Abstract
Testing for antiphospholipid antibodies could be an important part in determining the cause of a cerebrovascular event (CVE). Currently, it is also unknown whether antiphospholipid antibodies represent a risk factor for the development of a CVE and whether the selected therapy options are efficacious. So, this study aimed at (1) determining the frequency of patients experiencing a CVE and fulfilling the laboratory criterion for an antiphospholipid syndrome (APS), (2) investigating whether the persistent presence of antiphospholipid antibodies represented a risk factor for a CVE, and (3) focusing on the efficacy of the selected treatment strategy in the first year after the CVE. Eighty-nine patients with an acute CVE were prospectively followed for 1 year. At least two sera from each were tested for lupus anticoagulants, anticardiolipin, anti-β2-glycoprotein I, anti-phosphatidylserine/prothrombin and anti-annexin V antibodies. Twenty out of eighty-nine (22%) of CVE patients fulfilled the criteria for APS (17/20 for definitive and 3 for probable APS). There was a significant association between persistently present antiphospholipid antibodies and the CVE (OR, 4.62). No statistically significant difference was found in the CVE recurrence rate between APS-CVE and non-APS-CVE patients being treated mainly with acetyl salicylic acid. Antiphospholipid antibodies represent an independent risk factor for a CVE. In the first year after the CVE, antiplatelet therapy seemed to be sufficient in secondary CVE thromboprophylaxis in most APS patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ischemic cerebrovascular events (CVE) are frequent in patients with underlying vascular risk factors, such as arterial hypertension, hyperlipidemia, diabetes, smoking, and obesity. Nevertheless, in a large proportion of patients, especially younger adults with a CVE, the cause often remains unexplained. In such cases, a more extensive search is mandatory, with an emphasis on structural cardiac or vessel disease, autoimmune diseases, and hypercoagulable states. One among the acquired thrombophilia is an autoimmune disorder, antiphospholipid syndrome (APS), a multi-organ disease, which can also affect the central nervous system, with a stroke, and a transient ischemic attack (TIA) being the most common neurological manifestations [1, 2].
The classification criteria considered “definite APS” is a condition in which at least one of the two major clinical manifestations (i.e., thrombosis or pregnancy morbidity) is met and one of three standardized laboratory assays to detect antiphospholipid antibodies (aPL) is positive, specifically IgG/M anticardiolipin (aCL), anti-β2-glycoprotein I antibodies (aβ2GPI), or lupus anticoagulant (LA) [3]. However, several other autoantibodies, directed at other negatively charged phospholipids and their complexes with protein cofactors, have been proposed to be relevant to APS [4]. Among them are anti-phosphatidylserine/prothrombin (aPS/PT) and anti-annexin V antibodies (aANXV) [5, 6], as well as IgA aCL and IgA aβ2GPI. Such “non-criteria” aPL have not yet been included in the classification criteria of APS, however, they contribute to a “probable APS” [7].
The aim of our study was therefore primarily to determine the frequency of patients experiencing CVE and fulfilling the classification criteria for APS [3] or probable APS. Additionally, we focused on whether the persistent presence of aPL represents a risk factor for experiencing an episode of a CVE. We also aimed at defining the optimal treatment strategy in the first year after a CVE.
Materials and methods
The study was performed as a single-center, prospective follow-up clinical trial. Patients younger than 69 years who had experienced an acute CVE (first or recurrent) were consecutively included. Patients with a known active or newly diagnosed malignant disease were excluded. Eighty-nine patients (male/female, 67/22; mean age, 48 years, ranging from 18 to 67 years) with a CVE were enrolled. They were all followed for 1 year starting immediately after they had been diagnosed by the neurologist at the Department of Neurology, University Medical Centre Ljubljana (UMC-LJ), Slovenia. The diagnoses, based on patient history, clinical manifestations, and an objective verification using computer tomography (CT), magnetic resonance images (MRI), and/or angiography, were set during admission. In the comparative group, patients with other central nervous system diseases were included, namely patients with migraine and Huntington’s disease, all in the chronic phase of their disease. We enrolled 25 patients with migraine without complications (male/female, 5/20; mean age, 40 years, ranging from 18 to 58 years) and 20 patients with Huntington’s disease (male/female, 8/12; mean age, 53 years, ranging from 32 to 67 years). All patients signed an informed consent form before enrolment in the study. The study was conducted within the National Research Programme “Systemic autoimmune diseases” #P3-0314 (funded by the Slovenian Research Agency), with ethical approval #163/02/09, approved by the Slovene National Medical Ethics Committee.
