Abstract
This study aimed to evaluate the fluoride uptake of dentine treated with a 38 % silver diamine fluoride (SDF) solution and laser irradiation at sub-ablative energy levels. Fifteen human dentine slices were prepared and divided into four samples each. Four types of laser were chosen: CO2 (10,600 nm), Er:YAG (2,940 nm), Nd:YAG (1,064 nm) and Diode (810 nm). First, the four samples from 12 of the dentine slices were treated with SDF, and then irradiated by one of the four types of laser at three different settings. One sample was untreated and acted as a control. The setting that rendered the highest fluoride uptake was selected. Second, the remaining dentine slices were treated with SDF and irradiated by the four lasers with the selected settings. Fluoride uptake was assessed using Energy Dispersive X-ray Spectrometry at the dentine surface and up to 20 μm below the surface. The selected settings were CO2 irradiation at 1.0 W for 1 s, Er:YAG irradiation at 0.5 W for 20 s, Nd:YAG irradiation at 2.0 W for 1 s and diode irradiation at 3.0 W for 3 s. The fluoride content (weight %) at the dentine surface following CO2, Er:YAG, Nd:YAG and diode irradiation was 6.91 ± 3.15, 4.09 ± 1.19, 3.35 ± 2.29 and 1.73 ± 1.04, respectively. CO2 and Er:YAG irradiation resulted in higher fluoride uptake than Nd:YAG and diode irradiation at all levels (p < 0.05). CO2 laser and Er:YAG laser irradiation rendered higher fluoride uptake in the SDF-treated dentine than Nd:YAG laser and diode laser irradiation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Silver diamine fluoride (SDF) treatment has gained much attention in the past decade due to its simplicity and affordability [1, 2]. Clinical trials have shown that SDF can be used to prevent pit and fissure caries [3] and to arrest coronal caries in the primary [4] and permanent [5] teeth of children. SDF is also used to prevent root caries in the elderly [6]. Laboratory studies have found that SDF prevents dental hard tissues from demineralising due to acid production from biofilms [1, 7, 8] or acid challenge [9, 10]. SDF-treated carious dentine also represented a biologically acceptable pulpal response [11]. However, the calcium fluoride deposits generated during treatment can be dissolved after washing with water [10, 12], and an increase in the fluoride concentration in saliva is evident within 12 h of the topical application of fluoride [13]. Therefore, methods are required to increase the fluoride uptake to improve the long-term effectiveness of the treatment.
Topical fluoride therapy is often performed on exposed dentine for caries prevention [14]. Studies have shown that dentine becomes more acid resistant if its fluoride content is increased [15, 16]. However, the amount of fluoride taken up is low and limited to the surface layer [10]. Laser irradiation can be used to promote fluoride uptake by dental hard tissue. Bahar and his co-workers reported neodymium-doped yttrium aluminium garnet (Nd:YAG) laser irradiation to be effective in increasing fluoride uptake into the pit and fissure enamel [17]. Another study found that CO2 promotes the fluoride uptake of enamel treated with sodium fluoride [18]. The use of a diode laser has been shown to increase the fluoride uptake of enamel and to protect the enamel surface from acid attack [19]. An erbium-doped yttrium aluminium garnet (Er:YAG) laser was also found to increase the fluoride uptake of enamel treated with acidulated phosphate fluoride gel [20]. Following laser treatment, fluoride is not only deposited on the enamel and dentine but is also incorporated into the enamel and dentine crystalline structure [18, 21].
At present, there are no standardised parameters for the use of lasers for the prevention of dental caries in dentine. Even manufacturers often do not provide guidelines for the use of their dental laser products for caries prevention. Moreover, a literature search in PubMed found no studies comparing the effect of different types of laser on the fluoride uptake of SDF-treated dentine for caries prevention. Thus, the objective of the study was to compare the fluoride uptake of 38 % SDF-treated dentine using four common dental laser irradiations at sub-ablative energy levels.
Materials and methods
Sample preparation
This study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (UW08-052). A flow chart of the study is shown in Fig. 1. Extracted sound human molars were collected with the patients’ consent. One section is taken from one tooth and the dentine is taken from the crown. Fifteen 3-mm-thick dentine slices were prepared from the molars. The surfaces of the slices were polished using micro-fine 4,000-grid sanding paper. The polished slices were examined using a stereomicroscope to exclude samples with cracks, hypoplasia or white spot lesions. The examined slices were treated with 1 % citric acid for 1 min and ultrasonically washed with deionised water to eliminate the smear layer. After autoclaving, each slice was divided into four parts or samples for different treatments; thus, 60 samples were prepared from 15 dentine slices. There were two parts to the experiment. In the first part, 48 samples from 12 of the dentine slices were used to study the fluoride uptake of 38 % SDF-treated dentine using four common dental laser irradiations at sub-ablative energy levels. In the second part, 12 samples from the remaining three dentine slices were used to compare the fluoride uptake of 38 % SDF-treated dentine by the four laser irradiations.
