Abstract
The purpose of this study was to compare dentinal tubule sealing effects of a 532-nm diode-pumped solid-state (DPSS) laser, gallic acid/Fe3+ complex, and three commercially available dentin desensitizers. Human premolars (n = 44) extracted for orthodontics had standardized cervical cavities prepared, etched (37% phosphoric acid) and randomly assigned to either a control (n = 4), or one of five treatment groups (n = 8/group). Desensitizing treatments were either a 532-nm DPSS laser, gallic acid/Fe3+ complex, oxalate-based Super Seal™ (SS), DIO™ Enamel Coating Pen Pro Tooth (Dio), or adhesive-type Hybrid Coat™ (HC). Dentinal fluid flow (DFF) was monitored continuously in real time during the application of each desensitizing agent, by using a nanoliter-scaled fluid flow-measuring device. Following treatment, morphological changes on dentinal surfaces and within tubules were observed by scanning electron microscopy (SEM). DFF rates were significantly reduced after treatment in all experimental groups (P < 0.05), except SS (P > 0.05). The gallic acid/Fe3+ complex reduced DFF rates the most, and significantly (P < 0.05) more than the three commercial dentin desensitizers. There were no significant differences in DFF reduction rates between the gallic acid/Fe3+ complex and the DPSS laser groups (P > 0.05). There were no significant differences in DFF reduction rates among the three commercial dentin desensitizers (P > 0.05). SEM examination of treated dentin showed that the degree of occlusion of dentinal tubules correlated closely with the corresponding reduction in DFF rates. The gallic acid/Fe3+ complex and 532-nm DPSS laser were superior to other desensitizing methods in occluding dentinal tubules and reducing DFF rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dentin hypersensitivity (DH) is commonly attributed to the hydrodynamic theory [1]. Stimuli applied to dentin induce fluid flow within dentinal tubules, which activate nociceptors in the pulp-dentin complex causing pain and DH [2]. Unsealed dentinal tubules and high levels of dentin permeability are observed in DH [3]. Therefore, occluding dentinal tubules via in situ remineralization is the objective of dentin desensitizers [4]. Most commonly, oxalate or fluoride ions are used to form complexes with calcium, and in vitro studies have demonstrated oxalate crystals occluding dentinal tubules [5,6,7]. Additionally, varnishes such as adhesives [8] and protein precipitation [9] have been applied to occlude dentinal tubules. However, superficial layers of calcium oxalate crystals or varnish may wear out by brushing and/or dietary acids [10, 11]. Therefore, therapies with long-term effectiveness have pursued intratubular mineral crystal deposition [12].
Bioactive materials that are capable of intratubular mineralization have been used to block exposed dentinal tubules [13]. Toothpastes containing bioactive glass ceramics or nano-hydroxyapatite (n-HA) have demonstrated the occlusion of open dentinal tubules through mineral deposition [13, 14]. DIO Enamel Coating Pen Pro Tooth (Dio Corporation, Pusan, Korea) contains tricalcium phosphate (TCP) and n-HA, which the manufacturer claims can fill abraded enamel, thereby managing DH. However, its effectiveness in occluding dentinal tubules is yet to be substantiated.
Gallic acid/metal ion complexes adhered and formed stable cross links on the dentinal surface, and thus blocked dentinal tubules by as much as 52% within 4 min [15]. However, a comparison of their occluding efficacy with that of adhesive type desensitizers is missing.
Laser treatments for DH were introduced in the 1980s [16]. The five types of lasers used in these treatments are Nd:YAG, Er:YAG, Er;Cr:YSGG, CO2, and GaAlAs (diode) lasers [16, 17]. The diode lasers have low-power output, while the others have middle-power output, and the former produce a continuous wave without overheating their substrate [18], whereas the latter may harm the underlying pulp [19]. Diode lasers with wavelengths between 780 and 900 nm have been clinically effective in the treatment of dentine hypersensitivity [20, 21], and it was thought that they mediate an analgesic effect through depressed nerve transmission [16]. However, the effectiveness of a 532-nm diode-pumped solid-state (DPSS) laser in reducing DH has not been studied.
