Abstract
This study was aimed to analyze the survival of patients with spinal chordomas. Patients’ data in the Surveillance, Epidemiology, and End Results (SEER) database were retrieved and analyzed statistically. There were 765 patients with spinal chordomas between 1974 and 2013. The overall survival did not improve significantly over decades for patients receiving surgery and radiotherapy (SR) (P = 0.221). There were significant differences in overall survival among subgroups of patients receiving surgery (S), radiotherapy (R), and neither S nor R (NSR) (P = 0.031, 0.037, and 0.031, respectively). Cancer-specific survival did not change significantly among subgroups of patients receiving R (P = 0.411), while it increased steadily among subgroups of patients receiving S, SR, and NSR (P < 0.001, 0.001, and 0.049, respectively). In the multivariate Cox regression model, younger onset age (hazard ratio [HR] 1.052, P < 0.001), surgery (HR 0.291, P = 0.001), and tumor location of the sacrum (HR 0.401, P = 0.002) were associated with a better overall survival. Similarly, younger onset age (HR 1.036, P = 0.029), surgery (HR 0.221, P = 0.009), and tumor location of the sacrum (HR 0.287, P = 0.002) were also associated with a higher cancer-specific survival. The changes in overall and cancer-specific survival over time differ among different treatment groups. Younger onset age, surgical strategy, and tumor location of the sacrum may be correlated with a higher overall and cancer-specific survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chordomas are rare malignant tumors that originate from notochordal remnants during the spine development period. They are typically low grade but locally invasive malignancies [1]. The tumors prefer occurring in patients with mean age of 60 years old [2]. The overall incidence is about one per million individuals and they account for approximately 1 to 4% of all bone malignancies [3, 4].
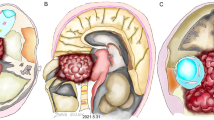
Chordomas are often divided into three types according to the tumor location: skull base, mobile spine, and sacral chordomas, with incidence rates of 30, 20, and 50% respectively [1]. Cases originating from other sites have also been described, but they are very rare [5]. According to their histopathological classification, chordomas can also be divided into three types: classic, chondroid, and dedifferentiated chordomas. However, the latter two types are rarely studied because they are much more infrequent than classic cases.
Patients are often clinically asymptomatic until later stages [6] when the tumors invade into adjacent tissues and cause the local destruction of bone or dysfunction of nerves. The destructive and latent characteristics make it a terrible disease. In addition, approximately 30–40% of patients develop metastases, usually after evidence of local recurrence. Metastases can occur in the lung, liver, bone, and other sites. However, the lethal effect of this disease is primarily due to its local aggressiveness instead of its potential to metastasize [1]. The overall survival rates are 65 and 35% at years 5 and 10, respectively [7,8,9].
Chordomas are the most frequent primary tumors of the mobile spine [10]. Due to their close relationship with the backbone and their invasion to the spinal cord and nerve roots, an increasing number of (radio)surgical strategies have been investigated [10,11,12,13]. However, most studies mainly focused on skull base and sacral chordomas [14,15,16,17,18,19,20]. Some publications reported both mobile spine and sacral chordomas, but they included very few cases [10, 12, 21]. Besides, treatment strategies have changed over time, especially radiotherapy strategies [22,23,24,25,26,27]. Although new treatment strategies have been described with longer survival time and better local control when compared with control group horizontally [28], there is no previous study demonstrating the longitudinal changes in survival in different treatment groups over the last few decades. Thus, whether the survival of patients with spinal chordomas has improved significantly over time is not well understood. In addition, to the best of our knowledge, there is no recent large-scale study investigating the incidence patterns and the influence of clinical factors on overall and cancer-specific survival of patients with spinal chordomas (including mobile spine and sacral chordomas). Silvia et al. reported the largest study with 138 consecutive patients [12]. Although 345 cases of sacral chordomas were investigated last year, a study of mobile spine chordomas and cancer-specific survival has not been conducted, and changes in survival were also not well described [20].
In this study, 765 cases diagnosed between 1974 and 2013 were evaluated using the Surveillance, Epidemiology, and End Results (SEER) program database to reveal the changes in incidence and survival of spinal chordomas. In order to avoid the bias produced by evolution of treatment strategies, 379 patients diagnosed between 2004 and 2013 were further investigated exclusively to determine the influence of clinical factors on the overall and cancer-related survival.