Part 1—determining the best settings for the four dental laser irradiations
A 38 % (w/v) SDF solution (Saforide; Toyo Seiyaku Kasei Co. Ltd., Osaka, Japan) was topically applied to the specimens using a micro-brush (Micro applicator—regular, Premium Plus International Ltd., Hong Kong, China). The mean (±SD) amount of SDF applied was 0.22 ± 0.07 mg (or 8.8 ± 2.8-μg fluoride), estimated by calculating the difference in the gravimetric micro-brush before and after application. The specimens were gently blown dry with a 3-in-1 syringe. Sub-ablative low-energy laser irradiation was then applied to the surface of the specimens. Four common types of laser used in dentistry, namely, CO2, Er:YAG, Nd:YAG and diode, were assessed. A CYMA dental laser (Bison Medical Co., Seoul, South Korea) was used to deliver the CO2 laser (10,600 nm); a Fidelis Plus III dental laser (Fotona Co., Ljubljana, Slovenia) was used to deliver the Er:YAG laser (2,940 nm); a Fidelis Plus III dental laser (Fotona Co., Ljubljana, Slovenia) was used to deliver the Nd:YAG laser (1,064 nm); and an Elexxion Claros dental laser (Elexxion AG Co., Radolfzell am Bodensee, Germany) was used to deliver the diode laser (810 nm). As no parameters have been specified for the use of these laser machines for fluoride treatment for caries prevention, three parameters at sub-ablative energy levels were chosen for each laser after consultation with the manufacturers. The output energy of the laser was validated by a laser power metre (Nova Handheld Laser Power Meter, Ophir Optronics, Utah, USA). Three samples from each dentine slice received the laser irradiation at the three selected settings, and deionised water was applied to the remaining sample as a control (Table 1).
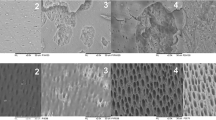
After the application of SDF followed by laser irradiation, the samples were sectioned vertically for assessment. The fluoride uptake of the samples was examined using energy dispersive X-ray spectrometry (EDX) under scanning electron microscopy (SEM) (Hitachi S-4800 FEG Scanning Electron Microscope, Hitachi Ltd., Tokyo, Japan). An elemental assessment was performed by measuring five areas 5 × 5 μm2 at the surface and at 5, 10, 15 and 20 μm below the surface [22]. The mean weight percentage of fluoride uptake was calculated. The setting with the highest fluoride uptake was chosen as the selected parameter [23].
Part 2—comparison of the fluoride uptake of dentine treated by different dental lasers
Twelve samples from three dentine slices were prepared and treated with a 38 % SDF solution, as described for experiment 1. The four samples from each dentine slice received CO2 irradiation (group 1), Er:YAG irradiation (group 2), Nd:YAG irradiation (group 3) and diode irradiation (group 4), respectively, using the best parameters obtained in the first experiment. The samples were sectioned vertically for elemental assessment. The fluoride uptake of dentine was conducted using EDX under SEM. Elemental assessment was performed by measuring five areas 5 × 5 μm2 at the surface and at 5, 10, 15 and 20 μm from the surface. The five areas were randomly selected. The mean weight percentage of fluoride uptake was calculated.
Statistical analyses
The Shapiro–Wilk test of normality (p > 0.05) was used to assess whether the data had a normal distribution. A separate two-way mixed model analysis of variance was used to compare the mean weight percentage of fluoride among the groups and the mean weight percentage of fluoride among each treatment among the five depths, with sample as a random effect. All of the analyses were conducted using IBM SPSS Version 2.0 software (IBM Corporation, Armonk, New York, USA). The cut-off level of significance was taken as 5 % for all of the analyses.