Most studies on the effects of desensitizing agents have been limited to scanning electron microscopic examination of dentinal tubules [13, 22]. Since dentinal fluid flow (DFF) induced by external stimuli is the main mechanism for DH, the measurement of DFF in real time during the application of desensitizing agents, by using a nanoliter-scale fluid flow-measuring device, is crucial in evaluating the effectiveness of desensitizing agents [5, 6].
The purpose of this study was to evaluate the dentinal tubule sealing effect by measuring DFF in real time during each application. Five different types of desensitizers, which included a 532-nm DPSS laser, gallic acid/Fe3+ complex, oxalate-based Super Seal™, Dio™ Enamel Coating Pen Pro Tooth, and adhesive-type Hybrid Coat™, were tested. Morphological changes in the dentinal tubules following these treatments were examined by scanning electron microscopy (SEM). The null hypothesis was that there would be no difference in the DFF rate before and after desensitizing agent application, and there would be no differences between the desensitizers.
Materials and methods
Structure of the real-time fluid flow-measuring instrument
DFF was measured by using a nanoliter-scale fluid flow-measuring device (Nano-Flow, IB Systems, Seoul, Korea) as used in the previous studies [5, 6] (Fig. 1). The instrument contained three components: (i) a glass capillary and photosensor for detecting fluid movement; (ii) a servomotor, lead screw, and ball nut for tracking fluid movement; and (iii) a rotary encoder and computer software for recording data. An air bubble was created in a water-filled glass capillary (internal diameter of 0.5 mm), which connected the tooth to a water reservoir. A photosensor consisting of an infrared light-emitting diode and a phototransistor detected movement of the air bubble in the capillary. The servo amplifier and servomotor rotated a lead screw in response to voltage from the photosensor, which continuously tracked the air-water interface. The rotation of the screw was measured by a rotary encoder (1000 pulses/rotation), and recorded by a computer. This instrument measured water movement at a threshold volume of 0.2 nL.
Specimen preparation
This study was approved by the Institutional Review Board, Seoul National University Dental Hospital, Seoul, Korea (ERI15005). Maxillary and mandibular premolars (n = 44) that had been extracted for orthodontic treatment and devoid of caries or restorations were collected. Their roots were resected at 5 mm below the cementoenamel junction (CEJ) with an IsoMet® Low Speed Saw (Buehler, Lake Bluff, IL, USA). The pulp tissue was removed from the pulp chamber with endodontic files. A metal tube (diameter 0.9 mm) was inserted into the canal to connect the tooth through silicone tubing with the glass capillary of the fluid flow-measuring device (Fig. 1). The tooth was mounted on a glass slide and secured with a dentin bonding agent (Adper™ Scotchbond™ Multi-Purpose, 3M ESPE, St. Paul, MN, USA) and a flowable composite (Denflow, Vericom, Anyang, Korea). The exposed root surface and outer surface of the bonded interface between the tooth and glass slide were covered with nail varnish to prevent leakage.
Cervical cavity preparation and measurement of dentinal fluid flow during desensitizing agent application/laser irradiation
The mounted teeth were connected to the measuring device, and the absence of leakage under hydrostatic pressure (20 cm H2O, 10 min) was confirmed. A standardized V-shaped cervical cavity was prepared at the CEJ of each tooth (mesiodistal width 5 mm, occluso-cervical height 3 mm, depth 2 mm) by using a high-speed handpiece (MACH-QD, NSK, Tokyo, Japan) with a round-end tapered diamond bur (TR-12, Mani, Tochigi, Japan). The cavity was etched with 32% phosphoric acid (Scotchbond™ Universal Etchant, 3M ESPE) for 15 s to remove the smear layer, rinsed with water, and dried with a cotton pellet. Throughout these procedures, the DFF was measured continuously in real time.