Methods
The SEER database and related codes
The study cohort was obtained from the SEER program’s 2015 Research Data release. We used code number “011” under the North American Association of Central Cancer Registries item “CS Schema v0204+” and found all bone malignancies. All patients with bone malignancies were filtered by the International Classification of Diseases for Oncology (ICD-O-3 edition) histology codes consistent with chordomas (9370, 9371, 9372). Mobile spine and sacrum were coded as C412 and C414. All patients diagnosed with spinal chordomas between 1974 and 2013 were included to reveal the changes in incidence and survival. Patients with unknown treatment strategies (code numbers 8 and 9) were excluded when investigating the influence of clinical factors on survival. Survival time was calculated from the date of diagnosis to the date of death or last follow-up.
Statistical analysis
All patients were divided into four groups according to the treatment strategies: radiotherapy alone (R), surgery alone (S), and surgery combined with radiotherapy (SR), neither surgery nor radiotherapy (NSR). To study the changes in survival over time, each of the groups was further divided into four subgroups according to the year of diagnosis: 1974–1983, 1984–1993, 1994–2003, and 2004–2013.
Changes in survival over time were analyzed via Kaplan-Meier survival analysis. The Cox proportional hazard model was utilized for univariate and multivariate analysis to identify factors associated with survival. Adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) were reported. The significance level for all tests was two sided at 5%. Original data were extracted using Perl language. All data were analyzed using SPSS Statistics software (V.24; IBM Corporation, USA).
Results
Demographics
There were 765 patients with spinal chordomas between 1974 and 2013 (Table 1). Mobile spine and sacral chordomas accounted for 44.3% (n = 339) and 55.7% (n = 426) of total cases, respectively. The median follow-up time was 52 months. The 5- and 10-year overall survival rates for all patients were 65.6 and 38.1%, respectively. The 5- and 10-year cancer-specific survival rates were 71.5 and 47.8%, respectively.
Incidence and changes in survival
The frequency of spinal chordomas increased obviously over the last 40 years (Fig. 1). The incidence rate of such disease was 0.3 per 100,000 and was age-adjusted to the 2000 US Standard Population.
There were no significant differences in overall survival among subgroups of patients receiving SR (P = 0.221) (Fig. 2c), while there were significant differences among subgroups of patients receiving S, R, and NSR (P = 0.031, 0.037, and 0.031, respectively) (Fig. 2b, Fig. 2a, and Fig. 2d). For patients receiving S and NRS, overall survival increased steadily over time, with those diagnosed between 2004 and 2013 presenting the longest overall survival. However, for patients receiving R, those diagnosed between 1984 and 1993 presented the longest overall survival.
a The difference in overall survival among subgroups of patients receiving R was statistically significant (P = 0.037), with patients in 1984–1993 presenting the best overall survival. b The difference in overall survival among subgroups of patients receiving S was statistically significant (P = 0.031), with survival rate increasing steadily over time. c There is no significant difference in overall survival among subgroups of patients receiving SR (P = 0.221). d The difference in overall survival among subgroups of patients receiving NSR was statistically significant (P = 0.031), with survival rate increasing steadily over time
Cancer-specific survival did not change significantly among subgroups of patients receiving R (P = 0.411) (Fig. 3a), while it changed significantly among subgroups of patients receiving S, SR, and NSR (P < 0.001, 0.001, and 0.049, respectively) (Fig. 3b, Fig. 3c, and Fig. 3d). For patients receiving S, SR, and NSR, cancer-specific survival increased steadily over time, with those diagnosed between 2004 and 2013 presenting the longest cancer-specific survival.
