Abstract
Purpose
Only a few series of patients with a spigelian hernia managed on an outpatient basis have been reported in the literature. The aim of this prospective study was to evaluate the results of the elective spigelian hernia repair as an ambulatory procedure.
Methods
From June 2007 to June 2010, 8 patients with 9 spigelian hernias were electively operated on under local anesthesia as a day case. Four patients had unilateral spigelian hernia, 1 had spigelian and inguinal on the same side, 1 had spigelian and epigastric, 1 had spigelian and umbilical, and 1 patient had bilateral spigelian and umbilical hernia. Spigelian hernia was managed by the “open preperitoneal flat mesh technique.” In patients with several ventral hernias at different sites, “the open preperitoneal flat mesh technique” was performed using one separate flat mesh for each of the hernias; for the patient with inguinal hernia, the Lichtenstein procedure was performed in addition.
Results
No complications and recurrences were recorded during a mean follow-up of 23.5 months (range: 11–35).
Conclusion
The elective spigelian hernia can be successfully repaired under local anesthesia as a day-case procedure. The “open preperitoneal flat mesh technique” provides excellent results under these conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spigelian hernias are rare and difficult to diagnose. Series of patients operated on for spigelian hernia are reported mostly in specialized, high volume centers. The treatment was previously limited to open surgical repair, whereas, recently, laparoscopic hernioplasty has become more frequent. Only a few series of patients with spigelian hernia managed on an outpatient basis have been reported in the literature [1, 2]. Ambulatory surgery for spigelian hernia can be based on the laparoscopic procedures under general or regional anesthesia [1, 3] or on the open techniques under local anesthesia [4–6]. A day-case surgery of spigelian hernia provides good results regardless of the type of the approach; however, laparoscopic procedures are performed in general or regional anesthesia.
Methods
In our prospective study, we analyzed a series of 8 consecutive patients with 9 spigelian hernia electively operated on in the ambulatory settings between June 2007 and June 2010. Six patients had hernia on the left side, 1 on the right, and 1 had bilateral spigelian hernia. Four patients had isolated unilateral spigelian hernia and 4 had a combination of spigelian and other hernia types (1 had spigelian and inguinal on the same side, 1 had spigelian and epigastric, 1 had spigelian and umbilical, and 1 had bilateral spigelian and umbilical hernia). Seven patients were diagnosed preoperatively by clinical examination, and abdominal wall CT was performed in 2 patients (4 patients reported pain, 3 patients reported reducible palpable mass, and 2 patients reported both), and 1 patient was diagnosed intraoperatively during the inguinal hernia repair. The indication for elective operation was symptomatic spigelian hernia in patients with ASA I-II-III status.
All hernioplasties were performed under local anesthesia using a combination of 20 ml 0.5 % levobupivacaine, 50 ml 2 % procaine, and 30 ml saline solution. Depending on the number of simultaneously repaired hernias, local anesthetic dose was multiplied one or two times. Nine spigelian hernias in 8 patients were managed with “the open preperitoneal flat mesh technique.” In patients with several ventral hernias at different sites (spigelian and epigastric, spigelian and umbilical and bilateral spigelian and umbilical hernia), a simultaneous “open preperitoneal flat mesh technique” was performed, using one separate flat mesh for each of the hernia. For the patient with spigelian and inguinal hernia on the same side, the simultaneous Lichtenstein procedure was performed through a single oblique incision. Regardless of the hernia number, all the patients were operated on as a day case under local anesthesia.
Surgical technique
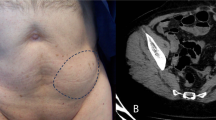
“The open preperitoneal flat mesh technique” for spigelian hernia is the following: an oblique skin and subcutaneous tissue incision are made above the spigelian hernia sac followed by the oblique incision of m.obliquus externus aponeurosis in the direction of its fibers; the spigelian hernia sac dissection up to the hernia neck is performed along with the dissection of m.obliquus externus from m.obliquus internus, 2–3 cm all round (dissection of the preperitoneal space is not performed); the hernia sac is repositioned into the abdominal cavity with its contents, without opening (when this is not possible, the hernia sac is entered and its contents released and then returned into the abdominal cavity; hernia sac is reconstructed with absorbable running suture and repositioned into the abdominal cavity); the polypropylene flat mesh overlapping the size of the hernia defect by 2–3 cm in all directions is positioned above the hernia sac and anchored with at least 8 mattress non-absorbable sutures; the mattress sutures are passed through the m.obliquus internus (medially through m.rectus abdominis) at 2–3 cm from the rim of the hernia defect and through the edge of the mesh and tied on the front fascia sides of both muscles; the hernia defect of the m.obliquus internus aponeurosis is closed by running absorbable suture, followed by closing the incision of the m.obliquus externus aponeurosis on the same principle. While for the umbilical and the epigastric hernia repair, the simultaneous operative technique is the same, for the spigelian hernia, it is somewhat different, in consideration of its specific anatomical characteristics (Fig. 1a–b).
