Abstract
Psychotic disorders typically manifest from late adolescence to early adulthood, and an earlier onset might be associated with greater symptom severity and a worse long-term prognosis. This study aimed to compare the cognitive characteristics of patients with first-episode psychosis (FEP) by their age at onset. We included 298 patients diagnosed with FEP and classified them as having an early onset (EOS), youth onset (YOS), or adult onset (AOS) based on age limits of ≤ 18 years (N = 61), 19–24 years (N = 121), and ≥ 25 years (N = 116), respectively. Socio-demographic and clinical variables included age at baseline, gender, socio-economic status, antipsychotic medication, DSM-IV diagnoses assessed by clinical semi-structured interview, psychotic symptom severity, and age at onset. Neuropsychological assessment included six cognitive domains: premorbid intelligence, working memory, processing speed, verbal memory, sustained attention, and executive functioning. The EOS group had lower scores than the YOS or AOS groups in global cognition, executive functioning, and sustained attention. Although the scores in the YOS group were intermediate to those in the EOS and AOS groups for most cognitive factors, no statistically significant differences were detected between the YOS and AOS groups. Age at onset results in specific patterns of cognitive interference. Of note, impairment appears to be greater with EOS samples than with either YOS or AOS samples. A longitudinal study with a larger sample size is needed to confirm our findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psychotic disorders, which typically develop from late adolescence to early adulthood, are severe mental disorders that have a considerable impact on the lives of both patients and their families [1,2,3]. The outcome of patients diagnosed with first psychotic episode (FEP) is highly variable, and although remission is achieved in 58% of the cases, recovery is only achieved in 38% [4]. The duration of untreated psychosis, poor premorbid adjustment, the severity of negative symptoms, the comorbidity of substance abuse and the diagnosis of a non-affective psychotic disorder are variables which influence the patient’s outcome [5].
Most studies divide psychotic disorders by age at onset, with onset before age 18 years considered early onset (EOS) and onset after 18 years considered adult onset (AOS) [6]. Thus, while EOS includes patients with a limited age range, AOS generally includes samples from 18 to late adulthood, which does not differentiate between very young adults and much older adult patients.
When developing in adolescence and young adulthood, psychotic disorders can interfere with normal maturation [7] and socio-functional development [8]. Not all studies into how age at onset affects clinical outcomes have observed significant differences between EOS and AOS [9], but most agree that patients with EOS have worse premorbid adjustment, longer duration of untreated psychosis, more negative symptoms, higher suicidality, more depressive symptoms, and higher prevalence of cannabis use than patients with an AOS [10,11,12,13]. Moreover, some studies suggest that an earlier age at onset may be associated with higher genetic loading [14], greater cognitive deficits [15], and lower responsiveness to cognitive training [16]. Research among adults also suggests that age at onset may be significant. Chen et al. compared patients diagnosed with a schizophrenia spectrum disorder and young (< 26 years), middle (26–40 years), and late (> 40 years) adult onsets. They observed that older onsets were associated with lower rates of substance abuse, better psychosocial functioning, and a higher educational achievement [17].
Regarding cognition, there is strong evidence that patients diagnosed with either an EOS [18, 19] or an AOS [20, 21] psychotic disorder have global cognitive difficulties. Moreover, these difficulties have been associated with worse functional outcomes [22, 23], and for this reason, are considered potential treatment targets [24]. Studies analyzing differences in cognition between EOS and AOS offer conflicting results, probably due to different methodological approaches. Some studies have only included adult samples (sometimes with a long illness duration), splitting them retrospectively into EOS and AOS. However, the longer duration fosters bias due to the interference of other variables, such as antipsychotic medication or symptom chronicity, on cognitive performance.
To our knowledge, only three studies have directly compared cognitive domains in EOS and AOS following FEP [25,26,27], and in all three cases, the studies were conducted in non-affective psychosis patients and more than a year had elapsed between onset and assessment. Biswas et al. studied a group of 15 children, 20 adolescents, and 20 adults with schizophrenia and observed that the children showed lower scores than the other groups in intelligence quotient, memory, and perceptuomotor skills [25]. Moreover, adolescents experienced greater difficulties in intelligence and memory than adults. Holmen et al. compared executive function in 20 EOS patients, 90 AOS patients, 66 healthy adolescents, and 127 healthy adults. They observed that both patient groups (EOS and AOS) had significantly poorer executive functions than healthy controls, but reported no significant differences between the EOS and AOS groups [26]. Finally, White et al. included 49 patients with EOS schizophrenia spectrum disorder, 139 with AOS schizophrenia spectrum disorder, 32 healthy adolescents, and 204 healthy adults. In this comparison, the EOS group performed worse than the AOS group in working memory, language, and motor function tasks, but the healthy adolescents also performed significantly worse than the healthy adults in working memory and language. Thus, they concluded that only differences in motor function between the EOS and AOS groups were due to the age at onset [27]. However, these studies have important methodological limitations, including assessment only after long disorder durations, assessment limited to specific cognitive functions, and the inclusion of EOS groups with mean ages close to adulthood. A final study worth noting is that by Tuulio-Henriksson et al., which reported that earlier onset among adults older than 18 years was associated with greater impairments in verbal learning and memory [28].
As evidenced, few studies have directly assessed cognitive function by comparing EOS and AOS at a FEP when interference from psychotic symptoms and antipsychotic medications are less marked. There is also a scarcity of research that divides AOS groups into young and adult onset to study the influence of age on cognition. In this study, we, therefore, aimed to compare the cognitive characteristics of patients diagnosed with a FEP by three ages of onset: EOS, young adult onset (YOS), and AOS. We hypothesized that an EOS would be associated with the most severe pattern of cognitive difficulties, followed by an intermediate profile for a YOS, and the least severe profile for an AOS.
