Abstract
Objectives
The aim of this study was to investigate the mechanical, chemical, optical, and adhesive properties of BisGMA-free experimental resin composites containing Exothane-24—an elastomeric urethane monomer—and different co-initiators.
Materials and methods
A blend of urethane dimethacrylate (UDMA), extended dimethacrylate urethane (PEG 400), triethylene glycol dimethacrylate (TEGDMA), and camphorquinone was prepared. Two different co-initiators—dimethyl aminoethyl methacrylate (DMAEMA) or 4-N alcohol, N-dimethylamine phenylethyl (DMPOH)—were added to the blend. Exothane-24 monomer was added to the blend for each co-initiator and four groups were established as follows: DMAEMA; DMAEMA + Exothane; DMPOH; and DMPOH + Exothane. Specimens were photo-activated using a multi-wave LED light-curing unit (VALO; 954 mW/cm2 of irradiance). Mechanical (ultimate tensile strength, flexural strength, flexural modulus and hardness), chemical (degree of conversion, hardness reduction, water sorption and solubility), optical (color change), and adhesive (microtensile bond strength) properties were analyzed. Data were submitted to two-way ANOVA and Tukey’s test (α = 0.05).
Results
The resin composite containing DMPOH and Exothane-24 showed similar or superior performance to those of the other experimental composites for mechanical and chemical properties, except for flexural strength. It also showed less color change and greater micro-tensile bond strength.
Conclusions
Among the combinations tested, the BisGMA-free resin composite containing Exothane-24 combined with the DMPOH co-initiator showed the best mechanical, chemical, optical, and adhesive properties.
Clinical relevance
Exothane-24 monomer and DMPOH co-initiator could be useful in the formulation of BisGMA-free resin composites in order to minimize exposure to BPA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dental resin composites are frequently used for direct restorations in dentistry [1]. One of the drawbacks of these materials is the shrinkage resulting from polymerization; this condition, leads to stress in the adhesive interface, often causing complications such as cusp deflection, postoperative sensitivity, recurrent caries, and gap formation [2, 3]. To minimize these complications and to compensate for the lack of in-depth polymerization of the light-cured resin composites, the incremental insertion technique is recommended [4].
The chemical composition of resin composites basically includes monomers, such as Bis-GMA (bisphenol A glycerolate dimethacrylate), Bis-EMA (bisphenol A ethoxylate dimethacrylate), UDMA (urethane dimethacrylate), and TEGDMA (triethylene glycol dimethacrylate) [5, 6]. To reduce the polymerization shrinkage stress, alternative monomers have been tested to provide the composite with better physical and chemical properties [7].
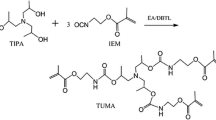
Among these monomers is the elastomeric urethane, commercially known as Exothane™. It could be used in a wide range of dental resin materials to provide them with better viscoelastic properties, lower elastic modulus, and higher resistance to abrasion and chemicals [8, 9]. Among the types of Exothane™, Exothane-24 has physicochemical properties that seem more suitable than those of UDMA and BisGMA, monomers commonly found in resin-based composites [8, 9]. As a categorically elastomeric monomer, Exothane-24 can increase the mobility and the relaxation capacity of the forming polymer network due to the size of its molecule. Due to its higher elongation and toughness, Exothane-24 might also minimize the polymerization shrinkage effect by dissipating the stress generated [10], a condition that might preserve the adhesion of the restorative resin composite in preparations with high C-factor and in those with margins in dentin [4].
Also, it could be an alternative to Bis-GMA, because the potential presence of bisphenol-A (BPA) as an impurity or a degradation product from dental resins has raised concerns around the use of BisGMA-containing formulations [11]. Some studies have found the presence of BPA in patient’s urine and saliva after dental procedures, which is worrisome due to its capability for triggering estrogenic effects, especially in pediatric patients [12,13,14]. The worldwide trend is that bisphenol-A-based materials, especially those used to manufacture household utensils, are to be banned [15]. However, bisphenol-based monomers (Bis-GMA and Bis-EMA) have less polymerization shrinkage than other monomers used as diluents due to their higher molecular weight. In this sense, the addition of Exothane-24 in BisGMA-free resin composites would be interesting to minimize the effects of the polymerization shrinkage, since it also has high molecular weight.
Alternative monomers based on urethane methacrylates are being investigated in an attempt to replace the BisGMA in resin composite formulations [6, 16]. The urethane methacrylates have a chemical structure that can be easily tailored, making it possible to design and synthesize a wide variety of monomers with different physicochemical properties [11], such as PEG400, UDMA, and Exothane™. Recently, showing a promising outcome, a newly synthesized hydrophobic, rigid core, and low viscosity diurethane dimethacrylate (2EMATE-BDI) was tested as an alternative monomer used in combination with a UDMA-based monomer to achieve BisGMA-free formulations [11].
Resin composites have photo-initiators that can be activated by visible light within the blue-violet spectrum of 400–500 nm. Generally, camphorquinone (CQ) is used as the photo-initiator, associated with a tertiary amine—a co-initiator [17, 18]. The tertiary amines most commonly found in resin composite formulations are DMAEMA (dimethyl aminoethyl methacrylate) and EDMAB (4-dimethylamino benzoate) [19].