Demographic data on smoking, hypertension, diabetes, the use of oral contraceptives, and an evaluation for additional autoimmune diseases were obtained through the following visits at 3, 6 and 12 months after the CVE and for the comparative patients twice, 3 months apart at the Department of Rheumatology, UMC-LJ. Patients reporting daily smoking at least until the index event were defined as smokers; occasional smokers were classified as non-smokers. Hypertension was defined as a systolic blood pressure of ≥ 160 mmHg, and/or diastolic blood pressure of ≥ 95 mmHg, and/or the use of an antihypertensive medication. Hypercholesterolemia was defined when the serum cholesterol exceeded 5.2 mmol/l at the index event and/or the use of an antihyperlipidemia medication. Blood samples were collected at the index event, 3, 6, and 12 months after the CVE and twice, 3 months apart, for the check-ups. Aliquots of sera were immediately frozen and stored at − 80 °C until analyzed.
Immunoserological testing was performed for different aPL. For LA determination, plasma samples were analyzed according to the guidelines [8] using a coagulation analyzer (BCS Siemens) and reagents (Siemens AG, Munich, Germany) following the manufacturer’s instructions. IgG/IgM/IgA aCL and aβ2GPI were determined by an in-house ELISAs [9, 10]. IgG/IgM anti-phosphatidylserine/prothrombin (aPS/PT) antibodies were determined with an in-house aPS/PT ELISA [11] and IgG/IgM aANXV were measured using an ELISA from Orgentec Diagnostika GmbH, Mainz, Germany, according to the manufacturer’s instructions. The cut-off for all in-house ELISAs was set at the 99th percentile of 220 healthy blood donors.
Patients with a persistent presence (on two or more occasions, at least 12 weeks apart, and for CVE patients 3 months after the CVE) of at least one type of the tested criteria aPL were considered as definite APS. Patients with a persistent presence of other aPL, not included in the APS classification criteria [3], were considered as probable APS.
Statistical analyses were performed using the SPSS 15.0 program. For testing the differences between the CVE and the comparative group, chi-square and Mann-Whitney U tests were performed. A 2-sided probability (p) value of less than 0.05 was considered statistically significant. The multiple logistic regression model was used to test the influence of different risk factors on CVE occurrence. The results were approximated by the odds ratio with its 95% confidence interval (OR [95%]).
Results
Patients’ characteristics
The demographic and clinical characteristics of the patients enrolled are shown in Table 1. We found six patients with an additional autoimmune disease, namely three CVE patients with the disease already identified and treated at the time of the CVE diagnosis (one rheumatoid arthritis, one IgA nephropathy, and one psoriatic arthritis), with the latter patient subsequently fulfilling the classification APS criteria, and three migraine patients (one with rheumatoid arthritis and Sjögren syndrome, one with the Sjögren syndrome, and one with peripheral spondyloarthritis), none of which fulfilled the APS laboratory criteria. Patients with Huntington’s disease had no additional systemic autoimmune disease. Classical cardiovascular thrombotic risk factors were all statistically significantly more common in the CVE group (Table 1).
Antiphospholipid antibodies and CVE
Among 89 CVE patients, 20 (22%) were positive for a particular tested aPL at least twice, with the first testing no earlier than 3 months after the CVE. In this positive group, 17 had the criteria aPL, while three had only non-criteria aPL (the first aCL IgA, the second aANXV IgG, and the last aβ2GPI IgA together with aPS/PT IgM). Only 4/20 of those APS-CVE patients had simultaneously more than one type of aPL present (three patients had a combination of two criteria and one patient the combination of two non-criteria aPL, while there were no triple or more positive patients).
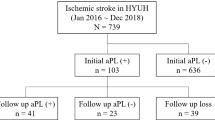
Considering the age of the patients, there was no statistically significant difference in the frequency of CVE-APS patients in the group of those younger and those older than 50 years. Namely, 10/53 (19%) APS-CVE patients were younger and 10/36 (28%) older than 50 years (p = 0.44). Importantly, using the TOAST CVE classification [12] with persistently detected aPL, the cause of the CVE could be consecutively explained in 14/89 (16%) of the CVE patients with the formerly unexplained CVE (Fig. 1).