Methods
This is part of the “Phenotype-Genotype and Environmental Interaction: Application of a Predictive Model in First Psychotic Episodes (PEPs) Study” [29]. The broader PEPs study is a multicenter, naturalistic, and longitudinal study assessing the clinical neuropsychological and psychosocial functioning variables in a cohort with FEP performed through the Biomedical Research Network Center for Mental Health. Patients were assessed at baseline and at 2, 6, 12, and 24 months. A complete description of the methodology has been published elsewhere [29].
This study was conducted in accordance with the ethical principles of the Declaration of Helsinki, Good Clinical Practice, and Hospital Clinic Ethics and Research Board. All participants and all parents/legal guardians of subjects younger than 18 years provided written informed consent before inclusion.
Sample
All participants were recruited in Spain from 2009 to 2011. The following inclusion criteria were used: (a) age 7–35 years at the time of the evaluation; (b) a psychotic disorder of less than 12 months’ duration, according to DSM-IV criteria; (c) being fluent in Spanish; and (d) provision of written informed consent. We excluded those with an intellectual disability according to DSM-IV criteria (including both an IQ below 70 and impaired functioning), a history of head trauma with loss of consciousness, and organic disease with mental repercussions. This resulted in the inclusion of 335 patients with FEP. However, only those who completed at least one cognitive domain were considered, giving a final sample of 298 patients. Based on previous literature [6] we considered as EOS all those subjects with a diagnosis of psychotic disorder under 18 years. Unfortunately, there is no agreement about how to divide the AOS sample. Following the studies conducted by Kessler et al. and McGorry et al., where both authors concluded that 75% of subjects diagnosed with a psychiatric disorder received the diagnosis before the age of 25 [30, 31], we chose 24 as the cut-off to divide between YOS and AOS. Thus, among the 298 patients, 61 were classified as EOS (age ≤ 18 years), 121 were classified as YOS (age 19–24 years), and 116 were classified as AOS (age ≥ 25 years).
Socio-demographic and clinical assessment
Baseline socio-demographic and clinical data were systematically collected and analyzed for all participants. Socio-demographic data included age, sex, and parental socio-economic status (SES), as estimated using the Hollingshead Scale [32]. Diagnosis at 12-month follow-up was taken into account to ensure diagnostic stability. Clinical variables included:
-
Diagnoses according to DSM-IV criteria were determined using the Spanish versions of the Structured Clinical Interview for DSM I-IV Axis I disorders (SCID-I) [33] or the Schedule for Affective Disorders and Schizophrenia for School-Aged Children (K-SADS) [34], depending on age. The SCID-I and K-SADS are reliable for assessing psychopathology in adults and adolescents. They were administered by trained psychiatrists or psychologists.
-
Pharmacological treatment was assessed as the prescribed daily antipsychotic dose converted to the estimated chlorpromazine equivalents (CPZe), following international consensus guidelines [35].
-
The severity of psychotic symptoms was assessed with the validated Spanish version of the Positive and Negative Syndrome Scale (PANSS) in schizophrenia [36]. The PANSS is a 30-item rating scale subdivided into three subscales (positive symptoms, negative symptoms, and general psychopathology) with a total score. Each subscale is evaluated from 1 to 7 according to the severity of the symptoms.
-
Age at onset was assessed using the Symptom Onset in Schizophrenia (SOS) inventory [37], which considers information given by patients and family members. In the event of a discrepancy between family members and patients, interviewers used their clinical judgment to make a decision.
-
Family history of psychotic disorders was determined on the basis of an interview with the parents or legal guardians which included questions about first- and second-degree relatives.
-
Substance abuse was assessed with the European Adaptation of the Multidimensional Assessment Instrument for Drug and Alcohol Dependence scale [38].
Cognitive assessment
Cognitive assessment was conducted in the two-month follow-up visit to ensure psychopathologic stability of patients. The test battery included standardized neuropsychological tests that have been validated in Spanish. They encompassed the cognitive dimensions included in the MATRICS battery, except for social cognition. The neuropsychological tests were grouped into the following domains:
-
Estimated premorbid intelligence quotient (IQ), assessed with the vocabulary sub-test from the Wechsler Intelligence Scale for Children IV (WISC-IV) [39] or the Wechsler Adult Intelligence Scale III (WAIS-III)[40], depending on age.
-
Working Memory included the Digit Span and the Letter and Number sequencing sub-tests of the WISC-IV [39] or WAIS-III [40].
-
Processing speed was assessed with the Trail Making Test form A [TMT-A] [41] and two parts of the Stroop test (reading speed of words and colors) [42].
-
Sustained attention was tested with the following variables of the Continuous Performance Test-II [43]: omissions, commissions, hit reaction time, perseverations, variability, and detectability.
-
Verbal Memory was assessed with the Spanish version of the California Verbal Learning Test (the Spanish Complutense Verbal Learning Test). Immediate and delayed recall were included in this domain [44].
-
Executive function variables included errors, perseverative errors, non-perseverative errors, and number of categories from the Wisconsin Card Sorting Test (WCST) [45], the Trail Making Test form B (TMT-B) [41], the interference score from the Stroop Test [42], and the F-A-S test [46].
-
A global cognition score derived from the mean of all cognitive domains, except the premorbid IQ, was also calculated.
A detailed description of the cognitive assessment and the derived cognitive domains is reported elsewhere [47].
Statistical analyses
Inter-rater reliability was assessed for neuropsychological tests liable to variability (vocabulary of the WAIS-III and WCST). Ten cases per test were sent to researchers for correction and we compared these results against gold standards derived from the consensus of three expert evaluators in administration and correction. Interclass correlation coefficients (ICCs) were calculated for each test. Evaluators who did not reach the established cut-off point (ICC > 0.80) had to repeat the process. There was agreement among 90% of the neuropsychologists.
