Abstract
Objective
To evaluate the efficacy and safety of the addition of olanzapine to ondansetron and dexamethasone for chemotherapy-induced nausea vomiting (CINV) prevention in patients receiving highly emetogenic chemotherapy (HEC).
Methods
In this randomized, double-blind, placebo-controlled, crossover study, we randomly assigned chemotherapy-naïve patients receiving HEC to receive olanzapine or placebo in addition to ondansetron and dexamethasone. All subjects were crossed over to another treatment arm on second-cycle chemotherapy. The primary endpoint was complete response (CR) rate defined as no vomiting and no use of rescue drugs.
Results
At the first cycle, there were significantly more patients with CR in the olanzapine group than in the placebo group in overall phase (68.7% vs. 25.0%, p < 0.001), acute phase (0–24 h) (75.0% vs. 31.2%, p < 0.001) and delayed phase (24–120 h) (68.7% vs. 43.7%, p = 0.038). After crossover, there were significantly more patients with CR in the olanzapine group than in the placebo group in overall phase (67.2% vs. 25.0%, p < 0.001), acute phase (71.9% vs. 32.8%, p < 0.001) and delayed phase (67.2% vs. 37.5%, p < 0.001). In crossover analysis, the olanzapine group had significantly lower mean nausea (1.28 vs. 3.05, p < 0.001) and fatigue (3.5 vs. 4.58, p < 0.001) scores but higher mean appetite (2.5 vs. 1.55, p = 0.003) and sleepiness (3.26 vs. 2.2, p < 0.001) scores. There were no grade 3 and 4 anti-emetic-drug-related toxicities. Mean QT interval changes did not different between two groups (−4.30 vs. −1.86, p = 0.69).
Conclusion
The addition of olanzapine to ondansetron and dexamethasone significantly improved CINV prevention and was safe in patients receiving HEC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy-induced nausea and vomiting (CINV) is a common side effect that can result in suboptimal cancer treatment and affect the patient’s quality of life [1,2,3]. However, prophylactic anti-emetic drugs have been significantly improved over the years and can now reduce CINV from 80 to 35% in patients receiving highly and moderately emetogenic chemotherapy [4].
Olanzapine is now a standard anti-emetic agent for CINV prevention. It is an antipsychotic drug that centrally blocks multiple neurotransmitters involved in CINV [5, 6]. Several studies showed that when olanzapine was used with dexamethasone and 5-HT3 antagonist, it was effective in preventing CINV [7,8,9,10,11]. Among these trials, two-phase 3 trials demonstrated the efficacy of olanzapine when used with palonosetron (a 5-HT3 antagonist) and dexamethasone with or without aprepitant (an NK1 antagonist) [12, 13]. As a result, these anti-emetic regimens have been recommended for CINV prevention in patients receiving highly emetogenic chemotherapy (HEC) [14, 15]. However, in resource-limited setting, this regimen is unattainable due to the cost of palonosetron and NK-1 antagonists. An alternative regimen is much needed to prevent CINV in patients on HEC.
Ondansetron is a first-generation 5-HT3 antagonist used to prevent CINV. Since there are lots of generic ondansetron available in the market, therefore it is much more accessible than palonosetron. However, as compared to palonosetron, it has a shorter half-life and can cause QTc interval prolongation, an overlapping side effect with olanzapine [16, 17].
Thus, this prospective, crossover, randomized study assessed the efficacy and safety of adding olanzapine to ondansetron and dexamethasone to prevent CINV in patients receiving HEC.
Method
Study design and patients
This double-blind, placebo-controlled, crossover study assessed the efficacy and safety of olanzapine versus matching placebo adjunct to ondansetron and dexamethasone as an anti-emetic regimen to prevent CINV in patients receiving HEC at the King Chulalongkorn Memorial Hospital.
Patients aged 18 years or older with cancer who had not received chemotherapy were eligible if they were scheduled to receive adriamycin–cyclophosphamide (adriamycin 60 mg/m2 and cyclophosphamide 600 mg/m2, AC) or high-dose cisplatin (> 70 mg/m2) regimens. The patients with at least creatine clearance of 60 mL/min, aspartate and alanine aminotransferase levels no more than three times the upper limit of the normal range, and had an absolute neutrophil count of at least 1500 per mm3 were enrolled into the study. Patients with nausea and vomiting within 24 h, upper gastrointestinal malignancy causing nausea and vomiting, brain metastases or any neurological disease, psychosis, chronic alcoholism, allergy to olanzapine, QTc prolongation (corrected QT was calculated with Bazett’s formula; prolongation was defined as greater than 450 ms), significant heart disease, and uncontrolled diabetes mellitus were excluded from the study. The study also excluded patients who had chest or abdominal irradiation, on antipsychotic drugs, and/or on quinolone antibiotics.