Classification of cerebrovascular events according to the TOAST classification [9]. APS, antiphospholipid syndrome, definitive and probable; CVE, cerebrovascular event; atherosclerosis, a significant (> 50%) atherosclerotic stenosis or occlusion of the large artery; cardioembolism, an arterial occlusion due to an embolus arising in the heart; lacunar, a small artery occlusion; other etiology, other determined etiology, such as nonatherosclerotic vasculopathies, hypercoagulable states, and hematologic disorders; more causes, when two or more potential causes of stroke present; unknown etiology, despite evaluation, the stroke cause could not be determined
Using a multiple logistic regression model, we found a significant association between hyperlipidemia (OR, 15.23; 95% CI, 4.13–56.15) and arterial hypertension (OR, 4.31; 95% CI, 1.33–13.92), while a significant association was also found between persistently present aPL and the CVE (OR, 4.62; 95% CI, 1.09–19.66).
APS-CVE treatment
Immediately following the CVE, all patients started the treatment with acetyl salicylic acid (together with other medications necessary in secondary stroke prevention according to the guidelines [13]). Anticoagulant therapy was introduced only if so required due to other accompanying diseases or conditions (venous sinus thrombosis, childbirth period, newly confirmed atrial fibrillation, or hereditary thrombophilia). In our study, immediately following the CVE, anticoagulant treatment was indicated in 8/89 (9%) CVE patients, two patients had a CVE and venous sinus thrombosis, two others experienced a CVE in the childbirth period, and in four patients, new atrial fibrillation was confirmed. Later, anticoagulant therapy was introduced in three APS-CVE patients, namely in two patients due to confirmed additional hereditary thrombophilia and in one due to a CVE reoccurrence. All other patients were treated only with acetyl salicylic acid. During this treatment strategy, in the first year of follow-up, we observed no differences in the CVE recurrence frequency between APS-CVE and the non-APS-CVE group (Table 2).
Patients with APS-CVE were divided into two groups, according to the profile of the aPL. We defined them as having a high risk profile, when they were positive at least two times 12 weeks apart for more than one criteria antiphospholipid antibody (LA, aCL IgG/M, aβ2GPI IgG/M) or for LA only (category I and IIa, according to the revised classification criteria [3]). We found 9/20 (45%) APS-CVE patients as having a high-risk profile (six of them with solely LA positivity and no one with triple positivity). The rest 11/20 (55%) patients had a low-risk profile, having a single-criterion antiphospholipid antibody or non-criteria aPL (aCL IgA, aβ2GPI IgA, aPT/PS IgG/M, and/or aANXV IgG/M). In the first year of follow-up, there were 3/11 (27%) patients with a low-risk profile and 1/9 (11%) patients with a high-risk profile aPL, who experienced a CVE recurrence, which was not statistically significantly different (p = 0.591).
Discussion
Antiphospholipid antibodies have been recognized as one of the possible etiological factors for a CVE [14]. In the present study, we found aPL in 20/89 (22%) of CVE patients with 3/20 patients having only non-criteria aPL. The detected frequency is somewhat higher than the recent APS ACTION findings that reported 13.5% of ischemic stroke patients having APS [15]. But it should be considered that a direct comparison among different studies is impossible due to the different study protocols: in some, aPL were tested only once, in some older studies, not all the criteria aPL were tested, while in others, similar to our own, non-criteria aPL were also considered. Additionally, none of the methods for the detection of aPL have been standardized, therefore a considerable degree of interlaboratory variation still remains.
While routine testing for aPL is not recommended in all CVE patients, it comes into consideration in patients with suspected APS or in those with no alternative explanation for the ischemic clinical event, such as atherosclerosis, carotid stenosis, or atrial fibrillation [13, 16]. Importantly, in our group of CVE patients, we confirmed APS in 16% (14/89) of formerly considered to be patients with cryptogenic stroke, six patients were younger and eight APS patients older than 50 years. All these patients had persistently present aPL in intervals and levels, as defined by the APS classification criteria [3]. On the other hand, for non-criteria aPL, their persistent elevation had exceeded the value of the 99th percentile of healthy blood donors. Despite the fact that APS is usually considered as a cause of a CVE in younger patients, there are descriptions of disease onset, as well in the elderly [17]. Similarly to our results, APS should be evaluated within cryptogenic CVE patients of all ages, as a cause of CVE.