Although all neuropsychological tests were standardized and validated for the Spanish population, not all tests were standardized for all age ranges because the study covered ages 12–35 years. Thus, all cognitive variables were transformed into standard equivalents (z scores: mean = 0; SD = 1) based on data from a control group matched by age and sex [48]. The socio-demographic characteristics of the control group are detailed in the supplementary material (Section and Table S1). Age at baseline was included as a covariate in the analyses to control for normative developmental differences between groups. The scores for cognitive domains were calculated by averaging the z scores of the neuropsychological tests included in each domain. The global cognitive score was calculated by averaging scores of all cognitive domains except for premorbid IQ [47]. Higher scores indicated better performance.
Neuropsychological variables were evaluated using the Kolmogorov–Smirnov test to confirm the normality of the sample distribution. The Levene test was also used to assess the equality of variances. To compare socio-demographic and clinical differences between groups (EOS, YOS and AOS), categorical variables were analyzed using the chi-square Test and continuous variables were compared by analysis of covariance (ANCOVA). Differences between groups in cognitive variables were assessed via ANCOVA, using age, sex, SES, CPZe, and total PANSS score at baseline as covariates. Bonferroni correction for multiple comparisons was applied. All tests were two tailed, significance was set at p < 0.05, and analysis was performed using IBM SPSS version 23.0 (IBM Corp., Armonk, NY, USA).
Results
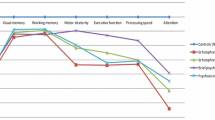
Baseline data are shown by age of onset in Table 1. As shown, no significant differences were observed between the EOS, YOS and AOS groups in socio-demographic or clinical variable other than age and age at onset. We then analyzed differences in cognitive domains between groups, including age at baseline as a covariate, and these results are shown in Table 2 and Fig. 1. The presence of current or past psychopathology (other than psychotic disorders), tobacco use, sex, SES, total PANSS score at baseline, and the CPZe were also included as covariates in the model to ensure that differences between groups were not due to the effect of these variables. Significant differences were observed in sustained attention, executive function, and global cognition scores. For each variable, the EOS group obtained lower scores than either the YOS or AOS groups; however, although the YOS group had lower scores than the AOS group in all cognitive functions except processing speed, we observed no statistically significant differences. The influence of covariates on cognitive variables as well as the specific role of age can be found in the supplementary material (section and Tables S2, S3, S4 and S5).
Discussion
This is one of only a few studies to have directly compared cognitive domains in patients with EOS and AOS, in which the adult sample is further subdivided into YOS and AOS groups, to study the role of age of onset with greater nuance. The results show that EOS FEP patients have lower scores in global cognition, executive functioning, and sustained attention compared with either YOS or AOS FEP. Contrary to our initial hypothesis, however, no statistical differences were observed between YOS and AOS FEP.
There is strong evidence of difficulties in both executive function and sustained attention for patients with EOS and AOS samples [19,20,21, 49,50,51,52]. Attention and executive functioning improve during adolescence [53, 54] and are associated with frontal and pre-frontal areas, which are the last brain areas to mature [7]. Thus, executive functioning improves from adolescence and reaches an adult level at age 20 years [54]. Sustained attention progressively increases during adolescence, when using the Continuous Performance Test reveals a decrease in the number of omissions and the reaction time until age 15 [53]. Thus, an FEP during this key period in adolescence could interrupt or at least delay the normal development of both cognitive functions.
Previous studies comparing EOS and AOS directly in samples with FEP have offered widely varying results [25,26,27]. Some have observed significant differences between groups in intelligence [25], memory [25], or motor skills [27], while others have not [26]. Discrepancies between these studies and ours may be due to methodological differences concerning the assessment of specific cognitive functions or the time lapse between cognitive assessment and symptom onset, which was ≥ 1 year in some cases.
A meta-analysis by Rajji et al. compared cognitive difficulties in youth-onset schizophrenia (< 19 years), late-onset schizophrenia (> 40 years), and adults with FEP (19–40 years) [15]. They concluded that individuals with youth-onset had larger deficits than adults with an FEP in their executive function, IQ, psychomotor speed, and verbal memory. The youth-onset group was also more impaired than late-onset group in both executive function and attention. However, the adults with an FEP showed larger deficits in attention, full-scale IQ, and global cognition than the patients with late-onset schizophrenia. Although we found no significant differences between the YOS and AOS groups in our study, Fig. 1 does show a similar pattern to that described by Rajji et al., with scores increasing in the order EOS (lowest), YOS (intermediate), and AOS (highest) for all cognitive functions except premorbid IQ. Interestingly, Rajii et al. included patients with a wide age range up to 60 years, suggesting that our age range (12–35 years) was insufficiently wide to detect differences between YOS and AOS FEP [15].
Age at onset is an important factor to consider when studying psychiatric disorders, but its role has been mainly analyzed in adults with a long disorder duration. In these patients, we cannot exclude the influence of antipsychotic medications and chronic psychotic symptoms. Indeed, when Hilker et al. studied the relationship between age at onset and risk of schizophrenia spectrum disorders using data from the Danish Psychiatric Central Research register, they observed diagnosing one twin with schizophrenia under the age of 22 years increases the risk in the other twin fivefold [14]. An EOS, therefore, seems to be linked to a greater genetic component or predisposition. Moreover, some studies have associated earlier ages of onset to worse courses of illness, family history of psychosis, and increased risk in siblings [12, 55]. Together, these findings suggest an association between an earlier age of onset and a higher genetic load.
