Abstract
Cognition and clinical variables are known to be among the most predictive factors of real-world social functioning and daily living skills in adult-onset schizophrenia. Fewer studies have focused on their impact in adolescents with early-onset schizophrenia (EOS). The aim of this study is to examine the relationships and the predictive value of cognition and clinical variables on real-world daily living skills in a sample of adolescents with EOS. Cognitive, clinical and real-world everyday living skills measures were administered to 45 clinically and pharmacologically stabilized adolescent outpatients with EOS and 45 healthy control subjects matched by age and sex. Multi-variant analyses to compare cognitive and real-world functioning profiles between patients and controls and regression analysis to identify predictors of real-world functioning scores in patients were used. Adolescents with EOS showed a generalized cognitive and real-world daily living skills dysfunction. Several cognitive and clinical variables significantly correlated with real-world daily living skills functioning but only the processing speed and executive functions emerged as independent predictors of everyday living skills scores, explaining 25.1% of the variance. Slowness in processing information and executive dysfunction showed a significant impact on real-world daily living skills in EOS, independently from clinical symptoms and other cognitive variables. Nevertheless, much of the variance in the daily living skills measure remained unaccounted for, suggesting that other factors were involved as well in this young population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Early-onset schizophrenia (EOS), defined as schizophrenia with onset before the age of 18 years, has been described as a more severe form of the illness. Although there is evidence that EOS bears many similarities to adult-onset schizophrenia (AOS) [1], the onset of schizophrenia during childhood and adolescence has specific features and characteristics that suggest a more insidious type of illness, with more negative symptoms, poorer premorbid functioning and developmental deviance, more schizophrenia spectrum traits and worse clinical and functional outcomes [2–7].
Cognitive deficits are known to be a core feature in EOS, with large deficits in almost all cognitive domains and severe deficits in arithmetic, executive functions, intelligence quotient, verbal memory and psychomotor speed of processing [8]. In the Maudsley Early Onset Schizophrenia follow-up study, Frangou et al. [9] compared a sample of 20 EOS clinically and pharmacologically stabilized patients with 20 healthy controls at two points: at baseline when patients had a mean age of 15 years and after a mean interval of 4 years. They found that most aspects of cognitive function in EOS were relatively stable at 4-year follow-up, although there was evidence of deterioration in verbal memory and attention, and some improvement in speed of information processing. In a longer follow-up study, Oie et al. [10] found that after 13 years, patients with EOS had a significant decline or arrest in neurocognitive functioning, particularly in attention, verbal memory and processing speed.
Cognition and negative symptoms are known to be among the most predictive variables of social and daily living functioning in AOS [11–15], although the relationship between cognition and real-world functional outcome is complex and partially mediated by competence skills level [16]. Social and independent living may be independent domains of functional outcome, with somewhat different associations with different cognitive processes. Social competence appeared to be more related to verbal fluency, working and episodic memory, while everyday living skills appeared to be more related to processing speed, episodic memory and executive functions [17]. When examining real-world performance (what the individual does in day-to-day living) in a large sample of 222 adult schizophrenic patients with a mean age of 56 years, Bowie et al. [16] found that attention/working memory and executive functions showed an effect on work and interpersonal behavior, and processing speed had direct effects on all real-world behaviors (work, interpersonal and community behaviors). Symptoms have also been found to have direct effects on real-world behaviors [16, 18].
In EOS, it is known that premorbid adjustment predicts outcome and developmental delays predict poor prognosis [19]. Some studies have also looked at how cognition and clinical symptoms relate to functional outcome. However, compared to AOS, such associations in EOS have received relatively less attention, despite the fact that the impact of these variables may be greater among young patients whose social and daily living skills are not yet fully developed. Landro and Ueland [20] reported an association between verbal fluency and a global measure of psychosocial functioning. Recently, Hooper et al. [21] have found significant relationships between communication, social and daily living skills and several cognitive domains (full IQ, social cognition, problem solving efficiency, working memory, attention and fine-motor speed). A longitudinal study with a 13-month follow-up linked baseline verbal memory, working memory and attention/vigilance deficits to social/communication abilities, personal living and community living skills at follow-up [22]. In a 13-year follow-up, Oie et al. [23] found that baseline scores in executive function, memory, processing speed and attention were related to social and community functioning at follow-up. Among clinical variables, it has been reported that type of onset [24], and both positive [25] and negative symptoms [26, 27] predict functional outcome in EOS.
Overlap between cognitive and clinical variables, when predicting functional outcome in schizophrenia has been pointed out as a source of confusion that is not always well controlled [14, 28]. Furthermore, the importance of assessing patients under stable treatment and in the absence of acute symptoms to clarify the role of cognition versus symptoms has also been stressed [29]. In AOS, it has been suggested that cognitive status is a better predictor of social and daily living skills outcome than symptom status and a possible target for interventions [30]. Regarding EOS, some studies have found cognitive deficits to be independent of psychopathological symptoms [31, 32], while others have found significant relationships between cognitive dysfunction and positive [3], negative [33] and total scores in the Positive and Negative Symptoms Scale (PANSS) [34]. To our knowledge, there is no previous study in EOS that has analyzed simultaneously both cognitive and clinical variables as potential predictors of daily living skills outcome.
