Abstract
The aims of this study were to compare the clinical and microbiological characteristics from patients with polymicrobial bloodstream infections (BSI) to those from patients with monomicrobial BSI and to determine their influence on the prognosis. A prospective study was conducted on 371 nosocomial BSI in an intensive care unit (ICU). Seventy-five (20.2%) of them were polymicrobial. The mean APACHE II score at the onset of bacteremia in polymicrobial and monomicrobial BSI were 17.7 ± 6.6 and 18.9 ± 7.5, respectively (p = 0.228). Severe sepsis and septic shock were present in 68.0% and 50.6% of polymicrobial BSI and in 73.9% and 55.1% of monomicrobial BSI, respectively (p = 0.298 and p = 0.494, respectively). The length of stay and the length of stay post-infection were significantly longer in patients with polymicrobial BSI. APACHE II score at the onset of BSI, high-risk microorganisms, and septic shock were predictors of related mortality, but polymicrobial BSI and inadequate empirical antimicrobial treatment were not. Our findings suggest that the clinical and microbiological characteristics of polymicrobial BSI are not different from monomicrobial BSI, and polymicrobial BSI do not have any influence on the related mortality. However, they occurred in patients with a longer length of stay in the hospital and were associated with longer stays in the hospital after the episode of BSI.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Nosocomial bloodstream infections (BSI) are among the most frequent and severe infections in intensive care unit (ICU) patients, especially in those with severe sepsis and septic shock [1–4]. A great majority of polymicrobial BSI have a nosocomial origin, but the proportion of polymicrobial BSI in series of nosocomial infections in critical ill patients are relatively low [5, 6] and recent studies on these infections are scarce [7]. The differences in the clinical and microbiological features between monomicrobial and polymicrobial BSI in critically ill patients are not well established, and, most importantly, their impact on the prognosis remains unclear [8].
The aims of this study were: (1) to ascertain the clinical and microbiological characteristics of polymicrobial nosocomial BSI in an ICU, in comparison with hospital-acquired monomicrobial bacteremias and (2) to determine their influence on global and related mortality in hospital and on the length of stay.
Materials and methods
Study location and patients
The study was carried out in a university-affiliated urban teaching hospital with 600 beds: Hospital Universitario Dr. Peset in Valencia, Spain. During a period of 136 months (October 1998 to February 2010), all adult medical-surgical ICU patients with nosocomial-acquired bloodstream infection were prospectively analyzed.
Study design
A prospective cohort study was used. Its characteristics have been previously described [9]. We collected demographic, clinical, microbiological, hospital course, and outcome data. Patients were segregated according to the polymicrobial origin of bacteremia and hospital survival. Hospital-related mortality was the main outcome variable evaluated.
Definitions
A bacteremia was classified as nosocomial-acquired if the first positive blood culture occurred >48 h after hospital admission [10]. Each positive blood culture was categorized as either clinically significant or contaminant, taking into account organism identification, clinical signs and symptoms, number of positive blood cultures out of the total number drawn, results of other cultures, pathology findings, imaging results, and clinical course [11]. Organisms that are commonly recovered from the environment or the skin were judged to be contaminants, unless the clinical findings, the results of cultures of material from other body sites, and the number of positive sets (two or more) indicated a high probability of bloodstream infection [12]. Bacteremias considered as clinically nonsignificant or contaminants were excluded. Bacteremias were considered as polymicrobial when two or more microorganisms were isolated in the same set of blood cultures.
Sepsis, severe sepsis, septic shock, and multiple organ dysfunction syndrome were defined using established criteria [13]. A modified McCabe classification [14] was used to place the patients' underlying disease in the following categories: rapidly fatal, ultimately fatal, and nonfatal. Nosocomial BSI were defined according to criteria established by the Centers for Disease Control and Prevention (CDC) [15]. Respiratory and abdominal sources of bacteremia were considered as risk foci of infection, because these foci were associated with a higher mortality compared to other sources of bacteremia [5, 10]. Enterobacteriaceae other than Escherichia coli, Pseudomonas aeruginosa, and Candida spp. were considered to be high-risk microorganisms, due to having been reported to cause high mortality [5, 16].