An EOS of FEP has a particularly meaningful impact on individuals due to the period of life when it occurs. Adolescence is not only a time where brain undergoes dramatic changes [7] but also a period characterized by changes affecting psychological and social development [8]. The presence of psychotic symptoms interrupting normal maturational and developmental processes in adolescence may create a more severe psychotic disorder characterized by a worse outcome and greater cognitive difficulties. Interestingly, executive function and sustained attention are cognitive domains that improve significantly during adolescence [53, 54], and onset during this period may specifically interfere with their development. Longitudinal studies comparing EOS, YOS, and AOS are needed to assess if the evolution of cognitive function differs by the age at onset.
Our results have a clear practical application, namely they can be used to support early interventions to maximize the benefit of psychiatric and psychological treatments. Nowadays, specific cognitive remediation programs exist, which have demonstrated their efficacy in improving cognitive functions in adolescents [16], despite evidence that they respond less in areas such as verbal memory compared with adults [16]. Other research among adults has shown that age moderates the effect of cognitive training on cognitive outcomes, with younger adults showing greater improvement than older subjects [56]. Thus, age at onset may be considered an important variable when planning cognitive interventions.
Additional methodological points should be taken into account when interpreting the results of this paper. All statistical analyses were performed including SES, CPZe levels, PANSS score and age. Moreover, age was considered as a categorical variable rather than a continuous variable. Lower parental socio-economic status (SES) has been associated with lower cognitive functioning both in child/adolescent [57,58,59] and adult samples [60]. Lower parental SES has also been linked to a higher risk of developing psychotic disorders [61, 62]. In our study, parental SES was significantly associated with all measures of cognitive functioning except verbal memory (section S2 and table S2 in the supplementary material section). Nevertheless, even if we include SES as covariate, the group variable (EOS, YOS and AOS) remained significant. Regarding the inclusion of CPZe levels as covariate, there is no agreement as to the effects of antipsychotic medication on cognition. A recent meta-analysis by Prates Baldez et al. observed that the effects of antipsychotics on cognitive functioning are not uniform [63]. Thus, when more than one antipsychotic medication is used in the same study, it is imperative to convert different antipsychotic doses into a single measure. There is no single method to calculate dose equivalents. In this study we followed the consensus established by Gardner et al. 2010, which provides one of the most complete estimates of equivalencies and specific clinical scenarios. Finally, age of patients was considered as a categorical variable instead of a continuous variable. Previous literature has shown that, in terms of maturational and cognitive development, childhood, adolescence and adulthood are quite different. Thus, between 5 and 20 years of age, most cognitive functions improve due to normal maturational processes with a peak of growth between 10 and 15 years of age [53, 54, 64,65,66]. To show this difference we included age as a discrete variable. A complete analysis of the role of these three variables in our results can be found in supplementary material sections and Tables S1, S2, S3 and S4.
This study has some limitations that must be taken into account. First, although 298 patients with an FEP were included, we divided those patients into three groups, thereby reducing the relative sample sizes of those groups. To control for the effect of covariates (The presence of current and past psychopathology, tobacco use, age, sex, SES, severity of psychotic symptoms, and CPZe), these were included in the statistical analyses and Bonferroni correction was applied. As a consequence, we may have lost some significant differences between groups due to a lack of statistical power. Second, previous research has clearly defined age at onset prior to 18 years as the cut-off for EOS FEP, but to our knowledge, no general consensus exists about the optimal point to divide samples into YOS and AOS. Our cut-off limit set at 25 years old is therefore arbitrary. A theoretical model with three sub-groups (age at onset of 17, 27, and 46 years) has been discussed in a recent study [67] and no accurate threshold for age at onset was identified to define valid sub-groups. However, given that McGorry et al. concluded that 75% of mental illness emerged before the age of 25 years, we considered this a good cut-off point [31]. Third, the age range of patients with FEP was 7–35 years in this study, and as such, does not include late-onset psychosis. This may have prevented us from identifying significant differences between the YOS and AOS groups. Furthermore, there is no direct comparison with a healthy control group to control for possible confounders due to normal developmental processes. Finally, the cross-sectional study design means that no conclusions can be drawn regarding the evolution over time.
In conclusion, we observed that patients with EOS FEP have greater impairments in executive function and sustained attention than either YOS or AOS groups. Although this suggests that age at onset interferes specifically in cognition, longitudinal studies are needed to assess if the early onset of psychotic symptoms also interfered with its normal development.