Overall, there is a scarcity of studies focusing on the relationships between real-world daily living functioning and cognitive and clinical characteristics among adolescents with EOS, especially in stabilized clinical and pharmacological conditions. The aims of this study were to analyze the cognitive and real-world daily living skills profile of a sample of clinically and pharmacologically stabilized adolescents with EOS and examine the relationships and the predictive value of cognition and clinical variables on real-world daily living skills scores. Based on the previous studies in EOS, we hypothesized that overall cognitive and everyday living skills impairment would be found in the EOS sample. Taking into account previous studies in EOS as well as studies in AOS suggesting specific determinants for everyday living skills and real-world behaviors [16, 17], we expected verbal memory, processing speed, attention/working memory and executive functions to predict Life Skills Profile (LSP) scores. In accordance with previous findings regarding the associations between symptoms and functional outcome in EOS samples [25–27] and in AOS [18], we hypothesized that both positive and negative symptoms would emerge as significant predictors of real-world everyday living skills scores.
Methods
Sample
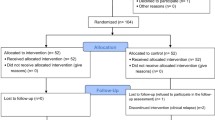
Subjects were 45 adolescent patients with EOS and 45 healthy adolescents matched by age and sex. Patients were consecutively recruited from the population of outpatient adolescents with EOS at the Child and Adolescent Psychiatry and Psychology Department of Hospital Clínic in Barcelona, Spain. Inclusion criteria were: age between 12 and 18 years, a DSM-IV-TR schizophrenia-type disorder (schizophrenia, schizoaffective disorder or schizophreniform disorder) with onset before the age of 17 and being clinically and pharmacologically stabilized during the last 6 weeks before the assessments. Diagnoses and psychopathological stability were confirmed by the treating psychiatrist using DSM-IV-TR criteria based on clinical interviews with patients and their families. Thirty-two patients (71.1%) were first-episode cases of schizophrenia. Patients’ mean duration of illness was 3.11 years (SD = 1.39). An expert child and adolescent psychiatrist verified diagnoses and psychopathological stability at the time of the assessment. Patients were excluded if they scored five (moderate–severe symptom) or more (severe symptom) on two or more items in the Positive symptoms factor of Bell’s 5-factor solution for the PANSS [35]. Although all patients were treated in outpatient settings and had been on the same antipsychotic dose for the previous 6 weeks, it was deemed that having two moderate–severe or severe symptoms on the PANSS could indicate a non-remitted acute episode of the illness, or a relapse. The other exclusion criteria were antipsychotic type/dosage modification during the previous 6 weeks, intelligence quotient (IQ) below 70, active substance misuse disorder, organic brain syndromes or neurological disorders, and having received electroconvulsive therapy in the previous 6 months. IQ was assessed at the time of the cognitive examination. The potential sample comprised 88 consecutively attended subjects of whom 43 did not fulfill inclusion criteria. The most frequent reason was not having achieved clinical and/or pharmacological stability during a minimum of 6 weeks prior to the assessments (15 patients, 34.9%). Ten patients had an IQ below 70 (23.3%), six had active drug dependence/abuse disorder (14%), four families did not consent (9.3%), three patients did not collaborate with the assessments (7%), two had neurological disorders (4.7%), two had non-valid scores in the real-world functioning measure (4.7%) and one patient left the city before assessment could be completed (2.3%).
Control subjects were recruited through posters hung in schools of the same catchment area as patients and they were matched to patients by gender and age (within 6 months). It was not possible to match groups according to familial socioeconomic background. Regarding general intelligence ability, groups were not matched by estimated IQ. Although this approach may be debated, general intelligence ability is known to be impaired in EOS [36]. Also, at the premorbid stage of the illness, early onset is related to greater IQ decrement [37]. Therefore, differences in IQ could be considered an inherent effect of the disorder rather than a confounding variable [20, 38]. The groups were not matched by academic grade because this variable was analyzed as a real-world outcome. Control subjects and their parents were interviewed with the Spanish adaptation of the Kiddie-Schedule for Affective Disorders and Schizophrenia (K-SADS-PL) [39]. Exclusion criteria for the control group were a history of any axis I psychiatric disorder, IQ below 70, active substance misuse disorder and the presence of organic brain syndromes or neurological disorders. The subjects received, through their parents, economic compensation for their participation.
The study was approved by the Ethics Committee of the institution. All parents or legal guardians gave written informed consent and all patients and controls agreed to participate.
Cognition measures
Cognitive testing was administered by two child and adolescent psychologists with experience in both clinical and cognitive assessments. They were blind to clinical and real-world data. Inter-rater reliability for cognitive assessments was higher than 0.8 (within-class correlation coefficients between 0.90 and 0.99). To provide a standard metric for comparisons across cognitive domains and controlling for age and developmental effects, scores were converted to demographically corrected T-scores. Cognitive domains were defined following the MATRICS consensus battery [40] which has been recently validated in adolescents with EOS [38]. Since a Spanish translation of the battery is not yet ready, available tests in Spanish that are similar to the consensus were used to assess cognitive domains. The domains score represented the average of the T scores for the tests included, if more than one. For IQ, T score was derived from the weighted mean of the subtests included, taking into account their weight on the total intelligence quotient described in the respective Wechsler Intelligence Scales manuals (Wechsler Intelligence scales for children, WISC-IV [41], or for adults WAIS-III [42]).
-
IQ: Vocabulary and Block Design subtests from the Spanish version of WISC-IV or WAIS-III, depending on age.
-
Verbal Memory: Logical Memory subtests from the Wechsler Memory Scales, 3rd edition (WMS-III) [43], immediate and delayed recall subtests. Total word recall and delayed recall subtests of the Rey Auditory Verbal Learning Test (RAVLT) [44].
-
Visual Memory Visual Reproduction subtests from the WMS-III.
-
Attention Digit Span subtest from WISC-IV/WAIS-III.
-
Working Memory Letter Number Sequencing subtest from WISC-IV/WAIS-III.
-
Processing Speed Part A of the Trail Making Test (TMT) [45].