Randomization, masking and treatment regimen
Patients were enrolled via the permuted block randomization procedure by computerized method. The stratification factor was chemotherapy regimen, AC or high-dose cisplatin. Both investigators and patients were blinded to the treatment regimens. The patients were randomly assigned in 1:1 ratio to receive olanzapine or matching placebo. Upon the second cycle of chemotherapy, those who initially received olanzapine now received the matching placebo while the other group who were on matching placebo now received olanzapine. The patients received olanzapine 10 mg tablet or a matching placebo per oral, ondansetron 8 mg intravenously and dexamethasone 20 mg intravenously for 30 min before starting chemotherapy. On days 2–4 of chemotherapy, the patients received olanzapine 10 mg tablet or a matching placebo once daily with dexamethasone 4 mg tablet twice daily.
Study endpoints
The primary endpoints were the first-cycle complete response (CR) rates in acute, delayed and overall phases of treatment. CR was defined as no emesis and no use of rescue drug.
The secondary endpoints were the crossover CR rate, no nausea rate, patient’s satisfaction, reported adverse events and QTc interval changes. CINV severity was graded by CTCAE version 4.0, and the patient’s satisfaction was evaluated by visual analog scale (VAS).
Assessment procedure
At 0–120 h of chemotherapy, the patients were asked to daily record episodes of vomiting and use of rescue therapy in a diary. Nausea was assessed by VAS, scale ranging from 0 to 10. No nausea was defined as nausea scale 0. The anti-emetic-drug-related adverse events were assessed by investigators. However, fatigue, loss of appetite and sleepiness were assessed by VAS. There was a study nurse that reminded the patients daily to fill out the records on days 2–5. ECG was performed before and 2 h after taking the premedications.
Trial oversight
The protocol for this trial was reviewed and approved by the institutional review board of the Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand. The trial was conducted in accordance with the provisions of the Declaration of Helsinki. All patients provided written informed consent before enrollment. The first and last authors drafted the manuscript. All authors contributed to subsequent drafts and approved the final version of the manuscript.
Statistical analysis
Based on the improvement of overall CR from 13 to 42% in patients receiving aprepitant versus placebo in addition to dexamethasone and ondansetron [18], and the equivalent efficacy of aprepitant and olanzapine in CINV prevention [19], the study required 58 patients to obtain a 0.80 power at one-sided type I error level of 0.05 to demonstrate the better CR of olanzapine versus placebo in CINV prevention. The total number of enrolled patients was increased to 64 patients based on a 10% drop out rate.
The percentage of intention-to-treat population with CR for the acute, delayed and overall phases was calculated. The Chi square test was performed to compare the CR rates between the treatment arms for the first cycle. The McNemar’s test was performed to compare the CR rates between treatment arms for the second cycle.
We used ANOVA for crossover method to determine changes of mean VAS of nausea, sleepiness, loss of appetite and the patient’s appreciation across both cycles.
All adverse events were reported as percentage according to the CTCAE version 4.0. The paired t test and McNemar’s test were used to compare QTc prolongation before and after medications in the first and second cycles.
All statistical analyses were run by using IBM SPSS statistics, version 22.
Results
Patients’ characteristics
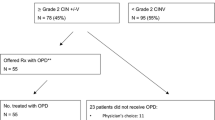
From May to August 2017, 64 patients were eligible for the study. 32 patients were randomly assigned to either the olanzapine or placebo group. After first cycle, there were one and three patients in olanzapine and placebo arms, respectively, did not receive second-cycle chemotherapy due to intolerable nausea and vomiting. The study flow is shown in Fig. 1.
There were no significant differences in baseline characteristics between the two groups. About two third of the patients received AC. The mean dose of cisplatin was 72.96 mg/m2. Among patients receiving cisplatin, only one patient received cisplatin at dose less than 70 mg/m2 (69.19 mg/m2) in placebo group. The patients’ baseline characteristics are shown in Table 1.