a There is no significant difference in cancer-specific survival among subgroups of patients receiving R (P = 0.411). b The difference in cancer-specific survival among subgroups of patients receiving S was statistically significant (P < 0.001), with survival rate increasing steadily over time. c The difference in cancer-specific survival among subgroups of patients receiving SR was statistically significant (P = 0.001), with survival rate increasing steadily over time. d The difference in cancer-specific survival among subgroups of patients receiving NSR was statistically significant (P = 0.049), with survival rate increasing steadily over time
Influence of clinical factors on survival
As described above, to avoid bias produced by the evolution of treatment strategies, only 379 patients diagnosed between 2004 and 2013 were further investigated to reveal the influence of clinical factors on survival. 27.4% (n = 104) of them were dead at last follow-up and 13.7% (n = 52) died due to other reasons instead of chordomas. 82.1% SR were radiotherapy after surgery. 94.8% of radiotherapy was beam radiation; the others included radioactive implants, radioisotopes, and their combination. 6.6% (n = 25) patients were treated with chemotherapy, 80% (n = 20) of which were chemotherapy with radiation or surgery, while 20% (n = 5) were chemotherapy alone. 93.4% (n = 354) patients did not receive chemotherapy or whether they received chemotherapy or not was unknown (incomplete data).
In univariate analysis, factors predicting longer overall survival were younger onset age (HR 1.052, P < 0.001), tumor location of the sacrum (HR 0.668, P = 0.042), surgery (HR 0.288, P < 0.001), and surgery and radiotherapy (HR 0.524, P = 0.010), as well as classic chordomas (HR 0.215, P = 0.009). In the multivariate model, only younger onset age (HR 1.052, P < 0.001), tumor location of the sacrum (HR 0.401, P = 0.002, Fig. 4a), and surgery (HR 0.291, P = 0.001) were significantly associated with improved overall survival (Table 2).
Similarly, factors predicting better cancer-specific survival by univariate analysis included younger onset age (HR 1.053, P < 0.001), tumor location of the sacrum (HR 0.547, P = 0.034), surgery (HR 0.208, P < 0.001), and classic chordomas (HR 0.086, P = 0.001). While in a multivariate model, younger onset age (HR 1.036, P = 0.029), tumor location of the sacrum (HR 0.287, P = 0.002), and surgery (HR 0.221, P = 0.009) were significantly associated with improved cancer-specific survival (Table 3).
Discussion
Chordomas are very rare malignancies, which makes them very difficult to study. The SEER database has accumulated enough cases for large-scale research. We acknowledge that limited information exists regarding local recurrence, complications, chemotherapy, dose of radiotherapy, and margin status in the final pathological examination. To the best of our knowledge, however, this is the largest study on mobile spine and sacral chordomas up to now. In addition, this is the first research regarding the changes in incidence and survival of patients with spinal chordomas over the last decades.
In the updated SEER database, overall specificity and sensitivity are 100 and 80% for SEER radiotherapy data [29]. Since cases with unknown radiotherapy were excluded (n = 14) from our research when investigating the influence of clinical factors on survival, the sensitivity of the radiotherapy data should be higher than 80%. Although this is a retrospective study with inevitable limitations, the data are highly homogeneous since patients with skull base chordomas were excluded and patients were from almost everywhere in the USA, making the results highly generalizable. In addition, the follow-up time was reasonably long. The length of follow-up is important because tumor recurrence is often diagnosed more than 5 years after initial treatment [30].
Consistent with previous studies, our study showed that spinal chordomas occurred in all age groups, with a median age in the sixth decade [30]. We found that the incidence of spinal chordomas increased obviously over the last 40 years, especially during the last 10 years. In addition, our study showed the overall and cancer-specific survival improved steadily over time for patients receiving S. However, there was no significant difference in overall survival among subgroups of patients receiving SR. Surprisingly, patients receiving R diagnosed between 1984 and 1993 had the longest overall survival among subgroups of patients receiving the same treatment. In addition, survival of patients receiving NSR also improved during the most recent decades.
The current standard treatment of chordomas is an en bloc tumorectomy with negative margins [30]. The surgical techniques for margin free, including en bloc tumor resection, are effective in terms of local control and long-term prognosis of thoracic and lumbar spine chordomas [21, 31, 32]. In our study, we confirm that surgery was independently associated with improved survival outcomes.
Survival and local recurrence mainly depend on a complete resection with negative surgical margins. If negative margins are not achieved, recurrence rates will increase to 70% [33]. Unfortunately, a complete resection is almost impossible because chordomas are characterized by disseminated tumor islands, which are often far from the primary tumor mass. These islands are difficult to identify radiologically and intraoperatively [34]. In addition, gross total resection can result in many complications and patients have a high risk of local treatment failure [35]. Thus, local recurrences are frequent, even many years after primary resection [10, 36, 37]. In this situation, radiotherapy has been used as an adjuvant treatment [35].
