Abstract
Heparin-induced thrombocytopenia (HIT) is a rare but life-threatening side effect of heparin therapy. It is a demanding therapeutic challenge in patients undergoing left ventricular assist device (LVAD) implantation. We present our experience with LVAD implantation under extracorporeal life support (ECLS) in patients suffering from HIT. Seven patients (mean age 54.0 ± 16.7 years, 1 female, 6 male patients) suffering from acute heart failure were stabilized with ECLS. Under heparin therapy, they all showed a sudden decrease of mean platelet count (maximum 212.6 ± 41.5 tsd/μl; minimum 30.7 ± 13.1 tsd/μl). Due to the clinical suspicion of HIT anticoagulation was switched from heparin to argatroban (aPTT 70–80 s.). No improvement of cardiac function could be detected under ECLS, so LVAD implantation was indicated. We performed LVAD implantation under ECLS. During LVAD implantation under argatroban (aPTT of 50–60 s.) one patient developed massive intraventricular thrombus formations, so the device had to be removed. In 6 cases, we could successfully perform LVAD implantation under argatroban with a higher aPTT of 70–80 s and modified operative strategy. Four patients needed postoperative re-exploration because of bleeding complications. Perioperative management of LVAD patients under argatroban anticoagulation is very difficult. We were able to minimize the perioperative risk for thrombosis with a target aPTT of 70–80 s. To keep the phase of stasis within the device as short as possible we anastomosed the VAD outflow graft to the ascending aorta first before connecting the device to the apex. However, postoperative bleeding complications are frequent.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
By left ventricular assist device (LVAD) implantation in patients with severe cardiac insufficiency resistant to medical therapy, patients can either be bridged to transplantation or be supported with an assist device as a destination therapy (1, 2). In case of acute circulatory impairment with severe hemodynamic instability, multi-organ failure can appear which unfavorably affects survival after LVAD implantation. Extracorporeal life support (ECLS) is a well-established technique for quick and easy installable circulatory support that offers the opportunity of recoverment from such organ injury (3–7) prior to LVAD therapy. Once organ functions have been stabilized, long-term circulatory function can be sustained with an early bridge to uni- or biventricular assist device.
This paper refers to the immune form of Heparin-induced thrombocytopenia which will simply be abbreviated as HIT in the following text. HIT is a rare but life-threatening side effect of heparin therapy that occurs in up to 3 % of all heparin-treated patients (8) whereas the risk of developing a HIT rises up to 5 % in patients after vascular and cardiac surgery (9). Schenk et al. even described an incidence of up to 11 % in patients receiving mechanical circulatory support (10). Patients on mechanical circulatory support usually require strong anticoagulation. In this population, the diagnosis of HIT introduces a demanding therapeutic challenge. A further source of complications in this group of patients involves the use of cardiopulmonary bypass (CPB) due to the need for anticoagulation with heparin or bivalirudin to be on-pump.
This study details one center’s experience with left ventricular assist device implantation (HeartMate II, Thorarec, Pleasanton, CA, USA; HVAD, HeartWare International, Inc., MA, USA) in patients with acute heart failure under ECLS suffering from heparin-induced thrombocytopenia type II.
Materials and methods
Between March 2012 and August 2013 a total of thirty-five patients (mean age 50.0 ± 16.0 years, 9 female, 26 male patients) received VAD in our department because of dilative cardiomyopathy, chronic ischemic cardiomyopathy or after myocardial infarction. This study details on seven of these patients, who needed emergent ECLS prior to VAD implantation because of acute cardiac failure (mean age 54.0 ± 16.7 years, 1 female, 6 male patients). Detailed patient characteristics are given in Tables 1, 2.
Two patients suffered from dilative and three from ischemic cardiomyopathy, two from acute myocardial infarction and early postoperative heart failure after CABG. Three patients received a reoperation after cardiac surgery.
Cardiopulmonary bypass was performed using a roller pump (Maquet, Rastatt, Germany) using a hollow fiber-membrane oxygenator with a hard-shell venous reservoir (Quadrox I Adult/VHK 71000, Maquet, Rastatt, Germany) at a non-pulsatile flow rate of 2.6 l/min−2/m2. The noncoated CPB tubing (Maquet, Rastatt, Germany) was used in all patients. Blood flow was monitored by a Doppler flow probe on the arterial side of the circuit. ECLS was instituted through the right axillary artery and the femoral vein. To avoid limb ischemia, we used an 8-mm Dacron prosthesis (end-to-side anastomosis to the right axillary artery), which was tied on a 20F flexible arterial cannula (EOPA, Medtronic) to ensure central arterial blood flow as well as the distal perfusion of the arm. To achieve an activated partial thromboplastin time (aPTT) between 50 and 60 s, patients were initially heparinized. The aPTT was checked at least 2 times a day.
