Abstract
This study examined the histological changes and possible effects of intermittent parathyroid hormone (PTH) (1-34) treatment during the early and late phase of periodontal repair in a rat model of tooth root resorption. In a total of 70 animals, which either received intermittent PTH(1-34) systemically or sham injections for up to 70 days after discontinuation of an orthodontic force, histological characteristics were correlated to time-dependent distinct expression patterns of osteoprotegerin and receptor activator of nuclear factor kappaB ligand by PDL cells in the former compression and tension side of tooth movement by means of immunohistochemistry and histomorphometrical analysis. The balance of these key regulators of bone remodeling was demonstrated to be shifted in favor of hard tissue repair by intermittent PTH administration, which was demonstrated to exert anabolic effects in several cell culture and animal experiments as well as in humans, in the late phase of repair. These data indicate a role for PDL cells as potent regulators of periodontal repair by modifying the local microenvironment and point to the anabolic potential of an intermittent PTH administration to support these reparative processes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pathological root resorption is a common finding in the course of periodontitis, after trauma or reimplantation of teeth, and it occurs as a negative side effect of orthodontic tooth movement [6, 27, 47].
Although many studies on root resorption have attempted to investigate the etiological factors and predictability of this phenomenon, its origin remains to be elucidated. Individual susceptibility, hereditary predisposition, systemic, local, and anatomical factors associated with orthodontic mechanotherapy are frequently cited components. Furthermore, bone density, chronological age, history of trauma, and humoral or immunological factors play crucial roles in the development of root resorption [27].
The destructive process of root resorption is typically followed by reparative activity of the PDL tissues. PDL cells have been implicated to be regulatorily involved in reparative cementum formation based on several phenotypic characteristics they share with osteoblasts [10] and based on their osteoblast-like response to hormonal stimulation [36, 38]. Among those hormones, intermittent parathyroid (PTH) hormone administration has gained particular attention since it was demonstrated to elicit potentially anabolic cellular responses in several osteoblast cell culture experiments and animal model systems [19, 52]. This knowledge has already been transferred to the clinic and proved beneficial to post-menopausal women suffering from osteoporosis who displayed an increased bone mass following intermittent subcutaneous PTH administration [18]. Regarding PDL cells, several in vitro studies point to the analogy to osteoblasts with respect to the cellular response to PTH. In PDL cells, intermittent PTH is capable of inducing maturation-state dependent changes in proliferation, apoptosis, differentiation, and the production of key regulatory molecules of hard tissue remodeling such as osteoprotegerin (OPG) and receptor activator of nuclear factor kappaB ligand (RANKL) [30–33]. Besides PTH, mechanical stress was shown to alter the expression of several osteoblast- and osteoclast-related chemokines, including OPG and RANKL both in vitro and in vivo and, thereby, to contribute to the establishment of a distinct microenvironment in compression and tension sides of orthodontic tooth movement [16, 26, 35].
The possibility to influence the survival and the phenotypic expression of PDL cells provided a basis for a better understanding of the mechanisms underlying periodontal remodeling. In addition, PDL cells were identified as interesting target cells and PTH as a potentially value agent in the attempt to influence those remodeling processes.
It was the aim of the present investigation to transfer the assumptions obtained from in vitro experiments to an in vivo model and examine those findings for their physiological relevance in the regulation of periodontal repair processes in a rat model of intermittent PTH administration following tooth root resorption induced by orthodontic tooth movement [24]. We sought to describe the histological changes during the early and late phase of periodontal repair and tried to correlate those to the expression patterns of OPG and RANKL. Furthermore, we wanted to address the question of whether PTH would be able to influence the reparative processes. We hypothesized that an intermittent PTH administration would result in a reduction of the OPG/RANKL ratio expressed by PDL cells in the early phase of repair, whereas an increase during the late phase of repair was expected. Furthermore, it was speculated that distinct differences in the distribution patterns of OPG and RANKL in former compression sides of tooth movement and former tension sides would be distinguishable.
Materials and methods
Animals
All experimental procedures involving animals were approved by the Institutional Animal Care and Use Committee of the local district government and the Animal Care Commissioner of the University of Bonn (Germany). Seventy 3-month-old male Wistar rats with an average weight of 300 g, obtained from Charles River Laboratories (Sulzfeld, Germany) were used. Animals were kept in plastic cages with a standard 12-h light–dark cycle and fed on a soft diet and water ad libitum. During the experiments, the weights of the animals were recorded every day.