Inappropriate empirical antimicrobial treatment (IEAT) was considered as the occurrence of bloodstream infection that was not effectively treated at the time when the causative microorganism and its antibiotic susceptibility were known, including the absence of antimicrobial agents directed at a specific class of microorganisms and the administration of an antimicrobial agent to which the microorganism responsible for the infection was resistant [9]. Mortality related to a bloodstream infection was predetermined to be present when a patient died during treatment for a nosocomial bloodstream infection and death could not be directly attributed to any other cause [17].
Statistical analyses
The χ2 test was used to compare categorical variables. Continuous variables were compared using Student’s t-test for normally distributed variables and the Wilcoxon rank-sum test for non-normally distributed variables. Variables with a p-value ≤ 0.05 and a plausible biological relationship to the dependent outcome variable were further analyzed with a nonconditional multivariate analysis in order to determine the independent factors associated with hospital mortality. The results of the logistic regression analyses are reported as adjusted odds ratios with 95% confidence intervals. SPSS 15.0 software was used for the data analysis.
Results
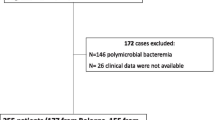
During the study period, 12,742 consecutive eligible patients were evaluated. There were 509 episodes of ICU bacteremia; among these, 371 bacteremias (72.88%) were nosocomial and 75 (20.2% of nosocomial bacteremias) were polymicrobial. The epidemiological and clinical characteristics of the 371 nosocomial bacteremias according to the polymicrobial or monomicrobial infection are shown in Table 1. In two groups (polymicrobial and monomicrobial bacteremias), there were no differences in age, sex, underlying disease (chronic respiratory disease, diabetes mellitus, liver cirrhosis, neoplasia), APACHE II score at admission and at onset, the presence of severe sepsis, septic shock and multiorgan failure, and inadequate empirical antibiotic treatment. Length of stay in the ICU, length of stay in the ICU pre-infection, and length of stay in the ICU post-infection, days on mechanical ventilation, and the presence of high-risk microorganisms in blood cultures were significantly more frequent in the polymicrobial bacteremias group in the univariate analysis, whereas global mortality was more frequent in the monomicrobial bacteremias group (49.3% vs. 61.8%, p = 0.049); there were no differences between the two groups.
The most common sources of polymicrobial bacteremias were respiratory (45.3%), unknown (24%), catheter-related (20%), and intra-abdominal (4%), without significant differences among monomicrobial bacteremias (Fig. 1). The systemic response in this group was classified as severe sepsis in 51 episodes (68.0%) and septic shock in 38 episodes (50.6%), with multiorgan failure in 50.6% of the cases.
A total of 154 microorganisms were isolated in the 75 episodes of polymicrobial bacteremia. The pathogens are listed in Table 2. There were 63 episodes with two microorganisms and 12 episodes with three microorganisms isolated. The microorganisms most frequently isolated in polymicrobial bacteremias were Acinetobacter baumannii in 34 episodes (45.3%), Enterococcus spp. in 32 episodes (42.7%), coagulase-negative staphylococci (CNS) in 23 episodes (30.7%), Staphylococcus aureus in 15 episodes (20.0%), and Pseudomonas aeruginosa in 12 episodes (16.0%), whereas in monomicrobial bacteremias, the microorganisms most frequently isolated were Acinetobacter baumannii (25.0%), Staphylococcus aureus (14.5%), CNS (14.5%), Enterococcus spp. (10.5%), Candida spp. (9.8%), and Escherichia coli (5.7%).