Maintenance of adequate systemic blood flow was monitored by mean arterial pressure, blood lactate concentration, central or mixed venous oxygen saturation and diuresis. Mean arterial pressure was maintained between 50 and 70 mmHg with vasopressor or vasodilator administration. Preserving residual left ventricular ejection was also expected to reduce the risk of intracardiac clot formation. Whenever pulsation disappeared, volume expansion or inotropic support was immediately started until pulsatile systemic blood flow reappeared. An important marker of stabilization and recovery was the improvement of the liver and kidney function, which considerably co-determined the time of LVAD implantation.
Due to relevant decrease of platelet count during ECLS in all patients, heparin medication was switched to argatroban with an initial dosage of 2 mg per hour. We afterwards regulated the dosage according to the aPTT—aimed values under ECLS were 70–80 s in all described cases. HIT was confirmed by a heparin-induced platelet aggregation (HIPA; antibodies against complexes of heparin and platelet factor 4).
We tried to wean all patients from ECLS, but as cardiac function did not recover, LVAD implantation was indicated. We performed LVAD implantation under ECLS. In 5 patients the HeartMate II device was implanted (HeartMate II, Thoratec. Corp., Pleasanton, CA, USA); another two patients received the HeartWare device. In 5 cases, ECLS was switched to right ventricular assist device (RVAD), in 1 case ECLS could be explanted after LVAD implantation and the patient with widespread thrombus formation needed further ECLS after LVAD explanation as bridge-to-transplant.
Operative procedure of LVAD implantation
Perioperative anticoagulation strategy and operative procedure in the first patient
Argatroban was used for anticoagulation under ECLS with an aPTT of 50–60 s. A median sternotomy was performed and the pocket for the device (HeartMate II) was prepared. As intracavitary thrombi had been detected by preoperative echocardiography, we chose not to perform LVAD implantation beating heart but in cardioplegic arrest to be able to remove the thrombotic material. Therefore a cardioplegia needle was inserted into the ascending aorta and the cardioplegia was started after clamping of the aorta. Using the core device we opened the apex on the arrested heart trying to minimize the blood loss. For this reason we used the Cell Saver. The left ventricle was inspected and the described thrombotic material was carefully removed. Then the pump ring was attached to the left ventricle. Afterwards the device was inserted parallel to the septum. The pump was filled with blood and after de-airing the aortic clamp was removed. The outflow cannula was anastomosed to the ascending aorta. The device was carefully de-aired, the ECMO support was slowly reduced and the HeartMate II VAD was started. But we could not generate any flow with the device. Transesophageal echocardiography showed newly developed massive thrombus formations within the left and right ventricle as well as inside the LVAD and its outflow graft. We then had to open the ventricle once again to remove this thrombus formation, which strongly interspersed the trabecular meshwork. After thoroughly laborious removal of the intracardiac thrombotic material, the LVAD had to be removed. ECLS explantation was impossible because of hemodynamic instability.
The change of anticoagulation strategy and surgical approach
The case of the patient described above let to the decision to reassess and modify our therapeutic regime. To avoid similar thromboembolic complications we also changed anticoagulation management. The target aPTT was increased to 70–80 s. The thrombosis may also or additionally have been abetted by the time between priming the device with blood and starting the pump after the outflow graft anastomosis was finished (about 20 min). During this time we had a prolonged stasis of blood in the left ventricle but also a small volume of blood stagnant within the HeartMate II device.
We decided to clamp the aorta tangentially and to anastomose the outflow prosthesis of the VAD to the ascending aorta first before opening the apex, to keep the phase of stasis within the device as short as possible. In addition, implantation technique with cardioplegic arrest was further performed in all patients as we decided to inspect the left ventricle and remove thrombotic material if needed in all following LVAD patients with HIT to reduce thromboembolic and neurologic risk.