The double bonds of aromatic amines can absorb UV light, creating color centers called chromophores, which increase the absorption of visible light particularly in the blue electromagnetic spectrum, resulting in a yellowing of the material [20]. Some amines, such as the DMPOH (4-N alcohol, N-dimethylamine phenylethyl) having greater color stability when compared with other co-initiators, have been investigated and suggested as an alternative to DMAEMA and EDMAB [21, 22]. Also, DMPOH showed a degree of conversion (DC) and mechanical properties similar or superior to those observed for DMAEMA and EDMAB [20, 21].
Based on previous findings, changes in the chemical composition of the BisGMA-free resin composites could provide them with better mechanical, chemical, and optical properties and consequently improve their bond strength to the tooth. Therefore, the aim of the present study was to investigate the mechanical, chemical, and optical properties of four BisGMA-free resin composites, two of which, containing elastomeric urethane monomers and different co-initiators. The hypotheses were that the elastomeric urethane monomers and different co-initiators would provide the experimental BisGMA-free resin composites with better or similar (1) bond strength, and (2) mechanical, (3) chemical, and (4) optical properties.
Materials and methods
Table 1 illustrates the materials used to formulate the experimental resin composites.
Experimental resin composite preparation
A centrifugal mixing device (SpeedMixer, DAC 150.1 FVZ-K, Hauschild Engineering, Hamm, North Rhine-Westphalia, Germany) was used to blend the composites. Four organic matrices were prepared according to the combination of monomers and photo-initiator systems:
-
1)
60 wt% UDMA; 25 wt% PEG400; 14 wt% TEGDMA; 0.5 wt% CQ, 0.5 wt% DMAEMA
-
2)
60 wt% UDMA; 25 wt% PEG400; 14 wt% TEGDMA; 0.5 wt% CQ, 0.5 wt% DMPOH
-
3)
35 wt% UDMA; 25 wt% PEG400; 25 wt% Exothane-24; 14 wt% TEGDMA; 0.5 wt% CQ, 0.5 wt% DMAEMA
-
4)
35 wt% UDMA; 25 wt% PEG400; 25 wt% Exothane-24; 14 wt% TEGDMA; 0.5 wt% CQ, 0.5 wt% DMPOH
Filler particles (10 wt% of 0.05-μm fumed silica and 55 wt% of 2.0-μm BaBSiO2 glass) were then added to each organic matrix. To avoid spontaneous polymerization, 0.01 wt% BHT inhibitor was added to all resin composites.
Flexural strength (FS) and flexural modulus (FM)
Ten bar-shaped specimens (7 mm long × 2 mm wide × 1 mm thick) [22] of each experimental resin composite were made using rubber molds. The resin composite was inserted into the mold, compressed with a flat glass slab, and light-cured for 40 s (Valo Cordless, Ultradent Products Inc, South Jordan, UT, USA) at 954 mW/cm2 irradiance. After polymerization, the specimens were demolded, stored dry in lightproof containers at 37ºC for 24 h, and then tested for flexural strength (FS) and flexural modulus (FM) (three-point bending test; 5-mm span between supports) using a universal testing machine (Instron, Canton, MA, USA) at a crosshead speed of 0.5 mm/min. The load was applied to the surface of the specimen that was irradiated. FS was calculated in MegaPascal (MPa) and FM in GigaPascal (GPa) using the following equations:
where L refers to the maximum load at failure (N), D to the distance between the supports, W to specimen width, h to specimen height, and d to crosshead displacement.
Ultimate tensile strength
Specimens (n = 10) of each experimental resin composite were fabricated using 1-mm-thick hourglass-shaped silicon molds (10 × 4 mm), containing a constriction of 1.5 × 1 mm (cross-sectional area of 1.5 mm2; Odeme Dental Research, Luzerna, SC, Brazil). They were inserted into the mold, compressed with a flat glass slab, and light-cured for 40 s (Valo Cordless, 954 mW/cm2; Ultradent, USA) and stored as previously mentioned. Specimens were fitted in a test jig device and tested for ultimate tensile strength (UTS) in a mechanical testing machine OM100 (Odeme Dental Research) at a crosshead speed of 0.75 mm/min. The UTS was calculated using the following formula: UTS = F/A, where F indicates the maximum fracture load (N) and A the transversal cross-sectional area (mm2). UTS values were expressed as MPa.
Knoop microhardness
Disk-shaped specimens (n = 10) of each resin composite were fabricated in a rubber mold with circular cavities (7 mm in diameter and 2 mm thick), in which the composite was inserted in a single increment and compressed with a flat glass slab. The specimens were then light-cured for 40 s (Valo Cordless, 954 mW/cm2; Ultradent, USA) and stored for 24 h at 37 °C, in dark and dry condition.
The specimen’s surface exposed to curing light was sandpaper polished, with the grits decreasing gradually—320, 400, 600, and 1000—and submitted to the Knoop microhardness test using in a microdurometer (HMV-2000; Shimadzu, Tokyo, Japan), at a load of 50 g for 15 s. Five readings were recorded for each specimen and the arithmetic mean value was then calculated.
Microhardness reduction
Following the Knoop microhardness (KH) test, the disk-shaped specimens (n = 10) were stored in 100% ethanol (Sigma-Aldrich Inc, USA) for 24 h for chemical softening [24]. To verify the microhardness reduction (HR) (%), the specimens were then resubmitted to the KH test. Five readings were taken for each specimen, considering the same surface previously tested. The average of the five readings was established as the HR mean value for each specimen. The HR was defined by the reduction in the KH values after ethanol storage and expressed as percentage.