Acinetobacter baumannii, Enterococcus spp., Pseudomonas aeruginosa, CNS, and Klebsiella pneumoniae were statistically more prevalent in the polymicrobial group by univariate analysis. The more frequent microorganism associations were A. baumannii + Enterococcus spp. (n = 10, 13.15%), Enterococcus spp. + CNS (n = 7, 9.21%), and A. baumannii + S. aureus (n = 4, 5.26%).
Multivariate analysis demonstrated that the APACHE II score at onset, the presence of septic shock, and the isolates in cultures of high-risk microorganisms were independent factors associated with related mortality, but not polymicrobial bacteremia (Table 3).
Discussion
In our study, we found that over one-fifth of patients with nosocomial bacteremias were polymicrobial. This high figure points to the importance of polymicrobial BSI in ICUs. However, despite the clinical importance of polymicrobial BSI, studies on this subject are scarce and quite old [7, 18–22].
The clinical characteristics of our patients were similar to those previously described in other studies [19–21, 23]: a mean age of about 60 years, a higher proportion of men than women, frequent comorbidities, and diabetes mellitus being the most prevalent disease. We could not identify any clinical or epidemiological factor related to polymicrobial bacteremia in comparison with monomicrobial bacteremia. Few studies provided comparative data with monomicrobial bacteremias; Rello et al. [7] did so in intensive care patients without finding any predictor of polymicrobial bacteremia.
The length of stay in the hospital was longer in patients who developed nosocomial polymicrobial BSI compared to patients with monomicrobial BSI. As far as we know, there were no previous works which describe this finding. Interestingly, the length of stay, in both the ICU and in the hospital, after the episode of BSI was significantly longer in patients with polymicrobial BSI compared to monomicrobial BSI, which suggests a higher severity of polymicrobial BSI, not only in medical terms but also in cost.
It is widely accepted that intra-abdominal infections are the most frequent origin of polymicrobial bacteremias [5, 18, 22, 24]; however, in our series, abdominal origin was found in only 4% of cases. This could be due to the small number of surgical patients admitted in our critical care unit. The sources of infection more frequently described in BSI are lower respiratory tract and unknown focus [24–26], in accordance with our results.
Nosocomial origin infections are caused frequently by Gram-negative bacilli [25], in the same way that polymicrobial bacteremias are [19, 22]. In recent years, there has been a shift in favor of Gram-positive organisms in BSI, and, even in some countries, its prevalence has overcome Gram-negative organisms [27–29]. We found that Gram-positive microorganisms caused 52.3% of polymicrobial BSI, probably due to a high prevalence of Enterococcus spp. and CNS from catheter and unknown origins in our setting. A. baumannii was the most prevalent microorganisms in both polymicrobial BSI (45.3%) and monomicrobial (25.0%) BSI. This high incidence of A. baumannii was due to a carbapenem-resistant outbreak in our ICU during the period of the study [9].
BSI have a high mortality in the ICU, 35–60%, in severe sepsis and septic shock [6, 30, 31]. There is no consensus on whether polymicrobial BSI is a risk factor of mortality. Several studies have found a positive relationship between polymicrobial BSI [19, 32] and mortality in patients admitted and not admitted to the ICU, whereas Rello et al. [7] found no association in critical care patients. We found a lower global mortality in polymicrobial BSI. This low rate of mortality in polymicrobial BSI might be due to a significantly higher rate of CNS and Enterococcus spp. in these cases. However, this association was lost when we analyzed the related mortality.
The APACHE II score at the onset of bacteremia, septic shock, and high-risk microorganisms were all independent predictive factors of related mortality. On the other hand, no significant differences were found between IEAT and related mortality. These results are in contrast to findings in previous studies which found that IEAT was a predictor of mortality in community-acquired and nosocomial BSI [24, 33, 34]. But, however, these results did support previous findings in a study carried out by our group [9]. Related infection mortality was neither related to respiratory nor abdominal foci (high risk foci of mortality) nor polymicrobial BSI.
