Abstract
Objective
To evaluate the effect of a fluoride toothpaste containing nano-sized sodium hexametaphosphate (HMPnano) on enamel demineralization on the biochemical composition and insoluble extracellular polysaccharide (EPS) in biofilm formed in situ.
Methods
This crossover double-blind study consisted of four phases (7 days each), in which 12 volunteers wore intraoral appliances containing four enamel bovine blocks. The cariogenic challenge was performed using 30% sucrose solution (6×/day). Blocks were treated 3×/day with the following toothpastes: no F/HMP/HMPnano (Placebo), conventional fluoride toothpaste, 1100 ppm F (1100F), 1100F + 0.5% micrometric HMP (1100F/HMP), and 1100F + 0.5% nano-sized HMP (1100F/HMPnano). The percentage of surface hardness loss (%SH), integrated loss of subsurface hardness (ΔKHN), and enamel calcium (Ca), phosphorus (P), and fluoride (F) were determined. Moreover, biofilms formed on the blocks were analyzed for F, Ca, P, and insoluble extracellular polysaccharide (EPS) concentrations. Data were analyzed using one-way ANOVA, followed by Student–Newman–Keuls’ test (p < 0.001).
Results
1100F/HMPnano promoted the lowest %SH and ΔKHN among all groups (p < 0.001). The addition of HMPnano to 1100F significantly increased Ca concentrations (p < 0.001). The 1100F/HMPnano promoted lower values of EPS when compared with 1100F (~ 70%) (p < 0.001) and higher values of fluoride and calcium in the biofilms (p < 0.001).
Conclusion
1100F/HMPnano demonstrated a greater protective effect against enamel demineralization and on the composition of biofilm in situ when compared to 1100F toothpaste.
Clinical relevance
This toothpaste could be a viable alternative to patients at high risk of caries.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the last few decades, a decline in dental caries prevalence was observed, mainly assigned to the use of fluoride toothpaste [1]. Since dental caries has been shown to be polarized in some groups, several studies have been conducted to evaluate new formulations of conventional toothpastes (CT, i.e., 1100 ppm F) with enhanced potential in reducing caries lesions, including the association of F with phosphates [2,3,4].
Sodium hexametaphosphate (HMP) interferes with the enamel de-remineralization process due to its ability to modify the solubility of dental enamel [3, 5]. da Camara et al. [3, 5] evaluated the effect of a CT-containing HMP on enamel demineralization and biofilm. In these studies, the authors observed that the association between 1.0% HMP and 1100 ppm F promoted the lowest surface hardness loss (%SH) and integrated loss of subsurface hardness (ΔKHN). Additionally, it has antimicrobial activity due to its ability to increase the permeability of the bacterial outer membrane [6] and inhibitory activity on biofilm formation [7, 8]. Nano-sized phosphates (nano) have also emerged as an innovative method with the goal of optimizing the effect of fluoride toothpaste on the demineralization and remineralization processes. Nanostructured nanomaterials, nanoparticles in particular, have unique physicochemical properties, such as ultra-small and controllable size, large surface area in relation to mass, high reactivity, and a functionalizable structure [9, 10]. Dalpasquale et al. [4] evaluated in vitro the effect of CT plus nano-sized HMP (HMPnano) at concentrations of 0.25%, 0.5%, and 1.0% in reducing enamel demineralization. The addition of 0.5% HMPnano to a CT significantly enhances its effects against enamel demineralization.
So far, no study has evaluated whether the addition of HMPnano could affect the biofilm composition and enamel demineralization under cariogenic challenge, simulating a condition of high caries risk. Thus, this study evaluated the effect of a F toothpaste containing HMPnano on enamel demineralization in situ and on the composition of biofilm. The null hypothesis was that F toothpaste associated with HMPnano would provide similar anticaries effect when compared to F toothpaste.
