and in the interlobar fissure (49 %). Eight percent of cases did not have any thickening in these three areas.
Conclusions
Upon examination of the CT scans at diagnosis, 18 % of mesothelioma cases did not show a clear irregularity. When diagnosing pleural effusion of unknown etiology, it is necessary to consider the possibility of mesothelioma even when no plaque and pleural irregularity are observed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mesothelioma is a rare, asbestos-related disease [1, 2] with a poor prognosis [3]. Asbestos was used extensively in Japan for construction and industrial products owing to its useful characteristics; however, since the discovery of its carcinogenic potential, alternative products have been introduced and the manufacture and use of asbestos is now prohibited. It takes 30–40 years of incubation to develop mesothelioma or lung cancer originating from asbestos [4–7], and the number of patients with mesothelioma has been increasing over recent years; this has become a problem in many countries. The United States prohibited asbestos usage earlier compared to other countries, and the number of patients developing asbestos-related problems reached a peak there in 2004, with the number now decreasing. In Europe, the peak is expected be around 2015–2020, and in Japan, where the prohibition occurred later, the peak will be around 2025, which implies that the number of patients will keep increasing until this time [6]. In accordance with Japanese law, crocidolite and amosite usage was stopped in 1995; chrysotile usage was stopped in 2004. The country’s recent discontinuation is evidence of the delay in asbestos regulations in our country, and the damage caused by these delays is apparent. A newspaper article published in June 2005 reported that five residents who lived near the now-closed asbestos cement pipe plant in Amagasaki, Japan, developed pleural mesothelioma [8]. Since this report, asbestos-related problems have raised significant social concern. We performed a nationwide retrospective survey to evaluate all cases of mesothelioma in Japan. As a result, we analyzed more than 6000 cases of mesothelioma that were registered in the Vital Statistics yearly survey performed by the Japanese Ministry of Health, Labour, and Welfare between 2003 and 2008. To the best of our knowledge, this is the largest study of Japanese cases of mesothelioma. Our study used images, mainly computed tomography (CT) and plain radiography, from deceased patients with pleural mesothelioma that were acquired with family and institutional permissions. In a review of the literature, we found no other reports examining the number of cases with mesothelioma and their images. The clinical features of the cases with mesothelioma in this study have already been reported [9]. The purpose of the current study was to clarify the characteristics of the imaging findings obtained at the time of the diagnosis of pleural mesothelioma, and determine precautions and guidelines for diagnosing mesothelioma early in imaging studies.
Subjects and methods
Study approval
This study was conducted according to the Ethical Guidelines for Epidemiological Research by the Japanese Ministry of Education, Culture, Sports, Science and Technology, and the Ministry of Health, Labor, and Welfare. The study was approved by the relevant institutional ethical review boards.
Patient selection and imaging studies
The methods of this retrospective survey have been previously described [9]. In brief, we requested and received authorization to view the death records in the Vital Statistics register in Japan, and we extracted all cases of death due to malignant mesothelioma between 2003 and 2008; in total, 6030 deaths were found to be due to mesothelioma. We contacted the closest living relatives of each patient to obtain consent for our study by postal mail. As a result, informed consent was obtained by mail from the relatives of 2069 patients (34.3 %). Subsequently, we contacted the patients’ respective medical institutions to obtain the following information by mail: medical records, radiographs, and/or CT images. Different institutions had different types of CT images. We accepted both digital and film CT scans for review to examine as many cases as possible. We also reviewed the medical records and radiological images to confirm the clinical and pathological diagnoses of malignant mesothelioma.
Image interpretation
All patients underwent CT and plain radiography at the time of diagnosis of pleural mesothelioma. CT images were obtained using various CT scanners and a range of scan protocols at each institution. CT scans with a 5-mm thickness were the most common, but other slice thicknesses were found, ranging from 1 to 10 mm. Plain radiographs and CT images were retrospectively reviewed with consensus by three co-researchers: one chest radiologist and two pulmonologists. The chest radiologist (K.K.) had 24 years of experience and the two respiratory physicians (T.K. and K.G.) had 28 and 20 years of experience, respectively. Additionally, all three co-researchers had worked in a hospital that specialized in occupational respiratory disease for more than 10 years, and they were members of the official pneumoconiosis examination committee for laborers in the Okayama prefecture.
