Abstract
Adult-onset Still’s disease (AOSD) is a systemic inflammatory disease of unknown etiology. Recently, it has been reported that quite a few cases of refractory AOSD were successfully treated with tocilizumab (TCZ) and corticosteroids were withdrawn in some of these patients. We report two AOSD patients who were treated successfully with TCZ monotherapy; thus, avoiding corticosteroid treatment. Because both of the patients refused to take corticosteroids, we planned to treat them with 8 mg/kg of TCZ monotherapy at weeks 0, 2, 6 and subsequently every 4 weeks. The efficacy of TCZ was assessed by patients’ clinical symptoms such as fever, arthralgia, skin eruptions, and laboratory markers such as serum levels of CRP, ferritin, and IL-6. We also reviewed 14 previous case reports including 30 cases who had been treated with TCZ for AOSD. Our patients responded rapidly and have been maintained in clinical remission without corticosteroid treatment. In the literature review, concomitant corticosteroid treatment described in 13 cases was successfully tapered in 7 and discontinued in 6 cases. TCZ monotherapy can be a candidate for the first-line therapy for some AOSD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adult-onset Still’s disease (AOSD) is a systemic inflammatory disease of unknown etiology and is characterized by remittent fever, evanescent salmon pink rash, and polyarthralgia frequently accompanied by neutrophilic leukocytosis [1, 2]. AOSD treatment comprises non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and immunosuppressive drugs such as methotrexate (MTX) [3]. Corticosteroids, in particular, still provide mainstay AOSD therapy despite various adverse effects [3].
Recently, numerous studies have revealed that proinflammatory cytokines such as IL-1, IL-6, IL-18, tumor necrosis factor (TNF), and interferon-gamma are involved in AOSD’s pathogenesis [4, 5]. In fact, AOSD patients have been successfully treated with anti-cytokine therapies such as with TNF-α blocking agents [6, 7], an IL-1 receptor antagonist (anakinra) [8, 9], and an anti-IL-6 receptor monoclonal antibody (tocilizumab, TCZ) [10–23]. Most of the cases are refractory to conventional therapies including high-dose corticosteroids and immunosuppressive drugs (cyclosporin and methotrexate, etc.) [11, 14, 16–18, 20, 22]. Among these case reports, TCZ seems to be highly effective for treating patients refractory to TNF antagonists [16, 17, 20] and anakinra [11, 14, 18, 22].
Here, we describe two patients with AOSD who were treated with TCZ monotherapy without corticosteroids. Table 1 summarizes the patients’ characteristics.
Case reports
Case 1
A 32-year-old woman was admitted to our hospital in January 2009 with fever, polyarthralgia, sore throat, and skin eruptions. Two years earlier, she experienced self-limiting high fever and cervical lymphadenopathy. Eight months prior to admission, she developed eruptions on her back, both arms and legs, which were improved by olopatadine hydrochloride and clobetasol propionate ointment treatment. Two weeks prior to admission, she developed a sore throat followed by skin eruptions, fever and polyarthralgia, which did not respond to cefcapene pivoxil hydrochloride hydrate and NSAIDs.
Laboratory test results on admission were as follows: leukocyte count 13,000/μl (neutrophils, 10,900/μl), hemoglobin 13.4 g/dl, platelet count 198,000/μl, erythrocyte sedimentation rate (ESR) 110 mm/hr, C-reactive protein (CRP) 33.8 mg/dl, aspartate aminotransferase (AST) 29 IU/l, alanine aminotransferase (ALT) 22 IU/l, lactate dehydrogenase (LDH) 285 IU/l, creatinine 0.55 mg/dl, ferritin 1,679 ng/ml, and normal urine values. Serological tests were negative for rheumatoid factor (RF) and antinuclear antibodies (ANA). The serum IL-6, TNF-α and soluble IL-2 receptor levels were 398 pg/ml (normal range <4.0 pg/ml), 3.2 pg/ml (normal range 0.6–2.8 pg/ml) and 1,090 U/ml (normal range 220–530 U/ml), respectively. Computed tomography revealed cervical lymphadenopathy and mild splenomegaly. Laboratory evaluations ruled out infections and malignancies, and she was therefore given a diagnosis of AOSD based on Yamaguchi’s classification criteria [2].
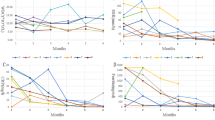
Because the patient refused to take corticosteroids, we tried etanercept (50 mg/week) first, since there are some case reports on anti-TNF agents’ efficacy for treating AOSD [6, 7]. However, there was no improvement in patient’s clinical symptoms (Fig. 1).