References
Kessler RC, Amminger GP, Aguilar-Gaxiola S et al (2007) Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry 20:359–364. https://doi.org/10.1097/YCO.0b013e32816ebc8c
Wong C, Davidson L, McGlashan T et al (2008) Comparable family burden in families of clinical high-risk and recent-onset psychosis patients. Early Interv Psychiatry 2:256. https://doi.org/10.1111/J.1751-7893.2008.00086.X
Saarni S, Viertiö S, Perälä J et al (2010) Quality of life of people with schizophrenia, bipolar disorder and other psychotic disorders. Br J Psychiatry 197:386–394. https://doi.org/10.1192/BJP.BP.109.076489
Lally J, Ajnakina O, Stubbs B et al (2017) Remission and recovery from first-episode psychosis in adults: systematic review and meta-analysis of long-term outcome studies. Br J Psychiatry 211:350–358. https://doi.org/10.1192/BJP.BP.117.201475
Suvisaari J, Mantere O, Keinänen J et al (2018) Is it possible to predict the future in first-episode psychosis? Front Psychiatry. https://doi.org/10.3389/FPSYT.2018.00580
McClellan J, Stock S (2013) Practice parameter for the assessment and treatment of children and adolescents with schizophrenia. J Am Acad Child Adolesc Psychiatry 52:976–990. https://doi.org/10.1016/j.jaac.2013.02.008
Gogtay N, Giedd JN, Lusk L et al (2004) Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci USA 101:8174–8179. https://doi.org/10.1073/pnas.0402680101
Blakemore S-J, Mills KL (2014) Is adolescence a sensitive period for sociocultural processing? Annu Rev Psychol 65:187–207. https://doi.org/10.1146/annurev-psych-010213-115202
Amminger GP, Henry LP, Harrigan SM et al (2011) Outcome in early-onset schizophrenia revisited: findings from the early psychosis prevention and intervention centre long-term follow-up study. Schizophr Res 131:112–119. https://doi.org/10.1016/j.schres.2011.06.009
Ballageer T, Malla A, Manchanda R et al (2005) Is adolescent-onset first-episode psychosis different from adult onset? J Am Acad Child Adolesc Psychiatry 44:782–789. https://doi.org/10.1097/01.chi.0000164591.55942.ea
Joa I, Johannessen JO, Langeveld J et al (2009) Baseline profiles of adolescent vs. adult-onset first-episode psychosis in an early detection program. Acta Psychiatr Scand 119:494–500. https://doi.org/10.1111/j.1600-0447.2008.01338.x
Rabinowitz J, Levine SZ, Häfner H (2006) A population based elaboration of the role of age of onset on the course of schizophrenia. Schizophr Res 88:96–101. https://doi.org/10.1016/j.schres.2006.07.007
Coulon N, Godin O, Bulzacka E et al (2020) Early and very early-onset schizophrenia compared with adult-onset schizophrenia: French FACE-SZ database. Brain Behav 10:1–13. https://doi.org/10.1002/brb3.1495
Hilker R, Helenius D, Fagerlund B et al (2017) Is an early age at illness onset in schizophrenia associated with increased genetic susceptibility? Analysis of data from the nationwide Danish twin register. EBioMedicine 18:320–326. https://doi.org/10.1016/j.ebiom.2017.04.002
Rajji TK, Ismail Z, Mulsant BH (2009) Age at onset and cognition in schizophrenia: meta-analysis. Br J Psychiatry 195:286–293. https://doi.org/10.1192/bjp.bp.108.060723
Puig O, Fisher M, Loewy R et al (2020) Early-versus adult-onset schizophrenia as a predictor of response to neuroscience-informed cognitive training. J Clin Psychiatry. https://doi.org/10.4088/JCP.18m12369
Chen L, Selvendra A, Stewart A, Castle D (2018) Risk factors in early and late onset schizophrenia. Compr Psychiatry 80:155–162. https://doi.org/10.1016/j.comppsych.2017.09.009
Zabala A, Rapado M, Arango C et al (2010) Neuropsychological functioning in early-onset first-episode psychosis: comparison of diagnostic subgroups. Eur Arch Psychiatry Clin Neurosci 260:225–233. https://doi.org/10.1007/s00406-009-0046-9
Bombin I, Mayoral M, Castro-Fornieles J et al (2013) Neuropsychological evidence for abnormal neurodevelopment associated with early-onset psychoses. Psychol Med. https://doi.org/10.1017/S0033291712001535
Uren J, Cotton SM, Killackey E et al (2017) Cognitive clusters in first-episode psychosis: overlap with healthy controls and relationship to concurrent and prospective symptoms and functioning. Neuropsychology 31:787–797. https://doi.org/10.1037/neu0000367
Mesholam-Gately RI, Giuliano AJ, Goff KP et al (2009) Neurocognition in first-episode schizophrenia: a meta-analytic review. Neuropsychology 23:315–336. https://doi.org/10.1037/a0014708
Puig O, Penadés R, Baeza I et al (2012) Processing speed and executive functions predict real-world everyday living skills in adolescents with early-onset schizophrenia. Eur Child Adolesc Psychiatry. https://doi.org/10.1007/s00787-012-0262-0
McGorry PD, Nelson B, Markulev C et al (2017) Effect of ω-3 polyunsaturated fatty acids in young people at ultrahigh risk for psychotic disorders: The NEURAPRO randomized clinical trial. JAMA Psychiat 74:19–27. https://doi.org/10.1001/jamapsychiatry.2016.2902
Wykes T, Joyce E, Velikonja T et al (2018) The CIRCuiTS study (implementation of cognitive remediation in early intervention services): protocol for a randomised controlled trial. Trials 19:1–12. https://doi.org/10.1186/s13063-018-2553-3
Biswas P, Malhotra S, Malhotra A, Gupta N (2006) Comparative study of neuropsychological correlates in schizophrenia with onset in childhood, adolescence and adulthood. Eur Child Adolesc Psychiatry 15:360–366. https://doi.org/10.1007/s00787-006-0542-7
Holmén A, Juuhl-Langseth M, Thormodsen R et al (2012) Executive function in early-and adult onset schizophrenia. Schizophr Res 142:177–182. https://doi.org/10.1016/j.schres.2012.10.006