-
Executive functions total errors score in the Wisconsin Card Sorting Test (WCST) [46], total words generated by patient in the verbal fluency subtest from Controlled Oral Word Association Tests (FAS) [47] and total seconds needed for completing Part B of the TMT were used to score the executive functions domain.
Clinical measures
Clinical assessment was administered by two expert child and adolescent psychiatrists. Clinicians were blind to patients’ cognitive and real-world functioning scores. Severity of symptoms was assessed using the Spanish Version of the PANSS [48]. The reliability of clinicians administering PANSS was assessed and the within-class correlation coefficient was higher than 0.8. We used four domains of the five factor analytic solution of Bell et al. [35]: negative symptoms, positive symptoms, emotional discomfort and hostility symptoms. The cognitive Symptoms factor was not included because cognition was tested directly. Depressive symptomatology was assessed with the Calgary Depression Scale [49].
Real-world functioning assessment
The Spanish version [50] of the Life Skills Profile (LSP) [51] was employed. It has demonstrated good psychometric properties in AOS [52] and also in adolescents with EOS (unpublished results). The LSP is a 39-item questionnaire which assesses patients’ real-world level of functioning by rating relevant domains of ability. The items rely on basic, specific and observable behaviors, and the focus is on actual performance rather than potential behaviors or competence. There are several versions of the LSP available. High scores could indicate either more difficulties or greater ability depending on the version, and whether its emphasis is on functioning or on disability [53]. We used the Spanish adaptation of the original LSP-39. The total score range is 39–156 and lower scores indicate more dysfunction and disability. If there was any missing data, that particular item was not scored (or scored as 0) for both groups. We used the total score as a proxy of the real-world daily living skills. The scale’s questions were answered by one of each subject’s parents. To adapt contents to an adolescent sample, we added a reference to school activities in two items which refer to work functioning. We also recorded the last completed school grade as a measure of academic functioning.
Data analysis
Clinical and real-world functioning variables were analyzed using raw-scores. Student’s t test was used to compare continuous variables and the Chi-squared test to compare categorical variables. Analyses of variance (ANOVA) were used to compare LSP scores and last complete academic grade scores between groups. Multiple analyses of variance (MANOVA) with follow-up ANOVAs were used to assess overall differences between groups on cognitive domains. If significant differences between groups were found in variables which could confound the results, data were further analyzed through analyses of covariance (ANCOVA and MANCOVA) to control for the effect of those variables. In order to maintain the whole sample for multi-variant analysis, the group mean was used to determine missing scores for five subjects (two patients and three controls). Subjects with more than two scores missing were excluded from the analysis. A total of eight missing scores were calculated.
To study the relationship between real-world functioning and clinical and cognitive variables, we examined the potential predictive value of cognitive and clinical variables in relation to the LSP scores. The last complete academic grade was not analyzed through correlational and regressional analysis, because it was retrospective data. Correlation coefficients were computed using Pearson correlations between daily living skills and cognitive and clinical scores. To establish the predictive capacity of the cognitive and clinical variables on the functional domain, a linear regression model was fitted using a stepwise method. Those variables which showed a significant correlation with the LSP score were included as potential predictors. Terms such as “predictor variable” and “explained variance” were used in a statistical sense, without implying causality. All tests were two-tailed. Statistical analyses were carried out with the Statistical Package for the Social Sciences, 16.0 (SPSS, v. 16).
Results
Sample characteristics
Table 1 shows socio-demographic and clinical characteristics of the sample. Familial socioeconomic status (SES) assessed using the Hollingshead system was significantly lower in patients than in control adolescents. It was included as a covariable in subsequent analysis. More than half of the patients’ sample had an insidious onset of the disease (n = 27, 60%). Eight (17.8%) patients had a very early onset of psychosis (VEOS) defined as onset of Positive symptoms before the age of 13. At enrolment, almost all patients were taking atypical antipsychotics (93.3%), and none were on typical neuroleptics. Mean dosage, standard deviation and range of each applied antipsychotic are shown in Table 1. Only three patients were not on antipsychotics, but taking antidepressants. This was due to predominant negative and depressive symptoms without positive symptoms when they were admitted to the study. Mean duration time since last change in antipsychotic medication was 20.56 weeks (SD = 17.57, range = 6–92). Mean duration time from last admission in acute units was 31.86 weeks (SD = 26.48, range = 6–109). Only 10 patients (22.2%) had been able to return to regular school at the time of enrolment.
Table 2 shows mean and standard deviations for cognitive domains and daily living skills scores. Patients with EOS had lower IQ and lower scores in all cognitive domains than control adolescents, in a range between 0.8 and 1.8 SD below the controls’ means (MANOVA Wilks λ = 0.40, F = 20.46, p < 0.001). The exclusion of patients with VEOS did not change the results (MANOVA Wilks λ = 0.38, F = 20.47, p < 0.001). In subsequent analysis, IQ and SES differences between groups were controlled for entering in the model as covariables. Overall differences in cognitive domains between groups remained after controlling for these confounders (MANCOVA Wilks λ = 0.67, F = 6.62, p < 0.001). Patients’ scores remained significantly below controls’ means in all cognitive domains except for attention (F = 1.52, p = 0.221) and working memory scores (F = 3.25, p = 0.075) when SES and IQ were controlled for.
Real-world functioning scores were significantly lower in the patients’ group than in controls (ANOVA for LSP score: F = 66.34, p < 0.001; for last complete academic grade: F = 44.59, p < 0.001) and remained significantly below controls’ mean when controlling for SES and IQ differences between groups (ANCOVA for LSP score: F = 33.99, p < 0.001; for last complete academic grade: F = 34.71, p < 0.001).