The mounted teeth were randomly assigned to five experimental groups (n = 8/group) and a control group (n = 4), and their cervical cavities subjected to one of the following desensitizing treatments, according to the manufacturers’ instructions. The mode of action of the desensitizing agents were further subdivided into (i) formation of mechanical barrier on the dentinal tubules (Super Seal™, Hybrid Coat™, Dio™ Enamel Coating Pen Pro Tooth), (ii) a structural change to the dentinal surface (DPSS laser), and (iii) a chemical action on the dentinal surface (gallic acid/Fe3+ complex).
-
Group 1: Super Seal™ (SS; Phoenix Dental, Fenton, MI, USA), an oxalate-based topical desensitizing agent, was applied for 30 s and gently air-dried for 30 s.
-
Group 2: Hybrid Coat™ (HC; Sun Medical, Moriyama, Japan), a 4-methacryloyloxyethyl trimellitate anhydride (4-META)-containing adhesive-type desensitizing agent, was applied using a coat sponge, keeping the tooth surface moist for 20 s, mildly air-dried for 5 s, and strongly air-dried for 5 s, and then lightly cured for 10 s using LED (B&Lite S, B&L Biotech, Ansan, Korea).
-
Group 3: DIO™ Enamel Coating Pen Pro Tooth (Dio; Dio Corporation), a n-HA- and TCP-containing toothpaste, was applied with a cotton swab for 60 s, left in place for 30 s, and then rinsed with water spray for 30 s.
-
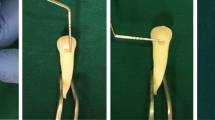
Group 4: Diode-pumped solid-state laser (L; Dental 5, Bison, Seoul, Korea) at wavelength 532 nm and energy level 0.5 W, irradiated for 10 s, with a 5-s rest time between each of three repeat applications. Each application was continuous-wave laser output, and in non-contact mode with 2–3 mm between the optical fiber and the irradiated surface.
-
Group 5: The gallic acid/Fe3+ complex (GF) was applied for 60 s, with 60 s of rest between each of the four repeat applications, as previously reported [15]. The GF solution was refreshed in each application. Gallic acid and FeCl3 were purchased from Sigma-Aldrich (St. Louis, MO, USA). Aqueous solutions of FeCl3 (1.2 × 10−3 M) and gallic acid (0.47 × 10−3 M) were separately prepared and mixed, and the pH was raised to 8.0 by slowly adding NaOH (0.1 M) solution.
Control: No desensitizing treatment was applied.
The DFF was continuously measured until 10 min after initiation of the desensitizing treatment. From the DFF curve, pre- (as a baseline flow rate) and post-application DFF rates were determined. Reduction of the DFF rate was calculated as follows: (%) = 100 × (baseline flow rate − post-application flow rate) / baseline flow rate.
SEM preparation
After measurement of DFF, three teeth in each group were randomly selected for SEM examination. The coronal part of the cervical cavity was sectioned horizontally to yield 3-mm-thick disks, by using a low-speed diamond disk (NTI-Kahla GmbH, Kahla, Germany). Buccal and lingual grooves were prepared using the low-speed diamond disk, avoiding passing through the disk specimen. These disks were then split along their longitudinal axis, dried in a critical point dryer (HCP-2h), and gold-sputtered. The treated surface and fractured subsurface were observed with an SEM (S-4700, Hitachi, Tokyo, Japan) at ×3000 and ×10,000 magnifications.
Statistical analysis
Differences in the DFF rate before and after desensitization treatment in each group were analyzed by paired t test. DFF rate reductions among groups were compared by one-way analysis of variance followed by Tukey’s HSD post hoc test. IBM SPSS version 21 software package (IBM Corp, Armonk, NY, USA) was used, and the level of significance was set at P < 0.05.