Evaluating items
First, pleural plaque and its calcification were evaluated on CT images. Pleural plaques were also assessed on plain chest radiographs of the same cases. Additionally, the images were checked for pleural effusion, lung asbestosis, diffuse pleural thickening, and rounded atelectasis.
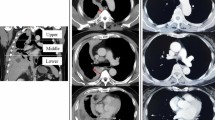
Next, the pleural findings from the CT images were classified into four stages: no irregularity, mild irregularity, high irregularity, and mass formation. The four stages are shown in Fig. 1. No irregularity indicated that there was no pleural thickening found or that the thickening was ≤3 mm with no irregular surface. Mild irregularity indicated a regular surface with a thickening >3 mm but ≤5 mm; this stage also included cases of slight asperity with no clear nodular irregularity. Clinically, this was non-specific thickening due to either a benign or a malignant lesion. Mild irregular findings on CT may indicate benign pleural lesions such as pleurisy. High irregularity indicated a thickening >5 mm. Clear nodular thickening was required for this classification, and clinically, a malignancy was strongly suspected. Mass formation indicated that the irregularity was even more severe and that a partial mass with a diameter of >1 cm was clearly formed. We did not include massive irregularity in mass formation; we included only the CT findings that identified a clearly formed mass. We examined the entire pleura very carefully, because the grading of pleural irregularity changes even with a localized pleural thickening. Both multiple and isolated masses were defined as a mass formation; clinically, this indicated a malignant lesion.
a No irregularity: pleural effusion but no irregularity of the pleura. b Mild irregularity: a slight irregularity of the pleura; however, the irregularity does not indicate a severe irregularity, such as a malignancy. c High irregularity: severe irregular thickening of the pleura; a malignant lesion is suspected. d Mass formation: severe irregular thickening of the pleura, with clear mass formation; this finding suggests a malignant lesion
When we considered the tumor (T) part of the tumor node metastasis classification of malignant tumors staging system, used by the International Mesothelioma Interest Group, for pleural mesothelioma, it was difficult to distinguish between T1 and T2 by using CT alone; therefore, T1 and T2 were considered a single group. Thus, our examination was based on three groups: T1–2, T3, and T4.
Following the staging classification, localization of the pleural lesions was examined; we evaluated for signs of mediastinal pleural lesions, which are characteristic of mesothelioma [10]. The interlobar pleura, where pleural lesions are more easily identified, and the basal lung, which frequently has lesions, were also examined for the presence of abnormalities (Fig. 2).
a Mediastinal pleural irregularity: a thickened pleura with a slight irregularity in a broad area of the mediastinal pleura. The thickness is not severe in this classification, but if broad thickening is found in this area, a high potential for mesothelioma can be suspected. b Pleura irregularity in the base of the lungs: Tuberous irregular pleural thickening at the base of the left lung. A malignant pleural lesion can be suspected. c Irregular interlobar pleura: Tuberous thickening begins in the right interlobar pleura. The interlobar pleural layer is surrounded by lung parenchyma; therefore, the pleura can be easily evaluated on the images. High-resolution computed tomography (CT) can provide clearer images, but evaluation of the interlobar pleural irregularities is also possible using average CT scans, if carefully examined
Statistical analysis
Statistical analysis was performed using the chi-squared test to analyze the correlation of each CT finding with the pathological diagnoses that were divided into the epithelial type and non-epithelial type. We considered p < 0.05 significant. Statistical calculations were performed using the SPSS statistical package, version 22.0 (IBM Corp., Armonk, NY, USA).
Results
Data from 1111 patients were obtained. We confirmed the clinical diagnosis of mesothelioma in 929 patients, including 753 men (81.1 %) and 176 women (18.9 %). The median age at diagnosis was 67.0 years (range, 16–94 years). The origin of mesothelioma was the pleura in 794 patients (85.5 %), peritoneum in 123 (13.2 %), pericardium in seven (0.8 %), and testicular tunica vaginalis in five (0.5 %). Of those 794 patients, 327 (273 men, 54 women; mean age, 68 years) had chest CT images obtained at the time of diagnosis; we examined those images (Fig. 3).
The histological subtypes of mesothelioma were determined in 327 cases based on the World Health Organization’s criteria [11]: 176 (54 %) with epithelioid mesothelioma, 75 (23 %) with sarcomatoid mesothelioma, 59 (18 %) with biphasic mesothelioma, and 17 (5 %) with other types.