Predictive value of cognition and clinical variables on real-world daily living skills scores
Correlations between LSP score, cognitive domains and clinical variables were calculated to identify the potential predictors for regression analysis (Table 3). All cognitive domains except IQ and attention were significantly correlated with LSP score, while among clinical variables, only negative and positive symptoms showed such significant correlation. Table 4 shows the results of the regression analysis for LSP score. The stepwise method was employed. Those variables which showed a significant correlation with the LSP score were included as potential predictors in the same block: PANSS negative symptoms scale score, PANSS positive symptoms scale score, verbal memory domain score, visual memory domain score, working memory domain score, processing speed domain score and executive functions domain score. Processing speed and executive functions explained 25.1% of the variance of total score in LSP. Processing speed was the first variable to enter in the model and explained 18.2% of the variance (adjusted R 2 = 0.182, F = 10.81, p = 0.002). The final model included executive functions which increased the predictive value of the model, an additional 6.9% (adjusted R2 = 0.251, F = 8.39, p = 0.001). None of the other potential cognitive predictors made significant contributions to the model (verbal memory: t = −0.02, p = 0.985; visual memory: t = 1.19, p = 0.241; working memory: t = −0.07, p = 0.944). Neither negative nor positive symptoms contributed to increase the predictive value of the model (negative symptoms: t = −1.16, p = 0.252; positive symptoms: t = −1.25, p = 0.220). Table 5 shows the correlations between the potential cognitive predictors.
Discussion
This cross-sectional study of adolescent outpatients with EOS showed that a quarter (25.1%) of the real-world daily living skills score variance was predicted by processing speed and executive functions domains. Also, the results corroborated that EOS is associated with a generalized pattern of cognitive and real-world functioning abnormalities. This finding is consistent with previous reports in chronic AOS [28, 54], first-episode young adults [55] and other EOS adolescent samples [22, 32, 33, 56, 57]. Despite the young age of the sample, the mean LSP total score was similar to those reported in chronic schizophrenic adults of the same cultural and environmental area [58, 59]. The LSP is designed to assess performance in very basic everyday living skills, such as routines of grooming and hygiene, maintaining eye contact and not being offensive in social contact. Although differences between patient and control groups were not so large, the EOS group showed a significant degree of disability which was at least as severe as that found among chronic schizophrenic adults.
Overall differences between groups in cognitive and real-word functioning scores remained significant when controlling for IQ and SES. Although it may be a controversial issue, groups were not matched by IQ, academic grade or SES. As EOS is associated with compromised general cognitive intellectual ability [36] and schizophrenia is associated with low socioeconomic status, especially in patients with low cognitive abilities [60], matching the groups in these areas could actually remove the effect of the disease, leading to biased comparisons between overachieving patients and underachieving controls [20, 38]. Despite this, we have controlled for IQ and SES differences through further analysis of covariance. As has been found in previous reports, our results showed that cognitive deficits are a relevant trait of EOS beyond patients’ lower IQ and lower SES [32, 38, 57]. Regarding academic grade, our results confirmed previous reports which showed that EOS patients achieve worse educational level [3, 61] and showed that such worse achievements were present from initial stages of the illness independently from IQ and SES.
The regression analysis for LSP score showed that prediction of real-world daily living skills in EOS could be partially accomplished using simple and rapidly completed cognitive tests such as processing speed tests and by executive functions tests. The results were consistent with previous reports which found cognition as a better predictor than symptoms in AOS samples [11, 30]. Nevertheless, the predictive value of cognitive variables explained a quarter of the variance of real-world scores, which is less than in studies of adult patients with long duration of illness [11]. The value of correlations between our daily living skills measure and cognitive domains was similar to those reported by other previous EOS studies. For instance, Hooper et al. [21] reported correlation values between 0.22 and 0.41 between their measure of daily living skills and several cognitive domains, such as fine motor speed, problem solving efficiency, working memory and sustained attention. Others have pointed out that there may be other non-controlled factors playing a role in younger samples or that in individuals with a more chronic course and longer duration of the illness, the link between cognitive performance and functional outcome may be stronger [14]. From another perspective, the finding may also be due to the outcome measure used. The LSP assesses distal or macrosocial behaviors. Deployment of these behaviors in real time in the real world will depend on the functional competence [16] of the patient and also on having the appropriate opportunities and motivation [12]. Cognition appears to be necessary for effective everyday functioning, but insufficient as a sole predictor [12]. Real-world daily living functioning additionally relies on social/environmental opportunities, including availability of psychosocial rehabilitation, social support networks and educational facilities. It might be the case that in EOS, these environmental factors could have a greater weight than in AOS.
Processing speed deficits have been found to be a central and consistent feature of the illness [62], although this can be substantially affected by antipsychotic medication dosage [63]. It could be hypothesized that the main effect of processing speed scores in predicting real-world functioning scores could be mediated by the patients’ pharmacological treatment, but in our sample the chlorpromazine equivalent daily dose variable was not significantly correlated with the LSP score. Thus, one of the steps required for a mediation model [64] was not verified. Despite this, the role of medication could not be totally ruled out, particularly in a small sample like the one in this study. Processing speed deficits have repeatedly been found to be associated with functional outcome in AOS [14, 16, 28, 65]. In EOS, Oie et al. [23] found that processing speed scores was a significant predictor of social functioning at follow-up, and Cervellione et al. [22] related community living skills with attention/vigilance scores which were assessed by processing speed tests such as Digit Symbol and TMT.