Water sorption and solubility
These tests were done in compliance with ISO 4049:2019. To verify the Wsp and Wsl, disk-shaped specimens (n = 10; 1 mm thick × 15 mm in diameter) were light-cured for 40 s (Valo Cordless, 954 mW/cm2; Ultradent, USA), stored in silica gel-containing desiccators at 37 °C, and weighed daily using a digital analytical balance (accuracy 0.1 mg; Chyo Balance Co., model JK-180, Kyoto, Japan) until a constant mass (mL) was obtained (i.e., until mass change of each specimen was not more than ± 0.1 mg in any 24 h period). Thickness and diameter of each specimen were measured using a digital electronic caliper (Mitutoyo Corporation, Tokyo, Japan). Mean values were used to calculate the volume (V) of each specimen (mm3). The specimens were stored in plastic vials with 10 mL of distilled water at 37 °C for 7 days. The specimens were then removed from the plastic vials, washed with water, surface water blotted away until free from visible moisture, waved in the air for 15 s, and finally weighed 1 min after removal from the plastic vials. This mass was registered as m2, and the specimens were returned to the desiccators. The mass reconditioning cycle was repeated and the constant mass (m3) was recorded again (until mass change of each specimen was not more than ± 0.1 mg in any 24 h period). The values (μg/mm3) for Wsp and Wsl were calculated using the following equations:
Degree of conversion
Fourier transform near infrared spectroscopy (FT-NIR) was used to measure the cure efficiency for each resin composite. Five resin composite disks (7 mm in diameter and 2 mm thick) were made in rubber molds and light-cured for 40 s (Valo Cordless, 954 mW/cm2; Ultradent, USA). Each sample was clamped in a holder inside the NIR chamber (Nicolet Nexus 6700, Thermo Scientific, Waltham, MA, USA). Unconverted carbon double bonds were quantified by calculating the ratio derived from the aliphatic C = C (vinyl) absorption (6165 cm−1) to the aromatic C = C absorption (4623 cm−1) signals for both polymerized and non-polymerized samples. Absorbance spectra involved 16 scans at a resolution of 1 cm−1. The DC was calculated as follows: \(DC \left(\%\right)=\left(1- \frac{R pol}{R non pol}\right) x 100\), where R indicates the ratio of the peak areas at 6165 cm−1 and 4623 cm−1 in the polymerized (pol) and non-polymerized (non-pol) specimens.
Color change
The disk-shaped specimens (n = 10; 10 mm in diameter × 1 mm thick) of each experimental resin composite were made in rubber molds and light-cured for 40 s (Valo Cordless, 954 mW/cm2; Ultradent, USA). The specimens were finished and polished using wet sandpapers (#600, #800, and #1200) and 1-µm diamond suspension applied with felkt disk for 60 s using a polishing machine (Buehler, Lake Bluff, IL, USA). To evaluate the color change (CC) concerning each specimen, CIELAB coordinates (L*, a*, b*) were recorded before and after the UV artificial aging using a spectrophotometer (CM700d, Konica Minolta, Tokyo, Japan) with a D65 illuminant on a white ceramic tile (CIE L* = 91.1; a* = 1.2; b* = − 3.4; and Y = 78.8). Differences in each parameter were determined as ΔL*, Δa*, and Δb* by subtracting the coordinate parameter values obtained before aging from those recorded after aging (+ L* = white, − L* = black; + a* = red, − a* = green; + b* = yellow, − b* = blue). To determine the CC, ΔE of each specimen was calculated using the CIEDE2000 (ΔE00) formula:
All resin composite specimens were UV-light aged for 120 h at 37 °C. To standardize the UV-light exposure, the specimens were placed 10 cm away from the UV light bulb (UV-B 313, Equilam, Diadema, SP, Brazil).
Microtensile bond strength
Forty sound human third molars were extracted, cleaned, and stored in an aqueous solution containing 0.2 wt.% thymol at 4 °C up to 3 months before test (Protocol # 55,806,016.6.0000.5418, Local Research Ethics Committee). Their roots were cut off 2 mm below the cementoenamel junction using a diamond wafering blade mounted in a cutting machine (Isomet 1000, Büehler, Lake Buff, IL, USA). A box-shaped cavity was made in each tooth according to a technique proposed by Silame et al. [25]. A caliper (Minellium, São Caetano do Sul, SP, Brazil) was then used to measure the distance from the pulp chamber roof to the occlusal surface. Resin composite (Charisma, Hereus Kulzer, Dormagen, Germany) was bonded (Adper Single Bond-2 adhesive system, 3 M/ESPE, St. Paul, MN, USA) to the occlusal surface of each tooth and pressed to form a flat surface. All procedures were carried out according to the manufacturers’ instructions.
The teeth were fixed to a standardized preparation machine (Elquip, São Carlos, SP, Brazil), coupled with a high-power turbine (Kavo, Joinvile, SC, Brazil) and cylindrical diamond burs (#3099, KG Sorensen, São Paulo, SP, Brazil). A box-shaped class I cavity (5 mm in length, 4 mm in width, and 4 mm in depth; C-factor ≈4.5) was made in each tooth. The diamond bur was discarded after 5 preparations.
The teeth were assigned to 4 groups (n = 10), according to each experimental resin composite. Each cavity was acid-etched for 15 s with 35% phosphoric acid (3 M ESPE, USA) and washed—water excess was removed. Adhesive system (Adper Single Bond 2, 3 M ESPE, USA) was applied under its manufacturer’s instructions and light-cured for 10 s (Valo Cordless, 954 mW/cm2; Ultradent, USA). Each experimental resin composite was then horizontally inserted into the cavity in two increments of 2 mm, and light-cured for 40 s (Valo Cordless, 954 mW/cm2; Ultradent, USA). All restored teeth were kept in water at 37 °C for 24 h.