Current National Comprehensive Cancer Network guidelines recommend surgical resection with or without adjuvant radiotherapy or definitive radiotherapy for unresectable cases [38]. Indeed, high doses of radiotherapy are often employed as an alternative for patients with inoperable chordomas [35, 39], and about 50% patients are recommended to receive postoperative radiotherapy [40]. However, the utilization of radiotherapy decreased over the last 40 years but the reason is still unknown [20]. Some different types of radiotherapy have been described in recent years, including conventional photon beam radiation, intensity-modulated radiation, stereotactic radiation, brachytherapy, and proton beam radiation [41]. Some other published series showed better local control and survival with particle therapy compared with conventional radiotherapy techniques [24, 42, 43]. Combining surgery and radiotherapy resulted in a significant improvement in local control and in a decreased surgical morbidity compared with surgery alone in skull base and cervical spine chordomas [39, 44,45,46]. Despite all this improvement in radiotherapy, the present study revealed that it was not independently associated with higher survival and this was consistent with the results of several other studies [12, 20, 41, 47, 48].
Chordomas have historically been described as radioresistant [30], requiring at least 60 Gy with a standard, fractionated external beam radiation to achieve durable local control [26, 49]. However, the doses of radiotherapy were not recorded in the SEER database. Besides, the majority of cases of radiotherapy in the SEER database were adjuvant radiotherapy, and the timing of treatment was unclear. The benefits may be offset if the adjuvant radiotherapy is not delivered in a timely fashion [50].
Whether tumor size is associated with survival is controversial. Smaller tumor size has been shown to be associated with improved survival [9, 12, 51], while Jones et al. also demonstrated that there was no statistically significant difference in survival among groups based on mean tumor size for patients with skull base chordomas [48]. By using univariate and multivariate Cox proportional hazards analysis, our study showed that tumor size was not an independently prognostic factor for overall survival or cancer-specific survival for patients with spinal chordomas.
In addition, there was no significant difference on overall survival between patients with tumors on mobile spine and sacrum as reported [12]. However, our study proved that patients with tumors on the sacrum presented significantly better overall and cancer-specific survival than those with tumors on mobile spine. The reason to such a controversial outcome might be that the cohort and the potential prognostic factors in their study were different from ours. Only patients who experienced surgery were included in their study.
Clinically, the prognosis of dedifferentiated chordomas was worse than that of the other two histologic subtypes, and histological subtype was a prognostic factor to survival in univariate Cox regression model in our study. However, it was not an independently prognostic factor to survival in the multivariate Cox regression model. Small sample size of dedifferentiated cases might be the potential reason, since the incidence of such cases is particularly rare.
Conclusions
In conclusion, the incidence of spinal chordomas increased over the last 40 years. The changes in overall and cancer-specific survival over time differ among different treatment groups. We confirmed that younger onset age, tumor location on the sacrum, and surgical strategy may be correlated with a longer overall and cancer-specific survival. Large-scale and multi-center studies with more detailed treatment information are required to further determine the optimal treatment strategies for this disease.