Executive functions are known to be a significant predictor of daily living functioning [11] and of interpersonal behavior in AOS [16]. In EOS, executive functions have also been consistently found to be related to functional outcome [20–23]. In our results, executive functions were the unique cognitive variable which added a relatively small but significant predictive value to the model when processing speed was accounted for; there was not only a partial overlap between the variance explained by processing speed and executive functions but also some non-shared variance. Taking all of the data into account, results suggested that improving processing speed—or slowing down its decline [10]—and improving executive functions might be a primary target in EOS treatment programs.
Contrary to our initial hypothesis, none of the other cognitive domains or clinical variables predicted real-world functioning scores. As in some previous EOS studies [22, 23] and AOS literature [11, 14], verbal memory score showed significant correlations with our daily living skills measure, but it did not emerge as a significant predictor when controlling for processing speed and executive functions. In our results, verbal memory was significantly correlated with processing speed scores. Dickinson et al. [62] highlighted that many higher cognitive operations—including encoding and retrieval—involve internal dynamics that are significantly speed-dependent. Others have found that speed of processing is a strong predictor of verbal memory performance in schizophrenia [66, 67]. Therefore, it might be that processing speed scores have prevented verbal memory from entering the model. Verbal memory was also highly correlated with executive functions scores, and that could also explain the result. In a deep review about the verbal memory dysfunction in schizophrenia, Cirillo and Seidman [68] highlighted the involvement of the frontally mediated “central executive” in memory deficits.
Regarding the attention domain, our results showed that patients’ scores were not significantly below controls’ mean after controlling for SES and IQ differences between groups. These findings corroborated previous reports which have found preservation of attentional functions in adolescents with EOS [32, 69, 70], and supported the hypothesis that attentional deficits in adolescents with schizophrenia do not have the same high discriminative value as attention disorders in adult schizophrenia [32].
Among clinical variables, neither positive nor negative symptoms emerged as predictors despite their significant correlation with LSP score. In AOS, positive symptoms appeared to have an impact on functional outcome in some studies of chronic schizophrenia [18] and first-episode psychosis [71]. In EOS, some previous studies have found a significant relationship between positive symptoms and functional outcome [25] but others have not [27]. None of these previous EOS studies had considered cognition along with symptoms in predicting functional outcome. Our results showed positive symptoms to be significantly correlated with real-world daily living skills scores, but this did not remain significant in the regression model when cognition was controlled for. Nevertheless, patients scoring five or higher on two or more items of the PANSS were excluded from the study, because it was deemed that having two or more marked positive symptoms which could need direct supervision could indicate a non-remitted acute episode or a relapse; this approach may have affected the potential predictive value of severe positive symptoms in relation to functional outcome. This is especially relevant in a sample of adolescents with EOS, because the early-onset of the illness usually tends to result in a more symptomatically severe form of the disorder, with more severe positive and negative symptoms than adult-onset schizophrenia [72].
An unexpected finding was that negative symptoms were not found to be a significant predictor of real-world scores. Negative symptoms are known to be a major source of functional impairments in AOS [15] and first-episode samples [14]. Individual negative symptoms such as blunted affect and passive-aphetic social withdrawal have been found to be the main predictors of real-world social outcomes in chronic schizophrenia [18]. Negative symptoms have also been described as having a moderating effect [13] and a mediator effect [15] in the relationship between cognition and psychosocial functioning. In EOS, some have found negative symptoms to predict functional outcome [26, 27], but this result has not been found by others [25]. Our results showed that negative symptoms significantly correlated with real-world scores, but when considered along with cognition, cognitive variables emerged as stronger predictors. Nevertheless, one limitation of this study is that we did not examine negative symptoms individually. Individual symptoms, as reported by Leifker et al. [18], might also be significant predictors of real-world functioning in the early form of the illness. It would be interesting for future studies in EOS to focus on these potential relationships.
The use of the LSP, a scale originally created to be used in adults, could be debated. The scale includes some items referring to behaviors that are usually supervised by parents, such as taking medication without needing reminders or being collaborative with medical services. Furthermore, those items may not be totally applicable to healthy controls. Other instruments exist which are specifically designed to assess functional behavior in children and adolescents. These include the Vineland Adaptive Behavior Scales (VABS) [73] and the Child and Adolescent Functional Assessment Scale (CAFAS) [74], both of which are used by the TEOSS group [21, 72]. Although these instruments have advantages such as allowing direct comparisons with previous EOS studies, we took into consideration the fact that the LSP has recently been selected as one of the most valid measures for assessing everyday living skills in schizophrenia [75] and that it is one of the most widely used scales to assess daily living functioning [76]. This allows direct comparisons with AOS studies and with future longitudinal data. Furthermore, it is a low-burden instrument that can be answered in a few minutes by subjects’ parents, while the VABS or the CAFAS are instruments designed to be scored by mental-health clinicians or trained interviewers following a comprehensive interview. Finally, our own previous unpublished findings have validated the use of the LSP in adolescents with EOS, indicating that it is a reliable and valid instrument in young populations and that the items are actually understood and answered by almost all parents, both in the patient and the healthy control groups (unpublished results).