After water storage (24 h), each restored tooth was sectioned in the X and Y directions, perpendicular to the bottom adhesive-tooth interface, using a low-speed diamond wafering blade (Isomet 1000, Buehler, USA) under water cooling to obtain beams with a cross-sectional area of approximately 0.81 mm2 (0.9 × 0.9 mm). Cyanoacrylate-based glue (Super Bonder gel, Loctite, Henkel, Düsseldorf, Germany) was used to attach the beams to a microtensile device, coupled to a testing machine (OM100; Odeme, Luzerna, SC, Brazil) at a crosshead speed of 0.75 mm/min until fracture. The μTBS values (MPa) were calculated dividing the fracture load (N) by the surface area (mm2) of each beam.
Each tooth yielded a different number of beams. The mean value for each tooth was calculated by summing the μTBS value of each beam and dividing that by the number of beams obtained from each tooth. The μTBS mean value for each group was obtained by summing the μTBS mean values of each tooth and dividing that by the number (n = 10) of teeth in each group.
Each interfacial fracture pattern was analyzed using a stereomicroscope (Olympus Corp, Tokyo, Japan) at × 40 magnification and classified as (1) cohesive in dentin, (2) cohesive in composite, (3) adhesive, or (4) mixed.
Statistical analysis
The sample size for each test had a power of at least 0.8 at a significance level of 0.5 (β = 0.2). Data normality was verified using Shapiro–Wilk’s test and the homoscedasticity using Lavene’s test. Statistical analyses were carried out according to the different experimental designs at a significance level of α = 0.05. Data concerning FS, FM, UTS, KH, HR, Wsp, Wsl, DC, CC, and μTBS were statistically analyzed by Two-Way ANOVA—factors: the resin matrix (with and without Exothane-24) and the type of co-initiator (DMAEMA and DMPOH)—and Tukey’s test (α = 0.05), using the SPSS software (version 15.0; Statistical Package for the Social Science, SPSS Inc., Chicago, IL, USA).
Results
Table 2 shows the mean values and standard deviations for FS and FM, regarding all resin composites tested. For both tests, no statistical difference was observed between DMAEMA and DMPOH (FS—p = 0.52923; FM – p = 0.99080), considering both resin matrices. However, statistical difference (FS—p = 0.00805; FM – p = 0.00879) was observed between the resin matrices, where the resin composites without Exothane-24 showed higher mean values for both co-initiators.
Table 3 shows the mean values and standard deviations for UTS and CC concerning all resin composites tested. For UTS, no significant difference was observed between the co-initiators and between the resin matrices (p = 0.12601). For CC, no statistical difference was observed between the resin matrices (p = 0.97521). However, statistical difference (p = 0.01575) was observed between the co-initiators, where DMAEMA showed higher mean values considering both resin matrices.
Table 4 shows the mean values and standard deviations for KH and HR regarding the resin composites tested. The KH test showed no significant difference between the co-initiators (p = 0.256209). However, statistical difference (p = 0.01289) was observed between the resin matrices, where the resin matrix containing Exothane-24 and DMPOH showed higher mean values than that without Exothane-24. No difference was found between the resin matrices containing DMAEMA.
The HR test showed statistical difference (p = 0.0001) between the resin matrices, where the resin composite with Exothane-24 showed lower mean values, for both co-initiators. Statistical difference was observed between the co-initiators for the resin composite without Exhotane-24, where DMPOH showed lower HR mean values. No statistical difference was found between the co-initiators for the resin composite containing Exothane-24.
Table 5 shows the mean values and standard deviations for Wsp and Wsl regarding all the resin composites tested. Wsp analysis showed statistical difference between the resin matrices and between the co-initiators (p = 0.00152), where the resin matrix containing Exothane-24 showed lower mean values than that without Exothane-24 for both co-initiators. The resin composites containing DMPOH showed lower mean values than those with DMAEMA for both resin matrices. As for Wsl, no significant difference was observed between the co-initiators and between the resin matrixes (p = 0.29636).
Table 6 shows the mean values and standard deviation for DC and microtensile bond strength (µTBS) concerning all the resin composites tested. No statistical difference was observed between DMAEMA and DMPOH (DC, p = 0.10673; µTBS, p = 0.67462) for both resin matrices. Statistical difference (DC—p = 0.00001; µTBS – p = 0.00001) was found between the resin matrices, where the Exothane-24 resin composites showed higher mean values for both co-initiators.
Figure 1 shows the distribution of fracture patterns regarding all groups. The mixed, cohesive in dentin, and adhesive patterns were more predominant than the cohesive in composite.
Discussion
The hypotheses that the elastomeric urethane monomers and different co-initiators would provide the experimental BisGMA-free resin composites with better or similar mean values for (1) bond strength and (3) chemical, and (4) optical properties were accepted, because the experimental resin composite containing Exothane-24 and the co-initiator DMPOH showed better or similar mean values for all these properties when compared with those of the other experimental composites. However, the hypothesis referring to the (2) mechanical properties was rejected because the resin composites containing Exothane-24 (with both co-initiators) showed lower FS and FM mean values when compared with those without Exothane-24.