Material and methods
Experimental design
This study was approved by the Human Ethical Committee of São Paulo State University (UNESP), School of Dentistry, Araçatuba, Brazil (Protocol: 58549716.8.0000.5420), and all participants read and signed informed consent statements prior to study onset. This in situ, crossover, double-blind study was conducted in four phases of 7 days each [5]. The sample size of 12 volunteers was based on a previous study [11], considering as primary outcome the surface and cross-sectional hardness analysis, mean difference between groups (30 and 1300, respectively), standard deviation (20 and 900, respectively), an α-error of 5%, and a β-error of 20%. Volunteers (n = 12) aged 20–30 years, who were in good general and oral health [12], were included in the study. The subjects wore an acrylic palatal appliance with sound bovine enamel blocks (4 mm × 4 mm, n = 192), previously polished and selected according to the initial surface hardness (SHi) (baseline). The specimens were allocated to treatments: no F/HMP/HMPnano (Placebo), conventional fluoride toothpaste, 1100 ppm F (1100F), 1100F + 0.5% micrometric HMP (1100F/HMP), and 1100F + 0.5% nano-sized HMP (1100F/HMPnano). After each phase, the biofilm was collected for analysis of F, Ca, P, and insoluble extracellular polysaccharides (EPS). In the enamel blocks, the percentage of surface hardness loss (%SH) and integrated loss of subsurface area (ΔKHN) were assessed again. F, Ca, and P contents in enamel were determined.
Processing and characterization of nano-sized HMP
The processing and characterization of nano-sized HMP were based on the study by Dalpasquale et al. [4]. Initially, 70 g of pure HMP (Na6P6O18H6, CAS 68915-31-1, average size of 31 ± 33 μm, purity ≥ 95%, Aldrich Chemistry, CAS 68915-31-1, UK) was ball milled using 500 g of zirconia spheres (diameter of 2 mm) in 1 l of hexane. After 48 h, the material was filtered and sealed with aluminum foil, and the vials were dried at 75 °C to evaporate the hexane. X-ray diffraction (XRD) was used to identify the crystalline structure and estimate the crystallographic coherency domain of HMP, thereafter milled for 48 h (HMPnano). The X-ray diffractograms were obtained from samples in powder form, using Shimadzu XRD 6000 equipment with a CuK radiation source (λ = 1.54056 Å), voltage of 30 kV, and current of 30 mA. Measurements were made continuously in the range of 10° ≤ 2θ ≤ 80° with a 2° sweep speed/min. The structural identification of the samples was carried out by comparing the diffraction patterns obtained with tabulated patterns available in the databases, BJoint Committee on Powder Diffraction Standards—Powder Difraction File (JCPDS—PDF). The particle morphology of HMP and HMP milled for 48 h (HMPnano) was analyzed by scanning electron microscopy (SEM). The SEM images were collected using a Philips XL-30 FEG.
Toothpaste formulation and fluoride and pH assessment
Toothpastes were produced with the following components: 0.5 g of titanium dioxide,1.7 g of carboxymethyl cellulose, 0.08 g of methyl p-hydroxybenzoate sodium, 0.1 g of saccharin, 0.5 g of mint oil, 26.6 g of glycerin, 10.0 g of abrasive silica, 1.7 g of sodium lauryl sulfate, 0.5 g of micrometric HMP, and 0.5 g of nano-sized HMP, adjusted with deionized water to 100 g. NaF (Merck, Darmstadt, Germany) was added to the F toothpaste to reach a concentration of 1100 ppm F. A toothpaste without F (Placebo) was also prepared.
The amounts of total fluoride (TF) and ionic fluoride (IF) were determined [13] using a F− specific electrode (Orion 9609-BN; Orion Research Inc., Beverly, MA, USA) connected to an ion analyzer (Orion 720 A+; Orion Research Inc.). The pH levels of toothpaste slurries were determined using a pH electrode (2A09E, Analyzer, São Paulo, Brazil) calibrated with standard pH levels of 7.0 and 4.0.