Efficacy analysis
At the first cycle, there were significantly more patients with CR in the olanzapine group than in the placebo group in overall phase (68.7% vs. 25.0%, p < 0.001), acute phase (0–24 h) (75.0% vs. 31.2%, p < 0.001) and delayed phase (24–120 h) (68.7% vs. 43.7%, p = 0.038). At the second cycle, four patients did not receive the second cycle but were included in the analysis as event occurrence (i.e., no CR) in the second cycle. After crossover, there were significantly more patients with CR in the olanzapine group than in the placebo group in overall phase (67.2% vs. 25.0%, p < 0.001), acute phase (71.9% vs. 32.8%, p < 0.001) and delayed phase (67.2% vs. 37.5%, p < 0.001). All CR rates are shown in Table 2. The number of vomiting or retching during the olanzapine cycle was lower than during the placebo cycle in all treatment phases. Most of the emetic episodes occurred on day 1 through day 3 as shown in Fig. 2.
At the first cycle, no nausea rates in the olanzapine group were significantly lower than the placebo group for all treatment phases (overall; 40.6% vs. 12.5%, p = 0.011, 0–24 h; 53.1% vs. 25%, p = 0.021 and 24–120 h; 40.6% vs. 12.5%, p = 0.011). At the second cycle, the four patients who did not receive the second cycle were kept in the analysis and were counted as event occurrence (i.e., nausea). In the crossover analysis, no nausea rates in olanzapine group were significantly higher than in the placebo group for all treatment phases (overall; 40.6% vs. 10.9%, p < 0.001, 24 h; 48.4% vs. 20.3%, p = 0.001, 24–120 h; 42.2% vs. 14.1%, p = 0.001). All no nausea rates are shown in Table 3.
In the crossover analysis using VAS, the patients in the olanzapine group had significantly lower mean VAS in nausea (1.28 vs. 3.05, p < 0.001) and fatigue (3.5 vs. 4.58, p < 0.001) but higher mean VAS in appetite (2.5 vs. 1.55, p = 0.003) and sleepiness (3.26 vs. 2.2, p < 0.001). The mean VAS of nausea was higher in the placebo group than in the olanzapine group for all treatment phases and were much greater on days 1 and 2 (Fig. 3a). On the other hand, the mean VAS of appetite and sleepiness in the olanzapine group were higher on day 1 through day 5. The VAS results are shown in Fig. 3.
Safety
There were no serious anti-emetic-drug-related adverse event in this study. There were no clinically significant hyperglycemia (defined as having a score greater than grade 2) or undesirable sleepiness that disrupted the daily activity (defined as having a score greater than grade 1) in the olanzapine group.
There were 12 patients that had QTc prolongation after chemotherapy including seven and five patients in the olanzapine and placebo groups, respectively (p = 0.28). Two patients had QTc prolongation in both cycles. Means QTc interval change were not different between the two groups: −4.30 ms in the olanzapine group vs. −1.86 ms in the placebo group (p = 0.69). However, there were more QTc prolongation rates in the patients on cisplatin than in patients on AC. Among patients receiving cisplatin, QTc prolongation occurred more frequently in the olanzapine group compared to those in the placebo group (23% vs. 12%).
Patient satisfaction
Among 60 patients receiving crossover anti-emetic regimen, 52 patients chose to continue olanzapine containing anti-emetic regimen (p < 0.001).
Discussion
This randomized, double-blind, crossover trial demonstrated the benefit of adding olanzapine to dexamethasone and ondansetron to prevent CINV compared to the placebo. We observed clinical improvement in CR and no nausea rates with no significant undesired adverse event in patients receiving olanzapine.
Similar to previous studies, we demonstrated that the addition of olanzapine improved CINV prevention in patients receiving HEC. In previous phase III trials, the addition of olanzapine led to better CINV prevention when used with 5-HT3 antagonist, dexamethasone and NK-1 inhibitor [12, 13, 19, 20]. The benefit of adding olanzapine is quite consistent, even though there were some variations in the study endpoint, olanzapine dosage, and chemotherapy regimens among these trials.