References
Coindre JM (2012) New WHO classification of tumours of soft tissue and bone J. Ann Pathol 32(5 Suppl):S115–S116
Yang XR, Ng D, Alcorta DA, Liebsch NJ, Sheridan E, Li S, Goldstein AM, Parry DM, Kelley MJ (2009) T (brachyury) gene duplication confers major susceptibility to familial chordoma[J]. Nat Genet 41(11):1176–1178
Healey JH, Lane JM (1989) Chordoma: a critical review of diagnosis and treatment[J]. Orthop Clin N Am 20(3):417–426
Smoll NR, Gautschi OP, Radovanovic I, Schaller K, Weber DC (2013) Incidence and relative survival of chordomas: the standardized mortality ratio and the impact of chordomas on a population[J]. Cancer 119(11):2029–2037
Lauer SR, Edgar MA, Gardner JM, Sebastian A, Weiss SW (2013) Soft tissue chordomas: a clinicopathologic analysis of 11 cases[J]. Am J Surg Pathol 37(5):719–726
Koutourousiou M, Snyderman CH, Fernandez-Miranda J, Gardner PA (2011) Skull base chordomas[J]. Otolaryngol Clin N Am 44(5):1155–1171
Dorfman HD, Czerniak B (1995) Bone cancers[J]. Cancer 75(1 Suppl):203–210
Mukherjee D, Chaichana KL, Gokaslan ZL, Aaronson O, Cheng JS, McGirt MJ (2011) Survival of patients with malignant primary osseous spinal neoplasms: results from the Surveillance, Epidemiology, and End Results (SEER) database from 1973 to 2003[J]. J Neurosurg Spine 14(2):143–150
McMaster ML, Goldstein AM, Bromley CM, Ishibe N, Parry DM (2001) Chordoma: incidence and survival patterns in the United States, 1973–1995[J]. Cancer Causes Control 12(1):1–11
Boriani S, Bandiera S, Biagini R, Bacchini P, Boriani L, Cappuccio M, Chevalley F, Gasbarrini A, Picci P, Weinstein JN (2006) Chordoma of the mobile spine: fifty years of experience[J]. Spine (Phila Pa 1976) 31(4):493–503
Staab A, Rutz HP, Ares C, Timmermann B, Schneider R, Bolsi A, Albertini F, Lomax A, Goitein G, Hug E (2011) Spot-scanning-based proton therapy for extracranial chordoma[J]. Int J Radiat Oncol Biol Phys 81(4):e489–e496
Stacchiotti S, Casali PG, Lo Vullo S, Mariani L, Palassini E, Mercuri M, Alberghini M, Pilotti S, Zanella L, Gronchi A, Picci P (2010) Chordoma of the mobile spine and sacrum: a retrospective analysis of a series of patients surgically treated at two referral centers[J]. Ann Surg Oncol 17(1):211–219
Clarke MJ, Dasenbrock H, Bydon A, Sciubba DM, McGirt MJ, Hsieh PC, Yassari R, Gokaslan ZL, Wolinsky JP (2012) Posterior-only approach for en bloc sacrectomy: clinical outcomes in 36 consecutive patients[J]. Neurosurgery 71(2):357–364 discussion 64
Wu Z, Zhang J, Zhang L, Jia G, Tang J, Wang L, Wang Z (2010) Prognostic factors for long-term outcome of patients with surgical resection of skull base chordomas-106 cases review in one institution[J]. Neurosurg Rev 33(4):451–456
Yasuda M, Bresson D, Chibbaro S, Cornelius JF, Polivka M, Feuvret L, Takayasu M, George B (2012) Chordomas of the skull base and cervical spine: clinical outcomes associated with a multimodal surgical resection combined with proton-beam radiation in 40 patients[J]. Neurosurg Rev 35(2):171–182 discussion 82–3
Ouyang T, Zhang N, Zhang Y, Jiao J, Ren J, Huang T, Chen J (2014) Clinical characteristics, immunohistochemistry, and outcomes of 77 patients with skull base chordomas[J]. World Neurosurg 81(5–6):790–797
Rachinger W, Eigenbrod S, Dutzmann S, Simon M, Feigl GC, Kremenevskaja N, Kretzschmar H, Zausinger S, Kreth FW, Thon N, Tonn JC (2014) Male sex as a risk factor for the clinical course of skull base chordomas[J]. J Neurosurg 120(6):1313–1320
Fuchs B, Dickey ID, Yaszemski MJ, Inwards CY, Sim FH (2005) Operative management of sacral chordoma[J]. J Bone Joint Surg Am 87(10):2211–2216