Pleural plaque was found on chest CT images of 114/327 patients (35 %), and 56 of those (49 %) had calcification. Plain chest radiographs showed that only 36 (11 %) of 327 patients had plaque.
Pleural effusion was found in 304 patients (93 %), but lung asbestosis, diffuse pleural thickening, and rounded atelectasis were only found in seven (2 %), five (2 %), and two patients (1 %), respectively.
Table 1 shows the classification of pleural findings into the four stages. Table 1 compares these four stages with the T classification system. Among the 327 cases of pleural mesothelioma, seven were classified with no irregularity (2 %); 53 with a mild irregularity that included a possible benign lesion (16 %); 140 with a high irregularity that included seemingly malignant lesions (43 %); and 127 with a mass formation that indicated a malignant lesion. Thus, 82 % of cases showed severe pleural irregularities on CT images that were indicative of a potential malignancy, and 18 % of cases did not have irregularities that were indicative of malignant lesions. All the cases with no irregularity were classified as T1–2; 49 cases (92 %) with a mild irregularity were also classified as T1–2. Cases with a mild pleural irregularity progressed slowly. However, cases with a high irregularity and mass formation had a high malignant potential; 78 % of cases with a high irregularity and 84 % of cases with a mass formation were classified as T3–4.
Lesion localization was as follows: the mediastinal pleura in 251 patients (77 %), base of the lungs in 250 (76 %), and interlobular pleura in 159 (49 %) (Table 2). Only 27 cases (8 %) had no lesions in the mediastinal and interlobular pleurae.
Statistically, there was no significant correlation between the CT findings and pathological subtypes (Table 2).
Discussion
Eighty percent of patients with pleural malignant mesothelioma are men [6, 12]. In the present study, 273 patients (83 %) were men. The high percentage of men in our study is similar to the finding of a previous report [6]. The age range of our study was extremely wide, ranging from 16–94 years at diagnosis. This wide age range indicates that cases of mesothelioma caused by environmental exposure were included in this study. The average latency period (i.e., the time interval between the first asbestos exposure and death) for mesothelioma development is 30–40 years [13]. Bianchi et al. [7] reported that the latency period ranges from 14–75 years (mean 48.8 years, median 51.0 years). This suggests that if the onset is diagnosed at 16 years old, the patient must have been exposed to the attributing environmental conditions since birth. This could be the case, for example, if the patient was born in a neighborhood with an asbestos factory. Due to this environmental exposure, juvenile mesothelioma would occur; these cases were also included in our study.
The image findings, mainly CT results, of 327 patients with pleural mesothelioma were selected from 6030 patients who died of mesothelioma between 2003 and 2008. Although there are a number of previous studies that have described the findings of pleural mesothelioma on CT scans [10, 13–16], no reports have evaluated the CT scans of as many as 327 patients by using uniform criteria. Therefore, the results of our study are of interest, as we present the first broad report on the results of mesothelioma on CT scans obtained at the time of the initial diagnosis.
Pleural plaque was observed in 35 % of the CT scans but in only 11 % of plain chest radiographs. Previous studies that used CT have shown pleural plaque in 12.1–78 % of cases [10, 14–16]. Additionally, only one-third of cases that had plaque on CT scans also had plaque on radiographs; this result is similar to that of a previous study [17]. Only 2 % of cases had pulmonary fibrosis equivalent to asbestosis in the current study. Asbestosis results from high-dose asbestos exposure. This examination was a national investigation that included patients who did not work with asbestos and those who worked in asbestos-related industries. Plaque was observed in only 35 % of cases. Therefore, we believe that the ratio of persons with a high concentration of asbestos exposure among the target cases was low.
Regarding pleural irregularities, 18 % of cases had either no irregularity (no clear malignancy on the image) or a mild irregularity (these cases were mainly T1–2). Although previous reports have described the pleural effusion occurrence rate [5, 18], to our knowledge, no reports to date have described the difficulties in diagnosing malignancy based on CT images among the more than 300 known cases. To make a successful early diagnosis, it is necessary to be aware that there could be cases with no irregularities among T1–2 cases. It is necessary to pay extra attention to the possibility of a mild pleural irregularity. According to the International Mesothelioma Interest Group staging system, the median overall survival (OS) rates for patients with stages I and II (T1–2 and N0), stage III, and stage IV tumors were 11.2 months (9.4–13.0 months), 7.9 months (7.1–8.7 months), and 3.9 months (3.0–4.6 months) (95 % confidence interval), respectively. The OS was significantly shorter for stage III patients than for stages I and II patients (p < 0.001); the OS was significantly shorter for stage IV patients than for stage III patients (p < 0.001) [8].