This study evaluated the effects of Exothane-24 and different co-initiators on BisGMA-free resin composites aimed at improving their mechanical, chemical, optical, and adhesive properties. Mechanical, chemical, optical, and adhesion tests were carried out to plead for a new formulation of a BisGMA-free resin composite. Changes in the composition of composites have been investigated; such changes must meet specific requirements related to the properties mentioned above [26, 27].
When added to resin composites, monomers such as UDMA, PEG400, and TEGDMA are known to increase the extension and stiffness of the polymer chains in composites [6]. In the present study, while the co-initiators had no influence, Exothane-24 significantly decreased the FS and FM of the resin composites (Table 2), probably due to the reduction in the polymer chain stiffness, which was already expected for this type of elastomeric monomer [6]. In an attempt to carry out light-curing in one shot, the specimens’ dimensions (10 × 2 × 2 mm) were reduced when compared with those established by ISO 4049 (25 × 2 × 2 mm). Yap et al. [28] reported comparable results with specimens (12 × 2 × 2 mm) smaller than those established by ISO 4049 and suggested such dimensions could be an alternative to those recommended by ISO 4049, provided that the same formula and test conditions be used. Despite the decrease in FS, Exothane-24 showed no decrease in the UTS of the resin composites, a condition that could clinically increase the risk for restoration fracture. However, the reduction in FM is a factor that could clinically decrease the shrinkage stress during the polymerization of the material, preserving the resin composite bonding to the tooth.
Table 3 shows the UTS mean values. No statistically significant difference was observed between DMAEMA and DMPOH co-initiators, and between the matrices with Exothane-24 and those without. The UTS test is considered a reliable approach to evaluate the mechanical properties of both resin composites and tooth structures [29]. Unlike the FS test, having the tensile and compression stresses as its basis (in addition to shear stress, as a resultant), the UTS test has predominantly tensile stress [9], which might explain our results obtained with the FS and UTS tests. In the present study, the UTS results obtained with BisGMA-free resin composites without (68–72 MPa) and with Exothane-24 (68–70 MPa) were lower than those reported in studies [29, 30] on nano-hybrid composites (94–98 MPa) and higher than those found in studies on resin cements (28–33 MPa) [31] and resin-based fissure sealants (35–39 MPa) [32]. This difference might be related to the number and type of filler particles in the organic matrix of resinous materials. No studies were found to apply the UTS test to BisGMA-free resin composites.
Table 4 shows KH and HR mean values for the resin composites tested. The resin composite containing DMPOH and Exothane-24 showed higher KH mean values than that having no Exothane-24. Among the co-initiators used with composites containing camphorquinone, DMPOH is the most reactive, a characteristic that might increase the polymeric network of the resin composite [19, 22]. Also, the higher KH mean values obtained for the DMPOH and Exothane-24 group might be related to the higher degree of conversion (Table 6). Regarding the HR mean values, the groups containing both co-initiators and Exothane-24 showed lower values, with the quality of the polymer chains being significantly better. Such lower mean values might be due to the higher cross-link density of the composite [27].
Table 5 shows the Wsl mean values for the experimental composites tested. Wsl analysis showed no statistically significant difference among the groups. This finding might be due to the inability of the resin composite to solubilize in aqueous medium; also, the 7-day period of water immersion might have been insufficient for the leaching of the resin composite [33]. Table 5 also shows Wsp mean values for the resin composites tested, where those containing Exothane-24 showed significantly lower values when compared to those having no Exothane-24. Simpler than the Wsl test, the Wsp test leads to less variability in the results because the specimens undergo drying only once. Consequently, statistical difference between groups, even with very close mean values, is expected. Clinically, solubility is not a concern for resinous materials [34]; however, sorption can lead to staining of the resin composite surface due to polymer degradation and the inclusion of dietary pigments.
The resin composites containing Exothane-24 showed significantly lower Wsp values, suggesting that water absorption might have been impaired by Exothane-24, which is known to be highly hydrophobic [10]. In addition, Exothane-24 might also account for the significantly lower HR values obtained for the groups containing Exothane-24 (Table 6); such lower values might be due to the higher cross-link density of the composite, a condition that might have reduced the water diffusion into the resin composite.
When compared with DMAEMA, with or without Exothane-24, DMPOH showed significantly lower Wsp mean values (Table 5). This finding might be due to the lower HR values of composites containing DMPOH. Also, the water diffusion into the resin composite structure might have been reduced by the high cross-link density of the polymeric network formed, leading to less water absorption.
DC is the chemical property used to measure the conversion of monomers into polymers [35]. According to Fugolin et al. [11], when compared with those containing BisGMA-TEGDMA, the resin composites containing UDMA-TEGDMA showed higher DC values. Such finding might be due to the lack of a stiff central core in the UDMA-TEGDMA and the strong intermolecular hydrogen bonding ability of the BisGMA [11]. The network formed with UDMA is less sterically hindered, allowing higher molecular mobility to the reaction environment and, consequently, promoting segmental movement of radicals up to later stages in conversion [11]. In the present study, the DC mean values (Table 6) were similar to those reported by Fugolin et al., probably due to the greater mobility of the polymer chains during the polymerization reaction of the BisGMA-free resin composite [11], which contains no viscous monomers, such as Bis-GMA [36, 37].
When the two co-initiators were compared, no statistical difference was observed for DC (Table 6). However, when compared with the composites without, those with Exothane-24 showed statistically higher DC mean values for both co-initiators. This finding might be correlated with the high DC (around 94 to 98%) of Exothane-24, as described by its manufacturer (Esstech, Inc., Essington, PL, USA), a factor that can increase the final conversion of a resin composite containing this monomer [38]. Besides, the greater mobility of the Exothane-24 in the polymer chains during the polymerization reaction of the resin composite may have contributed to the increase in the DC.