Results
DFF reduction
The nanoliter-scale fluid flow-measuring device was effective at measuring DFF in real time. Any changes in DFF that occurred before, during, and after the application of each desensitizing agent could be monitored by plotting DFF (nL) as a function of time (s) for each specimen (Fig. 2). All groups experienced negative flow during cavity preparation and wash, and positive flow during acid etching and drying procedure. In the untreated control, DFF increased constantly after drying (Fig. 2a). During the application of SS, DFF was blocked momentarily, then increased abruptly from gentle air drying, and soon re-established at a slightly reduced rate of flow than the original baseline (Fig. 2b). In the HC group, steep positive flow was shown during air blow after HC application. Then, negative flow was observed during light curing, followed by positive flow with a decreased slope (Fig. 2c). In the Dio group, the slope of fluid flow maintained during application of the agent and waiting, followed by a negative curve during wash. After washing, positive flow with a decreased slope was observed (Fig. 2d). Laser irradiation markedly decreased the slope of the fluid flow to a steady state. After laser irradiation, the curve of DFF showed a positive flow with a decreased slope (Fig. 2e). Application of GF reduced the DFF rate to nearly zero or even caused a slightly negative curve. After the GF application, DFF demonstrated a positive flow with a remarkably decreased slope (Fig. 2f).
Representative graphs of dentinal fluid flow (nL) measured in real time (s) during the application of each desensitizing agent. a Non-treated control. b Super Seal. c Hybrid Coat. d Dio. e DSPP laser. f Gallic acid/Fe3+ complex. An asterisk (*) means that the post-application flow rate significantly reduced compared with that of the baseline flow rate in HC, Dio, L, and GF groups. p, cavity preparation; e, acid etching; w, wash; d, dry; BFR, baseline flow rate; PFR, post-application flow rate; A, application of the agent; g.a, gentle air dry; lc, light curing; r, water rinse; L, laser irradiation
The DFF rate after application of desensitizing agent/laser irradiation was significantly reduced compared to the initial DFF rate for all experimental groups (P < 0.05), except in the SS group (P > 0.05) (Table 1). The DFF rate did not significantly change in the control group (P > 0.05) (Table 1). The GF group showed the greatest reduction in the DFF rate (79.4 ± 13.6%), followed by L (66.1 ± 8.1%), HC (45.8 ± 8.1%), Dio (42.6 ± 4.9%), and SS (37.5 ± 5.0%). The GF and L groups did not show significant difference in reduction of DFF (P > 0.05) (Fig. 3). There was no statistically significant difference in the DFF reduction rate among the SS, Dio, and HC groups (P > 0.05) (Fig. 3). All experimental groups showed significantly greater DFF reduction than the control (P < 0.05) (Fig. 3).
SEM examination
A SEM examination of the dentin surfaces revealed morphological changes following treatments with desensitizing agents (Fig. 4). The untreated controls and acid-etched specimens showed dentinal tubules that were open and empty (Fig. 4a). The SS group had dentinal tubules that were partially occluded with micron-sized particles of various diameters, which loosely filled their orifices (Fig. 4b). These precipitates extended to a depth of up to 20 μm within the tubules, when their fractured subsurface was examined (Fig. 4b). Similarly, Dio-treated dentin showed partial occlusion of the dentinal tubule orifice. In the cross-sectional view, many tiny crystal precipitates were in the dentinal tubule. The deposits extended to a depth of up to 20 μm within the tubules (Fig. 4d). HC-treated dentin showed that nearly half the tubules were blocked. In the fractured subsurface view, columnar mass plugging tubule orifices were observed in the HC group (Fig. 4c), whereas globular particles filled tubule orifices in SS and Dio. Nearly half of the tubules had been obstructed and constricted by laser irradiation. In the cross-sectional view, the blocked dentinal tubules demonstrated an indistinct boundary of the tubule (Fig. 4e). In the GF group, almost all tubule orifice was occluded in the cross-sectional view. In the fractured subsurface view of the GF-treated dentin, adjacent peritubular dentin was connected by the gallic acid/Fe3+ complex (Fig. 4f).
Representative SEM images of the treated dentin surfaces that show exposed dentinal tubules at their openings (left panels) and within their lumen (middle and right panels), following the application of each desensitizing agent. a Untreated control. b Super Seal. c Hybrid Coat. d Dio. e DSPP laser. f Gallic acid/Fe3+ ion complex group. Left and middle panels, (original magnification, ×3000); right panel, magnified image of the box in the middle panel (original magnification, ×10,000)
Discussion
In this study, DFF was measured in real time during the application of each desensitization technique, by using a nanoliter-scale fluid flow-measuring device. Despite the ex vivo design, our model is revealed more clinically relevant than previous studies, which were evaluated on dentin disks [22, 23]. Furthermore, the reductions in DFF can be quantified, and the statistical differences between the groups could be compared.
