Abstract
Menstrual problems and non-suicidal self-injury (NSSI) are common in adolescent girls. This study examined whether onset of menstruation and menstrual problems were related to NSSI in Chinese female adolescents. A total of 5696 adolescent girls participated in the baseline survey of Shandong Adolescent Behavior and Health Cohort (SABHC) study in Shandong, China. A structured questionnaire was used to ask about participants’ lifetime and last-year NSSI, age at menarche, menstrual cycle interval, menstrual flow length, menstrual irregularity, period pain, body weight and height, and demographics. Impulsivity was assessed by the Eysenck I7 impulsiveness scale. Internalizing and externalizing problems were measured by the Youth Self-Report of Child Behavior Checklist. The mean age of the sample was 15.0 years (SD = 1.4). The prevalence of lifetime and last year NSSI were 28.1% and 21.4% in Chinese adolescent girls. After adjusting for adolescent and family covariates (age, body mass index, impulsivity, internalizing and externalizing problems, paternal education, and family economic status), onset of menstruation was significantly associated with increased risk of lifetime NSSI (OR = 1.62, 95%CI = 1.20–2.20) and last year NSSI (OR = 1.92, 95%CI = 1.37–2.67). Among adolescent girls who had menarche, often irregular menstruation and period pain were significantly and independently associated with lifetime NSSI (OR = 1.36, 95%CI = 1.03–1.79; OR = 1.29, 95%CI = 1.05–1.58) and last year NSSI (OR = 1.46, 95%CI = 1.07–1.98; OR = 1.29, 95%CI = 1.03–1.61). Our findings suggest that onset of menarche, irregular periods, and period pain appear to be associated with increased risk of NSSI. These findings highlight the importance of menstruation hygiene education and treatment of menstrual problems to reduce the risk of NSSI among adolescent girls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-suicidal self-injury (NSSI) refers to the deliberate, self-inflicted destruction of body tissue resulting in immediate damage, without suicidal intent and for purposes not culturally sanctioned (Zetterqvist 2015). NSSI in adolescents is a worldwide public health concern for its high prevalence and adverse consequences (Hawton et al. 2012a; Swannell et al. 2014; Zetterqvist 2015). Recent epidemiological studies reported that 17.0–32.7% of adolescents engaged in NSSI during the past year (Wan et al. 2011; Giletta et al. 2012; Shek and Yu 2012; Wan et al. 2015). Although majority of self-injuries is of low medical lethality, NSSI is associated with clinical and functional impairment and is a significant predictor of future suicide attempts and completed suicide (Cooper et al. 2005; Hawton et al. 2012a; Carroll et al. 2015).
The incidence of NSSI begins to increase in the early adolescence, particularly in adolescent girls (Hawton et al. 2012b; Zetterqvist et al. 2013). Most of studies have shown that the prevalence of NSSI is significantly higher in female adolescents than in male adolescents (Wan et al. 2011; Giletta et al. 2012; Zetterqvist et al. 2013). Although the female-to-male ratios vary across studies (Wan et al. 2011; Zetterqvist et al. 2013), it can be as high as 5 or 6 to 1 in adolescents aged 12–15 years (Hawton et al. 2012b). NSSI in adolescents is associated with a wide variety of psychosocial factors, genetic and biological factors, and mental health problems or disorders, and may be caused by the complex interaction of genetic and environmental factors (Wan et al. 2011; Maciejewski et al. 2014; Wan et al. 2015; Zetterqvist 2015; Liu et al. 2017a, b, c). Identifying modifiable risk factors is crucial for developing effective programs to prevent and intervene adolescent NSSI (Brent et al. 2013; Hawton et al. 2015). One of the potential risk factors, which has received little attention, is menstrual problems in adolescent girls.