Understanding the basics of ASP, it has already been stated that aPL are not only a diagnostic marker for APS but also a risk factor for thrombosis and pregnancy complications [18]. The results of the present study also support the concept that aPL themselves represent an independent risk factor for thrombosis. In accordance with the recent systematic review of Sciascia et al. [15], we similarly found that continuously present aPL increase the risk of a CVE (OR, 4.62).
While a significant association between aPL and CVE is noted, the risk of the recurrence of aPL-associated thrombosis after the first CVE is not well defined [19]. Systematic reviews report that the profile of aPL represents a characteristic risk for further development of APS clinical manifestations. LA were reported to be a stronger risk factor, among the three criteria aPL [20], while some newer data have showed that the risk of thrombosis in solely LA-positive APS patients is low [21]. However, undoubtedly the thrombotic risk increases with the number of positive aPL tests, particularly in patients having all three types of criteria aPL positive (referred to as triple positivity), who are at a higher risk for the occurrence of a thrombotic event [22, 23]. Because of their important causative role in thrombosis, a secondary prevention of further thrombotic events in aPL-positive patients is very important. However, there is a lack of a clear consensus regarding the optimal antithrombotic management of patients with an ischemic stroke/TIA and aPL [18, 24]. The latest AHA/ASA guidelines for the prevention of stroke suggest considering anticoagulant therapy depending on the perception of the risk for recurrent thrombotic events and bleeding in patients with an ischemic stroke or TIA, who meet the criteria for APS. However, in these patients, in whom anticoagulation had not begun, antiplatelet therapy is recommended [13].
In our study, all CVE patients started treatment with acetyl salicylic acid immediately at the time of the CVE, and anticoagulant therapy was introduced only if additional individual patient’s characteristics showed a need. Following such a treatment regimen in the first year after a CVE, we found no statistically significant differences between the frequency of a CVE reoccurrence in the APS-CVE and non-APS-CVE groups (Table 2). That may also be due to the fact that the number of APS-CVE patients with two or more types of aPL was rather low (3/20 patients had a combination of two criteria and one patient the combination of two non-criteria aPL, while there were no triple-positive patients). Regarding these results, in the first year after a CVE or at least until APS confirmation, a secondary CVE prevention strategy with the focus on antiplatelet therapy together with the control of other risk factors (e.g., strict control of classical cardiovascular risk factors and thromboprophylaxis with low molecular weight heparin in high-risk situations for thrombosis) seems to be sufficient.
Possible limitations of our study are certainly a relatively small number of patients and only a 1 year systematic follow-up of the CVE patients. However, although the risk of a stroke reoccurrence remains high for several years, it is the highest in the first year after the first CVE [25]. Additionally, according to our clinical experience and considering the results of previous studies [26], as well as the mechanism of drug action [27], it seems reasonable to modulate treatment decisions during a careful follow-up of APS patients. There is a need to fortify the secondary thromboprophylaxis in APS-CVE patients when (1) they experience a new CVE or other vascular thrombotic event, (2) they have a high-risk profile of aPL (especially in triple positivity), or (3) in clinically asymptomatic patients, when new ischemic lesions are seen with a control brain MRI 1 year after the index event, despite regular antiplatelet therapy. In such cases, a treatment strategy with a combination of moderate-intensity warfarin (INR, 2–3) with acetyl salicylic acid should be considered.
In conclusion, persistently present aPL, as required to fulfill the APS criteria, are one of the possible etiologic factors for a CVE. They also seem to increase the risk for a CVE at least fourfold. Therefore, they should be examined, both for determining the cause of the CVE, especially in patients with a CVE of unknown etiology, as well as for providing further optimal treatment decisions.