Results
Part 1—determining the best settings for the four dental laser irradiations
The weight percentages of fluoride uptake at different depths of dentine using different settings for the CO2, Er:YAG, Nd:YAG and diode lasers are summarised in Table 2. The fluoride uptake of dentine using setting P3 was significantly higher at all depths than for other settings after CO2, Nd:YAG and diode laser irradiation. The fluoride uptake of dentine using setting P1 was significantly higher at all depths than for other settings after Er:YAG laser irradiation. Therefore, the selected parameters for the second experiment were 1.0 W, 50 Hz, 8 ms pulse for the CO2 laser; 0.5 W, 10 Hz, 1 ms pulse for the Er:YAG laser; 2.0 W, 10 Hz, 0.2 ms pulse for the Nd:YAG laser; and 3.0 W continuous wave for the diode laser.
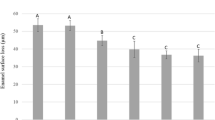
Part 2—comparison of the fluoride uptake of dentine treated by different dental lasers
The weight percentages of fluoride uptake at different depths of dentine after CO2, Er:YAG,Nd:YAG and diode laser irradiation are summarised in Table 3. The results demonstrate that the CO2 laser, followed by the Er:YAG laser, resulted in a higher fluoride uptake at all depths (p < 0.05) than the Nd:YAG and diode lasers. No significant difference in weight percentages of fluoride were detected among different depth in Er:YAG and Nd:YAG groups. While in CO2 and Diode groups, weight percentages of fluoride at 5 μm seemed to be higher than some other levels.
Discussion
Various studies have suggested that laser irradiation promotes fluoride uptake and prevents caries [14–16]. However, there are currently no standardised parameters for the use of laser irradiation with fluoride agents for the prevention of dental caries. Even the manufacturers of the laser machines used in this study did not provide clear guidelines for the use of their dental laser products for caries prevention. This study provides useful information to help dentists select the best laser types and parameters to promote fluoride uptake in exposed dentine, which is at risk of developing root caries. The use of different lasers in combination with fluoride has been shown to have a synergistic effect on the prevention of caries by increasing fluoride uptake in the enamel or root surface [20–23]. Laser-tissue interactions are mainly controlled by laser parameters such as the wavelength, energy density, pulse duration, exposure time, emission mode and repetition rate [24]. However, these factors vary across laser types, and different studies have used different parameters for the same type of laser. Therefore, it is important to develop a set of guidelines on the best laser parameters to use for dental caries prevention.
This was an in vitro study, and the experimental conditions were simplified to compare the results with different types of laser. Because the elemental components of teeth vary, four samples from the same dentine slice were allocated to the four experimental groups in the first and second parts of the experiment to allow the comparison of the results among groups [23]. Therefore, the percentages for fluoride content in Table 2 are somewhat different from those at the same depth and same settings in Table 3 due to different specimens. Furthermore, the variation within a dentine slice was small because of the small standard deviation. It should be noted that fluoride uptake is only one of the factors that influences the prevention effect, and the parameters chosen were regulated by the available settings of the laser machines used in the study. We measured both loosely bound and firmly bound fluoride, and we did not wash the slices after the laser irradiation. Previous study suggested that laser treatment seemed to be more effective in enhancing loosely bound fluoride uptake in the dentine than in enamel due to its porous surface [21]. In addition, accuracy of EDX spectrum can be affected by nature of the samples and amount and density of materials. Inhomogeneous and rough samples could also adversely affect accuracy. Furthermore, there could be variations among the areas even within the same slice and this is considered a limitation of and discussed in this study. Therefore, caution should be exercised in the interpretation of the results.
Higher-energy laser treatment has been used to melt dental tissue and seal the dental surface for caries prevention [22, 25]. However, clinicians are concerned that high-powered lasers may potentially damage gingival or pulpal tissues. Therefore, we used a sub-ablative energy laser to treat the dentine tissues in this study. SEM observation confirmed that the laser-treated dentine surface suffered no ablation (data not shown). Sub-ablative energy has been shown to have an organic blocking effect in caries prevention, in contrast to the inorganic blocking caused by high-energy laser therapy [24, 26]. Some study indicates even that when a sub-ablative energy was used, Er,Cr:YSGG laser can alter the micro-structure of radicular dentine [27]; future study may investigate the effect of alteration in micro-structure on surface roughness changes. To choose an appropriate irradiation condition for each laser, the effects of different wavelengths on certain components of the target tissue must be considered. CO2 and Er:YAG lasers are both absorbed in water and hydroxyapatite. Nd:YAG and diode lasers exhibit high absorption peaks for coloured tissue such as melanin and haemoglobin, but have limited interactions with water and hydroxyapatite [28]. The laser machines used in this study had different sized laser beams, which could not be standardised. The diameter of the laser beam, whether delivered in contact or non-contact with the tissue, creates a certain energy density: the smaller the beam, the greater the energy density. Thus, the use of a small spot greatly increases thermal transfer from the laser to the tissue, with a corresponding increase in absorption due to heating a small area. The amount of time that the beam is allowed to strike the target tissue affects the rate at which the tissue temperature increases. The time can also be regulated by the repetition rate of the pulsed laser emission mode [27]. Therefore, the settings selected in part 1 were based on the characteristic properties of each laser. Selecting an energy level that would not cause thermal damage to the pulp and periodontal tissues was an important consideration, and we also referred to related studies and asked the manufacturers for advice.