White T, Ho BC, Ward J et al (2006) Neuropsychological performance in first-episode adolescents with schizophrenia: a comparison with first-episode adults and adolescent control subjects. Biol Psychiatry 60:463–471. https://doi.org/10.1016/j.biopsych.2006.01.002
Tuulio-Henriksson A, Partonen T, Suvisaari J et al (2004) Age at onset and cognitive functioning in schizophrenia. Br J Psychiatry 185:215–219. https://doi.org/10.1192/bjp.185.3.215
Bernardo M, Bioque M, Parellada M et al (2013) Assessing clinical and functional outcomes in a gene-environment interaction study in first episode of psychosis (PEPs). Rev Psiquiatr Salud Ment 6:4–16. https://doi.org/10.1016/j.rpsm.2012.11.001
Kessler RC, Berglund P, Demler O et al (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National comorbidity survey replication. Arch Gen Psychiatry 62:593–602
McGorry PD, Mei C (2018) Early intervention in youth mental health: progress and future directions. Evid Based Ment Health 21:182–184
Hollingshead A, Redlich F (1958) Social class and mental illness. Wiley, New York
First M, Spitzer R, Gibbon M, Willimans J (1997) Structured clinical interview for DSM-IV axis I disorders, clinician version (SCID-CV). American Medical Association, Washington DC
Kaufman J, Birmaher B, Brent D et al (1997) Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988. https://doi.org/10.1097/00004583-199707000-00021
Gardner DM, Murphy AL, O’Donnell H et al (2010) International consensus study of antipsychotic dosing. Am J Psychiatry 167:686–693. https://doi.org/10.1176/appi.ajp.2009.09060802
Peralta V, Cuesta MJ (1994) Psychometric properties of the positive and negative syndrome scale (PANSS) in schizophrenia. Psychiatry Res 53:31–40. https://doi.org/10.1016/0165-1781(94)90093-0
Perkins DO, Leserman J, Jarskog LF et al (2000) Characterizing and dating the onset of symptoms in psychotic illness: the symptom onset in schizophrenia (SOS) inventory. Schizophr Res 44:1–10. https://doi.org/10.1016/S0920-9964(99)00161-9
Kokkevi A, Hartgers C (1995) European adaptation of a multidi-mensional assessment instrument for drug and alcohol dependence. Eur Addict Res 1:208–210
Wechsler D (2003) Wechsler intelligence scale for children-IV (WISC-IV). TEA Ediciones, Madrid
Wechsler D (2001) Escala de inteligencia para adultos, 2nd edn. TEA Ediciones, Madrid
Tombaugh TN (2004) Trail making test A and B: normative data stratified by age and education. Arch Clin Neuropsychol 19:203–214. https://doi.org/10.1016/S0887-6177(03)00039-8
Golden CJ (1997) Stroop color and word test. Stoelting Company, Wood Dale
Conners K (2000) Conners’ continuous performance test, CPT-II. Multi-Health Syst Inc, North Tonwanda
Benedet MJ (1998) Test de aprendizaje verbal españa-complutense (TAVEC). TEA Ediciones, Madrid
Heaton RK, Chelune G, Talley J, Kay G, Curtiss G (1997) Wisconsin card sorting test (WCST). TEA Ediciones, Madrid
Ruff RM, Light RH, Parker SB, Levin HS (1996) Benton controlled oral word association test: reliability and updated norms. Arch Clin Neuropsychol 11:329–338. https://doi.org/10.1016/0887-6177(95)00033-X
Cuesta MJ, Sánchez-Torres AM, Cabrera B et al (2015) Premorbid adjustment and clinical correlates of cognitive impairment in first-episode psychosis: the PEPsCog study. Schizophr Res. https://doi.org/10.1016/j.schres.2015.02.022
Puig O, Baeza I, De La Serna E et al (2017) Persistent negative symptoms in first-episode psychosis: early cognitive and social functioning correlates and differences between early and adult onset. J Clin Psychiatry 78:1414–1422. https://doi.org/10.4088/JCP.16m11122
Mayoral M, Zabala A, Robles O et al (2008) Neuropsychological functioning in adolescents with first episode psychosis: a two-year follow-up study. Eur Psychiatry 23:375–383. https://doi.org/10.1016/j.eurpsy.2008.01.1420
Zabala A, Rapado M, Arango C et al (2010) Neuropsychological functioning in early-onset first-episode psychosis: comparison of diagnostic subgroups. Eur Arch Psychiatry Clin Neurosci. https://doi.org/10.1007/s00406-009-0046-9
Reichenberg A, Harvey PD, Bowie CR et al (2009) Neuropsychological function and dysfunction in schizophrenia and psychotic affective disorders. Schizophr Bull 35:1022–1029. https://doi.org/10.1093/schbul/sbn044
Fagerlund B, Pagsberg AK, Hemmingsen RP (2006) Cognitive deficits and levels of IQ in adolescent onset schizophrenia and other psychotic disorders. Schizophr Res 85:30–39. https://doi.org/10.1016/j.schres.2006.03.004
Mulder H, Pitchford NJ, Hagger MS, Marlow N (2009) Development of executive function and attention in preterm children: a systematic review. Dev Neuropsychol 34:393–421. https://doi.org/10.1080/87565640902964524
Romine CB, Reynolds CR (2005) A model of the development of frontal lobe functioning: findings from a meta-analysis. Appl Neuropsychol 12:190–201
Husted J, Greenwood CMT, Bassett AS (2006) Heritability of schizophrenia and major affective disorder as a function of age, in the presence of strong cohort effects. Eur Arch Psychiatry Clin Neurosci 256:222–229. https://doi.org/10.1007/s00406-005-0629-z
Bowie CR, Grossman M, Gupta M et al (2014) Cognitive remediation in schizophrenia: efficacy and effectiveness in patients with early versus long-term course of illness. Early Interv Psychiatry 8:32–38. https://doi.org/10.1111/eip.12029
Lévesque IS, Abdel-Baki A (2019) Homeless youth with first-episode psychosis: a 2-year outcome study. Schizophr Res. https://doi.org/10.1016/j.schres.2019.10.031
Moulton V, Goodman A, Nasim B et al (2021) Parental wealth and children’s cognitive ability, mental, and physical health: evidence from the UK millennium cohort study. Child Dev 92:115–123. https://doi.org/10.1111/CDEV.13413