The gallic acid/Fe3+ complex provided the greatest reduction in DFF, as their ion complexes bound tightly to the entrance of dentinal tubules. In gallic acid, the pyrogallol group binds to dentin through Fe3+ ion, which create stable cross-linked complexes in an aqueous environment, due to the high binding energy of the pyrogallol-iron complex in water [24]. Under SEM, the treated dentinal surfaces showed tight bridge-like connections between adjacent peritubular dentin, which markedly reduced the outward flow. This study has demonstrated the immediate effects of the gallic acid/Fe3+ complex on DFF, and a previous study reported its long-term effects on mineral formation after 7 days of incubation in artificial saliva [15]. They mentioned that GF could slightly discolor dentin; however, the color change fell into a category that was esthetically acceptable (ΔE = 5.5) [25].
Alternatively, lasers have already proven to be proficient at treating DH [17]. This study is the first to have used a 532-nm DPSS laser while measuring DFF in real time. The 532-nm DPSS laser treatment yielded the second greatest reduction in DFF, which was not significantly different from that of the gallic acid/Fe3+ complex. The DFF rate was maintained at a steady level during the application of this low energy laser, whereas Kim et al. [6] reported inward dentinal fluid flow from the higher thermal energy of an Nd:YAG laser. SEM showed tubules sealed by laser irradiation, which differed from the mechanical interference that was created by the SS or HC treatments. In this study, there were three laser applications (0.5 W) of 10-s duration so that the dentin could be cooled at the rest time between laser irradiation. Pulp temperature increase of approximately 2.2 °C resulted in minimal change to pulp and dentin [26]. Although the energy level of the 532-nm DPSS laser used in this study was not intense, the effects of the laser on temperature of the pulp will need to be evaluated more carefully. Since diode lasers may block depolarization of afferent fibers and thereby suppress nerve transmission, the desensitizing effects of this marked reduction (60%) in DFF are likely to be further augmented by the suppression of nerve transmission in vivo [27].
In the SS group, oxalate ions bound calcium ions on the dentin surface to form calcium oxalate crystals [5]. SEM showed that the orifices of dentinal tubules were filled with many tiny crystals, as previously reported [5, 6, 28]. However, the precipitates were sparsely packed, with gaps between the crystals and the tubule wall, and the reduction in DFF was insignificant.
Hybrid Coat is an adhesive type of desensitizing agent that contains 4-META, which is a functional monomer with both hydrophobic and hydrophilic groups on the same molecule [29]. It might reduce DFF by forming a hybrid layer and tag within open dentinal tubules [30]. In this study, the reduction of DFF by HC was inferior to GF, which suggests that GF formed a stronger bond to dentin than HC. After application of HC, light curing was performed according to the manufacturer’s instruction. The light curing resulted in thermal expansion of fluid within the pulp chamber, which caused a transient negative curve as previously reported [5, 6].
The manufacturer of Dio claims n-HA and TCP will fill within the abraded enamel layer. Under SEM, the particles loosely filled open dentinal tubules without interaction with the dentin structure. Since the degree of dentinal tubule occlusion by Dio was less than the L or GF groups, the DFF reduction rate was lower. In this study, Dio was applied once, for 90 s. Dentinal tubule-occluding effects could be potentiated by repeated application of Dio. Remineralization effects of n-HA on demineralized lesions in teeth have been reported [31, 32].