All patients were operated on by a single surgeon. Parameters such as the size of hernia defect and duration of the operation, postoperative stay at the Day Surgery Unit and complications were registered and analyzed. After discharge from the hospital, all patients were followed up at the Day Surgery Unit after 1, 3, and 6 months and thereafter at 6-month intervals.
There were 6 male and 2 female patients (median age 61.5, range 24–83). Two patients were ASA I, four ASA II, and two patients were ASA III.
Results
The median size of the spigelian hernia defect was 3.3 cm (range: 2–5). The mean operative time for the patients operated on for unilateral spigelian hernia was 47 min (range: 30–70), and for the combination of several hernia types, it was 90 min (range: 70–130). The mean stay at the Day Surgery Unit for patients operated on for unilateral spigelian hernia was 2.3 h (range: 2–3), and for the combination of several hernia types, it was 2.9 h (range: 2–4). The mean postoperative follow-up was 23.5 months (range: 11–35). There were no postoperative complications or recurrences.
Discussion
Spigelian hernia can occur together with other types of abdominal wall hernia. There are published reports on rare cases of simultaneous bilateral spigelian and bilateral inguinal hernia, or bilateral spigelian hernia associated with umbilical and bilateral inguinal hernia [7, 8]. In a large series of 76 patients with 81 spigelian hernias reported by Larson and Farley [9], 11.8 % of the patients were simultaneously operated for other types of hernia (7 inguinal, 1 umbilical, and 1 femoral). In the series reported by Vos and Scheltinga [10], 25 patients were operated for spigelian hernia and 24 % of them had undergone previous operations for other types of hernia. In the present series, one half of the patients had one or more simultaneous operations for other types of hernia (2 patients had umbilical, 1 epigastric and 1 inguinal), which suggests collagen disease (herniosis) as a common denominator in all the patients.
Due to its infrequent occurrence, non-specific clinical presentation, and the fact that it is an interstitial hernia developing and presenting within the anterior abdominal wall, it is often necessary to perform ultrasound, CT, or MRI of the abdominal wall for more accurate diagnosis. [11] However, in the series reported by Vos and Scheltinga [10], the majority of the patients were operated without additional imaging techniques. In the present series, 2 patients required abdominal CT.
There is no consensus which operative technique is the best for the spigelian hernia repair. Spigelian hernia repair can be tension or tension-free, performed by the open or laparoscopic approach. The following techniques can be applied: (a) tissue repair [9, 12], (b) preshaped polypropylene umbrella plug [13], (c) flat mesh placement between the external oblique and the internal oblique muscles [4], (d) flat mesh in the preperitoneal space [3, 14], (e) Prolene Hernia System (the underlay patch is in the preperitoneal space, the connector as a plug in the parietal defect, and the onlay patch is above the internal oblique muscle) [5, 6], (f) laparoscopic transabdominal suture repair [15], (g) total extraperitoneal laparoscopic mesh repair [1, 3], and (h) laparoscopic intraperitoneal onlay mesh repair [3, 16–18]. The authors prefer “the open preperitoneal flat mesh technique” as a day-case procedure under local anesthesia [19, 20].
The advantage of mesh repair over suture repair for small ventral and incisional hernias was demonstrated by Luijendijk et al. [21] and Burger et al. [22].