Park L, Delaney TF, Liebsch NJ, Hornicek FJ, Goldberg S, Mankin H, Rosenberg AE, Rosenthal DI, Suit HD (2006) Sacral chordomas: impact of high-dose proton/photon-beam radiation therapy combined with or without surgery for primary versus recurrent tumor[J]. Int J Radiat Oncol Biol Phys 65(5):1514–1521
Yu E, Koffer PP, DiPetrillo TA, Kinsella TJ (2016) Incidence, treatment, and survival patterns for sacral chordoma in the United States, 1974–2011[J]. Front Oncol 6:203
Bergh P, Kindblom LG, Gunterberg B, Remotti F, Ryd W, Meis-Kindblom JM (2000) Prognostic factors in chordoma of the sacrum and mobile spine: a study of 39 patients[J]. Cancer 88(9):2122–2134
Fuller DB, Bloom JG (1988) Radiotherapy for chordoma[J]. Int J Radiat Oncol Biol Phys 15(2):331–339
Gupta T, Wadasadawala T, Master Z, Phurailatpam R, Pai-Shetty R, Jalali R (2012) Encouraging early clinical outcomes with helical tomotherapy-based image-guided intensity-modulated radiation therapy for residual, recurrent, and/or progressive benign/low-grade intracranial tumors: a comprehensive evaluation[J]. Int J Radiat Oncol Biol Phys 82(2):756–764
Kano H, Iqbal FO, Sheehan J, Mathieu D, Seymour ZA, Niranjan A, Flickinger JC, Kondziolka D, Pollock BE, Rosseau G, Sneed PK, McDermott MW, Lunsford LD (2011) Stereotactic radiosurgery for chordoma: a report from the North American Gamma Knife Consortium[J]. Neurosurgery 68(2):379–389
Gutin PH, Leibel SA, Hosobuchi Y, Crumley RL, Edwards MS, Wilson CB, Lamb S, Weaver KA (1987) Brachytherapy of recurrent tumors of the skull base and spine with iodine-125 sources[J]. Neurosurgery 20(6):938–945
Catton C, O'Sullivan B, Bell R, Laperriere N, Cummings B, Fornasier V, Wunder J (1996) Chordoma: long-term follow-up after radical photon irradiation[J]. Radiother Oncol 41(1):67–72
Terahara A, Niemierko A, Goitein M, Finkelstein D, Hug E, Liebsch N, O'Farrell D, Lyons S, Munzenrider J (1999) Analysis of the relationship between tumor dose inhomogeneity and local control in patients with skull base chordoma[J]. Int J Radiat Oncol Biol Phys 45(2):351–358
Alonso-Basanta M, Lustig RA, Kennedy DW (2011) Proton beam therapy in skull base pathology[J]. Otolaryngol Clin N Am 44(5):1173–1183
Noone AM, Lund JL, Mariotto A, Cronin K, McNeel T, Deapen D, Warren JL (2016) Comparison of SEER treatment data with medicare claims[J]. Med Care 54(9):e55–e64
Stacchiotti S, Sommer J (2015) Chordoma Global Consensus G. Building a global consensus approach to chordoma: a position paper from the medical and patient community[J]. Lancet Oncol 16(2):e71–e83
Bosma JJ, Pigott TJ, Pennie BH, Jaffray DC (2001) En bloc removal of the lower lumbar vertebral body for chordoma. Report of two cases[J]. J Neurosurg 94(2 Suppl):284–291
Hsu KY, Zucherman JF, Mortensen N, Johnston JO, Gartland J (2000) Follow-up evaluation of resected lumbar vertebral chordoma over 11 years: a case report[J]. Spine (Phila Pa 1976) 25(19):2537–2540
Chugh R, Tawbi H, Lucas DR, Biermann JS, Schuetze SM, Baker LH (2007) Chordoma: the nonsarcoma primary bone tumor[J]. Oncologist 12(11):1344–1350
Guinto G, Guinto-Nishimura Y (2014) Clivus chordomas: role of surgery[J]. World Neurosurg 81(5–6):688–689
DeLaney TF, Liebsch NJ, Pedlow FX, Adams J, Dean S, Yeap BY, McManus P, Rosenberg AE, Nielsen GP, Harmon DC, Spiro IJ, Raskin KA, Suit HD, Yoon SS, Hornicek FJ (2009) Phase II study of high-dose photon/proton radiotherapy in the management of spine sarcomas[J]. Int J Radiat Oncol Biol Phys 74(3):732–739
Baratti D, Gronchi A, Pennacchioli E, Lozza L, Colecchia M, Fiore M, Santinami M (2003) Chordoma: natural history and results in 28 patients treated at a single institution[J]. Ann Surg Oncol 10(3):291–296