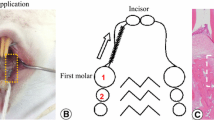
Experimental protocol
Animals were subdivided into seven experimental groups of ten rats each. Tooth movement was realized by separation of the first and second maxillary molars in both quadrants according to the method described by Waldo and Rothblatt [51], resulting in and a mesial movement of the first molar. This treatment regimen was carried out for 5 days prior to the discontinuation of the force. After 5 days, the appliance was removed (day 0). Afterward, half of the animals of each experimental group received intermittent subcutaneous injections of 5 µg/kg body weight PTH [41] every second day for 8, 10, 14, 17, 21, 56, and 70 days. The other half of the animals of each group received sham injections of an equivalent dose of buffer. The observation period up to day 17 after the discontinuation of the force images the early phase of repair, whereas the interval from day 21 to 70 represents the late phase of repair.
After killing, rats were perfused with phosphate-buffered saline supplemented with 4% paraformaldehyde for fixation purposes. Afterward, the maxilla of each animal was dissected, divided in two halves, and prepared for light microscopical examination as recently described [17, 23].
Histology
Specimens were decalcified in neutral 10% ethylene diamine tetra-acetic acid and processed for paraffin histology. For orientation purposes, serial sagittal sections were prepared. Selected sections were stained with hematoxylin and eosin. In order to identify osteoclasts, odontoclasts, and their precursors, selected tissue sections were stained to demonstrate tartrate-resistant acid phosphatase (TRAP) according to Barka and Anderson [2].
Immunohistochemistry
Tissue sections were placed in a tris-hydroxy methyl aminomethane buffered saline solution (TBS) at pH 7.4 for 10 min. Thereafter, endogenous peroxidase activity was blocked in methanol/H2O2 for 10 min in the dark. Subsequently, sections were rinsed and then preincubated with TBS containing 4% bovine serum albumin (TBS/BSA) for 20 min to avoid unspecific background staining. Thereafter, sections were incubated with a polyclonal primary antibody of goat origin raised against a peptide mapping at the carboxy terminus of the protein (anti-OPG (C-20): sc-7625 or anti-RANKL (C-20): sc-7627, respectively; Santa Cruz Biotechnology, USA) in a 1:200 working solution (OPG) or 1:25 working solution (RANKL) of TBS/BSA at 4°C overnight in a humidified chamber. The slides were rinsed again and incubated for 30 min with a rabbit anti-goat immunoglobulin diluted 1:100 in TBS/BSA (Dako A/S, Denmark) as secondary antibody. Incubation was stopped in TBS before the PAP-complex (1:150 in TBS/BSA; Dako A/S Denmark) was administered for 30 min. After another rinse, the tissue sections were stained in a 3,3′-diaminobenzidine (Sigma Chemicals, USA) solution for about 5 min, rinsed, and then counterstained with Mayer's hematoxylin, dehydrated, and cover-slipped for light microscopical analysis.
In order to prove the specificity of the immunoreactions, negative controls were carried out by (a) omitting the primary antibody or using non-immune IgG instead and (b) omitting both the primary and secondary antibody and using TBS/BSA instead.
In addition, pre-adsorption controls were run for both OPG and RANKL in order to exclude unspecific binding of the antibodies to unrelated antigens. For neutralization, the antibody was combined with a two-fold excess of blocking peptide and incubated at 4°C overnight. Following neutralization, the antibody/peptide mixture was diluted into the appropriate working solution. Afterward, immunohistochemistry was carried out as described above.
Positive controls were carried out with sections of selected tissues carrying significant amounts of the OPG and RANKL antigen (human tonsils with adherent skeletal muscle, fetal bone), which were treated in the same way as the periodontal sections.
Histomorphometrical analysis
Two light microscopical images of defined size (750 µm × 375 µm) were captured per specimen at the bifurcation of the maxillary first molars (magnification ×40) in former compression and tension sides. Each image was subdivided into three areas resembling tooth third, PDL third, and bone third to gather information on where immunopositive cells originate from. The number of immunoreactive cells in each third was counted and expressed as a function of total cell number. Extracellular immunoreactivity was not analyzed due to difficulties with quantification of such staining results. All counts were performed by the same investigator. To avoid bias, the investigator was blinded with respect to the origin of the specimens under analysis.
Statistical analysis
Reproducibility of the histomorphometrical readouts was ensured by analyzing 30 selected specimens in triplicate. The intraobserver error was demonstrated to be less than 4%.