Exothane-24 had no influence on the CC (ΔE00) mean values for all resin composites (Table 3). However, the resin composites containing DMPOH showed CC mean values significantly lower than those obtained for the composites containing DMAEMA. Because the specimens were exposed to artificial accelerated aging with UV-B light [20], color changes were expected since the co-initiators, combined with camphorquinone, have different levels of absorbance in the UV-B light.
DMAEMA is known to absorb UV light more intensively than DMPOH and, thus, it is more prone to color change caused by amine oxidation [22]. All non-reacted amines have double bonds and can absorb UV light and, thus, reach high stages of energy, during which they react with non-reacted monomers or impurities. Consequently, larger and more conjugated systems, also called color centers or chromophores, are formed [21]. Thus, clinically, resin composites containing DMPOH could result in better color stability when exposed to oxidation-inducing factors.
In the present study, the µTBS mean values in all groups were lower (12.50 to 18.42 MPa) than those reported in previous studies using flat surfaces [39, 40]. This might be due to the severe closure condition of the box-shaped cavity provided for the composites during the µTBS test. These cavities were made by using the pulp chamber of molar teeth, which resulted in a challenging situation for the adhesive interface since the C-factor in these conditions is very high [4, 25]. Silame et al. [25], using the same box-shaped cavity condition as that of the present study, reported µTBS values slightly higher (20 to 23 MPa) than those found in the present study (12–14 MPa, no Exothane-24 and 17–18 MPa, with Exothane-24) for 2-mm increments. Probably, differentiations in the monomers and filler content in the organic matrix of the resin composites, as well as in the adhesive system used, might have contributed to the different µTBS mean values. Ersen et al. [41], evaluating box-shaped preparations with high C-factor, reported that different types of bulk-fill resin composites showed variation in the polymerization shrinkage and a decrease in the volumetric shrinkage of the composites in the cavity when the adhesive system was used. Thus, the behavior of a composite with greater resilience under such closure conditions should be further investigated.
Data analysis (Table 6) showed no effect of the co-initiators on µTBS. However, the composites containing Exothane-24 showed µTBS mean values statistically higher than those obtained for the composites without Exothane-24. The mechanical and chemical tests showed favorable results for the composites containing Exothane-24 in the µTBS test. The lowest FM mean values, the highest DC mean values, and the elastic characteristics of Exothane-24 may account for the better µTBS results obtained for the composites containing Exothane-24. Despite the higher degree of conversion, the shrinkage stress generated may have been compensated by the lower FM, as well as by the greater elongation and toughness of Exothane-24, contributing to the lower probability of adhesive debonding and higher µTBS mean values [42]. The fracture pattern analysis (Fig. 1) showed higher prevalence for failure types I (cohesive in dentin), III (adhesive), and IV (mixed), when compared with type II (cohesive in composite). This reflects the good mechanical properties of the BisGMA-free resin composites tested and the different stresses on the adhesive interface during the polymerization of the resin composites within the cavities.
Based on the findings of the present study, the monomeric matrix containing Exothane-24, associated with DMPOH, might be a promising BisGMA-free resin composite for direct restorations. The dental market today has few options for BisGMA-free resin composites and this monomeric matrix could be an alternative to the existing ones because of its good optical and adhesive properties. However, further studies are needed to evaluate the shrinking stress and the cytotoxicity of these novel restorative materials as to verify the findings of this study.
Conclusion
Exothane-24—an elastomeric urethane monomer—associated with DMPOH—a co-initiator—provided the BisGMA-free resin composite with better or similar mechanical, chemical, optical, and adhesive properties when compared with those of the other groups, except for FS and FM. Therefore, it may be a promising formulation for direct restorations.
References
Van Dijken JW, V, Lindberg A, (2015) A 15-year randomized controlled study of a reduced shrinkage stress resin composite. Dent Mater 31:1150–1158. https://doi.org/10.1016/j.dental.2015.06.012
Jang J-H, Park S-H, Hwang I-N (2015) Polymerization shrinkage and depth of cure of bulk-fill resin composites and highly filled flowable resin. Oper Dent 40:172–180. https://doi.org/10.2341/13-307-L
Moorthy A, Hogg CH, Dowling AH, Grufferty BF, Benetti AR, Fleming GJP (2012) Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. J Dent 40:500–505. https://doi.org/10.1016/j.jdent.2012.02.015