A previous study showed that the depth of fluoride penetration was within 20 μm of the root surface after laser treatment [22]. We therefore chose to measure fluoride uptake up to 20 μm below the dentine surface. The results showed that the fluoride uptake in the samples treated by the CO2 and Er:YAG lasers was higher than that in the samples treated by the Nd:YAG and diode lasers at all depths measured. Previous studies have suggested several general mechanisms. Heat has been found to enhance the uptake of fluoride to form fluoride apatite, and the thermal effect of the laser was speculated to be the main factor in promoting fluoride uptake [18]. Another possible mechanism may be the laser-induced alteration of the surface. Surface changes such as an increase in cracks and roughness may play a role in increasing the fluoride uptake [22]. A recent study indicated that sub-ablative low-energy laser irradiation following fluoride treatment increased fluoride deposition and transformed hydroxyapatite into fluoridated hydroxyapatite [24]. However, the exact mechanism is not known. It is noticeable that the fluoride uptake of the dentine after SDF treatment without laser irrigation (represented by the values in control group) might also account for the variation in fluoride uptake across the different dentine slices in different treated areas of the slices.
The different tissues targeted by different types of laser also play an important role in the fluoride uptake effect. Each laser wavelength affects the interrelated components of the target tissue, such as the water content, chemical composition, vascularity and colour. The CO2 and Er:YAG lasers have relatively long wavelengths that are readily absorbed by water and hydroxyapatite, and thus, minimal energy is transmitted to the adjacent tissues. In contrast, light in the visible and near-infrared spectrum is negligibly absorbed and moderately scattered by enamel and dentine. The Nd:YAG and diode lasers are so-called colour dependency lasers that mainly interact with coloured tissues such as melanin, and are only slightly absorbed by water. As human dentine is a light-coloured tissue, dentine may not interact with these two lasers as effectively as with the CO2 and Er:YAG lasers. In addition, although SDF can cause the staining of dentine, the effect is not significant on sound dentine. Although staining can occur, it takes a while for SDF to darken the tissue after application. This may be one of the reasons why SDF was found to be less effective than black ink in enhancing the absorption of Nd:YAG laser energy [25].
Conclusion
Among the four commercially available dental lasers assessed in this study, the CO2 and Er:YAG lasers resulted in a higher fluoride uptake in the SDF-treated dentine than the Nd:YAG and diode lasers.
References
Mei ML, Li QL, Chu CH, Lo EC, Samaranayake LP (2013) Antibacterial effects of silver diamine fluoride on multi-species cariogenic biofilm on caries. Ann Clin Microbiol Antimicrob 12:4
Chu CH, Lo EC (2008) Promoting caries arrest in children with silver diamine fluoride: a review. Oral Health Prev Dent 6:315–321
Liu BY, Lo EC, Chu CH, Lin HC (2012) Randomized trial on fluorides and sealants for fissure caries prevention. J Dent Res 91:753–758
Chu CH, Lo EC, Lin HC (2002) Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res 81:767–770
Llodra JC, Rodriguez A, Ferrer B, Menardia V, Ramos T, Morato M (2005) Efficacy of silver diamine fluoride for caries reduction in primary teeth and first permanent molars of schoolchildren: 36-month clinical trial. J Dent Res 84:721–724
Tan HP, Lo EC, Dyson JE, Luo Y, Corbet EF (2010) A randomized trial on root caries prevention in elders. J Dent Res 89:1086–1090
Chu CH, Mei L, Seneviratne CJ, Lo EC (2012) Effects of silver diamine fluoride on dentine carious lesions induced by Streptococcus mutans and Actinomyces naeslundii biofilms. Int J Paediatr Dent 22:2–10