The findings should be interpreted in light of several other limitations. First, the prevalence of substance misuse disorder is known to be high in early psychosis [77]. Our results are only generalizable to stabilized patients without substance misuse comorbidity. Second, EOS is associated with a significant decline in measures of general intelligence that could include a drop in IQ below 70 [78], while our sample only included patients with IQ above 70. A prior estimation of IQ, before the first-episode of psychosis, may have been better, as this would have included patients who had suffered a decline in their general intelligence due to the effects of the disease but did not have a prior functional history of mental retardation. Third, data about the duration of the inpatient treatment up to examination and about the duration of antipsychotic treatment prior to the assessment were not available. Fourth, the exclusion criteria of two or more positive symptoms scored as five or more on the PANSS was to some extent an arbitrary cut-off, and did not indicate that patients in the study were completely in remission [79]. Nevertheless, our focus was on clinically (and pharmacologically) stabilized patients and, as stated by the same authors, around two-thirds of patients who are clinically stable do not meet the criteria for remission [79]. Fifth, the cross-sectional nature of our analyses is another limitation. More longitudinal studies are necessary to confirm the value of cognition as a predictor of functional outcome in EOS. Despite these limitations, the present study also has a number of strengths, such as using a blind assessment of cognitive and real-world functioning, and the use of one of the best real-world daily living skills measures for schizophrenia [75]. Moreover, the influence of acute symptoms and recent change of medications was avoided by including a relatively large and homogeneous sample of stabilized outpatients with stable pharmacological treatments.
Conclusion
The present findings confirm that EOS implies generalized cognitive impairment and a significant degree of disability. Processing speed and executive functions emerged as the main independent predictors of real-world daily living skills in EOS, independently from symptoms and other cognitive functions. The results highlighted that both slowness of processing information and executive deficits impacted on real-world functioning of this young population, although the model leaves much of the variance in the daily living skills measure unexplained. Our results are of relevance because they extend knowledge about the impact of the illness when presenting early in patients’ development and, more importantly, they can help to focus rehabilitation efforts on influential factors interfering with the performance of actual day-to-day living skills in EOS.
References
Asarnow JR, Tompson MC, McGrath EP (2004) Annotation: childhood-onset schizophrenia—clinical and treatment issues. J Child Psychol Psychiatry 45:180–194
Ballageer T, Malla A, Manchanda R, Takhar J, Haricharan R (2005) Is adolescent-onset first-episode psychosis different from adult onset? J Am Acad Child Adolesc Psychiatry 44:782–789
Hoff AL, Harris D, Faustman WO, Beal M, Devilliers D, Mone RD, Moses JA, Csernansky JG (1996) A neuropsychological study of early onset schizophrenia. Schizophr Res 20:21–28
Rabinowitz J, Levine SZ, Hafner H (2006) A population based elaboration of the role of age of onset on the course of schizophrenia. Schizophr Res 88:96–101
Schmidt M, Blanz B, Dippe A, Koppe T, Lay B (1995) Course of patients diagnosed as having schizophrenia during first episode occurring under age 18 years. Eur Arch Psychiatr Clin Neurosci 245:93–100
Vourdas A, Pipe R, Corrigall R, Frangou S (2003) Increased developmental deviance and premorbid dysfunction in early onset schizophrenia. Schizophr Res 62:13–22
Werry JS, McClellan JM, Chard L (1991) Childhood and adolescent schizophrenic, bipolar, and schizoaffective disorders: a clinical and outcome study. J Am Acad Child Adolesc Psychiatry 30:457–465
Rajji TK, Ismail Z, Mulsant BH (2009) Age at onset and cognition in schizophrenia: meta-analysis. Br J Psychiatry 195:286–293
Frangou S, Hadjulis M, Vourdas A (2008) The Maudsley early onset schizophrenia study: cognitive function over a 4 year follow-up period. Schizophr Bull 34:52–59
Oie M, Sundet K, Rund BR (2010) Neurocognitive decline in early-onset schizophrenia compared with ADHD and normal controls: evidence from a 13-year follow-up study. Schizophr Bull 36:557–565
Green MF, Kern RS, Braff DL, Mintz J (2000) Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull 26:119–136
Green MF, Kern RS, Heaton RK (2004) Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res 72:41–51
Greenwood KE, Landau S, Wykes T (2005) Negative symptoms and specific cognitive impairments as combined targets for improved functional outcome within cognitive remediation therapy. Schizophr Bull 31:910–921
Milev P, Ho BC, Arndt S, Andreasen NC (2005) Predictive values of neurocognition and negative symptoms on functional outcome in schizophrenia: a longitudinal first-episode study with 7-year follow-up. Am J Psychiatry 162:495–506
Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein KH (2009) Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophr Res 113:189–199
Bowie CR, Leung WW, Reichenberg A, McClure MM, Patterson TL, Heaton RK, Harvey PD (2008) Predicting schizophrenia patients’ real-world behavior with specific neuropsychological and functional capacity measures. Biol Psychiatry 63:505–511