Menarche is the first menstrual cycle or first menstrual bleeding in adolescent girls, due to the culmination of a series of physiological and anatomic processes of puberty. The menstrual cycle is controlled by the hypothalamic-pituitary-ovarian axis and is influenced by general health, biological, genetic, nutritional, and psychosocial factors (Hickey and Balen 2003; Adams Hillard 2008). The median age of menarche is 12–13 years in most developed countries (ACOG and Committee 2015). Early menarche has been demonstrated to be associated with anxiety/depression, substance use, and suicidal behavior in adolescents (Angold et al. 1998; Copeland et al. 2010; Deng et al. 2011; Chen et al. 2017; Sequeira et al. 2017). However, little is known about the association between age at menarche and NSSI. To our knowledge, only one study reported a significant association between early menarche and NSSI in a sample of Chinese high school and college students. The major limitation of the study is that potential confounding effects of mental health problems, such as depression and externalizing behavioral problems were not adjusted for (Deng et al. 2011).
Menstrual problems such as dysmenorrhea, irregular menstrual cycles, and heavy bleeding are common gynecologic complaints in adolescent girls (Hickey and Balen 2003; Yu et al. 2016). According to a recent literature review, for example, the prevalence of dysmenorrhea or menstrual pain in adolescent girls is between 16% and 93%, with severe pain being 2% to 19% (De Sanctis et al. 2015). In a recent study of adolescent girls, 34% of the sample defined their menstrual cycle as irregular (Esen et al. 2016). Menstrual problems have significant effect on daily activities and quality of life and are associated with mental health problems, sleep disturbance, and school absence (Williams and Creighton 2012; Nur Azurah et al. 2013; Yu et al. 2016; Liu, Chen et al. 2017). Menstrual problems may also increase the risk of NSSI because mental health problems and sleep disturbances are associated with both self-injury/suicidal behavior and menstrual problems (Liu and Buysse 2006; Pigeon et al. 2012; Yu et al. 2016). However, no studies have specifically examined the association between menstrual problems and NSSI.
The current study was conducted to address the data gaps and answer the questions of whether menarche and menstrual problems were associated with NSSI in a large sample of Chinese adolescent girls. Our first aim of the study was to examine if onset of menarche was associated with increased risk of NSSI. The second aim was to examine if age at menarche was associated with NSSI. The third aim was to examine if menstrual problems were associated with increased risk of NSSI.
Methods
Participants and procedure
The Shandong Adolescent Behavior & Health Cohort (SABHC) is an ongoing longitudinal study of adolescent behavior and health in Shandong, China. Detailed sampling and data collection have been described elsewhere (Liu, Chen et al. 2017; Liu et al. 2018). In brief, 12,301 students were sampled from five middle and three high schools in three counties of Shandong Province. Shandong, located in the middle eastern coast of China, is a typical province in terms of population structure and social and cultural life. Shandong has a total population of 95.8 million and about half of its population lives in rural areas. The three counties and eight schools in Shandong were selected for the study, with consideration of the representativeness of adolescent students in the region, prior study collaboration, convenience, and budget.
In November–December 2015, participants were invited to complete a self-administered, structured adolescent health questionnaire (AHQ) to assess pubertal development, menstrual problems, risk behaviors, mental health, and family socioeconomic status. After getting permission from the target schools, trained master’s-level public health workers administered the AHQ to participants in their classrooms during regular school hours. Before filling out the questionnaire, participants were instructed to read the instructions carefully and informed that the survey was anonymous, and their participation was voluntary without any penalties for nonparticipation.
We obtained permission to conduct the study from the principals in the target schools and informed consent from participants in the target classes before the survey. Participants were asked to get permission from their parents to participate in the survey. The study was approved by the research ethics committee of Shandong University School of Public Health and target schools.
Measures
Measures of non-suicidal self-injury. The AHQ has two questions about non-suicidal self-injury (NSSI): “I have tried to hurt myself deliberately without intention to kill myself over the entire lifetime” and “I tried to hurt myself deliberately without intention to kill myself during the past year.” If a respondent answered “yes” on the first question, he or she was considered to have lifetime NSSI. If the answer was “yes” on the second question, the responder was considered to have last-year NSSI.