For the control of postoperative anticoagulation, which was initially continued with argatroban, an aPTT control was performed in all patients at least 3 times a day if possible until the 3rd postoperative day and later on switched to aPTT control twice or once a day. Afterwards we switched to coumadin in combination with 100 mg acetylsalicyl for long-term anticoagulation.
Statistical methods
Data are presented as mean ± standard deviation.
Results
Status pre LVAD implantation
As already depicted above, all patients suffered from acute cardiomyopathy with dilated ventricles and excessively reduced ventricular ejection function (mean LVEF 12 %) and received emergent ECLS with initial heparin therapy for anticoagulation. Under ECL support organ function improved. Duration of ECLS therapy ranged from 5 to 16 days, mean ECLS to LVAD interval was 10.4 ± 4.2 days. All patients recovered from organ injury. Laboratory data demonstrated a decline of: GOT 2116.3 ± 963.3–37.7 ± 10.0 U/l, GPT 2462.7 ± 947.8–46.7 ± 28.9 U/l, creatinine 2.5 ± 1.0–1.5 ± 1.0 mg/dl (see Table 3).
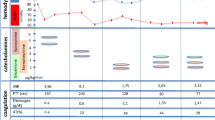
Except one patient, all other patients demonstrated with normal number of platelets at time of hospital admission. Under ECLS all patients showed a sudden decrease of platelets. Mean platelet count decreased from maximum values of 212.6 ± 41.5 tsd/μl before ECLS down to a minimum of 30.7 ± 13.1 tsd/μl. Maximum platelet values, decrease of platelet count during the first 5 days of ECLS and minimal platelet values under ECLS are depicted in Fig. 1. Due to the clinical suspicion of HIT, anticoagulation was changed from heparin to argatroban (4.14 ± 2.27 days after ECLS implantation) with a target PTT of 70–80 s. All patients were tested for HIT by a heparin-induced platelet aggregation test (HIPA). In 6 cases the HIT test was positive; in one patient it was negative. This one patient with a negative HIPA test was also treated with argatroban due to clinical suspicion for HIT but anticoagulation was not switched to heparin again despite negative HIPA test.
Platelet count under ECLS therapy (tsd/µl) with mean values and standard variations. X-axis the maximum and minimum platelet counts before and after ECLS implantation are presented in contrasted color as these values were defined by absolute values that appeared to different time points in each patient. In contrast to this, the given values of the ELCS implantation day and the 1st to 5th postoperative day were defined by dates
Status post LVAD implantation
We were able to successfully implant the HeartMate II device in 4 and the HeartWare device in 2 cases. Concerning the function of the right heart, it was possible to explant the ECLS at the same time as LVAD implantation in 1 patient. ECLS was switched to right heart support via pulmonary artery and femoral vein in 5 other cases and the patient with the intracardial thrombosis was in need for further ECLS as bridge-to-transplant. Mean duration of RVAD support interval was 2.8 ± 4.1 days. Postoperative anticoagulation was initially continued with argatroban. Regarding the aPTT values and the titration of the argatroban dosage, we could observe that it took about three days (the day of the operation until the 2nd postoperative day) to achieve stable circumstances. To demonstrate this, we depicted the above-named values and added the values of the 3rd postoperative day in Fig. 2.
Postoperative argatroban titration: Course of the aPTT (left) and the actual dose of argatroban (right) and its range in each patient. The aPTT is given in seconds and the corresponding argatroban dosages in μg/kg/min. We used the same scaling for all diagrams but for the description of case number 1, as this patient represents an exceptional case: patient number 1 suffered from fatal coagulation disorder and died on the 2nd postoperative day. In this case, numerous additional aPTT controls were performed and a much higher dosage of argatroban (up to 2.0 μg/kg/min) than in all other patients was administered. Measurements number 1–9 refer to the day of the operation, measurements number 10–17 to the 1st postoperative day and measurements 18–21 to the 2nd postoperative day, which was the day he died. Patient number 4 died on the 2nd postoperative day, so only nine aPTT controls were performed. Overall the required dosage of argatroban ranged up to 0.7 μg/kg/min, disregarding patient number 1. The particular increase of the dosage of argatroban ranged from 0.1 to 0.4 μg/kg/min
Four patients left hospital with good quality of life defined as improved physical capacity (reduction of NYHA class from IV down to 0–II), possibility of self-supply and freedom of neurologic deficites.