Regarding lesion localization, the mediastinal pleura was the most common site (77 % of cases). Abnormal findings were also observed in the basal lung and interlobular pleurae. Overall, lesions in these three sites encompassed 82 % of all cases. Mediastinal pleural lesions can be considered to have a relatively high specificity as malignant pleural lesions, and the basal lung and interlobar pleura are surrounded by lung parenchyma, which makes the evaluation of microlesions easier. Therefore, focusing on these three locations on CT images during diagnosis could improve the sensitivity and potential for diagnosing mesothelioma earlier.
There was no significant correlation between each CT finding and the pathological subtypes. Although the epithelial type of mesothelioma is associated with a better prognosis than the sarcomatous and biphasic subtypes [19], less irregularity subtype groups are not significantly correlated with the epithelial subtype of mesothelioma.
There are a number of limitations in our study. First, our study was retrospective, and the cases were collected from many institutions. Therefore, a variety of imaging devices and methods for both CT and plain radiography were used. However, because we evaluated CT images obtained with various scanners, our image evaluation process was simple; the principal objective was to identify irregular findings that the mesothelioma expert believed to be malignant. In Japan, there is a wide range of CT imaging techniques, but in most cases, an evaluable image was obtained. However, an advantage of this multi-center study was the large number of cases we were able to collect and examine. Secondly, the ability to diagnose mesothelioma differed among the hospitals. As the timing of the mesothelioma diagnosis varied according to the diagnostic ability of each institution, this may have introduced bias into our study; the progression of the mesothelioma lesion could be associated with a delay in diagnosis. Therefore, we speculate that the number of cases with mesothelioma with less severe irregularity findings would increase if each institution had made the diagnosis at an appropriate time. Additionally, in our study, we did not evaluate interobserver variation, thus this was a limitation too. However, all observers were adequately experienced with asbestos-related diseases, and thus good evaluation for radiologic images was performed.
In conclusion, 18 % of cases with mesothelioma in our study did not display a clear irregularity on CT images, and these cases were classified as low T-stage at the time of diagnosis. Therefore, when diagnosing pleural effusion of unknown etiology, the possibility of pleural mesothelioma must be considered even in cases with no identifiable plaque. When the findings do not indicate a malignant lesion, we can still suspect potential mesothelioma when slight changes are observed in the mediastinal or interlobar pleura. Images of early-stage mesothelioma need to be interpreted accurately.
References
Wagner JC, Sleggs CA, Marchand P. Diffuse pleural mesothelioma and asbestos exposure in the North Western Cape Province. Br J Ind Med. 1960;17:260–71.
Prazakova S, Thomas PS, Sandrini A, Yates DH. Asbestos and the lung in the 21st century: an update. Clin Respir J. 2014;8:1–10.
Muers MF, Stephens RJ, Fisher P, Darlison L, Higgs CM, Lowry E, et al. Active symptom control with or without chemotherapy in the treatment of patients with malignant pleural mesothelioma (MS01): a multicentre randomised trial. Lancet. 2008;371:1685–94.
Rusch VW. A proposed new international TNM staging system for malignant pleural mesothelioma from the International Mesothelioma Interest Group. Lung Cancer. 1996;14:1–12.
Metintas M, Ucgun I, Elbek O, Erginel S, Metintas S, Kolsuz M, et al. Computed tomography features in malignant pleural mesothelioma and other commonly seen pleural diseases. Eur J Radiol. 2002;41:1–9.
Robinson BW, Lake RA. Advances in malignant mesothelioma. New Engl J Med. 2005;353:1591–603.
Bianchi C, Brollo A, Ramani L, Bianchi T, Giarelli L. Asbestos exposure in malignant mesothelioma of the pleura: a survey of 557 cases. Ind Health. 2001;39:161–7.
Oshima H. 51 death asbestos-related illness in ten years. Mainichi Newspapers. 2005;1.