For any given experiment, each data point represents the mean ± SEM. Each value is the mean ± SEM of five animals per group and three specimens per animal resulting in a total of 15 values per group. Variance and statistical significance of data were analyzed using Bonferroni's modification of Student's t test. P values <0.05 were considered to be significant.
Results
Morphology
Following the discontinuation of the orthodontic force (day 0), resorption sites could be observed at the mesial surfaces of the alveolar bone. Hyaline zones indicated tissue degradation caused by sterile necrosis accompanied by the appearance of monocytic cells and other inflammatory cells as well as attachment loss and tooth root resorption predominantly in areas of acellular root cementum (Fig. 1a). There were still multiple TRAP-positive resorptive cells within resorption lacunae, on the root surface or adjacent to the hyalinized zones (Fig. 1b). Within the lacunae, not only odontoclasts but also fibroblasts and inflammatory cells were observed. In addition, scattered cementoblast-like cells showing a smaller, round-cuboidal appearance were found within the lacunae (Fig. 1d). Interindividual variations regarding the size of resorption lacunae and the time course of the removal of hyalinized tissue were noticed. During the following experimental days, decreasing amounts of resorbing cells and an increase in the number of reparative cells became obvious but signs of deposited reparative cementum were not observed in the early phase of the experiment.
Rat molar tooth root: a day 0, hyaline zone (asterisk), resorption lacuna (arrow), HE staining, magnification ×200; b day 0, odontoclasts in resorption lacuna (arrows), TRAP staining, magnification ×400; c day 8, influx of cells (arrows), HE staining, magnification ×200; d day 10, cementoblast-like reparative cells at the bottom of the resorption lacuna (arrow heads), only few cells stained positively for TRAP (arrows), TRAP staining, magnification ×400; e day 14, reattachment of PDL fibers in lacuna (arrows), HE staining, magnification ×200; f day 14, reparative cells at the bottom of the lacuna with early deposition of reparative cementum (asterisk), HE staining, magnification ×200; g day 17, influx of cells in resorption lacunae (arrows), HE staining, magnification ×400; h day 17, reattachment of PDL fibers in resorption lacuna (arrows), HE staining, magnification ×200; i day 21, thin layer of reparative cementum formation at the bottom of the resorption lacuna, HE staining, magnification ×400; j day 21, absence of TRAP-positive cells in resorption lacuna, magnification ×200; k day 70, advanced deposition of reparative cementum (arrows), HE staining, magnification ×400. PDL periodontal ligament, D dentin, C cementum
In close vicinity to resorption lacunae, groups of PDL cells appeared in parallel assembly between lacunar areas of the tooth root and the neighboring alveolar bone and perivascular areas. This assembly led to the impression of an influx of cells toward the resorption lacunae (Fig. 1c). In these areas, a focal reattachment of PDL fiber bundles with PDL cells oriented strictly parallel to the fiber direction occurred (Fig. 1e). The phenomenon of cell influx directed from the alveolar bone and perivascular areas toward resorption lacunae to be repaired and fiber reattachment was even more pronounced in the late phase of repair (Fig. 1g, h).
Signs of deposited acellular reparative cementum were seen for the first time on day 14 (Fig. 1f) and resulted in a smoothening of the lacunae after 21 days (Fig. 1i). At this stage of the experiment, there were no more TRAP-positive odontoclasts on the root surface (Fig. 1j). At the end of the observation period after 70 days, advanced reparative cementum deposition was observed (Fig. 1k). Occasionally, a complete repair of the defects was detected.
Histomorphometry
Regarding the immuolocalization of OPG and RANKL, data obtained from each third did not differ significantly from each other and were, therefore, summarized.
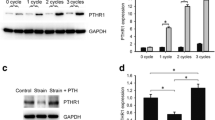
In the former compression side, OPG protein expression decreased after the discontinuation of the orthodontic force. Intermittent PTH administration failed to alter OPG expression in the early phase of periodontal repair but enhanced it significantly in the late phase from day 21 on (Fig. 2a). RANKL protein expression increased significantly with time and was further pronounced by PTH in the early phase of repair, whereas the same treatment regimen reduced RANKL expression in the late phase (Fig. 2b). The OPG/RANKL ratio displayed a time-dependent decrease after discontinuation of the force but was significantly enhanced by PTH in the late phase of repair (Fig. 2c).