Palatal appliance preparation and treatments
The palatal appliance was prepared in acrylic resin (Jet, Articles Classic Odontológico, São Paulo, Brazil), and four enamel blocks were fixed, using a different device in each phase of the experiment. To allow biofilm accumulation on the enamel blocks, a piece of plastic mesh was fixed to the acrylic appliance, leaving a 1-mm space from the block surface [5]. This crossover double-blinded study was performed in four phases of 7 days each. During each experimental fase, volunteers wore palatal appliances containing four enamel blocks and were randomly assigned to one of the four possible treatments. To provide a cariogenic challenge, the volunteers were instructed to remove the device and drip 30% sucrose solution (Sucrose, Synth, Diadema, Brazil) onto each enamel block 6×/day at predetermined times (8:00 am, 11:00 am, 2:00 pm, 5:00 pm, 7:00 pm, and 9:00 pm) [5]. The appliances were used 24 h/day (including at night, except when drinking or eating), and the volunteers brushed their natural teeth 3×/day (08:00 am, 13:00 pm, 21:30 pm) for 2 min, with the palatal appliance in the oral cavity, allowing the natural saliva/toothpaste slurry to come into contact with the enamel blocks by gently squishing the slurry in the mouth. During a 7-day pre-experimental period and washout periods, the volunteers brushed their teeth with the Placebo toothpaste.
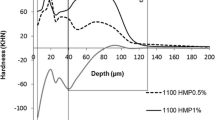
Hardness analysis
The SH was determined before (SHi) and after each experimental phase (SHf), using a Shimadzu HMV-2000 microhardness tester (Shimadzu Corp., Kyoto, Japan) under a 25-g load for 10 s [5], followed by calculation of the percentage of surface hardness loss: (%SH = [(SHf-SHi)/SHi] × 100). For the cross-sectional hardness measurements, the enamel blocks were longitudinally sectioned through their center and embedded in acrylic resin with the cut face exposed and gradually polished. A sequence of 14 indents was created 100 μm apart at different distances (5, 10, 15, 20, 25, 30, 40, 50, 70, 90, 110, 130, 220, and 330 μm) from the outer enamel surface using a Micromet 5114 hardness tester (Buehler, Lake Bluff, USA) and the software Buehler OmniMet (Buehler, Lake Bluff, USA) with a Knoop diamond indenter under a 5-g load for 10 s [4, 14]. Integrated hardness (KHN × μm) for the lesion into sound enamel was calculated by the trapezoidal rule (GraphPad Prism, version 3.02) and subtracted from the integrated hardness for sound enamel to obtain the integrated area of subsurface regions in enamel, which was named integrated loss of subsurface hardness (ΔKHN; KHN × μm) [15].
Fluoride, calcium, and phosphorus in enamel
F present in the enamel was determined as described by Weatherell et al. [16] and modified by Alves et al. [17]. Self-adhesive polishing discs (13-mm diameter) and 400-grit silicon carbide (Buehler) were fixed to the bottom of polystyrene crystal tubes (J-10; Injeplast, Sao Paulo, Brazil) and attached to a handpiece (N 270; Dabi Atlante, Ribeirão Preto, Sao Paulo, Brazil) fixed to the top of a modified microscope with a micrometer (Pantec, Sao Paulo, Brazil). One layer of enamel (50.9 ± 0.2 μm) was removed from each block, after addition of 0.5 mL HCl 1.0 mol L−1, and these were kept under constant stirring for 1 h [16, 17].
For F analysis, specific electrode 9409BN (Thermo Scientific, Beverly, Mass., USA) and microelectrode reference (Analyser, Sao Paulo, Brazil) coupled to an ion analyzer (Orion 720A+, Thermo Scientific, Beverly, MA, USA) were used. Ca analysis was performed using the Arsenazo III colorimetric method [18]. The absorbance readings were recorded at 650 nm, using a plate reader (PowerWave 340, Biotek, Winooski, VT, USA). P was measured according to Fiske and Subbarow [19], and the absorbance readings were recorded at 660 nm. The results of Ca and P were expressed in micrograms per cubic millimeter.
Analysis of dental biofilm composition
The biofilm formed on enamel was collected and stored in microcentrifuge tubes. The biofilm samples were dried in vacuum over P pentoxide for 12 h at room temperature. F was analyzed using an ion specific electrode (Orion 9409 BN) and a potentiometer (Orion 720 Aplus). The Ca concentration was analyzed by a colorimetric test [19]. The P concentration was measured using a colorimetric method [18]. EPS was extracted by adding 1.0 mol L−1 NaOH (10 μL/mg dry weight) to the biofilm [20, 21]. The amount of EPS was determined using the phenol-sulfuric acid method [22]. The results were expressed as moles per kilogram (F, Ca, and P) and milligrams per gram (EPS) dry weight.