The addition of olanzapine to ondansetron and dexamethasone improved CINV prevention in overall, acute and delayed phases in patients receiving HEC. These findings were consistent with previous studies regarding the benefit of adding olanzapine to anti-emetic regimens for both acute and delayed phases in CINV prevention [13, 21]. However, some previous studies did not demonstrate any improvement of CINV prevention during the acute phase [20]. This inconsistent benefit during the acute phase may be due to several factors such as chemotherapy regimens, different populations, different anti-emetic regimens and different 5-HT3 antagonists used. However, in this study, the efficacy of adding olanzapine to ondansetron and dexamethasone in CINV prevention in both acute and delayed phases in patients on HEC was confirmed by the crossover analysis which controlled the intervariability and intravariability of the patients between two groups.
The addition of olanzapine was well tolerated. Similar to previous studies, there were no serious anti-emetic-related adverse events but more sleepiness in patients on olanzapine [13, 20]. In the crossover analysis, most participants preferred olanzapine over the placebo, reflecting the patients’ perception of benefit over side effects of olanzapine. As a concerned overlapping toxicity, the preplanned QTc interval assessment was performed in this study. The study revealed no significant difference in QTc prolongation incidences and mean QTc changes between olanzapine and placebo groups. However, there was more QTc prolongation in olanzapine group than placebo group among patients receiving cisplatin. Although this finding needs to be validated, we caution the use of ondansetron and olanzapine combination in patients receiving high-dose cisplatin, especially in concurrent with other drugs or conditions that could increase risk of QTc prolongation.
Currently, the anti-emetic regimen consisting of dexamethasone and palonosetron plus a NK-1 antagonist or olanzapine is widely recommended in preventing CINV for HEC [12, 13, 22,23,24,25]. We demonstrated the benefit and safety of adding olanzapine to ondansetron and dexamethasone in patients on HEC. Although the sample size is quite small, these findings support olanzapine, ondansetron and dexamethasone as a standard regimen for patients who lack access to palonosetron and NK-1 antagonist.
Conclusion
Without the NK-1 antagonists, the addition of olanzapine to ondansetron and dexamethasone significantly improved CINV prevention and was safe in patients who were receiving HEC.
References
Ingle RJ, Burish TG, Wallston KA (1984) Conditionability of cancer chemotherapy patients. Oncol Nurs Forum 11(4):97–102
Mitchell EP (2006) Gastrointestinal toxicity of chemotherapeutic agents. Semin Oncol 33(1):106–120
Richardson JL, Marks G, Levine A (1988) The influence of symptoms of disease and side effects of treatment on compliance with cancer therapy. J Clin Oncol 6(11):1746–1752
Bloechl-Daum B, Deuson RR, Mavros P et al (2006) Delayed nausea and vomiting continue to reduce patients’ quality of life after highly and moderately emetogenic chemotherapy despite antiemetic treatment. J Clin Oncol 24(27):4472–4478
Bymaster FP, Rasmussen K, Calligaro DO, Nelson DL, DeLapp NW, Wong DT, Moore NA (1997) In vitro and in vivo biochemistry of olanzapine: a novel, atypical antipsychotic drug. J Clin Psychiatry 58(Suppl 10):28–36
Callaghan JT, Bergstrom RF, Ptak LR et al (1999) Olanzapine. Pharmacokinetic and pharmacodynamic profile. Clin Pharmacokinet 37(3):177–193
Srivastava M, Brito-Dellan N, Davis MP et al (2003) Olanzapine as an antiemetic in refractory nausea and vomiting in advanced cancer. J Pain Symptom Manage 25(6):578–582
Passik SD, Kirsh KL, Theobald DE et al (2003) A retrospective chart review of the use of olanzapine for the prevention of delayed emesis in cancer patients. J Pain Symptom Manage 25(5):485–488
Passik SD, Lundberg J, Kirsh KL et al (2002) A pilot exploration of the antiemetic activity of olanzapine for the relief of nausea in patients with advanced cancer and pain. J Pain Symptom Manage 23(6):526–532
Passik SD, Navari RM, Jung SH et al (2004) A phase i trial of olanzapine (zyprexa) for the prevention of delayed emesis in cancer patients: a hoosier oncology group study. Cancer Invest 22(3):383–388