Menarche and menstrual problems. Six questions were used to collect information about menstruation. Menarche was defined as the first menstrual period and was asked by “Have you begun to menstruate?” If the answer was “yes,” age at menarche was then asked by “How old were you when you had your first period?” Menstrual cycle interval was asked by “How long is your typical cycle interval from day one of a menstrual period to day one of the next period?” Menstrual flow length was asked by “On average, how many days does your period last?” Menstrual regularity was asked by “How regular is your menstrual period?” with a response option of “regular,” “sometimes irregular,” or “very irregular.” Period pain was asked by “Do you have painful periods or menstrual cramps?” with a response option of “none,” “mild,” “moderate,” or “severe.”
Study covariates. Adolescent and family factors selected for this analysis as covariates included adolescent age, body mass index (BMI), internalizing and externalizing problems, impulsivity, paternal education, and family economic status. These covariates were selected based on the associations of these variables with mental health, NSSI, and/or menstruation in previous studies (Angold et al. 1998; Liu et al. 2005; Copeland et al. 2010; Deng et al. 2011; Currie et al. 2012; Sequeira et al. 2017).
Participants were asked to report their body weight, height, paternal education (primary school, middle school, high school, professional school, or college and above), and family economic status (excellent, good, fair, poor, or very poor). BMI was calculated by body weight divided by the square of body height (kg/m2).
Internalizing and externalizing problems were assessed by the Chinese version of 1991 Achenbach Youth Self-Report (YSR) of Child Behavior Checklist (Achenbach 1991; Liu et al. 1997). The YSR comprises 103 problem items to which the respondent can answer “0” if the problem is not true of him or herself, “1” if the item is somewhat or sometimes true, or “2” if it is very true or often true within the past six months. By summing 1 and 2s on all problem items, eight syndromes and two second-order factors (internalizing and externalizing) can be assessed. The externalizing factor is made up of aggressive behavior and delinquent behavior; the internalizing factor is made up of the anxious/depressed, withdrawn and somatic complaints. The Chinese YSR has shown satisfactory psychometric properties in adolescents in China (Liu et al. 1997). Cronbach’s alpha was 0.91 for internalizing problems and 0.89 for externalizing problems with the current sample.
Impulsiveness was assessed by the Eysenck I7 impulsiveness scale (Eysenck et al. 1984). The scale is composed of 19 items with a modified response format from “never or rarely,” “sometimes,” “often,” to “always.” Example items are “Do you often get into trouble because you do things without thinking?” and “Are you an impulsive person?” Cronbach’s alpha was 0.92 with the current sample.
Statistical analysis
Chi-square tests and student t tests were used to compare differences in categorical data and continuous data between adolescents with and without NSSI, respectively. Univariate logistic regression analyses were performed to examine the associations between menarche and menstrual problems and lifetime NSSI and last year NSSI. Multivariate logistic regressions were performed to examine the independent associations of NSSI with menarche and menstrual problems, adjusting for the effects of adolescent and family covariates (age, school, BMI, impulsiveness, internalizing and externalizing problems, and father education, and family economic status). Statistical tests of the regression estimates or odds ratios were based on Wald statistics. All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 22.0 (Armonk, NY: IBM Corp).
Results
Of 12,301 students sampled for SABHC baseline survey, 11,836 who attended school on the day of survey returned questionnaires, 5 students returned their questionnaires in blank, leaving 11,831 for baseline data analysis (96.2%). Among the 11,831 participants, 5813 (49.1%) were adolescent girls. Of these adolescent girls, 5696 (98%) answered the questions about lifetime NSSI and last year NSSI and were included for the current analysis. The mean age was 15.0 years (SD = 1.4, range 12–18).
Prevalence of NSSI
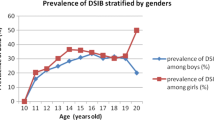
Table 1 shows the prevalence rates of lifetime NSSI and last year NSSI by age. The overall prevalence of lifetime NSSI and last year NSSI were 28.1% and 21.4%, respectively. The prevalence of lifetime NSSI (χ2 = 56.68, p < .0001) and last year NSSI (χ2 = 2172, p < .0001) differed significantly across ages 12–18. The NSSI prevalence tended to increase from ages 12 to 15 and then decrease from ages 16 to 18.