The ionic activities (IA) of the various species (Ca2+, CaPO4−, CaHPO40, CaH2PO4+, PO43−, HPO4−2, H2PO4−, CaF+, HF0, and F−) and the degree of saturation (DS) of the solid phases of hydroxyapatite (HA) and calcium fluoride (CaF2) were calculated from the concentrations (mol/kg) of F, Ca, and P on the biofilm of each toothpaste. All calculations were performed at 37 °C, 7.0 pH, and a density of 1.0 g/cm3 using the PHREEQC Interactive (version 2.18.3) speciation program [5, 11].
Statistical analysis
SigmaPlot 12.0 software (version 12.0, Systat Software Inc., San Jose, CA, USA) was used for statistical analysis, and the significance level was set at 5%. The statistical power calculated was 85%, considering all differences between groups for each outcome. Data from the dental biofilm analysis (Ca, P, F and EPS content, and ionic activities) and enamel analysis (%SH, ΔKHN and F, Ca, and P content) exhibited normal (Shapiro–Wilk) and homogeneous (Bartlet) distribution and were therefore subjected to one-way ANOVA, repeated measures (i.e., due to the fact that all treatments (toothpastes) were tested by the same group of volunteers), followed by the Student–Newman–Keuls’ testing.
Results
The X-ray diffraction (XRD) pattern of 48 h HMPnano after milling shows broader peaks owing to the smaller crystallites (Fig. 1). Figure 2a depicts the SEM images of HMP with large aggregates and particles of smaller sizes (average size of 31 ± 33 μm). Figure 2b portrays the SEM images of HMPnano particles with low size distribution and an average size of 91 ± 34 nm.
X-ray diffraction patterns of HMP before (HMP) and after (HMPnano) grinding of powder for 48 h in ball mill. The possible phases sodium hexametaphosphate (NaPO3)6, sodium metaphosphate NaPO3, disodium dihydrogen diphosphate (Na2H2P2O7), sodium dihydrogen phosphate monohydrate (NaH2PO4 (H2O)), sodium dihydrogen phosphate (NaH2PO4), and pentasodium triphosphate (Na5P3O10)
Mean (SD) concentrations of total F (TF) and ionic fluoride (IF) (n = 3) were as follows: Placebo—10.5 (0.1) and 10.0 (1.2); 1100F—1186.0 (33.2) and 1102.4 (28.5); 1100F/HMP—1168.3 (5.9) and 1136.5 (42.6); and 1100F/HMPnano—1156.6 (19.7) and 1100.9 (27.1). The mean pH value of the groups was 7.2 (0.3) ranging from 6.8 to 7.7.
The use of 1100F/HMPnano resulted in a 49% decrease in %SH in comparison with 1100F (Table 1). The addition of micrometric HMP to F toothpaste decreased the %SH in 36% when compared with the Placebo group (p < 0.001), and was similar to 1100F (p = 0.695). In addition, the capacity to reduce the lesion body (ΔKHN) was ~ 10% and ~ 55% higher with 1100F/HMP and 1100F/HMPnano, respectively (p < 0.001) when compared to 1100F (Table 1).
The addition of HMP and HMPnano to the CT did not influence enamel F concentration, so that its effect was similar to 1100F, except for the Placebo, which showed a lower concentration (p < 0.001). With 1100F/HMPnano, the enamel Ca concentration was increased by ~ 12% and ~ 78% when compared to 1100F/HMP and 1100F toothpastes (p < 0.001). No significant difference was observed between groups regarding enamel P concentrations except for the Placebo, which showed a lower concentration (p < 0.001).
As for the biofilm composition, 1100F/HMPnano promoted the highest retention of Ca (p < 0.001) and F (p < 0.001), when compared with 1100F (Table 1), while the P values were similar for the treatments (p = 0.084). 1100F/HMPnano showed lower values for alkali-soluble EPS concentration, when compared with 1100F (~ 65%) and 1100F/HMP (~ 60%) (p < 0.001). Similar concentrations were observed for the 1100F and 1100F/HMP groups (p = 0.709), which were significantly lower than that of the Placebo group (p < 0.001).