The intra-abdominally invaginated hernia sac for mesh placement in spigelian hernia repair has been used by other authors as well. Sanchez-Montes and Deysine [13] inserted a preshaped polypropylene umbrella-type plug into the intra-abdominally repositioned hernia sac and anchored it to the hernia ring under local anesthesia in ambulatory conditions. George et al. [23] positioned an inlay polypropylene patch and fixed it to the rim of the hernia defect under general anesthesia in the hospital setting. The polypropylene mesh (plug or patch) is in the inlay position, while in “the open preperitoneal flat mesh technique,” it is in the underlay position, with mesh/hernia defect overlapping 2–3 cm in all directions. In both aforementioned techniques, only the external oblique muscle aponeurosis is sutured over the mesh at the end of the procedure. In “the open preperitoneal flat mesh technique,” the suture of hernia defect at the level of the internal oblique muscle is followed by the suture of the external oblique muscle aponeurosis. Eight non-resorbable transparietal sutures anchoring the mesh and mesh/hernia defect overlapping 2–3 cm in all directions with complete anterior myofascial support provide additional strength to the hernioplasty. Since the median size of the hernia defect in the present series was 3.3 cm, a 2–3 cm mesh/hernia defect overlapping was sufficient for the open spigelian hernioplasty. Moreno-Egea et al. [3] and Richards [24] reported 3 cm mesh/hernia defect overlapping sufficient for the open preperitoneal hernioplasty. In laparoscopic spigelian hernioplasty, Moreno-Egea et al. [1] and Saber et al. [18] recommend at least 3 and 3–5 cm mesh/hernia defect overlapping. Other authors reported good results in the management of small ventral and incisional hernias using PHS, Proceed Ventral Patch, and Ventralex although the mesh/hernia defect overlapping was less then 5 cm [6, 25–27].
The authors of this study would manage large and/or incarcerated spigelian hernias by open or laparoscopic hernioplasty in regional or general anesthesia with the mesh positioned between external and internal oblique muscle providing at least 5 cm mesh/hernia defect overlapping.
In the published literature, series of patients with spigelian hernia managed in the ambulatory settings are infrequent [1, 2]. These are usually individual case reports of laparoscopic spigelian hernia repair under general anesthesia [7, 8, 15]. Larger series of patients managed by laparoscopic techniques under general or regional anesthesia, or with open techniques under local anesthesia as a day case are even more rarely reported [1–3, 13].
Local anesthesia in hernia repair is an ideal solution for both the patient (local analgesia, with minimal incidence of urinary retention) and the ambulatory surgery (no systemic effects, no motor block) [28, 29]. In the ambulatory settings, local anesthesia has great advantages over both general and regional anesthesia [30].
Jeekel [31] reported at the Joint Meeting of the EHS and AHS in Berlin 2010 Level 1 evidence data that indicate significantly reduced morbidity with local anesthesia.
The advantage of “the open preperitoneal flat mesh technique” for spigelian hernia repair is as follows: (a) it is as easy to learn as it is to perform by general surgeons or residents; (b) reduced operative time and complications due to minimal dissection using the hernia sac for mesh positioning; (c) it is feasible in all general surgical hospitals; (c) does not require any special surgical equipment (no laparoscopic or other special instruments); (d) the cost–benefit procedure (material used: all kinds of small size polypropylene mesh, monofilament sutures, and local anesthetics); (e) suitable for simultaneous repair of some inguinal and simple ventral abdominal wall hernias at different sites; (f) local anesthesia is applicable to almost all patients regardless of comorbidities; (g) safe procedure in ambulatory settings providing excellent results in elective spigelian hernia surgery.
In conclusion, the “open preperitoneal flat mesh technique” is an excellent technique for elective spigelian hernia repair as a day-case procedure under local anesthesia.