Time course of OPG (a) and RANKL (b) protein expression in the former compression side after the discontinuation of orthodontic force and effect of PTH on this development. The resulting OPG/RANKL ratio is depicted in c. Each value is the mean ± SEM for five animals per group and three specimens per animal resulting in a total of 15 values per group. *P < 0.05, particular group vs. control (day 0); # P < 0.05, PTH-treated group vs. sham-injected group after the same observation period
In the former tension side, OPG expression slightly decreased in the early phase but increased in the late phase of repair. PTH administration resulted in a further enhancement of OPG expression in the late phase of repair but had no effect in the early phase (Fig. 3a). RANKL expression slightly decreased with time. This observation was further pronounced by PTH administration in the early phase after the discontinuation of the force. During the late phase, PTH did not modify RANKL expression (Fig. 3b). After an initial decrease of the OPG/RANKL ratio on days 8 and 10, it gradually increased, peaking on day 21. PTH further shifted the ratio in favor of OPG, especially during the late phase of repair (Fig. 3c).
Time course of OPG (a) and RANKL (b) protein expression in the former tension side after the discontinuation of orthodontic force and effect of PTH on this development. The resulting OPG/RANKL ratio is depicted in c. Each value is the mean ± SEM for five animals per group and three specimens per animal resulting in a total of 15 values per group. *P < 0.05, particular group vs. control (day 0); # P < 0.05, PTH-treated group vs. sham-injected group after the same observation period
Serving as an example, selected immunostainings for OPG and RANKL at different time points and areas are depicted in Fig. 4.
Rat molar tooth root: a former compression (CS) and tension sides (TS) of orthodontic tooth movement, HE, magnification ×100; b negative control experiment using non-immune IgG instead of the primary antibody, magnification ×200; c OPG immunohistochemistry at day 14 after the discontinuation of the force, DAB, magnification ×400; d immunostaining for RANKL in the former compression side at day 14, DAB, magnification ×200; e day 10, immunoreactivity for OPG in the former tension side, DAB, magnification ×200; f day 10, detection of RANKL in the former tension side, DAB, magnification ×200; g OPG (inlay: PTH-treated specimen); and h RANKL immunohistochemistry in the late phase of repair (day 70) in the former compression side, DAB, magnification ×200; i day 21, staining for OPG in the former tension side, DAB, magnification ×200 (inlay: PTH-treated specimen); j day 21, positive immunoreactivity for RANKL in the former tension side, DAB, magnification ×200. PDL periodontal ligament, D dentin, AB alveolar bone
In the pre-adsorption control experiments, neither OPG- nor RANKL-immunoreactivity was observed (data not shown). Neither OPG- nor RANKL-immunostaining was observed in the negative control experiments (data not shown). In the positive control experiments with fetal bone, tonsils, and adherent skeletal muscle, specimens demonstrated immunoreactions as expected (data not shown).
Discussion
The present study examined the histological changes during the early and late phase of periodontal repair in a rat model of tooth root resorption. In addition, these histological characteristics were correlated to time-dependent distinct expression patterns of OPG and RANKL. The balance of these key regulators of bone remodeling was demonstrated to be shifted in favor of hard tissue repair by intermittent PTH(1-34) administration.
Prior to the discussion of the results, a technical consideration should be addressed. The discontinuation of the orthodontic force after 5 days might actually result in a reversal of the force, which means that cells that were exposed to a compressive force initially then would be subjected to a slight tensile force and vice versa. However, since hyalinized zones have developed after 5 days of continuous force application in the compression zones resulting in a necrosis and, consequently, in an absence of cells that might respond to such a reversed force, this consideration might only be of importance for the former tension zone. Here, the reversal of the initial direction of the force might indeed interfere with the early reparative processes. Nevertheless, this interference might only be of importance for the first couple of days after discontinuation of the force but not for long-term remodeling and reparative events, which were the primary focus of interest in this study.
After the release of the orthodontic force, there was a continuous decrease in the number of odontoclasts. Only very few resorbing cells were observed in the resorption lacunae on day 14, and no TRAP-positive cells were located in the lacunae on day 21. The continuing resorption processes might serve the removal of necrotic tissue and the round over of remaining edges [7, 8]. After completion of active resorption, odontoclasts became detached from the surface and showed signs of deterioration as described by Sahara and coworkers previously [40]. Noxon et al. demonstrated that osteoclasts recruited for orthodontic tooth movement are, at least in part, cleared by apoptosis [37].