The ionic activity of CaF+ and HF0 for the 1100F/HMPnano group was significantly higher when compared to the other groups (p < 0.001), while no significant differences were seen between 1100F/HMPnano and the other groups regarding ionic activity of Ca2+, CaPO4−, PO43−, HPO42−, and H2PO4− (p > 0.800). As for phase saturation, the 1100F/HMPnano group showed the highest supersaturation with respect to HA and CaF2 (p < 0.001).
Discussion
Studies have shown an additional effect of nano-sized phosphates in preventing enamel demineralization and promoting remineralization when added to fluoridated formulations [2, 4, 23]. Our study showed that the addition of HMPnano to conventional fluoridated toothpastes at a concentration of 0.5% was able to reduce enamel demineralization by 49% when compared to the 1100F group. Thus, the null hypothesis was rejected. Considering micrometric HMP, da Camara et al. [3, 5] observed that the addition of 1.0%HMP to a CT significantly reduces enamel demineralization when compared to 1100F. Unlike the previous findings, our results show that it is possible to reduce the particle concentration obtaining an additional result when compared to 1100F; however, if this is in its nano-sized form, its effect will be better and more effective.
The supplementation of 1100F with 0.5% HMPnano resulted in a ~ 50% reduction in mineral loss (%SH and ΔKHN) when compared to 1100F. Our findings were far superior when compared to those obtained by da Camara et al. [5], in which the reduction was ~ 25% with micro-sized 1.0% HMP when compared to 1100F. This synergistic effect is in line with previous in vitro findings with a CT supplemented with 0.5% HMPnano [4] and can be attributed to a higher ability of adsorption of HMPnano on enamel, even with the presence of biofilm on the enamel surface, preventing enamel mineral loss. It is noteworthy that HMP does not improve F enamel uptake [3,4,5] as verified in the present study (Table 1). However, Ca concentration in enamel is higher using 1.0% HMP [5] or 0.5% HMPnano (Table 1). Notwithstanding, 1.0% HMP [5] and 0.5% HMPnano (Table 2) produce higher supersaturation with respect to CaF2 and HA compared to 1100F. Thus, enamel Ca concentrations are increased; it is probably due to formation of HMP-Ca2+ layer on enamel, reducing enamel demineralization while favoring high incorporation of Ca2+ in enamel and acid diffusion into enamel and leading to the reduction of EPS [5, 24].
These findings are supported by the significantly higher Ca concentrations in enamel seen for the 1100F/HMPnano group (78%) when compared to 1100F, which seems to be related to a more resistant enamel. Conversely, HMPnano did not seem to have any effect on enamel F and phosphate concentrations, which is also in line with a previous in vitro study assessing the effects of HMPnano when added to a 1100-ppm F toothpaste [4]. Thus, it can be assumed that the mechanism of action of HMPnano containing F toothpastes is somehow different from that described for toothpastes containing F as the only active anticaries ingredient. Furthermore, the procedure used to synthesize HMPnano promoted more reactive particles with increased adsorption on enamel, due to the reduction in size and increase in surface area (in proportion to its volume), which leads to a higher number of atoms, as demonstrated by Dalpasquale et al. [4].
The use of 1100F/HMPnano promoted significant changes in the biochemical composition of biofilm, providing more insights into the mechanisms of action of this association. It is noteworthy that the increase in F concentrations in the biofilm is often correlated with Ca concentration [25,26,27], as observed for the 1100F group when compared to the Placebo group (Table 1). The addition of micro-sized 0.5% HMP to 1100F toothpaste presented similar outcomes, showing no additional effect on the biofilm. Nevertheless, micro-sized 0.5%HMP presented smaller depth of lesion (ΔKHN) and higher Ca concentration in enamel when compared to 1100F (Table 1). The lower cariogenic challenge observed in the present study can also have contributed to lower mineral loss of the 1100F toothpaste when compared to in vitro study [3]. This effect is due to the HMP capacity of enamel adsorption and reduction of acid diffusion into enamel [3]. Considering the effect in the biochemical composition of biofilm, micro-sized 0.5% HMP did not interfere with Ca retention, unlike the findings for micro-sized 1.0% HMP in a previous study [5]. However, the 0.5% HMP in its nano-sized form led to higher F and Ca ion retention as a consequence of its more reactive and smaller particles. Hence, ionic activity of CaF+ and HF0 for the 1100F/HMPnano was significantly higher when compared to the other groups; and might act on the inner part of the subsurface lesion [28]. In addition, only the 1100F/HMPnano toothpaste was supersaturated in relation to CaF2, when compared to 1100F and 1100F/HMP groups. In the 1100F/HMPnano group, the biofilm served as a reservoir of F and Ca ions during the high cariogenic challenge (30% sucrose solution), maintaining greater amount of Ca in the enamel (Table 1), which could contribute to minimize the enamel mineral loss (%SH and ΔKHN). Nonetheless, the mechanisms proposed above need to be carefully considered, given that data from ionic activity were calculated based on the total ion concentration from the whole biofilm, which comprises not only the free ions in the biofilm fluid but also ionizable and firmly bound pools. Such calculations, however, are useful for an overall comparison between groups, providing insights on the reasons why HMP nano promoted a significantly higher protective effect on enamel.