Therefore, we administered 8 mg/kg of TCZ, which rapidly mitigated symptoms and lowered inflammatory marker levels. Although the third infusion was planned at week 6, CRP and leukocyte count slightly increased and her symptoms such as low grade fever and polyarthralgia appeared at week 4 (Fig. 1). Therefore, the third infusion was administered at week 5 soon after. After the infusions at weeks 5, 8, and 11, all the symptoms and signs of AOSD disappeared, and the patient received TCZ subsequently every 4 weeks to remain in complete remission, which has lasted for more than 2 years. Serum IL-6 level also decreased to 5.4 pg/ml and ferritin level was normal. Corticosteroids were never administered throughout her disease course.
Case 2
An 18-year-old man was admitted to our hospital in August 2010 because of fever, polyarthralgia, sore throat, and myalgia. He had been well until about 3 weeks earlier. Two weeks prior to admission, he had received antibiotics, including azithromycin hydrate, levofloxacin hydrate, and panipenem/betamipron, but had shown no response. Laboratory test results on admission were as follows: leukocyte count 30,400/μl (neutrophils 25,500/μl), hemoglobin 12.5 g/dl, platelet count 521,000/μl, ESR 53 mm/h, prothrombin time INR 1.26, activated partial thromboplastin time 30.0 seconds, fibrinogen 700 mg/dl, D-dimer 1.96 μg/ml, CRP 25.6 mg/dl, AST 15 IU/l, ALT 26 IU/l, LDH 245 IU/l, serum creatinine 0.81 mg/dl, and ferritin 2,756 ng/ml. The urine values were all normal. Serological tests were negative for both RF and ANA. The serum IL-6 and soluble IL-2 receptor levels were, respectively, 18.8 pg/ml and 1,050 U/ml. Abdominal ultrasonography showed mild splenomegaly. We excluded infections, malignancies, and other rheumatic diseases by radiological examinations, gastrointestinal and colon endoscopy, and laboratory examinations that included repetitive culture for microorganisms as well as assays for various autoantibodies. The patient got a diagnosis of AOSD, but he and his family did not consent to corticosteroid therapy. We decided to administer 8 mg/kg of TCZ at weeks 0, 2, 6, and subsequently every 4 weeks. One day after the first TCZ infusion, fever and polyarthralgia abated markedly and serum CRP level returned to normal within 1 week. The second TCZ was administered at week 3 because of patient’s affairs, and the patient was discharged 3 days later. TCZ has been continued every 4 weeks for 8 months and the patient is still in complete remission.
Discussion
This is the first case report, to our knowledge, demonstrating that TCZ monotherapy was effective for AOSD. Corticosteroids are usually required to improve clinical symptoms and laboratory abnormalities and are still a mainstay for inducing remission in AOSD. In fact, most (76%–95%) AOSD patients can be successfully treated with corticosteroids, and they respond dramatically [3]. However, consensus is lacking on a therapeutic corticosteroid tapering scheme after achieving clinical remission. Slow reduction is often necessary to maintain a good response and to avoid relapse. Corticosteroid dependence increases the risk for potentially serious mid- and long-term side effects caused by Cushing-like phenomena, diabetes, osteoporosis, and osteonecrosis. Anti-rheumatic drugs such as MTX are also reported to be effective [24, 25], but we are not aware of any randomized controlled trials.
The mechanisms underlying AOSD are not completely understood, but the role of proinflammatory cytokines may play a significant role in its pathogenesis because biological response modifiers targeted to these cytokines have been used successfully to treat AOSD. Promising results have been reported with TNF inhibitors such as etanercept and infliximab, but treatment failures and apparent loss of efficacy have also been described [6, 7]. A role for IL-1 has been also demonstrated by patient’s response to anakinra [8, 9, 26].
IL-6 is also believed to play a crucial role in pathogenesis, and its serum levels correlate well with the AOSD’s severity [4, 27]. There have been several other reports regarding TCZ’s efficacy (Table 2) [10–23]. Fitzgerald et al. [8] proposed that TNF-α induces IL-1 production, which stimulates IL-6 expression. Therefore, Matsumoto et al. [13] stated that directly inhibiting IL-6 activity, which is the most downstream cytokine in the AOSD inflammatory cascade, may be better than blocking IL-1. In fact, AOSD patients who responded poorly to anakinra responded well to TCZ [11, 14, 18, 22]. Moreover, concomitant corticosteroid treatment described in 13 cases was successfully tapered in 7 [13–16, 18, 21, 23] and discontinued in 6 cases [10–12, 19, 20] after achieving TCZ-induced remission, suggesting that TCZ monotherapy may serve as first-line remission induction therapy.