Chiu L, Chow R, Popovic M et al (2016) Efficacy of olanzapine for the prophylaxis and rescue of chemotherapy-induced nausea and vomiting (cinv): a systematic review and meta-analysis. Support Care Cancer 24(5):2381–2392
Navari RM, Aapro M (2016) Antiemetic prophylaxis for chemotherapy-induced nausea and vomiting. New Engl J Med 374(14):1356–1367
Navari RM, Qin R, Ruddy KJ et al (2016) Olanzapine for the prevention of chemotherapy-induced nausea and vomiting. New Engl J Med 375(2):134–142
Berger MJ, Ettinger DS, Aston J et al (2017) NCCN guidelines insights: Antiemesis, version 2.2017. J Natl Compr Cancer Netw 15(7):883–893
Hesketh PJ, Kris MG, Basch E et al (2017) Antiemetics: American Society of Clinical Oncology Clinical Practice Guideline update. J Clin Oncol 35(28):3240–3261
Harrigan EP, Miceli JJ, Anziano R et al (2004) A randomized evaluation of the effects of six antipsychotic agents on QTc, in the absence and presence of metabolic inhibition. J Clin Psychopharmacol 24(1):62–69
Vieweg WV (2003) New generation antipsychotic drugs and QTc interval prolongation. Prim Care Companion J Clin Psychiatry 5(5):205–215
Albany C, Brames MJ, Fausel C et al (2012) Randomized, double-blind, placebo-controlled, phase III cross-over study evaluating the oral neurokinin-1 antagonist aprepitant in combination with a 5HT3 receptor antagonist and dexamethasone in patients with germ cell tumors receiving 5-day cisplatin combination chemotherapy regimens: a hoosier oncology group study. J Clin Oncol 30(32):3998–4003
Navari RM, Gray SE, Kerr AC (2011) Olanzapine versus aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a randomized phase III trial. J Support Oncol 9(5):188–195
Tan L, Liu J, Liu X et al (2009) Clinical research of olanzapine for prevention of chemotherapy-induced nausea and vomiting. J Exp Clin Cancer Res 28:131
Mizukami N, Yamauchi M, Koike K et al (2014) Olanzapine for the prevention of chemotherapy-induced nausea and vomiting in patients receiving highly or moderately emetogenic chemotherapy: a randomized, double-blind, placebo-controlled study. J Pain Symptom Manage 47(3):542–550
Twelves C, Wong A, Nowacki MP et al (2005) Capecitabine as adjuvant treatment for stage III colon cancer. New Engl J Med 352(26):2696–2704
DeRemer DL, Clemmons AB, Orr J et al (2016) Emerging role of olanzapine for prevention and treatment of chemotherapy-induced nausea and vomiting. Pharmacotherapy 36(2):218–229
National Comprehensive Cancer Network (NCCN) (2019) Antiemesis. Clin Pract Guidel Oncol
Tageja N, Groninger H (2016) Chemotherapy-induced nausea and vomiting: an overview and comparison of three consensus guidelines. Postgrad Med J 92(1083):34–40
Acknowledgement
The project was funded by Chulalongkorn University supporting fund for thesis project and Chulalongkorn Medical Oncology Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Vimolchalao declares that she has no conflict of interest. Dr. Sakdejyont declares that he has no conflict of interest. Ms. Ploytuangporn declares that she has no conflict of interest. Ms. Sukprakun declares that she has no conflict of interest. Ms. Angspatt declares that she has no conflict of interest. Ms. Thawinwisan declares that she has no conflict of interest. Ms. Chenaksara declares that she has no conflict of interest. Dr. Sriuranpong declares that he has no conflict of interest. Dr. Vinayanuwatikun declares that she has no conflict of interest. Dr. Parinyanitikun declares that she has no conflict of interest. Dr. Poowarawan declares that she has no conflict of interest. Dr. Tanasanvimon declares that he has no conflict of interest.
Ethical approval
The study procedures were in accordance with and approved by the Institution Review Board of the Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand, and with the 1964 Helsinki declaration.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Vimolchalao, V., Sakdejayont, S., Wongchanapai, P. et al. The efficacy and safety of the addition of olanzapine to ondansetron and dexamethasone for prevention of chemotherapy-induced nausea and vomiting in patients receiving highly emetogenic chemotherapy. Int J Clin Oncol 25, 396–402 (2020). https://doi.org/10.1007/s10147-019-01570-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-019-01570-3