McClure MM, Bowie CR, Patterson TL, Heaton RK, Weaver C, Anderson H, Harvey PD (2007) Correlations of functional capacity and neuropsychological performance in older patients with schizophrenia: evidence for specificity of relationships? Schizophr Res 89:330–338
Leifker FR, Bowie CR, Harvey PD (2009) Determinants of everyday outcome in schizophrenia: the influences of cognitive impairment, functional capacity, and symptoms. Schizophr Res 115:82–87
Fleischhaker C, Schulz E, Tepper K, Martin M, Hennighausen K, Remschmidt H (2005) Long-term course of adolescent schizophrenia. Schizophr Bull 31:769–780
Landro NI, Ueland T (2008) Verbal memory and verbal fluency in adolescents with schizophrenia spectrum disorders. Psychiatry Clin Neurosci 62:653–661
Hooper SR, Giuliano AJ, Youngstrom EA, Breiger D, Sikich L, Frazier JA et al (2010) Neurocognition in early-onset schizophrenia and schizoaffective disorders. J Am Acad Child Adolesc Psychiatry 49:52–60
Cervellione KL, Burdick KE, Cottone JG, Rhinewine JP, Kumra S (2007) Neurocognitive deficits in adolescents with schizophrenia: longitudinal stability and predictive utility for short-term functional outcome. J Am Acad Child Adolesc Psychiatry 46:867–878
Oie M, Sundet K, Ueland T (2011) Neurocognition and functional outcome in early-onset schizophrenia and attention-deficit/hyperactivity disorder: a 13-year follow-up. Neuropsychology 25:25–35
Ropcke B, Eggers C (2005) Early-onset schizophrenia: a 15-year follow-up. Eur Child Adolesc Psychiatry 14:341–350
Lay B, Blanz B, Hartmann M, Schmidt MH (2000) The psychosocial outcome of adolescent-onset schizophrenia: a 12-year followup. Schizophr Bull 26:801–816
Meng H, Schimmelmann BG, Mohler B, Lambert M, Branik E, Koch E et al (2006) Pretreatment social functioning predicts 1-year outcome in early onset psychosis. Acta Psychiatr Scand 114:249–256
Vyas NS, Hadjulis M, Vourdas A, Byrne P, Frangou S (2007) The Maudsley early onset schizophrenia study. Predictors of psychosocial outcome at 4-year follow-up. Eur Child Adolesc Psychiatry 16:465–470
Dickinson D, Coursey RD (2002) Independence and overlap among neurocognitive correlates of community functioning in schizophrenia. Schizophr Res 56:161–170
Norman RM, Malla AK, Cortese L, Cheng S, Diaz K, McIntosh E et al (1999) Symptoms and cognition as predictors of community functioning: a prospective analysis. Am J Psychiatry 156:400–405
Leung WW, Bowie CR, Harvey PD (2008) Functional implications of neuropsychological normality and symptom remission in older outpatients diagnosed with schizophrenia: a cross-sectional study. J Int Neuropsychol Soc 14:479–488
Banaschewski T, Schulz E, Martin M, Remschmidt H (2000) Cognitive functions and psychopathological symptoms in early-onset schizophrenia. Eur Child Adolesc Psychiatry 9:11–20
Kravariti E, Morris RG, Rabe-Hesketh S, Murray RM, Frangou S (2003) The Maudsley early onset schizophrenia study: cognitive function in adolescents with recent onset schizophrenia. Schizophr Res 61:137–148
Rhinewine JP, Lencz T, Thaden EP, Cervellione KL, Burdick KE, Henderson I et al (2005) Neurocognitive profile in adolescents with early-onset schizophrenia: clinical correlates. Biol Psychiatry 58:705–712
Mayoral M, Zabala A, Robles O, Bombin I, Andres P, Parellada M et al (2008) Neuropsychological functioning in adolescents with first episode psychosis: a two-year follow-up study. Eur Psychiatry 23:375–383
Bell MD, Lysaker PH, Beam-Goulet JL, Milstein RM, Lindenmayer JP (1994) Five-component model of schizophrenia: assessing the factorial invariance of the positive and negative syndrome scale. Psychiatry Res 52:295–303
Frangou S (2010) Cognitive function in early onset schizophrenia: a selective review. Front Hum Neurosci 3:1–6
Khandaker GM, Barnett JH, White IR, Jones PB (2011) A quantitative meta-analysis of population-based studies of premorbid intelligence and schizophrenia. Schizophr Res doi. doi:10.1016/j.schres.2011.06.017
Holmen A, Juuhl-Langseth M, Thormodsen R, Melle I, Rund BR (2010) Neuropsychological profile in early-onset schizophrenia-spectrum disorders: measured with the MATRICS battery. Schizophr Bull 36:852–859
Kaufman J, Birmaher B, Brent D, Rao U, Flynn E, Moreci P et al (1997) Schedule for affective disorders and schizophrenia for school-age children-present and life time version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988
Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD et al (2008) The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am J Psychiatry 165:203–213
Wechsler D (2003) The Wechsler intelligence scale for children. TEA Ediciones, Madrid
Wechsler D (2001) Escala De Inteligencia Para Adultos, III, 2nd edn. TEA Ediciones, Madrid
Wechsler D (1997) The Wechsler memory scale. The Psychological Corporation, San Antonio
Schmidt M (1996) Rey auditory verbal learning test: a handbook. Western Psychological Services, Los Angeles
Tombaught TM (2004) Trail making test A and B: normative data stratified by age and education. Arch Clinical Neuropsychol 2:203–214
Heaton RK (1981) A manual for the Wisconsin card sorting test. Psychological Assessment Resources, Odessa
Benton A, Hamsher K (1978) Multiphasic aphasia examination manual. University Of Iowa, Iowa City
Peralta V, Cuesta MJ (1994) Psychometric properties of the positive and negative syndrome scale (PANSS) in schizophrenia. Psychiatry Res 53:31–40
Addington D, Addington J, Schissel B (1990) A depression rating scale for schizophrenics. Schizophr Res 3:247–251
Bulbena A, Fernández de Larrinoa P, Domínguez A (1992) Adaptación castellana de la escala LSP (Life Skills Profile). Perfil de Habilidades de la Vida Cotidiana. Actas Luso Esp Neurol Psiquiatr Cienc Afines 20:51–60