Eilertsen T, Thorsen A, Holm S et al (2016) Parental socioeconomic status and child intellectual functioning in a Norwegian sample. Scand J Psychol 57:399–405. https://doi.org/10.1111/SJOP.12324
Yeo R, Martinez D, Pommy J et al (2014) The impact of parent socio-economic status on executive functioning and cortical morphology in individuals with schizophrenia and healthy controls. Psychol Med 44:1257–1265. https://doi.org/10.1017/S0033291713001608
Bratlien U, Øie M, Haug E et al (2014) Environmental factors during adolescence associated with later development of psychotic disorders—a nested case-control study. Psychiatry Res 215:579–585. https://doi.org/10.1016/J.PSYCHRES.2013.12.048
Luo Y, Zhang L, He P et al (2019) Individual-level and area-level socioeconomic status (SES) and schizophrenia: cross-sectional analyses using the evidence from 19 million Chinese adults. BMJ Open. https://doi.org/10.1136/BMJOPEN-2018-026532
Baldez D, Biazus T, Rabelo-da-Ponte FD et al (2021) The effect of antipsychotics on the cognitive performance of individuals with psychotic disorders: network meta-analyses of randomized controlled trials. Neurosci Biobehav Rev 126:265–275. https://doi.org/10.1016/J.NEUBIOREV.2021.03.028
Klingberg T (2006) Development of a superior frontal-intraparietal network for visuo-spatial working memory. Neuropsychologia 44:2171–2177. https://doi.org/10.1016/J.NEUROPSYCHOLOGIA.2005.11.019
Gathercole S, Pickering S, Ambridge B, Wearing H (2004) The structure of working memory from 4 to 15 years of age. Dev Psychol 40:177–190. https://doi.org/10.1037/0012-1649.40.2.177
Conners KK, Epstein JN, Angold A, Klaric J (2003) Continuous performance test performance in a normative epidemiological sample. J Abnorm Child Psychol 31:555–562. https://doi.org/10.1023/A:1025457300409
Leboyer M, Henry C, Paillerie-Martinot M-L, Bellivier F (2005) Age at onset in bipolar affective disorders: a review. Bipolar Disord 7:111–118. https://doi.org/10.1111/j.1399-5618.2005.00181.x
Acknowledgements
The authors are extremely grateful to all participants. PEPs Study is coordinated by MB and is part of the coordinated-multicenter project, funded by the Ministerio de Economía y Competitividad (PI08/0208; PI11/00325; PI14/00612), Instituto de Salud Carlos III – Fondo Europeo de Desarrollo Regional. Unión Europea. Una manera de hacer Europa, Centro de Investigación Biomédica en Red de salud Mental, CIBERSAM, by the CERCA Program/Generalitat de Catalunya And Secretaria d’Universitats i Recerca del Departament d’Economia I Coneixement (2017SGR1355, 2017SGR1365; 2017SGR881). Departament de Salut de la Generalitat de Catalunya, Pla Estratègic de Recerca i Innovació en Salut (PERIS) 2016–2020, modalitat Projectes de recerca orientats a l’atenció primària, amb el codi d’expedient SLT006/17/00345. MB is also grateful for the support of the Institut de Neurociències, Universitat de Barcelona. PEPs Group Members—Santiago Madero: Barcelona Clinic Schizophrenia Unit, Hospital Clinic of Barcelona, Neuroscience Institute, Barcelona, Spain, Department of Medicine, Institut de Neurociències, Universitat de Barcelona, Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, August Pi I Sunyer Biomedical Research Institute-IDIBAPS), Barcelona, Spain; Gerard Anmella: Barcelona Clinic Schizophrenia Unit, Hospital Clinic of Barcelona, Neuroscience Institute, Barcelona, Spain, Department of Medicine, Institut de Neurociències, Universitat de Barcelona, Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, August Pi I Sunyer Biomedical Research Institute-IDIBAPS), Barcelona, Spain; Renzo Abregu: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, Department of Child and Adolescent Psychiatry. Institute of Psychiatry and Mental Health, Hospital General Universitario Gregorio Marañon, IiSGM; Marta Rapado-Castro: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, Department of Child and Adolescent Psychiatry. Institute of Psychiatry and Mental Health, Hospital General Universitario Gregorio Marañon, IiSGM, School of Medicine, Universidad Complutense; Anna Alonso-Solís: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, Psychiatry Department, Institut d'Investigació Biomèdica-Sant Pau (IIB-SANT PAU), Hospital de la Santa Creu i Sant Pau; Universitat Autònoma de Barcelona (UAB), Barcelona, Spain; Eva Grasa: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, Psychiatry Department, Institut d'Investigació Biomèdica-Sant Pau (IIB-SANT PAU), Hospital de la Santa Creu i Sant Pau; Universitat Autònoma de Barcelona (UAB), Barcelona, Spain; Iñaki Zorrilla: BIOARABA. Department of Psychiatry. UPV/EHU. Vitoria, Spain; Itxaso Gonzalez-Ortega: BIOARABA. Department of Psychiatry. UPV/EHU. Vitoria, Spain; Pedro Saz: Department of Medicine and Psychiatry. Zaragoza University. Instituto de Investigación Sanitaria Aragón (IIS Aragón), Zaragoza; Concepción De-la-Camara: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, Department of Medicine and Psychiatry. Zaragoza University. Instituto de Investigación Sanitaria Aragón (IIS Aragón), Zaragoza; Jose Escarti: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, Department of Psychiatry, Hospital Clínico Universitario de Valencia. Biomedical Research Institute INCLIVA, Valencia, Spain , School of Medicine, Universidad de Valencia, Valencia, Spain; Jon-Iñaki Etxeandia-Pradera: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, Department of Psychiatry, Hospital Clínico Universitario de Valencia. Biomedical Research Institute INCLIVA, Valencia, Spain ; Laura Martínez: Hospital del Mar, Department of Psychiatry; Teresa Legido: Hospital del Mar, Department of Psychiatry, Medical Research Institute (IMIM), Neuroscience group; Maria Sagué-Vilavella: Bipolar and Depressive Disorders Unit, Department of Psychiatry and Psychology, Hospital Clinic, Barcelona, Catalonia, Spain; Laura Montejo: Bipolar and Depressive Disorders Unit, Department of Psychiatry and Psychology, Hospital Clinic, Barcelona, Catalonia, Spain; Gisela Sugranyes: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, August Pi I Sunyer Biomedical Research Institute-IDIBAPS), Barcelona, Spain, Department of Child and Adolescent Psychiatry and Psychology, Institut Clinic de Neurociències, Hospital Clínic Universitari, Barcelona, Spain. 