The current study evaluated the sealing capacity of five desensitizing methods on dentinal tubules. Dentin desensitizers that induced structural changes (L), or chemical actions on dentin (GF), showed greater DFF reductions compared to dentin desensitizers that provided physical/mechanical barriers (SS, HC, Dio). A new 532-nm DPSS laser and gallic acid/Fe3+ complex could be effectively used in the treatment of DH as suggested by their reducing DFF. However, the fluid flow measuring device was operated in vitro using water. In vivo, the process of demineralization and remineralization occurs continuously and the occlusion of dentinal tubules may be affected by saliva. Long-term effects of these agents and their durability over abrasive or erosive challenges need further clinical investigation.
Conclusion
The gallic acid/Fe3+ complex and the 532-nm DPSS laser were superior to other desensitizing methods in occluding dentinal tubules and reducing DFF rates.
References
Brännström M, Linden LA, Aström A (1967) The hydrodynamics of the dental tubule and of pulp fluid. A discussion of its significance in relation to dentinal sensitivity. Caries Res 1:310–317
Närhi M, Jyvasjarvi E, Virtanen A, Huopaniemi T, Ngassapa D, Hirvonen T (1992) Role of intradental A- and C-type nerve fibres in dental pain mechanisms. Proc Finn Dent Soc 88(Suppl 1):507–516
Pashley DH (1986) Dentin permeability, dentin sensitivity, and treatment through tubule occlusion. J Endod 12:465–474
Schmidlin PR, Sahrmann P (2013) Current management of dentin hypersensitivity. Clin Oral Investig 17(Suppl 1):S55–S59
Kim SY, Kim EJ, Kim DS, Lee IB (2013) The evaluation of dentinal tubule occlusion by desensitizing agents: a real-time measurement of dentinal fluid flow rate and scanning electron microscopy. Oper Dent 38:419–428
Kim MH, Kim RJ, Lee WC, Lee IB (2015) Evaluation of dentin tubule occlusion after laser irradiation and desensitizing agent application. Am J Dent 28:303–308
Petersson LG (2013) The role of fluoride in the preventive management of dentin hypersensitivity and root caries. Clin Oral Investig 17(Suppl 1):S63–S71
de Andrade e Silva SM, Marquezini L Jr, Manso AP, Garcia FP, Carrilho MR, Pashley DH, Tay FR, Carvalho RM (2007) Effects of a combined application of potassium oxalate gel/adhesive agent on dentin permeability in vitro. J Adhes Dent 9:505–512
Qin C, Xu J, Zhang Y (2006) Spectroscopic investigation of the function of aqueous 2-hydroxyethylmethacrylate/glutaraldehyde solution as a dentin desensitizer. Eur J Oral Sci 114:354–359
Miglani S, Aggarwal V, Ahuja B (2010) Dentin hypersensitivity: recent trends in management. J Conserv Dent 13:218–224
Schmalz G, Hellwig F, Mausberg RF, Schneider H, Krause F, Haak R, Ziebolz D (2017) Dentin protection of different desensitizing varnishes during stress simulation: an in vitro study. Oper Dent 42:E35–e43. https://doi.org/10.2341/16-068-l
Suge T, Kawasaki A, Ishikawa K, Matsuo T, Ebisu S (2005) Comparison of the occluding ability of dentinal tubules with different morphology between calcium phosphate precipitation method and potassium oxalate treatment. Dent Mater J 24:522–529
Kulal R, Jayanti I, Sambashivaiah S, Bilchodmath S (2016) An in-vitro comparison of nano hydroxyapatite, novamin and proargin desensitizing toothpastes—a SEM study. J Clin Diagn Res 10:Zc51–zc54. https://doi.org/10.7860/jcdr/2016/18991.8649
Zhong Y, Liu J, Li X, Yin W, He T, Hu D, Liao Y, Yao X, Wang Y (2015) Effect of a novel bioactive glass-ceramic on dentinal tubule occlusion: an in vitro study. Aust Dent J 60:96–103
Prajatelistia E, Ju SW, Sanandiya ND, Jun SH, Ahn JS, Hwang DS (2016) Tunicate-inspired gallic acid/metal ion complex for instant and efficient treatment of dentin hypersensitivity. Adv Healthc Mater 5:919–927