Neurologic complications
Postoperatively neurological function could be evaluated in 6 cases. One patient could not be evaluated as he suffered from multi-organ failure with hemodynamic instability and was therefore sedated continuously. None of the other 6 patients showed focal neurological deficits.
Hemostatic complications
Four patients needed re-exploration due to postoperative bleeding complications. One developed progressive intracardial thrombosis under ECLS.
Survival rate
The one patient who developed massive thrombi during LVAD implantation with consecutive LVAD explantation needed continuation of ECLS as bridge-to-transplant. Anesthesia was stopped and the patient woke up without any focal neurological deficit. He was immediately listed for heart transplantation (high urgency status), but due to multi-organ failure caused by an uncontrollable coagulation disorder with massive widespread arterial and venous thrombus formation, he died two days later. Two more patients died 2 and 17 days after LVAD implantation caused by not-device-related sepsis. It has to be emphasized that these two patients were operated on as ultima ratio due to cardiogenic shock (INTERMACS level 1). Therefore, the overall survival was 57.1 %.
Discussion
The use of left ventricular assist devices (LVADs) in acute and end-stage chronic heart failure has increased within the last years and it offers therapeutic options from bridge-to-recovery as well as bridge-to-transplant (11, 12). Meanwhile VADs are also used as destination therapy in patients with severe heart failure refractory to medical therapy and consecutive cardiogenic shock. Pre-existing organ dysfunction is thought to unfavorably affect patient survival after VAD implantation (13). ECLS is a well-established technology that provides circulatory support with the possibility to recover from organ injury (3–7). Once hemodynamics is stabilized and organ function has recovered, long-term circulatory function can be maintained with an early bridge to univentricular or biventricular assist device.
Heparin is the most commonly anticoagulant drug. One major risk of heparin therapy is the heparin-induced thrombocytopenia (HIT) that can emerge in two forms: the minor manifestation is caused non-immunologically within the first 2 days of exposure; a non-permanent and reversible process (HIT type I). The malign form of HIT (HIT type II) is an immunological event that usually appears within 5–12 days after the patient was initially treated with heparin. If there was an earlier exposure within the last 3–6 months, symptoms might also occur earlier. HIT is a prothrombotic dysfunction, which is associated with a high risk for severe thromboembolic events (1).
Anticoagulation in cardiac patients with HIT is still a clinical challenge. During the last years, several reports on alternative anticoagulation with tedelparin, enoxaparin, ancrod, prostacyclin analogs like iloprost or danaparoid-sodium (DS) for CPB in patients with HIT have been published (14). However, the knowledge about anticoagulation in adult and pediatric LVAD patients with HIT is poor and optimal anticoagulation strategy is still unclear (1, 14–16). Comparable to other groups (10), we detected a HIT rate of about 17 % in patients with ECLS and VAD.
In 2000 Christiansen et al. described anticoagulation in three cases of LVAD implantation as bridge-to-transplant in patients suffering from heparin-induced thrombocytopenia type II (14). Comparable to one of our patients, the authors describe the development of thrombus in the left ventricle despite heparin therapy. Because of positive HIPA test with detection of antibodies the patient received DS as anticoagulant for operative procedure. Postoperatively the patient received further therapy with DS, monitored by antifactor Xa activity. But despite effective anticoagulation, he developed a venous thrombosis of the jejunum and died because of multi-organ failure after jejunal resection. The authors recommend the use of DS or r-hirudin only in patients with positive HIPA test at the time of LVAD implantation. In cases of negative HIPA test, heparin should be used before postoperative change of anticoagulation to DS or r-hirudin.
Busch et al. published a change of a percutaneous VAD into an intracorporeal system—without the use of ECC and without anticoagulation—in a patient with severe coagulopathy. In this case, despite a negative HIT test (enzyme-linked immunoassay) a drop of platelets was described. But it is also mentioned that sepsis might have been the reason for reducing platelets. Angiomax was the used drug in postoperative therapy and argatroban or lepirudin the described alternatives (17).
Argatroban is a direct thrombin inhibitor (DTI) that selectively and reversibly inhibits thrombin; both clot bound and free, at the catalytic site. Argatroban manifests an antiplatelet effect by diminishing thrombin-induced platelet activation. It is primarily metabolized in the liver with minimal renal elimination (18, 19). In multicentre studies argatroban improved outcomes in patients with HIT, particularly reducing new thrombosis, without increasing bleeding (20). Koster et al. have shown that the presence of HIT antibodies is strongly associated with an increased risk of thromboembolism in patients with a VAD, and that only 30 % of VAD patients with HIT achieved procedural success in the era of lepirudin therapy (21). In a study reported by Pappalardo et al. when HIT was diagnosed, heparin was discontinued and argatroban was initiated as a continuous infusion, target aPTT 45–80 s, depending on the type of assist device (22).