Regarding alkali-soluble EPS concentration, our results showed an expressive reduction (64%) for the HMPnano toothpaste when compared with 1100F, which was not observed for micro-sized 1.0% HMP added to 1100F toothpaste [5]. That study hypothesized that 1.0% HMP reduces the calcium concentration in the biofilm. It is noteworthy that more fluoride in the biofilm is related with higher Ca concentration [25,26,27], as observed for 1100F and 1100F plus micrometric 0.5% HMP when compared to the Placebo (Table 1). In addition, the reduction of EPS is related to Ca concentration between 1 × 10−3 and 1 × 10−4 mol/L [29]. A lower percentage of HMP did not interfere with calcium in the biofilm as verified in the previous study [5], and 1100F and 1100F/HMP showed similar ability to reduce the EPS in the biofilm (Table 1). Thus, the higher F and Ca concentrations produced by 1100F/HMPnano in the biofilm may have been responsible for the reduction of bacterial metabolism and EPS production [30,31,32,33]. Notwithstanding, the HMP presents capacity to alter the permeability and glucose transport, since it forms a strong complex with Mg2+ in the outer bacterial membrane, leading to an antimicrobial effect [6], and thus the results of our study showed that this effect can be increased when HMP is used in its nano-sized form. The HMP in its nano-sized form can lead to reduction of EPS since its particles are more reactive. However, these data are not supported by the literature because a report showed antimicrobial action over cariogenic bacterial in concentrations over 6.0% [5]. These data are based on an in situ demineralization protocol, and we suggest that other similar studies should be conducted with biofilm accumulation and different cariogenic challenges (frequency × exposure to sucrose) to simulate patients with different caries activities. Studies analyzing the inorganic composition of saliva and plaque fluid, in situ remineralization protocol, and in vivo studies would be of great importance to confirm our findings.
We conclude that 1100F/HMPnano promoted a greater protective effect against enamel demineralization and significantly affected the composition of biofilm formed in situ when compared to 1100F toothpaste. Thus, this toothpaste could be an alternative for patients at high caries risk and activity.
References
Bratthal D, Hansel-Petersson G, Sundberg H (1996) Reasons for the caries decline: what do the experts believe? Eur J Oral Sci 104:416–422
Danelon M, Pessan JP, Neto FN, de Camargo ER, Delbem AC (2015) Effect of toothpaste with nano-sized trimetaphosphate on dental caries: in situ study. J Dent 43:806–813. https://doi.org/10.1016/j.jdent.2015.04.010
da Camara DM, Pessan JP, Francati TM, Souza JA, Danelon M, Delbem AC (2016) Fluoride toothpaste supplemented with sodium hexametaphosphate reduces enamel demineralization in vitro. Clin Oral Investig 20:1981–1985. https://doi.org/10.1007/s00784-015-1707-x
Dalpasquale G, Delbem ACB, Pessan JP, Nunes GP, Gorup LF, Souza-Neto FN, Camargo ER, Danelon M (2017) Effect of the addition of nano-sized sodium hexametaphosphate to fluoride toothpastes on tooth demineralization: an in vitro study. Clin Oral Investig 21:1821–1827. https://doi.org/10.1007/s00784-017-2093-3
da Camara DM, Pessan JP, Francati TM, Santos Souza JA, Danelon M, Delbem AC (2015) Synergistic effect of fluoride and sodium hexametaphosphate in toothpaste on enamel demineralization in situ. J Dent 43:1249–1254. https://doi.org/10.1016/j.jdent.2015.08.007