In the light of the sustained resorptive activity in the early phase of repair, the time-dependent reduction of the OPG/RANKL ratio in the former compression side resulting from an increase of RANKL expression as opposed to a comparatively constant OPG expression seems comprehensible and adds further support to the interpretation of ongoing resorption cycles that might serve the clearance of hyaline tissue and the round over of remaining edges. These findings are in line with data obtained from in vitro studies reporting on increased RANKL and constant OPG expression under compressive force [25]. In this early phase, intermittent PTH(1-34) led to a decrease of the OPG/RANKL ratio. These data are corroborated by Buxton et al. [9] and support the hypothesis that PTH (1-34) initially stimulates osteoblast maturation and function, which in turn leads to osteoclast activation and a gradual rebalancing of bone formation and resorption. By contrast, in the former tension side, OPG expression increased during the early phase of repair until day 17, whereas immunoreactivity for RANKL was reduced, resulting in an enhanced OPG/RANKL ratio. Recent studies suggested a differential expression of tissue remodeling mediators in tension and compression sides of the PDL during tooth movement [13, 48], and in particular, a force-dependent up-regulation of OPG mRNA expression in response to tensile force was demonstrated in vitro [49]. Analogous to the observation in the former compression side, PTH(1-34) did not modify the OPG/RANKL ratio significantly in the former tension side as well. Several studies, including animal and cell culture experiments, proved anabolic effects of PTH, e.g., on the differentiation and apoptosis of osteoblasts (for review, see [4, 34]), and similar cellular responses were reported in PDL cells as well [30, 32]. Possible differences between in vivo and in vitro systems might account for these discrepancies as well as the consideration that it might take longer than a couple of days for PTH to reach pharmacologically relevant levels in the PDL. Basically, a premature elimination of PTH in periodontal tissues might be considered, too, as suggested by Dobnig and Turner [12] although this explanation is unlikely since significant effects of PTH on OPG expression were observed in the late phase of repair. In the study by Sato and coworkers, stronger effects of PTH were observed not until an application period of 3 months [42].
Parallel to these resorptive events, scattered cementoblast-like cells showing a smaller, round-cuboidal appearance were found within the lacunae as early as from day 10 onward. These cells increased in number in the course of further repair processes. These findings suggest a simultaneous presence of clastic and reparative cells in the early phase of repair. It was demonstrated that resorption lacunae may present signs of active resorption and regeneration at the same time [43]. These histological findings indicate a floating transition from root resorption to early cementum repair (“resorption-repair sequence”), which can be compared to the coupling sequence described as characteristic for bone remodeling events [43].
Decompression of the periodontal ligament allowed for the start of repair mechanisms of the cementum. In close vicinity to resorption lacunae, groups of PDL cells in parallel assembly between lacunar areas of the tooth root and the neighboring alveolar bone and perivascular areas were observed. This assembly led to the impression of an influx of cells toward the resorption lacunae and might indicate an immigration of PDL cells or progenitor cells, which might then differentiate into cementoblasts at the bottom of the lacunae. Recently, it was speculated that stem cell niches for PDL cells might exist in perivascular areas of the PDL or in PDL-neighboring endosteal areas of the alveolar bone (for review, see [5, 14, 21]). The cell populations categorized as reparative cells were demonstrated to be S100 positive [24], indicating progenitor cells with a basically fibroblastic phenotype [28, 39]. Since these cells were also shown to be immunoreactive for markers typical of bone cells such as alkaline phosphatase, runx2, and osteocalcin, a more osteoblastic phenotype is suggested [24]. Such an osteoblastic phenotype was reported as characteristic for reparative cells in several models of periodontal regeneration [20]. Since those marker proteins were found to be expressed to a lower extent or to be even absent by actively repairing cementoblasts at the bottom of resorption lacunae [24], a change in the direction of differentiation of inflowing repair cells during migration may be postulated. These changes might be attributed to factors located in the extracellular matrix of the PDL or to biomechanical factors.
As an additional finding, repair processes in the rat model employed in this study did not seem to be associated with significantly increased mitogenic activity in the resorption lacunae as evidenced by immunohistochemical staining for the proliferation marker PCNA. The PCNA antibody demonstrated immunoreactions primarily in PDL cells of the former tension sides, whereas only a few PDL cells on the former compression sides and some epithelial remnants on Mallasez as well as perivascular cells in the PDL stained positively for PCNA (data not shown). These observations are in line with a similarly low proliferative activity in the PDL reported by Usuda et al. in a rat model of cementum repair induced by tooth movement [50]. Together with our histological findings of an influx of cells from a certain distance into the resorption lacunae, these considerations further support the conclusion drawn above that cells that proliferate in response to PTH in the PDL undergo further differentiation during migration to the resorption lacunae.