Limitations of this study
It has to be admitted, that one limitation of our study is the fact, that there is no comparison group in which patients received alternative strategy, anticoagulants and intensity of anticoagulation. Another limiting factor is the difficulty to prove the efficiency of argatroban treatment in the setting of HIT, as it is complex to obtain firm diagnosis. Delay of treatment due to further diagnostic investigation may restrain the chance of recovery from HIT. Clinical suspicion is of utmost importance in this type of clinical situation but it is dependent on clinical experience.
Conclusion
Perioperative management of LVAD patients under argatroban anticoagulation is a demanding therapeutic challenge and bleeding complications are frequent.
For LVAD implantation in patients with HIT a perioperative aPTT of 50–60 s does not seem to be sufficient to prevent thrombotic complications.
To reduce the perioperative risk for thrombosis within the ventricle and assist device itself it seems to be advisable to increase the target aPTT. The de-airing and priming of the LVAD should be done immediately prior starting the pump to avoid blood stasis within the device. Moreover—to keep the phase of stasis within the device as short as possible—we suggest to anastomose the outflow prosthesis of the VAD to the ascending aorta first before connecting the device to the left ventricle.
References
McCarthy PM, Portner PM, Tobler HG, Starnes VA, Ramasamy N, Oyer PE. Clinical experience with the Novacor ventricular assist system. Bridge to transplantation and the transistion to permanent application. J Thorac Cardiovasc Surg. 1991;102:578–86.
Kasirajan V, McCarthy PM, Hoercher KJ, Starling RC, Young JB, Banbury MK, Smedira NG. Clinical experience with long term use of implantable left ventricular assist devices: indications, implantation, and outcomes. Semin Thorac Cardiovasc Surg. 2000;12:229–37.
Doll N, Kiaii B, Borger M, Bucerius J, Kraemer K, Schmitt DV, Walther T, Mohr FW. Five-year results of 219 consecutive patients treated with extracorporeal membrane oxygenation for refractory postoperative cardiogenic shock. Ann Thorac Surg. 2004;77:151–7.
Chen YS, Ko WJ, Lin FY, Huang SC, Chou TF, Chou NK, Hsu RB, Wang SS, Chu SH. Preliminary result of an algorithm to select proper ventricular assist devices for high risk patients with extracorporeal membrane oxygenation support. J Heart Lung Transplant. 2001;20:850–7.
Levi D, Marelli D, Plunkett M, Alejos J, Bresson J, Tran J, Eisenring C, Sadeghi A, Galindo A, Fazio D, Gupta A, Burch C, George B, Laks H. Use of assist devices and ECMO to bridge pediatric patients with cardiomyopathy to transplantation. J Heart Lung Transplant. 2002;21:760–70.
Kihara S, Kawai A, Endo M, Koyangi H, Kurosawa H. Extracorporeal membrane oxygenation and left ventricular assist device: a case of double mechanical bridge. Heart Vessels. 2002;16:164–6.
Murashita T, Eya K, Miyatake T, Kamikubo Y, Shiiya N, Yasuda K, Sasaki S. Outcome oft he perioperative use of percutaneous cardiopulmonary support for adult cardiac surgery: factors affecting hospital mortality. Artific Organs. 2004;28:189–95.
Warkentin TE, Levine MN, Hirsh J, Horsewood P, Roberts RS, Gent M, Kelton JG. Heparin-induced thrombocytopenia in patients treated with low-molecular-weight heparin or unfractionated heparin. N Engl J Med. 1995;332:1330–5.
Welp H, Ellger B, Scherer M, Lanckohr C, Martens S, Gottschalk A. Heparin-induced thrombocytopenia during extracorporeal membrane oxygenation. J Cardiothorac Vasc Anaesth. 2014;28(2):342–4.
Schenk S, El-Banayosy A, Prohaska W, Arusoglu L, Morshuis M, Koester-Eiserfunke W, Kizner L, Murray E, Eichler P, Koerfer R, Greinacher A. Heparin-induced thrombocytopenia in patients receiving mechanical circulatory support. J Thorac Cardiovasc Surg. 2006;131:1373–81.e4 Epub 2006 May 2.