Rosen A, Hadzi-Pavlovic D, Parker G (1989) The life skills profile: a measure assessing function and disability in schizophrenia. Schizophr Bull 15:325–337
Fernández de Larrinoa P, Bulbena A, Domínguez AL (1992) Estudio de fiabilidad, validez y consistencia interna de la escala LSP (Life Skills Profile) perfil de habilidades de la vida cotidiana. Actas Luso Esp Neurol Psiquiatr Cienc Afines 20:71–75
Burgés V, Fernández J, Autonell F, Melloni A, Bulbena A (2007) Spanish adaptation and validation of the brief form of the Life Skills Profile-20: an instrument to assess daily living skills in real clinical settings. Actas Esp Psiquiatr 35:79–88
Fioravanti M, Carlone O, Vitale B, Cinti ME, Clare L (2005) A meta-analysis of cognitive deficits in adults with a diagnosis of schizophrenia. Neuropsychol Rev 15:73–95
Mesholam-Gately RI, Giuliano AJ, Goff KP, Faraone SV, Seidman LJ (2009) Neurocognition in first-episode schizophrenia: a meta-analytic review. Neuropsychology 23:315–336
Ueland T, Oie M, Inge LN, Rund BR (2004) Cognitive functioning in adolescents with schizophrenia spectrum disorders. Psychiatry Res 126:229–239
White T, Ho BC, Ward J, O’Leary D, Andreasen NC (2006) Neuropsychological performance in first-episode adolescents with schizophrenia: a comparison with first-episode adults and adolescent control subjects. Biol Psychiatry 60:463–471
Penadés R, Catalán R, Puig O, Masana G, Pujol N, Navarro V, Guarch J, Gastó C (2010) Executive function needs to be targeted to improve social functioning with cognitive remediation therapy (CRT) in schizophrenia. Psychiatry Res 177:41–45
Puig O, Penadés R, Gastó C, Catalán R, Torres A, Salamero M (2008) Verbal memory, negative symptomatology and prediction of psychosocial functioning in schizophrenia. Psychiatry Res 158:11–17
Goldberg S, Fruchter E, Davidson M, Reichenberg A, Yoffe R, Weiser M (2011) The relationship between risk of hospitalization for schizophrenia, SES and cognitive functioning. Schizophr Bull 37:664–670
Hollis C (2000) Adult outcomes of child- and adolescent-onset schizophrenia: diagnostic stability and predictive validity. Am J Psychiatry 157:1652–1659
Dickinson D, Ramsey ME, Gold JM (2007) Overlooking the obvious: a meta-analytic comparison of digit symbol coding tasks and other cognitive measures in schizophrenia. Arch Gen Psychiatry 64:532–542
Knowles EE, David AS, Reichenberg A (2010) Processing speed deficits in schizophrenia: reexamining the evidence. Am J Psychiatry 167:828–835
Baron RM, Kenny DA (1986) The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51:1173–1182
Harvey PD, Keefe RS, Patterson TL, Heaton RK, Bowie CR (2009) Abbreviated neuropsychological assessment in schizophrenia: prediction of different aspects of outcome. J Clin Exp Neuropsychol 31:462–471
Brebion G, David AS, Bressan RA, Pilowsky LS (2006) Processing speed: a strong predictor of verbal memory performance in schizophrenia. J Clin Exp Neuropsychol 28:370–382
Holthausen EA, Wiersma D, Sitskoorn MM, Dingemans PM, Schene AH, Van Den Bosch RJ (2003) Long-term memory deficits in schizophrenia: primary or secondary dysfunction? Neuropsychology 17:539–547
Cirillo MA, Seidman LJ (2003) Verbal declarative memory dysfunction in schizophrenia: from clinical assessment to genetic and brain mechanisms. Neuropsychol Rev 13:43–77
Rund BR, Zeiner P, Sundet K, Oie M, Bryhn G (1998) No vigilance deficit found in either young schizophrenic or ADHD subjects. Scand J Psychol 39:101–107
Oie M, Rund BR (1999) Neuropsychological deficits in adolescent-onset schizophrenia compared with attention deficit hyperactivity disorder. Am J Psychiatry 156:1216–1222
Menezes NM, Malla AM, Norman RM, Archies S, Roy P, Zipursky RB (2009) A multi-site Canadian perspective: examining the functional outcome from first-episode psychosis. Acta Psychiatr Scand 120:138–146
Frazier JA, McClellan J, Findling RL, Vitiello B, Anderson R, Zablotsky B et al (2007) Treatment of early-onset schizophrenia spectrum disorders (TEOSS): demographic and clinical characteristics. J Am Acad Child Adolesc Psychiatry 46:979–988
Sparrow SS, Cicchetti DV, Balla A (2005) Vineland adaptive behavior scales. American Guidance Service, Circle Pines
Hodges K (1995) Child and adolescent functional assessment scale. Departement of Psychology, Eastern Michigan University, Ypsilanti
Leifker FR, Patterson TL, Heaton RK, Harvey PD (2009) Validating measures of real-world outcome: the results of the VALERO expert survey and RAND panel. Schizophr Bull 37:334–343
Burns T, Patrick D (2007) Social functioning as an outcome measure in schizophrenia studies. Acta Psychiatr Scand 116:403–418
Addington J, Addington D (2007) Patterns, predictors and impact of substance use in early psychosis: a longitudinal study. Acta Psychiatr Scand 115:304–309
Fagerlund B, Pagsberg AK, Hemmingsen RP (2006) Cognitive deficits and levels of IQ in adolescent onset schizophrenia and other psychotic disorders. Schizophr Res 85:30–39
van Os J, Burns T, Cavallaro R, Leucht S, Peuskens J, Helldin L et al (2006) Standardized remission criteria for schizophrenia. Acta Psychiatr Scand 113:91–95
Acknowledgments
Supported in part by “Instituto de Salud Carlos III”, “Fondo Investigaciones Sanitarias (FIS)” and by the Government of Catalonia, Comissionat per Universitats i Recerca del Departament d’Innovació, Universitats i Empresa 2009-SGR-1119.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Puig, O., Penadés, R., Baeza, I. et al. Processing speed and executive functions predict real-world everyday living skills in adolescents with early-onset schizophrenia. Eur Child Adolesc Psychiatry 21, 315–326 (2012). https://doi.org/10.1007/s00787-012-0262-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-012-0262-0