In our present report, TCZ monotherapy rapidly improved each patient’s health, and the patients have remained in complete remission. However, case 1 appeared to relapse after the second TCZ infusions. Although other cytokines such as IL-18 [4, 28, 29] might have been more important targets, TCZ may have been effective if biweekly infusion had been continued as used to treat systemic type juvenile idiopathic arthritis (classical Still’s disease) [30]. Biweekly infusions of TCZ can be necessary for some AOSD patients to protect exacerbation completely.
TCZ was well tolerated by our patients. However, severe adverse events with macrophage activation syndrome (MAS) due to cytomegalovirus infection have been reported [11]. AOSD itself may cause MAS, and it may be difficult to distinguish TCZ’s adverse effects from treatment insufficiency noted in the other case [21]. However, both patients were able to resume TCZ and continued after the MAS abated. Another concern is exacerbation of AOSD or MAS due to a transient increase of serum levels of target cytokine right after the cytokine blockade [31]. However, no exacerbation was seen in our cases, and was not described in all the reported cases treated with TCZ except one case [22]. We should be watchful for this kind of adverse event when we treat AOSD patients with cytokine blockade, but it seems to be rare in TCZ therapy.
In conclusion, TCZ monotherapy may be effective in some patients with AOSD.
References
Bywaters EGL (1971) Still’s disease in the adult. Ann Rheum Dis 30:121–133
Yamaguchi M, Ohta A, Tsunematsu T, Kasukawa R, Mizushima Y et al (1992) Preliminary criteria for classification of adult-onset Still’s disease. J Rheumatol 19:424–430
Bagnari V, Colina M, Ciancio G, Govoni M, Trotta F (2010) Adult-onset Still’s disease. Rheumatol Int 30:855–862
Hoshino T, Ohta A, Yang D, Kawamoto M, Kikuchi M et al (1998) Elevated serum interleukin 6, interferon-gamma, and tumor necrosis factor-alpha levels in patients with adult Still’s disease. J Rheumatol 25:396–398
Efthimiou P, Kontzias A, Ward CM, Ogden NS (2007) Adult-onset Still’s disease: can recent advances in our understanding of its pathogenesis lead to targeted therapy? Nat Clin Pract Rheumatol 3:328–335
Fautrel B, Sibilia J, Mariette X, Combe B, Club Rhumatismes et Inflammation (2005) Tumour necrosis factor alpha blocking agents in refractory adult Still’s disease: an observational study of 20 cases. Ann Rheum Dis 64:262–266
Kraetsch HG, Antoni C, Kalden JR, Manger B (2001) Successful treatment of a small cohort of patients with adult-onset of Still's disease with infliximab: first experiences. Ann Rheum Dis 60(suppl 3):iii55–iii57
Fitzgerald AA, Leclercq SA, Yan A, Homik JE, Dinarello CA (2005) Rapid responses to anakinra in patients with refractory adult-onset Still’s disease. Arthritis Rheum 52:1794–1803
Naumann L, Feist E, Natusch A, Langen S, Klause A et al (2010) IL-1-receptor antagonist anakinra provides long-lasting efficacy in the treatment of refractory adult-onset Still’s disease. Ann Rheum Dis 69:466–467
Iwamoto M, Nara H, Hirata D, Minota S, Nishimoto N et al (2002) Humanized monoclonal anti-interleukin-6 receptor antibody for treatment of intractable adult-onset Still’s disease. Arthritis Rheum 46:3388–3389
De Bandt M, Saint-Marcoux B (2009) Tocilizumab for multirefractory adult-onset Still’s disease. Ann Rheum Dis 68:153–154
Nakahara H, Mima T, Yoshio-Hoshino N, Matsushita M, Hashimoto J et al (2009) A case report of a patient with refractory adult-onset Still’s disease who was successfully treated with tocilizumab over 6 years. Mod Rheumatol 19:69–72
Matsumoto K, Nagashima T, Takatori S, Kawahara Y, Yagi M et al (2009) Glucocorticoid and cyclosporine refractory adult-onset Still’s disease successfully treated with tocilizumab. Clin Rheumatol 28:485–487
Perdan-Pirkmajer K, Praprotnik S, Tomšič M (2010) A case of refractory adult-onset Still’s disease successfully controlled with tocilizumab and a review of the literature. Clin Rheumatol 29:1465–1467