Ferracane JL (2011) Resin composite - state of the art. Dent Mater 27:29–38. https://doi.org/10.1016/j.dental.2010.10.020
Floyd CJE, Dickens SH (2006) Network structure of Bis-GMA- and UDMA-based resin systems. Dent Mater 22:1143–1149. https://doi.org/10.1016/j.dental.2005.10.009
Moszner N, Fischer UK, Angermann J, Rheinberger V (2008) A partially aromatic urethane dimethacrylate as a new substitute for Bis-GMA in restorative composites. Dent Mater 24:694–699. https://doi.org/10.1016/j.dental.2007.07.001
Leprince JG, Palin WM, Vanacker J, Sabbagh J, Devaux J, Leloup G (2014) Physico-mechanical characteristics of commercially available bulk-fill composites. J Dent 42:993–1000. https://doi.org/10.1016/j.jdent.2014.05.009
Ferracane JL (2006) Hygroscopic and hydrolytic effects in dental polymer networks. Dent Mater 22:211–222. https://doi.org/10.1016/j.dental.2005.05.005
Van Landuyt KL, Snauwaert J, De Munck J, Peumans M, Yoshida Y, Poitevin A, Coutinho E, Suzuki K, Lambrechts P, Van Meerbeek B (2007) Systematic review of the chemical composition of contemporary dental adhesives. Biomaterials 28:3757–3785. https://doi.org/10.1016/j.biomaterials.2007.04.044
Münchow EA, De BGD, Alves S, Valente LL, Cava S, Piva E, Ogliari FA (2014) Effect of elastomeric monomers as polymeric matrix of experimental adhesive systems : degree of conversion and bond strength characterization. Appl Adhes Sci 2:3. https://doi.org/10.1186/2196-4351-2-3
Fugolin AP, de Paula AB, Dobson A, Huynh V, Consani R, Ferracane JL, Pfeifer CS (2020) Alternative monomer for BisGMA-free resin composites formulations. Dent Mater 36:884–892. https://doi.org/10.1016/j.dental.2020.04.009
Becher R, Wellendorf H, Sakhi AK, Samuelsen JT, Thomsen C, Bølling AK, Kopperud HM (2018) Presence and leaching of bisphenol a (BPA) from dental materials. Acta Biomater Odontol Scand 4:56–62. https://doi.org/10.1080/23337931.2018.1476869
Kingman A, Hyman J, Masten SA, Jayaram B, Smith C, Eichmiller F, Arnold MC, Wong PA, Schaeffer JM, Solanki S, Dunn WJ (2012) Bisphenol A and other compounds in human saliva and urine associated with the placement of composite restorations. J Am Dent Assoc 143:1292–1302. https://doi.org/10.14219/jada.archive.2012.0090
Maserejian NN, Trachtenberg FL, Wheaton OB, Calafat AM, Ranganathan G, Kim H-Y, Houser R (2016) Changes in urinary bisphenol A concentrations associated with placement of dental composite restorations in children and adolescents. J Am Dent Assoc 147:620–630. https://doi.org/10.1016/j.adaj.2016.02.020
vom Saal FS, Nagel SC, Coe BL, Angle BM, Taylor JA (2012) The estrogenic endocrine disrupting chemical bisphenol A (BPA) and obesity. Mol Cell Endocrinol 354:74–84. https://doi.org/10.1016/j.mce.2012.01.001
González-López JA, Pérez-Mondragón AA, Cuevas-Suárez CE, Alonso JC, Trejo-Carbajal N, Herrera-González AN (2019) Hydrophobic composite resins using a novel allylic urethane monomer as additive. J Mex Chem Soc 63:105–114. https://doi.org/10.29356/jmcs.v63i4.877
Taira M, Urabe H, Hirose T, Wakasa K, Yamaki M (1988) Analysis of photo-initiators in visible-light-cured dental composite resins. J Dent Res 67:24–28. https://doi.org/10.1177/00220345880670010401
Ogunyinka A, Palin WM, Shortall AC, Marquis PM (2007) Photoinitiation chemistry affects light transmission and degree of conversion of curing experimental dental resin composites. Dent Mater 23:807–813. https://doi.org/10.1016/j.dental.2006.06.016
Schroeder WF, Vallo CI (2007) Effect of different photoinitiator systems on conversion profiles of a model unfilled light-cured resin. Dent Mater 23:1313–1321. https://doi.org/10.1016/j.dental.2006.11.010
Oliveira DC, Silva CB, Muniz BV, Volpato MC, Costa AR, Sinhoreti MA (2014) Effect of 4-(N, N-dimethylamino)phenethyl alcohol on degree of conversion and cytotoxicity of photo-polymerized CQ-based resin composites. Braz Dent J 25:538–542. https://doi.org/10.1590/0103-6440201300113
De Oliveira DCRS, Ayres APA, Rocha MG, Giannini M, Puppin Rontani RM, Ferracane JL, Sinhoreti MA (2015) Effect of different in vitro aging methods on color stability of a dental resin-based composite using CIELAB and CIEDE2000 color-difference formulas. J Esthet Restor Dent 27:322–330. https://doi.org/10.1111/jerd.12155
De Oliveira DCRS, Rocha MG, Gatti A, Correr AB, Ferracane JL, Sinhoret MAC (2015) Effect of different photoinitiators and reducing agents on cure efficiency and color stability of resin-based composites using different LED wavelengths. J Dent 43:1565–1572. https://doi.org/10.1016/j.jdent.2015.08.015
Favarão J, Oliveira D, Zanini MM, Rocha MG, Correr-Sobrinho L, Sinhoreti M (2021) Effect of curing-light attenuation on color stability and physical and chemical properties of resin cements containing different photoinitiators. J Mech Behav Biomed Mater 113:104110. https://doi.org/10.1016/j.jmbbm.2020.104110
Schneider LF, Moraes RR, Cavalcante LM, Sinhoreti MA, Correr-Sobrinho L, Consani S (2008) Cross-link density evaluation through softening tests: effect of ethanol concentration. Dent Mater 24:199–203. https://doi.org/10.1016/j.dental.2007.03.010