Thin seams of acellular repair cementum were observed at the beginning of the late phase of repair after 21 days, which is in line with other reports on periodontal repair in rat models [43, 44]. This late phase was characterized by an absence of TRAP-positive cells along with a continuous but insignificant decrease of the OPG/RANKL ratio in the former compression side. In the former tension side, the ratio remained significantly elevated until day 70. Contrasting the lack of an effect in the early phase of repair, intermittent PTH(1-34) caused a significant increase of the OPG/RANKL ratio in the late phase with a more pronounced effect seen in the former compression side where repair of resorption lacunae took place. Likewise, PTH effects on bone mass in women suffering from osteoporosis and on fracture healing were reported after long-term administration periods of 3 and 6 months, respectively, in studies on mice, non-human primates, and humans [1, 3, 19, 42, 46]. Furthermore, pulsatile PTH(1-34) administration proved beneficial to the osseointegration of dental implants [45]. The changes of the OPG/RANKL ratio resulted from a stronger modification of OPG production than of RANKL production in our study. The increase of OPG might support anabolic repair processes by an inhibition of osteoclasts and odontoclasts [15, 29] and, thereby, shift the balance between tissue resorbing and tissue forming events in favor of hard tissue formation. The potential role of PDL cells in the regulation of tooth root resorption and repair via PTH(1-34)-induced changes in PDL cell proliferation, and survival and in their differentiation toward cementoblasts or osteoblasts that was implicated in previous experiments [30–32] is further supported by the present data. It is obvious that changes in the local microenvironment regarding OPG and RANKL production by PDL cells would not only influence cells capable of repairing the tooth root but at the same time affect cells in close vicinity to the alveolar bone as well. Likewise with the tooth roots, resorption lacunae developed at the alveolar bone surface in response to the orthodontic force. Consequently, the regulation of alveolar bone remodeling might benefit from the PTH(1-34)-induced changes of the OPG/RANKL ratio as well. An involvement of OPG and RANKL in the regulation of periodontitis-associated alveolar bone loss was already demonstrated [11]. An up-regulation of OPG in repair tissue was recently demonstrated after guided tissue regeneration treatment in humans [22].
Immunohistochemical staining demonstrated PTH receptors to be present predominantly on osteoblastic and PDL cells but not on original cementoblasts and repair cells, respectively [24]. Therefore, it can be speculated that PTH modifies the osteoblastic differentiation of PDL cells but not their secretory activity during cementum and reparative cementum formation. Since the rate of reparative cementum formation is much lower as compared with bone formation, the PTH effect on cementum formation might be difficult to prove within a reasonable time span.
However, the present investigation demonstrated the physiological relevance of the in vitro study evidence for a potential regulatory role of PDL cells in periodontal repair processes following orthodontic tooth movement or inflammatory periodontal disease. Furthermore, our data strengthen the hypothesis that PTH might be a valuable agent to support dental hard tissue remodeling processes in terms of anabolic effects.
References
Anastasilakis AD, Goulis DG, Polyzos SA et al (2008) Acute changes in serum osteoprotegerin and receptor activator for nuclear factor-kappaB ligand levels in women with established osteoporosis treated with teriparatide. Eur J Endocrinol 158:411–415
Barka T, Anderson P (1962) Histochemical methods for acid phosphatase using hexazonium as a coupler. J Histochem Cytochem 10:741–753
Barnes GL, Kakar S, Vora S et al (2008) Stimulation of fracture-healing with systemic intermittent parathyroid hormone treatment. J Bone Joint Surg Am 90(Suppl 1):120–127
Bilezikian JP, Rubin MR, Finkelstein JS (2005) Parathyroid hormone as an anabolic therapy for women and men. J Endocrinol Invest 28:41–49
Bosshardt DD (2005) Are cementoblasts a subpopulation of osteoblasts or a unique phenotype? J Dent Res 84:390–406
Brezniak N, Wasserstein A (2002) Orthodontically induced inflammatory root resorption. Part I: the basic science aspects. Angle Orthod 72:175–179