Mei ML, Chu CH, Low KH, Che CM, Lo EC (2013) Caries arresting effect of silver diamine fluoride on dentine carious lesion with S. mutans and L. acidophilus dual-species cariogenic biofilm. Med Oral Patol Oral Cir Bucal 18:e824–e831
Liu BY, Lo EC, Li CM (2012) Effect of silver and fluoride ions on enamel demineralization: a quantitative study using micro-computed tomography. Aust Dent J 257:65–70
Mei ML, Ito L, Cao Y, Li QL, Lo EC, Chu CH (2013) Inhibitory effect of silver diamine fluoride on dentine demineralisation and collagen degradation. J Dent 41:809–817
Gotjamanos T (1996) Pulp response in primary teeth with deep residual caries treated with silver fluoride and glass ionomer cement (‘atraumatic’ technique). Aust Dent J 41:328–334
Lou YL, Botelho MG, Darvell BW (2011) Reaction of silver diamine [corrected] fluoride with hydroxyapatite and protein. J Dent 39:612–618
Lambrou D, Larsen MJ, Fejerskov O, Tachos B (1981) The effect of fluoride in saliva on remineralization of dental enamel in humans. Caries Res 15:341–345
Chu CH, Mei ML, Lo EC (2010) Use of fluorides in dental caries management. Gen Dent 58:37–43
Iijima Y, Ruben JL, Zuidgeest TG, Arends J (1993) Fluoride and mineral content in hyper-remineralized coronal bovine dentine in vitro after an acid challenge. Caries Res 27:106–110
Mukai Y, Lagerweij MD, ten Cate JM (2001) Effect of a solution with high fluoride concentration on remineralization of shallow and deep root surface caries in vitro. Caries Res 35:317–324
Bahar A, Tagomori S (1994) The effect of normal pulsed Nd-YAG laser irradiation on pits and fissures in human teeth. Caries Res 28:460–467
Hsu SCY, Gao XL, Pang JS, Wefel JS (2004) Effects of CO2 laser on fluoride uptake in enamel. J Dent 32:161–167
Vitale MC, Zaffe D, Botticell AR, Caprioglio C (2011) Diode laser irradiation and fluoride uptake in human teeth. Eur Arch Paediatr Dent 12:90–92
Bevilacqua FM, Zezell DM, Magnani R, da Ana PA, Eduardo Cde P (2008) Fluoride uptake and acid resistance of enamel irradiated with Er: YAG laser. Lasers Med Sci 23:141–147
Gao XL, Pan JS, Hsu CY (2006) Laser-fluoride effect on root demineralization. J Dent Res 85:919–923
Zhang C, Kimura Y, Matsumoto K (1996) The effects of pulsed Nd: YAG laser irradiation with fluoride on root surface. J Clin Laser Med Surg 14:399–403
Mei ML, Ito L, Chu CH, Lo EC, Zhang CF (2013) Prevention of dentine caries using silver diamine fluoride application followed by Er: YAG laser irradiation: an in vitro study. Lasers Med Sci. doi:10.1007/s10103-013-1329-y
Liu Y, Hsu CY, Teo CM, Teoh SH (2013) Subablative Er: YAG laser effect on enamel demineralization. Caries Res 47:63–68
Zhang C, Kimura Y, Matsumoto K, Harashima T, Zhou H (1998) Effects of pulsed Nd: YAG laser irradiation on root canal wall dentin with different laser initiators. J Endod 24:352–355
Hsu CY, Jordan TH, Dederich DN, Wefel JS (2000) Effects of low-energy CO2 laser irradiation and the organic matrix on inhibition of enamel demineralization. J Dent Res 79:1725–1730
Botta SB, Ana PA, de Sa Teixeira F, da Silveira Salvadori MC, Matos AB (2011) Relationship between surface topography and energy density distribution of Er, Cr:YSGG beam on irradiated dentin: an atomic force microscopy study. Photomed Laser Surg 29:261–269
Convissar RA (2010) Laser-asssisted nonsurgical periodontal therapy In: Convissar RA (ed) Principles and practice of laser dentisty p 28
Acknowledgments
This study was supported by the General Research Fund (HKU765111M) of the Research Grants Council, Hong Kong.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mei, M.L., Ito, L., Zhang, C.F. et al. Effect of laser irradiation on the fluoride uptake of silver diamine fluoride treated dentine. Lasers Med Sci 30, 985–991 (2015). https://doi.org/10.1007/s10103-014-1521-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-014-1521-8