Eghtesady P, Nelson D, Schwartz SM, Wheeler D, Pearl JM, Cripe LH, Manning PB. Heparin-induced thrombocytopenia complicating support by the Berlin Heart. ASAIO J. 2005;51(6):820–5.
Schmitz ML, Massicote P, Faulkner SC, Bhutta AT, Johnson CE, Seib PM, Frazier EA, Fiser WP Jr, Imamura M, Jaquiss RD. Management of a pediatric patient on the Berlin Heart Excor ventricular assist device with argatroban after heparin-induced thrombocytopenia. ASAIO J. 2008;54(5):546–7.
Reinhartz O, Farrar DJ, Hershon JH, Avery GJ, Haeusselein EA. Donald Hill J. Importance of preoperative liver function as a predictor of survival in patients supported with thoratec ventricular assist devices as a bridge to transplantation. J Thorac Cardiovasc Surg. 1998;116:633–40.
Christiansen S, Jahn UR, Meyer J, Scheld HH, Van Aken H, Kehrel BE, Hammel D. Anticoagulative management of patients requiring left ventricular assist device implantation and suffering from heparin-induced thrombocytopenia type II. Ann Thorac Surg. 2000;69:774–7.
Brozena SC, Twomey C, Siegel J, Peterson P, Horrow JC, Samuels L, Morris R. Heart transplantation in patients with heparin-induced thrombocytopenia on the Novacor left ventricular assist system. J Heart Lung Transplant. 1998;17(7):729–31.
Tandler R, Weyand M, Schmid C, Gradaus R, Schmidt C, Scheld HH. Long-term anticoagulation with recombinant hirudin in a patient on left ventricular assist device support. ASAIO J. 2000;792–4.
Busch J, Wojciechowski Z, Torre-Amione G, Loebe M. Off-pump exchange of short-term percutaneous ventricular assist device (VAD) to long-term implantable VAD in severe coagulopathy and multi-organ failure. J Heart Lung Transplant. 2008;27(5):572–4.
Lewis BE, Wallis DE, Berkowitz SD, Matthai WH, Fareed J, Walenga JM, Bartholomew J, Sham R, Lerner RG, Zeigler ZR, Rustagi PK, Jang IK, Rifkin SD, Moran J, Hursting MJ, Kelton JG, ARG-911 Study Investigators. Argatroban anticoagulant therapy in patients with heparin-induced thrombozytopenia. Circulation. 2001;103:1838–43.
Lewis BE, Hursting M, McCollum D. Argatroban therapy in heparin-induced thrombozytopenia with hepatic dysfunction. Chest. 2006;129:1167–75.
Koster A, Buz S, Hetzer R, Kuppe H, Breddin K, Harder S. Anticoagulation with argatroban in patients with heparin-induced thrombocytopenia antibodies after cardiovascular surgery with cardiopulmonary bypass: first results from the ARGE03 trial. J Thorac Cardiovasc Surg. 2006;132:699–700.
Koster A, Huebler S, Potapov E, Meyer O, Jurmann M, Weng Y, Pasic M, Drews T, Kuppe H, Loebe M, Hetzer R. Impact of heparin induced thrombocytopenia on outcome in patients with ventricular assist device support: single-institution experience in 358 consecutive patients. Ann Thorac Surg. 2007;83:72–6.
Pappalardo F, Scandroglio AM, Potapov E, Stepanenko A, Maj G, Krabatsch T, Zangrillo A, Koster A, Hetzer R. Argatroban anticoagulation for heparin induced thrombocytopenia in patients with ventricular assist devices. Minerva Anaestesiol. 2012;78(3):330–5.
Conflict of interest
The authors declare that they have no conflict of interest and state that this manuscript has not been published previously and is not currently being assessed for publication by any other journal than the Journal of Artificial Organs. Each Author has contributed substantially to the research, preparation and production of the paper and approves of its submission to the journal.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hillebrand, J., Sindermann, J., Schmidt, C. et al. Implantation of left ventricular assist devices under extracorporeal life support in patients with heparin-induced thrombocytopenia. J Artif Organs 18, 291–299 (2015). https://doi.org/10.1007/s10047-015-0846-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-015-0846-9