Vaara M, Jaakkola J (1989) Sodium hexametaphosphate sensitizes Pseudomonas aeruginosa, several other species of Pseudomonas, and E. coli to hydrophobic drugs. Antimicrob Agents Chemother 3:1741–1747
Shibata H, Morioka T (1982) Antibacterial action of condensed phosphates on the bacterium Streptococcus mutans and experimental caries in the hamster. Arch Oral Biol 27:809–816. https://doi.org/10.1016/0003-9969(82)90034-6
Samiei M, Farjami A, Dizaj SM, Lotfipour F (2016) Nanoparticles for antimicrobial purposes in Endodontics: a systematic review of in vitro studies. Mater Sci Eng C 58:1269–1278. https://doi.org/10.1016/j.msec.2015.08.070
Zhang L, Pornpattananangku D, Hu CM, Huang CM (2010) Development of nanoparticles for antimicrobial drug delivery. Curr Med Chem 17:585–594. https://doi.org/10.2174/092986710790416290
He L, Deng D, Zhou X, Cheng L, ten Cate JM, Li J, Li X, Crielaard W (2015) Novel tea polyphenol-modified calcium phosphate nanoparticle and its remineralization potential. J Biomed Mater Res B Appl Biomater 8:1525–1531. https://doi.org/10.1002/jbm.b.33333
do Amaral JG, Martinhon CC, Delbem ACB (2013) Effect of low-fluoride toothpastes supplemented with calcium glycerophosphate on enamel demineralization in situ. Am J Dent 26:75–80
Delbem AC, Carvalho LP, Morihisa RK, Cury JÁ (2005) Effect of rinsing with water immediately after APF gel application on enamel demineralization in situ. Caries Res 39:258–260. https://doi.org/10.1159/000084808
Delbem AC, Sassaki KT, Vieira AE, Rodrigues E, Bergamaschi M, Stock SR, Cannon ML, Xiao X, De Carlo F, Delbem ACB (2009) Comparison of methods for evaluating mineral loss: hardness versus synchrotron microcomputed tomography. Caries Res 43:359–365. https://doi.org/10.1159/000231573
Danelon M, Takeshita EM, Sassaki KT, Delbem ACB (2013) In situ evaluation of a low fluoride concentration gel with sodium trimetaphosphate in enamel remineralization. Am J Dent 26:15–20
Spiguel MH, Tovo MF, Kramer PF, Franco KS, Alves KM, Delbem AC (2009) Evaluation of laser fluorescence in the monitoring of the initial stage of the de-/remineralization process: an in vitro and in situ study. Caries Res 43:302–307. https://doi.org/10.1159/000218094
Weatherell JA, Robinson C, Strong M, Nakagaki H (1985) Micro-sampling by abrasion. Caries Res 19:97–102. https://doi.org/10.1159/000260835
Alves KM, Pessan JP, Brighenti FL, Franco KS, Oliveira FA, Buzalaf MA, Sassaki KT, Delbem AC (2007) In vitro evaluation of the effectiveness of acidic fluoride dentifrices. Caries Res 41:263–267. https://doi.org/10.1159/000101915
Vogel GL, Chow LC, Brow WL (1983) A microanalytical procedure for the determination of calcium, phosphate and fluoride in enamel biopsy samples. Caries Res 17:23–31
Fiske CH, Subbarow Y (1925) The colorimetric determination of phosphorus. J Biol Chem 66:375–400
Nobre dos Santos M, Melo dos Santos L, Francisco SB, Cury JÁ (2002) Relationship among dental plaque composition, daily sugar exposure and caries in the primary dentition. Caries Res 36:347–352. https://doi.org/10.1159/000065959
Ccahuana-Vasquez RA, Tabchoury CPM, Tenuta LMA, Del Bel Cury AA, Vale GC, Cury JA (2007) Effect of frequency of sucrose exposure on dental biofilm composition and enamel demineralization in the presence of fluoride. Caries Res 41:9–15. https://doi.org/10.1159/000096100
Dubois M, Grilles KA, Hamilton JK, Rebers PA, Smith F (1956) Colorimetric method for determination of sugars and related substances. Anal Chem 28:350–356. https://doi.org/10.1021/ac60111a017
Danelon M, Pessan JP, Souza-Neto FN, de Camargo ER, Delbem AC (2017) Effect of fluoride toothpaste with nano-sized trimetaphosphate on enamel demineralization: an in vitro study. Arch Oral Biol 78:82–87. https://doi.org/10.1016/j.archoralbio.2017.02.014