Brudvik P, Rygh P (1995) Transition and determinants of orthodontic root resorption-repair sequence. Eur J Orthod 17:177–188
Brudvik P, Rygh P (1995) The repair of orthodontic root resorption: an ultrastructural study. Eur J Orthod 17:189–198
Buxton EC, Yao W, Lane NE (2004) Changes in serum receptor activator of nuclear factor-kappaB ligand, osteoprotegerin, and interleukin-6 levels in patients with glucocorticoid-induced osteoporosis treated with human parathyroid hormone (1-34). J Clin Endocrinol Metab 89:3332–3336
Chou AM, Sae-Lim V, Lim T et al (2002) Culturing and characterization of human periodontal ligament fibroblasts-a preliminary study. Mater Sci Eng 20:77–83
Cochran DL (2008) Inflammation and bone loss in periodontal disease. J Periodontol 79:1569–1576
Dobnig H, Turner RT (1997) The effects of programmed administration of human parathyroid hormone fragment (1-34) on bone histomorphometry and serum chemistry in rats. Endocrinology 138:4607–4612
Dudic A, Kiliaridis S, Mombelli A et al (2006) Composition changes in gingival crevicular fluid during orthodontic tooth movement: comparisons between tension and compression sides. Eur J Oral Sci 114:416–422
Foster BL, Popowics TE, Fong HK et al (2007) Advances in defining regulators of cementum development and periodontal regeneration. Curr Top Dev Biol 78:47–126
Fukushima H, Kajiya H, Takada K et al (2003) Expression and role of RANKL in periodontal ligament cells during physiological root-resorption in human deciduous teeth. Eur J Oral Sci 111:346–352
Garlet TP, Coelho U, Repeke CE et al (2008) Differential expression of osteoblast and osteoclast chemmoatractants in compression and tension sides during orthodontic movement. Cytokine 42:330–335
Gotz W, Kunert D, Zhang D et al (2006) Insulin-like growth factor system components in the periodontium during tooth root resorption and early repair processes in the rat. Eur J Oral Sci 114:318–327
Hodsman AB, Bauer DC, Dempster DW et al (2005) Parathyroid hormone and teriparatide for the treatment of osteoporosis: a review of the evidence and suggested guidelines for its use. Endocr Rev 26:688–703
Iida-Klein A, Zhou H, Lu SS et al (2002) Anabolic action of parathyroid hormone is skeletal site specific at the tissue and cellular levels in mice. J Bone Miner Res 17:808–816
Ivanovski S, Li H, Haase HR et al (2001) Expression of bone associated macromolecules by gingival and periodontal ligament fibroblasts. J Periodontal Res 36:131–141
Ivanovski S, Gronthos S, Shi S et al (2006) Stem cells in the periodontal ligament. Oral Dis 12:358–363
Ivanovski S, Lichanska AM, d'Aniello E et al (2007) Gene expression profiling of cells involved in periodontal regeneration. Tissue Eng 13:393–404
Jager A, Zhang D, Kawarizadeh A et al (2005) Soluble cytokine receptor treatment in experimental orthodontic tooth movement in the rat. Eur J Orthod 27:1–11
Jager A, Kunert D, Friesen T et al (2008) Cellular and extracellular factors in early root resorption repair in the rat. Eur J Orthod 30:336–345
Kanzaki H, Chiba M, Shimizu Y et al (2002) Periodontal ligament cells under mechanical stress induce osteoclastogenesis by receptor activator of nuclear factor kappaB ligand up-regulation via prostaglandin E2 synthesis. J Bone Miner Res 17:210–220
Kim T, Handa A, Iida J et al (2007) RANKL expression in rat periodontal ligament subjected to a continuous orthodontic force. Arch Oral Biol 52:244–250
Krishnan V, Davidovitch Z (2006) Cellular, molecular, and tissue-level reactions to orthodontic force. Am J Orthod Dentofacial Orthop 129(469):e461–432
Le Hir M, Hegyi I, Cueni-Loffing D et al (2005) Characterization of renal interstitial fibroblast-specific protein 1/S100A4-positive cells in healthy and inflamed rodent kidneys. Histochem Cell Biol 123:335–346
Lossdorfer S, Gotz W, Jager A (2002) Immunohistochemical localization of receptor activator of nuclear factor kappaB (RANK) and its ligand (RANKL) in human deciduous teeth. Calcif Tissue Int 71:45–52
Lossdorfer S, Gotz W, Jager A (2005) PTH(1-34) affects osteoprotegerin production in human PDL cells in vitro. J Dent Res 84:634–638
Lossdorfer S, Gotz W, Jager A (2006) Parathyroid hormone modifies human periodontal ligament cell proliferation and survival in vitro. J Periodontal Res 41:519–526