Demographical and psychosocial characteristics associated with NSSI
As shown in Table 2, mean age, body weight, and height were significantly higher in girls who had lifetime NSSI than in those without NSSI (all p < .001). However, no significant differences were found between girls with and without last year NSSI (all p > .05). Girls who reported lifetime and last year NSSI scored significantly higher than those without NSSI on impulsivity and internalizing and externalizing problems (all p < .0001). Poor family economic status was more common in girls with lifetime and last year NSSI than those without NSSI (p < .05). No significant differences in fathers’ education were observed between girls with and without NSSI (p > .05).
Menarche and NSSI
As presented in Tables 3 and 4, the prevalence of lifetime NSSI and last year NSSI were significantly higher in girls who had menarche than in those who had not (p < .0001). Univariate logistic regressions found that the odds of lifetime NSSI and last year NSSI were 1.85 (95%CI = 1.45–2.36, p < .001) and 1.69 (95%CI = 1.29–2.21, p < .001) in girls who had had menarche compared with those without menarche, respectively. After adjusting for adolescent and family covariates, the odds for lifetime NSSI (OR = 1.62, 95%CI = 1.20–2.20, p < .001) was decreased by 12% but the odds for last year NSSI (OR = 1.92, 95%CI = 1.37–2.67, p < .001) was increased by 14% and both odds remained to be significant.
Age at menarche, menstrual problems, and NSSI
Tables 3 and 4 present the prevalence of lifetime NSSI and last year NSSI across ages at menarche and menstrual problems. The prevalence of lifetime NSSI and last year NSSI were significantly higher in girls with irregular periods and period pain than in those without the problem (all p < .0001). The prevalence of last year NSSI were significantly higher in girls who had onset of menarche at age ≤ 11 years (p = .033) and whose menstrual cycle was ≤ 24 days or ≥ 35 days (p = .015).
After adjusting for adolescent and family covariates, often irregular periods and moderate period pain were significantly associated with lifetime NSSI (OR = 1.36, 95%CI = 1.03–1.79, p = .023) and last year NSSI (OR = 1.29, 95%CI = 1.03–1.61, p = .014). The odds of lifetime NSSI and last year NSSI with irregular periods and moderate period pain tended to decrease but remained to be significant (all p < .05), after adjusting for age (Adj1OR) and additional adjustment of body mass index, paternal education, family economic status, impulsivity, and internalizing and externalizing problems (Adj2OR).
Menarche at age ≤ 11 years for last year NSSI became insignificant after adjusting for age (p > .05). Menstrual cycle ≤ 24 days and ≥ 35 days for last year NSSI were no longer significant (p > .05) after adjusting for impulsivity and internalizing and externalizing problems (Adj2OR).
Discussion
To our knowledge, this is the first study to comprehensively examine the associations between menstrual problems and NSSI in a large sample of Chinese adolescent girls. Our major findings are summarized and discussed below.
First, our findings show that the prevalence of NSSI tended to increase from ages 12 to 15 and then decrease from ages 16 to 18 among adolescent girls. Higher prevalence of NSSI during the early adolescence may be explained by the finding that onset of menstruation was significantly associated with increased risk of lifetime NSSI (OR = 1.62) and last year NSSI (OR = 1.92). Although no specific studies have reported the associations between menarche and NSSI, the significant association observed in the current study is not surprising. This is because rapid physical and endocrinological changes and associated psychosocial stress around the onset of menses may make adolescent girls particularly vulnerable to emotion dysregulation and increase the risk of mental health problems and NSSI (Angold et al. 1998; Johnson et al. 2006; Sequeira et al. 2017). For instance, estrogen levels around the time of menarche increase rapidly and fluctuate dramatically in the body (Steiner et al. 2003). The body’s systems like the hypothalamic-pituitary-adrenal (HPA) axis may not be able to promptly adapt to these rapid changes of hormones that has been associated with increased risk of depression in women (Weiss et al. 1999). Furthermore, girls around the onset of menarche may experience more psychosocial distress like worries and concerns about their menstruation and are more vulnerable to stress (Steiner et al. 2003). In addition, menstrual problems and psychosomatic symptoms are more likely to occur in the first few years following menarche and may make adolescent girls at risk of mental health problems and self-injury (Williams and Creighton 2012; Pilver et al. 2013).