van Dijk JW, Borggreven JM, Driessens FC (1980) The effect of some phosphates and a phosphonate on the electrochemical properties of bovine enamel. Arch Oral Biol 25:591–595. https://doi.org/10.1016/0003-9969(80)90072-2
Whitford GM, Wasdin JL, Schafer TE, Adair SM (2002) Plaque fluoride concentrations are dependent on plaque calcium concentrations. Caries Res 36:256–265. https://doi.org/10.1159/000063931
Pessan JP, Sicca CM, de Souza TS, da Silva SMB, Whitford GM, Buzalaf MAR (2006) Fluoride concentrations in dental plaque and saliva after the use of a fluoride toothpaste preceded by a calcium lactate rinse. Eur J Oral Sci 114:489–493. https://doi.org/10.1111/j.1600-0722.2006.00409.x
Pessan JP, Silva SMB, Lauris JRP, Sampaio FC, Whitford GM, Buzalaf MAR (2008) Fluoride uptake by plaque from water and from toothpaste. J Dent Res 87:461–465. https://doi.org/10.1177/154405910808700501
Cochrane HJ, Saranathan S, Cai F, Cross KJ, Reynolds EC (2008) Enamel subsurface lesion remineralisation with casein phosphopeptide stabilized solutions of calcium phosphate and fluoride. Caries Res 42:88–97. https://doi.org/10.1159/000113161
Boyd RF (1978) The effect of some divalent cations on extracellular polysaccharide synthesis in Streptococcus salivarius. J Dent Res 57:380–383
Van Loveren B (2001) Antimicrobial activity of fluoride and its in vivo importance: identification of research questions. Caries Res 35:65–70. https://doi.org/10.1159/000049114
Marquis RE, Clock SA, Mota-Meira M (2003) Fluoride and organic weak acids as modulators of microbial physiology. FEMS Microbiol Rev 26:493–510. https://doi.org/10.1111/j.1574-6976.2003.tb00627.x
Choi IK, Wen WW, Smith RW (1993) Technical note the effect of a long chain phosphate on the adsorption of collectors on kaolinite. Miner Eng 6:1191–1197
van Wazer JR, Campanella DA (1950) Structure and properties of the condensed phosphates. IV. Complex ion formation in polyphosphate solutions. J Am Chem Soc 72:655–663. https://doi.org/10.1021/ja01158a004
Acknowledgments
We thank the volunteers for their participation in the study, CAPES (Coordination of Higher Education Personnel), FAPESP (The State of São Paulo Research Foundation, grant 2016/03148-7), and CNPq/PQ (National Council for Scientific and Technological Development, grant 308981/2014-6) for the concession of a scholarship to the first, second, fourth, and eighth authors, respectively.
Funding
This study was supported by CAPES (Coordination of Higher Education Personnel), FAPESP (The State of São Paulo Research Foundation, grant 2016/03148-7), and CNPq/PQ (National Council for Scientific and Technological Development, grant 308981/2014-6).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors Marcelle Danelon, Alberto Carlos Botazzo Delbem, Juliano Pelim Pessan, and Emerson Rodrigues de Camargo hold a patent request for a product used in the study, by the National Institute of Industrial Property—INPI/SP, on October 17, 2014 under number BR 10 2014 025902 3.
Ethical approval
This study was approved by the Human Ethical Committee of São Paulo State University (UNESP), School of Dentistry, Araçatuba, Brazil (Protocol: 58549716.8.0000.5420).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Garcia, L.S.G., Delbem, A.C.B., Pessan, J.P. et al. Anticaries effect of toothpaste with nano-sized sodium hexametaphosphate. Clin Oral Invest 23, 3535–3542 (2019). https://doi.org/10.1007/s00784-018-2773-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2773-7