Naniwa T, Ito R, Watanabe M, Hayami Y, Maeda S, et al. (2010) Case report: successful use of short-term add-on tocilizumab for multirefractory systemic flare of adult-onset Still’s disease. Clin Rheumatol. doi:10.1007/s10067-010-1562-8
Sumida K, Ubara Y, Hoshino J, Suwabe T, Hiramatsu R et al (2010) Etanercept-refractory adult-onset Still’s disease with thrombotic thrombocytopenic purpura successfully treated with tocilizumab. Clin Rheumatol 29:1191–1194
Yoshimura M, Makiyama J, Koga T, Miyashita T, Izumi Y et al (2010) Successful treatment with tocilizumab in a patient with refractory adult-onset Still’s disease (AOSD). Clin Exp Rheumatol 28:141–142
Rech J, Ronneberger M, Englbrecht M, Finzel S, Katzenbeisser J et al (2011) Successful treatment of adult-onset Still’s disease refractory to TNF and IL-1 blockade by IL-6 receptor blockade. Ann Rheum Dis 70:390–392
Kishida D, Okuda Y, Onishi M, Takebayashi M, Matoba K et al (2011) Successful tocilizumab treatment in a patient with adult-onset Still’s disease complicated by chronic active hepatitis B and amyloid A amyloidosis. Mod Rheumatol 21:215–218
Thonhofer R, Hiller M, Just H, Trummer M, Siegel C, et al. (2011) Treatment of refractory adult-onset still’s disease with tocilizumab: report of two cases and review of the literature. Rheumatol Int 31:1653–1656
Kobayashi M, Takahashi Y, Yamashita H, Kaneko H, Mimori A (2011) Benefit and a possible risk of tocilizumab therapy for adult-onset Still’s disease accompanied by macrophage-activation syndrome. Mod Rheumatol 21:92–96
Puéchal X, DeBandt M, Berthelot JM, Breban M, Dubost JJ, Club Rhumatismes Et Inflammation et al (2011) Tocilizumab in refractory adult Still’s disease. Arthritis Care Res 63:155–159
Sabnis GR, Gokhale YA, Kulkarni UP (2011) Tocilizumab in refractory adult-onset Still’s disease with aseptic meningitis—efficacy of interleukin-6 blockade and review of the literature. Semin Arthritis Rheum 40:365–368
Aydintug AO, D’Cruz D, Cervera R, Khamashta MA, Hughes GR (1992) Low dose methotrexate treatment in adult Still’s disease. J Rheumatol 19:431–435
Fujii T, Akizuki M, Kameda H, Matsumura M, Hirakata M et al (1997) Methotrexate treatment in patients with adult-onset Still’s disease—retrospective study of 13 Japanese cases. Ann Rheum Dis 56:144–148
Kalliolias GD, Georgiou PE, Antonopoulos IA, Andonopoulos AP, Liossis SN (2007) Anakinra treatment in patients with adult-onset Still’s disease is fast, effective, safe and steroid sparing: experience from an uncontrolled trial. Ann Rheum Dis 66:842–843
Chen DY, Lan JL, Lin FJ, Hsieh TY et al (2004) Proinflammatory cytokine profiles in sera and pathological tissues of patients with active untreated adult-onset Still’s disease. J Rheumatol 31:2189–2198
Kawaguchi Y, Terajima H, Harigai M, Hara M, Kamatani N (2001) Interleukin-18 as a novel diagnostic marker and indicator of disease severity in adult-onset Still’s disease. Arthritis Rheum 44:1716–1717
Kawashima M, Yamamura M, Taniai M, Yamauchi H, Tanimoto T et al (2001) Levels of interleukin-18 and its binding inhibitors in the blood circulation of patients with adult-onset Still’s disease. Arthritis Rheum 44:550–560
Yokota S, Imagawa T, Takei S, Murata T, Tomiita M et al (2011) Guidance on using tocilizumab for juvenile idiopathic arthritis. Mod Rheumatol 21:563–571
Kaneko K, Kaburaki M, Muraoka S, Tanaka N, Yamamoto T et al (2010) Exacerbation of adult-onset Still’s disease, possibly related to elevation of serum tumor necrosis factor-alpha after etanercept administration. Int J Rheum Dis 13:e67–e69
Conflicts of interest
H.K. has received honoraria from Mitsubishi-Tanabe Pharma, Pfizer, Abbott, Eisai Pharma, and Bristol-Myers KK. T.T. has received research support and consulting or lecture fees from Chugai Pharma. K.A. received research grants from Tanabe-Mitsubishi, Astellas, and Chugai pharmaceutical companies. The other authors have declared no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sakai, R., Nagasawa, H., Nishi, E. et al. Successful treatment of adult-onset Still’s disease with tocilizumab monotherapy: two case reports and literature review. Clin Rheumatol 31, 569–574 (2012). https://doi.org/10.1007/s10067-011-1917-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-011-1917-9