Second, early menarche (≤ 11 years) was not significantly associated with NSSI after adjusting for age and other adolescent and family covariates. Our finding is different from a study that reported early menarche was significantly associated with increased risk of NSSI in Chinese high school and college students (Deng et al. 2011). However, our finding is supported by recent longitudinal studies that found the effect of early menarche on depressive symptoms existed in mid-adolescence (14–15 years) and did not persist into late adolescence (16–19 years) (Joinson et al. 2013; Sequeira et al. 2017). That is, early menarche may have temporary effect on NSSI in early adolescence. Further longitudinal studies are needed to examine the long-term effects of early menarche on NSSI from early adolescence through adulthood.
Third, among adolescent girls who had menarche, often irregular menstruation, and period pain were significantly associated with lifetime NSSI and last year NSSI after adjusting for adolescent and family covariates. Many studies have demonstrated that menstrual problems, including period pain and irregular periods, are the leading cause of school absenteeism, can impact quality of life, and increase risk of mental health problems (Nur Azurah et al. 2013; Yu et al. 2016; Chen et al. 2017), all of which, in turn, can increase the risk of NSSI. However, the associations between menstrual problems and NSSI cannot be fully explained by the indirect effect of mental health problems. This is because the association remained to be significant and the degree of the association was only attenuated to a small extent after adjusting for both internalizing and externalizing problems. Further studies are needed to examine the pathways, mediators and moderators, and underlying biological and genetic mechanisms between menstrual problems and NSSI.
Study limitations
This is the first study to examine age at menarche and menstrual problems and NSSI in a sample of more than 5000 adolescent girls. Multiple potential child and family confounders were statistically controlled for, including age, BMI, impulsivity, internalizing and externalizing problems, and family social demographics. However, this study has several limitations that need to be considered when interpreting the findings. First, a single item (i.e., I have tried to hurt myself deliberately without intention to kill myself) used to measure NSSI cannot distinguish direct NSSI behaviors such as cutting and burning skin and indirect self-injuries such as hurting oneself through risky and reckless behaviors. Second, since all measures used in this study were self-report, it is possible that some of the effects may have been due to shared method variance. However, as menarche is a girls’ developmental milestone and menstrual problems may occur every month, they are less likely to be affected by recall bias. The age at menarche and menstrual problems are comparable to other studies of adolescent female populations (Song et al. 2015; Yu et al. 2016). With respect to NSSI, given that many adolescents who engaged in NSSI may never come to medical attention or result in hospitalization, self-report measures remain a valuable source of information (Hawton et al. 2002; Owens et al. 2015). The findings that menstrual problems were associated with both lifetime NSSI and last year NSSI were reassuring. Third, as is true for all cross-sectional research, we could not establish the causal relationships between menstrual problems and NSSI. Prospective studies with clinical interviews are needed to examine their causal associations. Fourth, although many adolescent and family factors were examined as covariates in the study, some other factors, such as early childhood life stress and eating disorders, which may be associated with NSSI and menstrual cycle or menstrual problems, were not included. In addition, although the sample size is large, it is unknown if the findings from participants in eight schools in Shandong could be generalized to adolescents in other regions.
In summary, our study demonstrated that menarche and menstrual problems were associated with increased risk of NSSI in a large sample of adolescent girls. These findings may have important implications for understanding the increased risk of NSSI in early adolescent girls and gender differences in NSSI emerging in early adolescence. Our findings may also have important public health and clinical implications for puberty education and menstrual hygiene management to help adolescent girls respond to and manage the changes and challenges they face in life. Puberty education and menstrual hygiene management should be conducted at school and in routine clinical practice to prevent self-injury associated with the onset of menstruation and menstrual problems in adolescent girls.