References
Brey RL (2000) Differential diagnosis of central nervous system manifestations of the antiphospholipid antibody syndrome. J Autoimmun 15:133–138. https://doi.org/10.1006/jaut.2000.0426
Shi H, Teng JL, Sun Y, Wu XY, Hu QY, Liu HL, Cheng XB, Yin YF, Ye JN, Chen PP, Yang CD (2017) Clinical characteristics and laboratory findings of 252 Chinese patients with anti-phospholipid syndrome: comparison with euro-phospholipid cohort. Clin Rheumatol 36:599–608. https://doi.org/10.1007/s10067-017-3549-1
Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, Derksen RH, DE Groot PG, Koike T, Meroni PL, Reber G, Shoenfeld Y, Tincani A, Vlachoyiannopoulos PG, Krilis SA (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 4:295–306. https://doi.org/10.1111/j.1538-7836.2006.01753.x
Bertolaccini ML, Hughes GR, Khamashta MA (2004) Revisiting antiphospholipid antibodies: from targeting phospholipids to phospholipid binding proteins. Clin Lab 50:653–665
Žigon P, Čučnik S, Ambrožič A, Kveder T, Šemrl SS, Rozman B, Božič B (2013) Detection of antiphosphatidylserine/prothrombin antibodies and their potential diagnostic value. Clin Dev Immunol 2013:1–8. https://doi.org/10.1155/2013/724592
Zhang S, Wu Z, Li J, Wen X, Li L, Zhang W, Zhao J, Zhang F, Li Y (2017) Evaluation of the clinical relevance of anti-annexin-A5 antibodies in Chinese patients with antiphospholipid syndrome. Clin Rheumatol 36:407–412. https://doi.org/10.1007/s10067-016-3510-8
Bertolaccini ML, Amengual O, Atsumi T, Binder WL, de Laat B, Forastiero R, Kutteh WH, Lambert M, Matsubayashi H, Murthy V, Petri M, Rand JH, Sanmarco M, Tebo AE, Pierangeli SS (2011) ‘Non-criteria’ aPL tests: report of a task force and preconference workshop at the 13th International Congress on Antiphospholipid Antibodies, Galveston, TX, USA, April 2010. Lupus 20:191–205. https://doi.org/10.1177/0961203310397082
Brandt JT, Triplett DA, Alving B, Scharrer I (1995) Criteria for the diagnosis of lupus anticoagulants: an update. On behalf of the Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibody of the Scientific and Standardisation Committee of the ISTH. Thromb Haemost 74:1185–1190
Bozic B, Kveder T, Stegnar M, Morosini-Berus E, Kos-Golja M, Peternel P, Rozman B (1997) Influence of degraded phosphatidylserine on binding of antiphospholipid antibodies. Int Arch Allergy Immunol 112:19–26. https://doi.org/10.1159/000237426
Cucnik S, Krizaj I, Rozman B, Kveder T, Bozic B (2004) Concomitant isolation of protein C inhibitor and unnicked beta2-glycoprotein I. Clin Chem Lab Med 42:171–174. https://doi.org/10.1515/CCLM.2004.031
Žigon P, Ambrožič A, Čučnik S, Kveder T, Rozman B, Božič B (2011) Modified phosphatidylserine-dependent antiprothrombin [corrected] ELISA enables identification of patients negative for other antiphospholipid antibodies and also detects low avidity antibodies. Clin Chem Lab Med 49:1011–1018. https://doi.org/10.1515/CCLM.2011.162
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE 3rd (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, Fang MC, Fisher M, Furie KL, Heck DV, Johnston SC, Kasner SE, Kittner SJ, Mitchell PH, Rich MW, Richardson D, Schwamm LH, Wilson JA, American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease (2014) Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45:2160–2236. https://doi.org/10.1161/STR.0000000000000024
Andreoli L, Chighizola CB, Banzato A, Pons-Estel GJ, Ramire de Jesus G, Erkan D (2013) Estimated frequency of antiphospholipid antibodies in patients with pregnancy morbidity, stroke, myocardial infarction, and deep vein thrombosis: a critical review of the literature. Arthritis Care Res (Hoboken) 65:1869–1873. https://doi.org/10.1002/acr.22066
Sciascia S, Sanna G, Khamashta MA, Cuadrado MJ, Erkan D, Andreoli L, Bertolaccini ML, Action APS (2015) The estimated frequency of antiphospholipid antibodies in young adults with cerebrovascular events: a systematic review. Ann Rheum Dis 74:2028–2033. https://doi.org/10.1136/annrheumdis-2014-205663