Gemba K, Fujimoto N, Aoe K, Kato K, Takeshima Y, Inai K, et al. Treatment and survival analyses of malignant mesothelioma in Japan. Acta Oncol. 2013;52:803–8.
Leung AN, Muller NL, Miller RR. CT in differential diagnosis of diffuse pleural disease. AJR Am J Roentgenol. 1990;154:487–92.
Churg A, Cagle PT, Roggli VL. Separation of benign and malignant mesothelial proliferations. In: AFIP Atlas of tumor pathology. Series 4. Tumors of the serosal membrane. Silver Springs: ARP Press; 2006. p. 83–101.
Roe OD, Stella GM. Malignant pleural mesothelioma: history, controversy and future of a manmade epidemic. Eur Respir Rev. 2015;24:115–31.
Erzen C, Eryilmaz M, Kalyoncu F, Bilir N, Sahin A, Baris YI. CT findings in malignant pleural mesothelioma related to nonoccupational exposure to asbestos and fibrous zeolite (erionite). J Comput Assist Tomogr. 1991;15:256–60.
Kawashima A, Libshitz HI. Malignant pleural mesothelioma: CT manifestations in 50 cases. AJR Am J Roentgenol. 1990;155:965–9.
Senyiğit A, Bayram H, Babayiğit C, Topcu F, Nazaroglu H, Bilici A, et al. Malignant pleural mesothelioma caused by environmental exposure to asbestos in the Southeast of Turkey: CT findings in 117 patients. Respiration. 2000;67:615–22.
Seely JM, Nguyen ET, Churg AM, Müller NL. Malignant pleural mesothelioma: computed tomography and correlation with histology. Eur J Radiol. 2009;70:485–91.
Staples CA. Computed tomography in the evaluation of benign asbestos-related disorders. Radiol Clin North Am. 1992;30:1191–207.
Okten F, Koksal D, Onal M, Ozcan A, Simsek C, Erturk H. Computed tomography findings in 66 patients with malignant pleural mesothelioma due to environmental exposure to asbestos. Clin Imaging. 2006;30:177–80.
Meyerhoff RR, Yang CF, Speicher PJ, Gulack BC, Hartwig MG, D’Amico TA, et al. Impact of mesothelioma histologic subtype on outcomes in the surveillance, epidemiology, and end results database. J Surg Res. 2015;196:23–32.
Acknowledgements
This research was funded primarily by grants from the research foundation of the Ministry of Health, Labor, and Welfare of Japan (200500129A, 200635021A, 200733015A, 200733015B, 200836010A, 200938007A, and 201032004B) and by the Industrial Disease Clinical Research Grants from the Ministry of Health, Labor, and Welfare of Japan (1403101). This study is one of the research and development and dissemination projects related to the 13 fields of occupational injuries and illnesses of the Japan Health, Labor, and Welfare Organization. The sponsors had no involvement in the study design, collection, and analysis and interpretation of the data; writing of the manuscript; or decision to submit the manuscript for publication. We thank the living relatives of the patients with mesothelioma who provided consent; medical institutions that provided the medical information on the patients with mesothelioma; and Mrs. Rie Sugimoto, Mrs. Keiko Fujimura, Miss Naomi Ogura, and Miss Shiori Sato for collecting data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Funding
This research was funded primarily by grants from the research foundation of the Ministry of Health, Labor, and Welfare of Japan (200500129A, 200635021A, 200733015A, 200733015B, 200836010A, 200938007A, and 201032004B) and by Industrial Disease Clinical Research Grants from the Ministry of Health, Labor, and Welfare of Japan (1403101).
Ethical statement
This study was conducted according to the Ethical Guidelines for Epidemiological Research by the Japanese Ministry of Education, Culture, Sports, Science and Technology, and the Ministry of Health, Labor, and Welfare. This study was approved by the Japan Health, Labor, and Welfare Organization and the institutional review boards of each institution. Patient confidentiality was strictly maintained. Informed consent was obtained from the closest living relatives of each patient.
About this article
Cite this article
Kato, K., Gemba, K., Fujimoto, N. et al. Fatal pleural mesothelioma in Japan (2003–2008): evaluation of computed tomography findings. Jpn J Radiol 34, 432–438 (2016). https://doi.org/10.1007/s11604-016-0539-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-016-0539-1