Silame FDJ, Geraldeli GP, Sinhoreti MAC, Pires-de-Souza FCP, Roulet JF, Geraldeli S (2017) Dentin µTBS and hardness of bulk-fill and conventional composites placed in a box-shaped cavity preparation. J Adhes Dent 19:395–400. https://doi.org/10.3290/j.jad.a39276
Yu B, Liu F, He J (2014) Preparation of low shrinkage methacrylate-based resin system without Bisphenol A structure by using a synthesized dendritic macromer (G-IEMA). J Mech Behav Biomed Mater 35:1–8. https://doi.org/10.1016/j.jmbbm.2014.03.012
Yin M, Liu F, He J (2016) Preparation and characterization of Bis-GMA free dental resin system with synthesized dimethacrylate monomer TDDMMA derived from tricyclo[5.2.1.0(2,6)]-decanedimethanol. J Mech Behav Biomed Mater 57:157–163. https://doi.org/10.1016/j.jmbbm.2015.11.020
Yap AU, Eweis AH, Yahya NA (2018) Dynamic and static flexural appraisal of resin-based composites: comparison of the ISO and mini-flexural tests. Oper Dent 43:E223–E231. https://doi.org/10.2341/17-224-L
Nayif MM, Nakajima M, Foxton RM, Tagami J (2008) Bond strength and ultimate tensile strength of resin composite filled into dentine cavity; effect of bulk and incremental filling technique. J Dent 36:228–234. https://doi.org/10.1016/j.jdent.2007.12.006
Feitosa VP, Fugolin AP, Correr AB, Correr-Sobrinho L, Consani S, Watson TF, Sinhoreti MA, Sauro S (2012) Effects of different photo-polymerization protocols on resin-dentine μTBS, mechanical properties and cross-link density of a nano-filled resin composite. J Dent 40:802–809. https://doi.org/10.1016/j.jdent.2012.05.014
Delgado AJ, Castellanos EM, Sinhoreti M, Oliveira DC, Abdulhameed N, Geraldeli S, Sulaiman TA, Roulet JF (2019) The use of different photoinitiator systems in photopolymerizing resin cements through ceramic veneers. Oper Dent 44:396–404. https://doi.org/10.2341/17-263-L
Borges BC, Souza-Júnior EJ, Catelan A, Paulillo LA, Aguiar FH (2012) Can extended photoactivation time of resin-based fissure sealer materials improve ultimate tensile strength and decrease water sorption/solubility? Eur J Dent 6:402–407
Yin M, Guo S, Liu F, He J (2015) Synthesis of fluorinated dimethacrylate monomer and its application in preparing Bis-GMA free dental resin. J Mech Behav Biomed Mater 51:337–344. https://doi.org/10.1016/j.jmbbm.2015.07.025
Van Landuyt KL, Nawrot T, Geebelen B, De Munck J, Snauwaert J, Yoshihara K, Scheers H, Godderis L, Hoet P, Van Meerbeek B (2011) How much do resin-based dental materials release? A meta-analytical approach. Dent Mater 27:723–747. https://doi.org/10.1016/j.dental.2011.05.001
Herrera-Gonzalez AN, Caldera-Villalobos M, Perez-Mondragon AA, Cuevas-Suarez CE, Gonzalez-Lopez JA (2019) Analysis of double bond conversion of photopolymerizable monomers by FTIR-ATR spectroscopy. J Chem Educ 96:1786–1789. https://doi.org/10.1021/acs.jchemed.8b00659
Podgórski M (2010) Synthesis and characterization of novel dimethacrylates of different chain lengths as possible dental resins. Dent Mater 26:188–194. https://doi.org/10.1016/j.dental.2010.02.011
Cornelio RB, Wikant A, Mjøsund H, Molvig H, Haasum J, Gedde UW, Ortengren UT (2014) The influence of bis-EMA vs bis GMA on the degree of conversion and water susceptibility of experimental composite materials. Acta Odontol Scand 72:440–447. https://doi.org/10.3109/00016357.2013.856467
Duff J, Barclift T, Newman S, Stansbury J, Lewis S, Abuelenain D (2012) Novel resins for dental composite and sealants. J Dent Res 91 (Spec Iss A): abstract #837
Guarda MB, Di Nizo PT, Abuna GF, Catelan A, Sinhoreti MAC, Vitti RP (2020) Effect of electric current-assisted application of adhesives on their bond strength and quality. J Adhes Dent 22:393–398. https://doi.org/10.3290/j.jad.a44870
Sano H, Chowdhury AFMA, Saikaew P, Matsumoto M, Hoshika S, Yamauti M (2020) The microtensile bond strength test: its historical background and application to bond testing. Jpn Dent Sci Rev 56:24–31. https://doi.org/10.1016/j.jdsr.2019.10.001
Ersen KA, Gürbüz Ö, Özcan M (2020) Evaluation of polymerization shrinkage of bulk-fill resin composites using microcomputed tomography. Clin Oral Invest 24:1687–1693. https://doi.org/10.1007/s00784-019-03025-5
Ye S, Azarnoush S, Smith IR, Cramer NB, Stansbury JW, Bowman CN (2012) Using hyperbranched oligomer functionalized glass fillers to reduce shrinkage stress. Dent Mater 28:1004–1011. https://doi.org/10.1016/j.dental.2012.05.003
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
This manuscript does not contain any studies with human participants or animals performed by any of the authors. All procedures performed involving human wastes were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Approval was obtained from the ethics committee of Piracicaba Dental School, University of Campinas, Brazil (#55806016.6.5418). The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Oliveira, R.F., Abuna, G.F., Roulet, JF. et al. Effect of an elastomeric urethane monomer on BisGMA-free resin composites containing different co-initiators. Clin Oral Invest 26, 957–967 (2022). https://doi.org/10.1007/s00784-021-04078-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04078-1