Lossdorfer S, Gotz W, Rath-Deschner B et al (2006) Parathyroid hormone(1-34) mediates proliferative and apoptotic signaling in human periodontal ligament cells in vitro via protein kinase C-dependent and protein kinase A-dependent pathways. Cell Tissue Res 325:469–479
Lossdorfer S, Stier S, Gotz W et al (2006) Maturation-state dependent response of human periodontal ligament cells to an intermittent parathyroid hormone exposure in vitro. J Periodontal Res 41:62–72
Masi L, Brandi ML (2005) Molecular, biochemical and cellular biology of PTH anabolic action. J Endocrinol Invest 28:37–40
Nakao K, Goto T, Gunjigake KK et al (2007) Intermittent force induces high RANKL expression in human periodontal ligament cells. J Dent Res 86:623–628
Nohutcu RM, Somerman MJ, McCauley LK (1995) Dexamethasone enhances the effects of parathyroid hormone on human periodontal ligament cells in vitro. Calcif Tissue Int 56:571–577
Noxon SJ, King GJ, Gu G et al (2001) Osteoclast clearance from periodontal tissues during orthodontic tooth movement. Am J Orthod Dentofacial Orthop 120:466–476
Ouyang H, McCauley LK, Berry JE et al (2000) Response of immortalized murine cementoblasts/periodontal ligament cells to parathyroid hormone and parathyroid hormone-related protein in vitro. Arch Oral Biol 45:293–303
Ryan DG, Taliana L, Sun L et al (2003) Involvement of S100A4 in stromal fibroblasts of the regenerating cornea. Invest Ophthalmol Vis Sci 44:4255–4262
Sahara N, Toyoki A, Ashizawa Y et al (1996) Cytodifferentiation of the odontoclast prior to the shedding of human deciduous teeth: an ultrastructural and cytochemical study. Anat Rec 244:33–49
Sato M, Vahle J, Schmidt A et al (2002) Abnormal bone architecture and biomechanical properties with near-lifetime treatment of rats with PTH. Endocrinology 143:3230–3242
Sato M, Westmore M, Ma YL et al (2004) Teriparatide [PTH(1-34)] strengthens the proximal femur of ovariectomized nonhuman primates despite increasing porosity. J Bone Miner Res 19:623–629
Sismanidou C, Lindskog S (1995) Spatial and temporal repair patterns of orthodontically induced surface resorption patches. Eur J Oral Sci 103:292–298
Sismanidou C, Hilliges M, Lindskog S (1996) Healing of the root surface-associated periodontium: an immunohistochemical study of orthodontic root resorption in man. Eur J Orthod 18:435–444
Skripitz R, Aspenberg P (2001) Early effect of parathyroid hormone (1–34) on implant fixation. Clin Orthop Relat Res 392:427–432
Sone T, Fukunaga M, Ono S et al (1995) A small dose of human parathyroid hormone(1-34) increased bone mass in the lumbar vertebrae in patients with senile osteoporosis. Miner Electrolyte Metab 21:232–235
Taithongchai R, Sookkorn K, Killiany D (1996) Facial and dentoalveolar structure and the prediction of apical root shortening. Am J Orthod Dentofacial Orthop 110:296–302
Takahashi I, Onodera K, Nishimura M et al (2006) Expression of genes for gelatinases and tissue inhibitors of metalloproteinases in periodontal tissues during orthodontic tooth movement. J Mol Histol 37:333–342
Tsuji K, Uno K, Zhang GX et al (2004) Periodontal ligament cells under intermittent tensile stress regulate mRNA expression of osteoprotegerin and tissue inhibitor of matrix metalloprotease-1 and -2. J Bone Miner Metab 22:94–103
Usuda J, Hashimoto S, Enokiya Y et al (2004) Proliferative activities of epithelial and connective tissue cells in the rat periodontal regeneration using argyrophilic nucleolar organizer regions staining. J Periodontol Res 39:175–187
Waldo CM, Rothblatt JM (1954) Histologic response to tooth movement in the laboratory rat; procedure and preliminary observations. J Dent Res 33:481–486
Yang ZJ CV, Barnes S, Cavalho L, Sindrey D (1997) Pulsatile parathyroid hormone (PTH) treatment increases bone formation in vitro in fetal rat calvarial cell (FRCC) culture system. J Bone Miner Res 12(Suppl 1):S317
Acknowledgments
The authors thank I. Bay-Müller for technical assistance and C. Maelicke for her help in preparing the manuscript. This research was supported by a research grant from the Deutsche Forschungsgemeinschaft (DFG, KFO 208). The authors declare that they do not have any conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lossdörfer, S., Yildiz, F., Götz, W. et al. Anabolic effect of intermittent PTH(1-34) on the local microenvironment during the late phase of periodontal repair in a rat model of tooth root resorption. Clin Oral Invest 14, 89–98 (2010). https://doi.org/10.1007/s00784-009-0263-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-009-0263-7