This study has some limitations. First, the data are from a single academic center, limiting its generalizability to other centers and settings. Second, despite the fact that stringent criteria were applied to each case of BSI caused by CNS, it is possible that some of our cases of polymicrobial BSI were monomicrobial, with CNS present as a contaminant. Third, the design of our study precluded us from collecting information about the time to antibiotic administration, which has been associated with better outcomes. Fourth, because the length of stay in the ICU and hospital is dependent on many factors, it is possible that some confounding variables were not analyzed. Our findings, however, provide significant information about the clinical and microbiological characteristics and prognosis of polymicrobial BSI in critically ill patients.
In summary, nosocomial polymicrobial bacteremias in intensive care represent a small but significant proportion of nosocomial BSI. They occur in patients with long-term hospitalization and are related to longer stays in the ICU and in the hospital compared to monomicrobial BSI. However, they were neither frequently IEAT nor did they have any influence on the mortality.
References
Balk RA (1994) Septic shock: pathophysiology. Curr Opin Anaesthesiol 7:136–140
Bone RC (1991) The pathogenesis of sepsis. Ann Intern Med 115:457–469
Bone RC (1991) Gram-negative sepsis. Background, clinical features, and intervention. Chest 100:802–808
Zaragoza R, Artero A, Borras S, Camarena JJ, González R, Nogueira JM (2001) Intensive care unit bacteremias and septic shock. Analysis of clinical and microbiological features and risk factors. Intensive Care Med 27(Suppl 2):S236
Vallés J, León C, Alvarez-Lerma F (1997) Nosocomial bacteremia in critically ill patients: a multicenter study evaluating epidemiology and prognosis. Spanish Collaborative Group for Infections in Intensive Care Units of Sociedad Española de Medicina Intensiva y Unidades Coronarias (SEMIUC). Clin Infect Dis 24:387–395
Laupland KB, Zygun DA, Davies HD, Church DL, Louie TJ, Doig CJ (2002) Population-based assessment of intensive care unit-acquired bloodstream infections in adults: Incidence, risk factors, and associated mortality rate. Crit Care Med 30:2462–2467
Rello J, Quintana E, Mirelis B, Gurguí M, Net A, Prats G (1993) Polymicrobial bacteremia in critically ill patients. Intensive Care Med 19:22–25
McKenzie FE (2006) Case mortality in polymicrobial bloodstream infections. J Clin Epidemiol 59(7):760–761
Zaragoza R, Artero A, Camarena JJ, Sancho S, González R, Nogueira JM (2003) The influence of inadequate empirical antimicrobial treatment on patients with bloodstream infections in an intensive care unit. Clin Microbiol Infect 9:412–418
Rello J, Ricart M, Mirelis B, Quintana E, Gurguí M, Net A, Prats G (1994) Nosocomial bacteremia in a medical-surgical intensive care unit: epidemiologic characteristics and factors influencing mortality in 111 episodes. Intensive Care Med 20(2):94–98
Diekema DJ, Beekmann SE, Chapin KC, Morel KA, Munson E, Doern GV (2003) Epidemiology and outcome of nosocomial and community-onset bloodstream infection. J Clin Microbiol 41:3655–3660
Leibovici L, Shraga I, Drucker M, Konigsberger H, Samra Z, Pitlik SD (1998) The benefit of appropriate empirical antibiotic treatment in patients with bloodstream infection. J Intern Med 244(5):379–386
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of chest Physicians/Society of Critical Care Medicine. Chest 101:1644–1655
McCabe WR, Jackson GG (1962) Gram negative bacteremia. Arch Intern Med 110:92–100
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1988) CDC definitions for nosocomial infections, 1988. Am J Infect Control 16:128–140
Kollef MH, Sherman G, Ward S, Fraser VJ (1999) Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest 115:462–474