Kimura Y, Wilder-Smith P, Yonaga K, Matsumoto K (2000) Treatment of dentine hypersensitivity by lasers: a review. J Clin Periodontol 27:715–721
Sgolastra F, Petrucci A, Severino M, Gatto R, Monaco A (2013) Lasers for the treatment of dentin hypersensitivity: a meta-analysis. J Dent Res 92:492–499
El Yazami H, Zeinoun T, Bou Saba S, Lamard L, Peremans A, Limme M, Geerts S, Lamy M, Nammour S (2010) Pulp temperature increase during photo-activated disinfection (PAD) of periodontal pockets: an in vitro study. Lasers Med Sci 25:655–659
Turkmen C, Gunday M, Karacorlu M, Basaran B (2000) Effect of CO2, Nd:YAG, and ArF excimer lasers on dentin morphology and pulp chamber temperature: an in vitro study. J Endod 26:644–648
Hashim NT, Gasmalla BG, Sabahelkheir AH, Awooda AM (2014) Effect of the clinical application of the diode laser (810 nm) in the treatment of dentine hypersensitivity. BMC Res Notes 7:31
Sicilia A, Cuesta-Frechoso S, Suárez A, Angulo J, Pordomingo A, De Juan P (2009) Immediate efficacy of diode laser application in the treatment of dentine hypersensitivity in periodontal maintenance patients: a randomized clinical trial. J Clin Periodontol 36:650–660
Gholami GA, Fekrazad R, Esmaiel-Nejad A, Kalhori KA (2011) An evaluation of the occluding effects of Er;Cr:YSGG, Nd:YAG, CO(2) and diode lasers on dentinal tubules: a scanning electron microscope in vitro study. Photomed Laser Surg 29:115–121
Saluja M, Grover HS, Choudhary P (2016) Comparative morphologic evaluation and occluding effectiveness of Nd: YAG, CO2 and diode lasers on exposed human dentinal tubules: an in vitro SEM study. J Clin Diagn Res 10:Zc66–Zc70. https://doi.org/10.7860/jcdr/2016/18262.8188
Ejima H, Richardson JJ, Liang K, Best JP, van Koeverden MP, Such GK, Cui J, Caruso F (2013) One-step assembly of coordination complexes for versatile film and particle engineering. Science 341:154–157
Douglas RD, Brewer JD (1998) Acceptability of shade differences in metal ceramic crowns. J Prosthet Dent 79:254–260
Zach L, Cohen G (1965) Pulp response to externally applied heat. Oral Surg Oral Med Oral Pathol 19:515–530
He S, Wang Y, Li X, Hu D (2011) Effectiveness of laser therapy and topical desensitising agents in treating dentine hypersensitivity: a systematic review. J Oral Rehabil 38:348–358
Kolker JL, Vargas MA, Armstrong SR, Dawson DV (2002) Effect of desensitizing agents on dentin permeability and dentin tubule occlusion. J Adhes Dent 4:211–221
Nakabayashi N (1992) Adhesive bonding with 4-META. Oper Dent Suppl 5:125–130
Nakabayashi N, Hiranuma K (2000) Effect of etchant variation on wet and dry dentin bonding primed with 4-META/acetone. Dent Mater 16:274–279
Haghgoo R, Ahmadvand M, Moshaverinia S (2016) Remineralizing effect of topical NovaMin and nano-hydroxyapatite on caries-like lesions in primary teeth. J Contemp Dent Pract 17:645–649
Tschoppe P, Zandim DL, Martus P, Kielbassa AM (2011) Enamel and dentine remineralization by nano-hydroxyapatite toothpastes. J Dent 39:430–437
Funding
This study was supported by the research fund of the Korea Ministry of Trade, Industry, and Energy (10047615), and the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-016R1A6A3A11932897), Republic of Korea.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Oh, S., Gu, Y., Perinpanayagam, H. et al. Dentinal tubule sealing effects of 532-nm diode-pumped solid-state laser, gallic acid/Fe3+ complex, and three commercial dentin desensitizers. Lasers Med Sci 33, 1237–1244 (2018). https://doi.org/10.1007/s10103-018-2464-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-018-2464-2