2017SGR881; Patricia Camprodon-Boadas: Department of Child and Adolescent Psychiatry and Psychology, Institut Clinic de Neurociències, Hospital Clínic Universitari, Barcelona, Spain. 2017SGR881, Fundacio Clinic per a la Recerca Biomèdica, Barcelona, Spain; Fernando Contreras: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, Bellvitge Biomedical Research Institute IDIBELL, Department of Psychiatry- Bellvitge University Hospital, Hospitalet de Llobregat- Barcelona, Spain; Cristina Saiz-Masvidal: Bellvitge Biomedical Research Institute IDIBELL, Department of Psychiatry- Bellvitge University Hospital, Hospitalet de Llobregat- Barcelona, Spain, University of Barcelona, Department of Clinical Sciences- School of Medicine, Barcelona, Spain; Elisa Seijo: Unidad de Hospitalización Infanto-Juvenil. Hospital Universitario Central de Asturias (HUCA). Servicio de Salud del Principado de Asturias (SESPA). Instituto de Investigación Sanitaria del Principado de Asturias (ISPA); Teresa Bobes: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, Centro de Salud Mental II de Oviedo, Servicio de Salud del Principado de Asturias (SESPA). Universidad de Oviedo. Instituto de Investigación Sanitaria del Prin- cipado de Asturias (ISPA), Instituto de Neurociencias del Principado de Asturias (IN- EUROPA); Miguel Gutierrez: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, Araba University Hospital, Bioaraba Research Institute, University of the Basque Country (UPV/EHU) Vitoria, Spain; Arantzazu Zabala: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, University of the Basque Country (UPV/EHU), Department of Neurosciences. BioCruces Health Research Institute. Vizcaya, Spain; Roberto Rodríguez-Jiménez: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, Instituto de Investigación Sanitaria Hospital 12 de Octubre (imas12), Madrid, Spain, CogPsy Group, Universidad Complutense de Madrid (UCM), Madrid, Spain; Jusdith Usall: Parc Sanitari Sant Joan de Déu, Sant Boi de Llobregat, Barcelona; Anna Butllosa: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, Parc Sanitari Sant Joan de Déu, Sant Boi de Llobregat, Barcelona, Institut de Recerca Sant Joan de Déu, Esplugues del Llobregat, Barcelona, Spain; Luis Sanchez-Pastor: Instituto de Investigación Sanitaria Hospital 12 de Octubre (imas12), Madrid, Spain; Salvador Sarro: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, FIDMAG Germanes Hospitalàries Research Foundation, Barcelona, Spain; Edith Pomarol: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, School of Medicine, Universitat Internacional de Catalunya, Barcelona, Spain; Angela Ibañez: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, Department of Psychiatry, Hospital Universitario Ramón y Cajal, IRYCIS. Universidad de Alcalá, Madrid, Spain; Ruth Lorente-Omeña: IdiSNA, Navarra Institute for Health Research, Pamplona, Spain; Vicente Balanza: Barcelona, Spain. Biomedical Research Networking Center for Mental Health Network-CIBERSAM, Barcelona, Spain, Universidad de Valencia, Valencia, Spain.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
AG-P has received grants and served as consultant, advisor or CME speaker for the following entities: Janssen-Cilag, Lundbeck, Otsuka, Pfizer, Sanofi-Aventis, Alter, Angelini, Exeltis, Takeda, the Spanish Ministry of Science and Innovation (CIBERSAM), the Ministry of Science (Carlos III Institute), the Basque Government, and the European Framework Program of Research. MM-G was supported by a Tatiana Pérez de Guzmán el Bueno predoctoral Fellowship. EV has received grants and served as consultant, advisor or CME speaker unrelated to the present work for the following entities: AB-Biotics, Abbott, Allergan, Angelini, Dainippon Sumitomo Pharma, Ferrer, GH Research, Gedeon Richter, Janssen, Lundbeck, Otsuka, Sage, Sanofi-Aventis, Sunovion, and Takeda. IB has received honoraria or travel support from Otsuka-Lundbeck, Angelini and Janssen, research support from Fundación Alicia Koplowitz and grants from Spanish Ministry of Health, Instituto de Salud Carlos III. MB has been a consultant for, received grant/research support and honoraria from, and been on the speakers/advisory board of ABBiotics, Adamed, Angelini, Casen Recordati, Janssen-Cilag, Menarini, Lundbeck, Otsuka, Rovi and Takeda. ES and the remaining members of the PEPs group have no personal affiliations or financial relationships with any commercial interests to disclose relative to the article.
Additional information
The members of the PEPs Group members are listed in the Acknowledgements section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
De la Serna, E., Puig, O., Mezquida, G. et al. Relationship between cognition and age at onset of first-episode psychosis: comparative study between adolescents, young adults, and adults. Eur Child Adolesc Psychiatry 32, 639–649 (2023). https://doi.org/10.1007/s00787-021-01901-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-021-01901-8