Ibrahim EH, Sherman G, Ward S, Fraser VJ, Kollef MH (2000) The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest 118:146–155
Cooper GS, Havlir DS, Shlaes DM, Salata RA (1990) Polymicrobial bacteremia in the late 1980s: predictors of outcome and review of the literature. Medicine (Baltimore) 69(2):114–123
Kiani D, Quinn EL, Burch KH, Madhavan T, Saravolatz LD, Neblett TR (1979) The increasing importance of polymicrobial bacteremia. JAMA 242:1044–1047
Mackowiak PA, Browne RH, Southern PM Jr, Smith JW (1980) Polymicrobial sepsis: an analysis of 184 cases using log linear models. Am J Med Sci 280:73–80
Roselle GA, Watanakunakorn C (1979) Polymicrobial bacteremia. JAMA 242:2411–2413
Reuben AG, Musher DM, Hamill RJ, Broucke I (1989) Polymicrobial bacteremia: clinical and microbiologic patterns. Rev Infect Dis 11:161–183
Lin JN, Tsai YS, Lai CH, Chen YH, Tsai SS, Lin HL, Huang CK, Lin HH (2009) Risk factors for mortality of bacteremic patients in the emergency department. Acad Emerg Med 16(8):749–755
Vallés J, Rello J, Ochagavía A, Garnacho J, Alcalá MA (2003) Community-acquired bloodstream infection in critically ill adult patients: impact of shock and inappropriate antibiotic therapy on survival. Chest 123:1615–1624
Alberti C, Brun-Buisson C, Burchardi H, Martin C, Goodman S, Artigas A, Sicignano A, Palazzo M, Moreno R, Boulmé R, Lepage E, Le Gall R (2002) Epidemiology of sepsis and infection in ICU patients from an international multicentre cohort study. Intensive Care Med 28:108–121
Boussekey N, Cantrel J, Dorchin Debrabant L, Langlois J, Devos P, Meybeck A, Chiche A, Georges H, Leroy O (2010) Epidemiology, prognosis, and evolution of management of septic shock in a French intensive care unit: a five years survey. Crit Care Res Pract 2010:436427
Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall C, Sakr Y, Reinhart K; EPIC II Group of Investigators (2009) International study of the prevalence and outcomes of infection in intensive care units. JAMA 302:2323–2329
Friedman G, Silva E, Vincent JL (1998) Has the mortality of septic shock changed with time? Crit Care Med 26(12):2078–2086
Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall JR, Payen D; Sepsis Occurrence in Acutely Ill Patients Investigators (2006) Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 34(2):344–353
Gatell JM, Trilla A, Latorre X, Almela M, Mensa J, Moreno A, Miro JM, Martinez JA, Jimenez de Anta MT, Soriano E, Garcia San Miguel J (1988) Nosocomial bacteremia in a large Spanish teaching hospital: analysis of factors influencing prognosis. Rev Infect Dis 10(1):203–210
Vosylius S, Sipylaite J, Ivaskevicius J (2003) Intensive care unit acquired infection: a prevalence and impact on morbidity and mortality. Acta Anaesthesiol Scand 47:1132–1137
Weinstein MP, Reller LB, Murphy JR (1986) Clinical importance of polymicrobial bacteremia. Diagn Microbiol Infect Dis 5(3):185–196
Kollef MH, Ward S, Sherman G, Prentice D, Schaiff R, Huey W, Fraser VJ (2000) Inadequate treatment of nosocomial infections is associated with certain empiric antibiotic choices. Crit Care Med 28:3456–3464
Garnacho-Montero J, Ortiz-Leyba C, Herrera-Melero I, Aldabó-Pallás T, Cayuela-Dominguez A, Marquez-Vacaro JA, Carbajal-Guerrero J, Garcia-Garmendia JL (2008) Mortality and morbidity attributable to inadequate empirical antimicrobial therapy in patients admitted to the ICU with sepsis: a matched cohort study. J Antimicrob Chemother 61:436–441
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sancho, S., Artero, A., Zaragoza, R. et al. Impact of nosocomial polymicrobial bloodstream infections on the outcome in critically ill patients. Eur J Clin Microbiol Infect Dis 31, 1791–1796 (2012). https://doi.org/10.1007/s10096-011-1503-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-011-1503-8