York JE, Kaczaraj A, Abi-Said D, Fuller GN, Skibber JM, Janjan NA, Gokaslan ZL (1999) Sacral chordoma: 40-year experience at a major cancer center[J]. Neurosurgery 44(1):74–79 discussion 9–80
Biermann JS, Chow W, Reed DR, Lucas D, Adkins DR, Agulnik M, Benjamin RS, Brigman B, Budd GT, Curry WT, Didwania A, Fabbri N, Hornicek FJ, Kuechle JB, Lindskog D, Mayerson J, McGarry SV, Million L, Morris CD, Movva S, O’Donnell RJ, Randall RL, Rose P, Santana VM, Satcher RL, Schwartz H, Siegel HJ, Thornton K, Villalobos V, Bergman MA, Scavone JL (2017) NCCN guidelines insights: bone cancer, version 2.2017[J]. J Natl Compr Cancer Netw 15(2):155–167
Foweraker KL, Burton KE, Maynard SE, Jena R, Jefferies SJ, Laing RJ, Burnet NG (2007) High-dose radiotherapy in the management of chordoma and chondrosarcoma of the skull base and cervical spine: part 1—clinical outcomes[J]. Clin Oncol (R Coll Radiol) 19(7):509–516
Mendenhall WM, Mendenhall CM, Lewis SB, Villaret DB, Mendenhall NP (2005) Skull base chordoma[J]. Head Neck 27(2):159–165
Chambers KJ, Lin DT, Meier J, Remenschneider A, Herr M, Gray ST (2014) Incidence and survival patterns of cranial chordoma in the United States[J]. Laryngoscope 124(5):1097–1102
Di Maio S, Rostomily R, Sekhar LN (2012) Current surgical outcomes for cranial base chordomas: cohort study of 95 patients[J]. Neurosurgery 70(6):1355–1360 discussion 60
Bugoci DM, Girvigian MR, Chen JC, Miller MM, Rahimian J (2013) Photon-based fractionated stereotactic radiotherapy for postoperative treatment of skull base chordomas[J]. Am J Clin Oncol 36(4):404–410
Ares C, Hug EB, Lomax AJ, Bolsi A, Timmermann B, Rutz HP, Schuller JC, Pedroni E, Goitein G (2009) Effectiveness and safety of spot scanning proton radiation therapy for chordomas and chondrosarcomas of the skull base: first long-term report[J]. Int J Radiat Oncol Biol Phys 75(4):1111–1118
Crockard HA, Steel T, Plowman N, Singh A, Crossman J, Revesz T, Holton JL, Cheeseman A (2001) A multidisciplinary team approach to skull base chordomas[J]. J Neurosurg 95(2):175–183
Colli B, Al-Mefty O (2001) Chordomas of the craniocervical junction: follow-up review and prognostic factors[J]. J Neurosurg 95(6):933–943
Amer HZ, Hameed M (2010) Intraosseous benign notochordal cell tumor[J]. Arch Pathol Lab Med 134(2):283–288
Jones PS, Aghi MK, Muzikansky A, Shih HA, Barker FG 2nd, Curry WT Jr (2014) Outcomes and patterns of care in adult skull base chondrosarcomas from the SEER database[J]. J Clin Neurosci 21(9):1497–1502
Cummings BJ, Hodson DI, Bush RS (1983) Chordoma: the results of megavoltage radiation therapy[J]. Int J Radiat Oncol Biol Phys 9(5):633–642
Holliday EB, Mitra HS, Somerson JS, Rhines LD, Mahajan A, Brown PD, Grosshans DR (2015) Postoperative proton therapy for chordomas and chondrosarcomas of the spine: adjuvant versus salvage radiation therapy[J]. Spine (Phila Pa 1976) 40(8):544–549
Lee J, Bhatia NN, Hoang BH, Ziogas A, Zell JA (2012) Analysis of prognostic factors for patients with chordoma with use of the California Cancer Registry[J]. J Bone Joint Surg Am 94(4):356–363
Acknowledgements
We acknowledge the SEER program committee for their permission of allowing us to use the data to conduct our research.
Funding
The work was supported by the National Natural Science Foundation of China (81572109 and 81572190).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
We signed the Data-Use Agreement for the SEER 1973–2013 Research Data File and had permission to use the database for research.
Rights and permissions
About this article
Cite this article
Sun, HH., Hong, X., Liu, B. et al. Survival analysis of patients with spinal chordomas. Neurosurg Rev 42, 455–462 (2019). https://doi.org/10.1007/s10143-018-0968-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-018-0968-7