References
Moreno-Egea A, Aquayo JL, Girela E (2002) Treatment of spigelian hernia using totally extraperitoneal laparoscopy ambulatory surgery. Surg Endosc 16(12):1806
Zaragoza C, Peiró F, Bebek H et al (2001) Spiegelian hernia: ambulatory surgical treatment. Ambul Surg 9(3):127–129
Moreno-Egea A, Carrasco L, Girela E et al (2002) Open vs laparoscopic repair of spigelian hernia. A prospective randomized trial. Arch Surg 137:1266–1268
Celdrán A, Señaris J, Mañas J, Frieyro O (2007) The open mesh repair of Spigelian hernia. Am J Surg 193(1):111–113
Licheri S, Pisano G, Pintus M et al (2004) The treatment of Spigelian hernia with the Prolene Hernia System: notes on techniques. Chir Ital 56(2):265–270
Campanelli G, Pettinari D, Nicolosi FM, Avesani EC (2005) Spigelian hernia. Hernia 9(1):3–5
Gedebou TM, Neubauer W (1998) Laparoscopic repair of bilateral spigelian and inguinal hernias. Surg Endosc 12:1424–1425
Wiedeman JE, Clay J (2008) Letters to the editors: the open mesh repair of Spigelian hernia. Am J Surg 19:460–462
Larson DW, Farley DR (2002) Spigelian hernias: repair and outcome for 81 patients. World J Surg 26:1277–1281
Vos DI, Scheltinga MRM (2004) Incidence and outcome of surgical repair of spigelian hernia. Br J Surg 91:640–644
Toms AP, Dixon AK, Murphy JMP, Jamieson NV (1999) Illustrated review of new imaging techniques in the diagnosis of abdominal wall hernias. Br J Surg 86:1243–1249
Spangen L (1984) Spigelian hernia. Surg Clin N Am 64:351–366
Sanchez-Montes I, Deysine M (1998) Spigelian hernias: a new repair technique using preshaped polypropylene umbrella plugs. Arch Surg 133(6):670–672
Malazgirt Z, Dervisoglu A, Polat C et al (2003) Preperitoneal mesh repair of Spigelian hernias under local anesthesia: description and clinical evaluation of a new technique. Hernia 7:202–205
Bittner JG, Edwards MA, Shah MB et al (2008) Mesh-free laparoscopic spigelian hernia repair. Am Surg 74:713–720
Appeltans BM, Zeebregts CJ, Cate Hoedemaker HO (2000) Laparoscopic repair of a Spigelian hernia using an expanded polytetrafluoroethylene (ePTFE) mesh. Surg Endosc 14(12):1189
Barie PS, Thompson WA, Mack CA (1994) Planned laparoscopic repair of a spigelian hernia using a composite prosthesis. J Laparoendosc Surg 4:359–363
Saber AA, Elgamal MH, Rao A et al (2008) Laparoscopic spigelian hernia repair: the scroll technique. Am Surg 2(74):108–112
Žuvela M, Milićević M, Galun D et al (2006) Ambulatory surgery of umbilical, epigastric and small incisional hernias: open preperitoneal flat mesh technique in local anaesthesia. Acta Chir Iugosl 53:29–34
Galun D, Žuvela M, Djurić-Stefanović A et al (2009) Spigelian hernia repair as a day case procedure. 4th joint hernia meeting, joint meeting of the AHS and EHS, Berlin 2009. Hernia 13(Suppl 1):S97
Luijendijk R, Hop W, van den Tol P et al (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 343:392–398
Burger JW, Roland A, Luijendijk RW et al (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–585
George C, Tauro LF, Dsouza C et al (2009) Spigelian hernia. JCDR 3(2):1437–1440
Richards AT (2004) Spigelian hernias. Oper Tech Gen Surgery 6(3):228–239
Tollens T, Struyve D, Aelvoet C, Vanrijekel JP (2010) Introducing the proceed ventral patch as a new device in surgical management of umbilical and small ventral hernias: preliminary results. Surg Technol Int 19:99–103
Bastidas JG, Khan AR, LeBlanc KA (2010) Spigelian hernia as a cause of small bowel obstruction. South Med J 103(6):567–569
Iversen E, Lykke A, Hensler M, Jorgensen LN (2010) Abdominal wall hernia repair with a composite ePTFE/polypropylene mesh: clinical outcome and quality of life in 152 patients. Hernia 14:555–560
Glassow F (1984) Inguinal hernia repair using local anaesthesia. Ann R Coll Surg Engl 66:382–387
Amid PK, Schulman AG, Lichtenstein IL (1994) Local anesthesia for inguinal hernia repair: step-by-step procedure. Ann Surg 220:735–737
Young DV (1987) Comparison of local, spinal, and general anesthesia for inguinal herniorrhaphy. Am J Surg 153:560–563
Jeekel J (2009) 50 years mesh in hernia: we did improve our results? 4th joint hernia meeting, joint meeting of the AHS and EHS, Berlin 2009. Hernia 13(Suppl 1):S58
Conflict of interest
This study was not funded by any individual or institution. The authors disclose no potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zuvela, M., Milicevic, M., Galun, D. et al. Spigelian hernia repair as a day-case procedure. Hernia 17, 483–486 (2013). https://doi.org/10.1007/s10029-012-1002-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-012-1002-6