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie-Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers DV, Tirschwell DL, American Heart Association Stroke Council (2018) 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 49:e46–e110. https://doi.org/10.1161/STR.0000000000000158
Delgado MG, Rodríguez S, García R, Sánchez P, Sáiz A, Calleja S (2015) Antiphospholipid syndrome of late onset: a difficult diagnosis of a recurrent embolic stroke. J Stroke Cerebrovasc Dis 24:e209–e211. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.04.016
Garcia D, Erkan D (2018) Diagnosis and management of the antiphospholipid syndrome. N Engl J Med 378:2010–2021. https://doi.org/10.1056/NEJMra1705454
Pyo JY, Jung SM, Lee SW, Song JJ, Lee SK, Park YB (2017) Subsequent thrombotic outcomes in patients with ischemic stroke with antiphospholipid antibody positivity. Yonsei Med J 58:1128–1134. https://doi.org/10.3349/ymj.2017.58.6.1128
Galli M, Luciani D, Bertolini G, Barbui T (2003) Lupus anticoagulants are stronger risk factors for thrombosis than anticardiolipin antibodies in the antiphospholipid syndrome: a systematic review of the literature. Blood 101:1827–1832. https://doi.org/10.1182/blood-2002-02-0441
Pengo V, Testa S, Martinelli I, Ghirarduzzi A, Legnani C, Gresele P, Passamonti SM, Bison E, Denas G, Jose SP, Banzato A, Ruffatti A (2015) Incidence of a first thromboembolic event in carriers of isolated lupus anticoagulant. Thromb Res 135:46–49. https://doi.org/10.1016/j.thromres.2014.10.013
Pengo V, Denas G, Padayattil SJ, Zoppellaro G, Bison E, Banzato A, Hoxha A, Ruffatti A (2015) Diagnosis and therapy of antiphospholipid syndrome. Pol Arch Med Wewn 125:672–677
Yelnik CM, Urbanski G, Drumez E, Sobanski V, Maillard H, Lanteri A, Morell-Dubois S, Caron C, Dubucquoi S, Launay D, Duhamel A, Hachulla E, Hatron PY, Lambert M (2017) Persistent triple antiphospholipid antibody positivity as a strong risk factor of first thrombosis, in a long-term follow-up study of patients without history of thrombosis or obstetrical morbidity. Lupus 26:163–169. https://doi.org/10.1177/0961203316657433
Ruiz-Irastorza G, Cuadrado MJ, Ruiz-Arruza I, Brey R, Crowther M, Derksen R, Erkan D, Krilis S, Machin S, Pengo V, Pierangeli S, Tektonidou M, Khamashta M (2011) Evidence-based recommendations for the prevention and long-term management of thrombosis in antiphospholipid antibody-positive patients: report of a task force at the 13th International Congress on antiphospholipid antibodies. Lupus 20:206–218. https://doi.org/10.1177/0961203310395803
Burn J, Dennis M, Bamford J, Sandercock P, Wade D, Warlow C (1994) Long-term risk of recurrent stroke after a first-ever stroke. The Oxfordshire Community Stroke Project. Stroke 25:333–337
Crowther MA, Ginsberg JS, Julian J, Denburg J, Hirsh J, Douketis J, Laskin C, Fortin P, Anderson D, Kearon C, Clarke A, Geerts W, Forgie M, Green D, Costantini L, Yacura W, Wilson S, Gent M, Kovacs MJ (2003) A comparison of two intensities of warfarin for the prevention of recurrent thrombosis in patients with the antiphospholipid antibody syndrome. N Engl J Med 349:1133–1138. https://doi.org/10.1056/NEJMoa035241
Okuma H, Kitagawa Y, Yasuda T, Tokuoka K, Takagi S (2009) Comparison between single antiplatelet therapy and combination of antiplatelet and anticoagulation therapy for secondary prevention in ischemic stroke patients with antiphospholipid syndrome. Int J Med Sci 7:15–18
Funding
The study was supported by the Slovenian Research Agency (ARRS) for the National Research Programme (P3-0314).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Ethics approval
The study was approved by the Slovene National Medical Ethics Committee (163/02/09).
Additional information
Rheumatology in Slovenia: Clinical practice and translational research
Rights and permissions
About this article
Cite this article
Gašperšič, N., Zaletel, M., Kobal, J. et al. Stroke and antiphospholipid syndrome—antiphospholipid antibodies are a risk factor for an ischemic cerebrovascular event. Clin Rheumatol 38, 379–384 (2019). https://doi.org/10.1007/s10067-018-4247-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-018-4247-3