References
Achenbach TM (1991) Manual for the youth self-report and 1991 profile. Department of Psychiatry, University of Vermont, Burlington, VT
ACOG and Committe (2015) ACOG committee opinion no. 651: menstruation in girls and adolescents: using the menstrual cycle as a vital sign. Obstet Gynecol 126(6):e143–e146
Adams Hillard PJ (2008) Menstruation in adolescents: what's normal, what’s not. Ann N Y Acad Sci 1135:29–35
Angold A, Costello EJ, Worthman CM (1998) Puberty and depression: the roles of age, pubertal status and pubertal timing. Psychol Med 28(1):51–61
Brent DA, McMakin DL, Kennard BD, Goldstein TR, Mayes TL, Douaihy AB (2013) Protecting adolescents from self-harm: a critical review of intervention studies. J Am Acad Child Adolesc Psychiatry 52(12):1260–1271
Carroll R, Thomas KH, Bramley K, Williams S, Griffin L, Potokar J, Gunnell D (2015) Self-cutting and risk of subsequent suicide. J Affect Disord 192:8–10
Chen H, Wang XT, Bo QG, Zhang DM, Qi ZB, Liu XC, Jia CX (2017) Menarche, menstrual problems and suicidal behavior in Chinese adolescents. J Affect Disord 209:53–58
Cooper J, Kapur N, Webb R, Lawlor M, Guthrie E, Mackway-Jones K, Appleby L (2005) Suicide after deliberate self-harm: a 4-year cohort study. Am J Psychiatry 162(2):297–303
Copeland W, Shanahan L, Miller S, Costello EJ, Angold A, Maughan B (2010) Outcomes of early pubertal timing in young women: a prospective population-based study. Am J Psychiatry 167(10):1218–1225
Currie C, Ahluwalia N, Godeau E, Nic Gabhainn S, Due P, Currie DB (2012) Is obesity at individual and national level associated with lower age at menarche? Evidence from 34 countries in the health behaviour in school-aged children study. J Adolesc Health 50(6):621–626
De Sanctis V, Soliman A, Bernasconi S, Bianchin L, Bona G, Bozzola M, Buzi F, De Sanctis C, Tonini G, Rigon F, Perissinotto E (2015) Primary dysmenorrhea in adolescents: prevalence, impact and recent knowledge. Pediatr Endocrinol Rev 13(2):512–520
Deng F, Tao FB, Wan YH, Hao JH, Su PY, Cao YX (2011) Early menarche and psychopathological symptoms in young Chinese women. J Women’s Health (Larchmt) 20(2):207–213
Esen I, Oguz B, Serin HM (2016) Menstrual characteristics of pubertal girls: a questionnaire-based study in Turkey. J Clin Res Pediatr Endocrinol 8(2):192–196
Eysenck SBG, Easting G, Pearson PR (1984) Age norms for impulsiveness, venturesomeness and empathy in children. Personal Individ Differ 5(3):315–321
Giletta M, Scholte RH, Engels RC, Ciairano S, Prinstein MJ (2012) Adolescent non-suicidal self-injury: a cross-national study of community samples from Italy, the Netherlands and the United States. Psychiatry Res 197(1–2):66–72
Hawton K, Rodham K, Evans E, Weatherall R (2002) Deliberate self harm in adolescents: self report survey in schools in England. Bmj 325(7374):1207–1211
Hawton K, Bergen H, Kapur N, Cooper J, Steeg S, Ness J, Waters K (2012a) Repetition of self-harm and suicide following self-harm in children and adolescents: findings from the multicentre study of self-harm in England. J Child Psychol Psychiatry 53(12):1212–1219
Hawton K, Saunders KE, O’Connor RC (2012b) Self-harm and suicide in adolescents. Lancet 379(9834):2373–2382
Hawton K, Witt KG, Taylor Salisbury TL, Arensman E, Gunnell D, Townsend E, van Heeringen K, Hazell P (2015) Interventions for self-harm in children and adolescents. Cochrane Database Syst Rev 12:CD012013
Hickey M, Balen A (2003) Menstrual disorders in adolescence: investigation and management. Hum Reprod Update 9(5):493–504
Johnson EO, Roth T, Schultz L, Breslau N (2006) Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics 117(2):e247–e256
Joinson C, Heron J, Araya R, Lewis G (2013) Early menarche and depressive symptoms from adolescence to young adulthood in a UK cohort. J Am Acad Child Adolesc Psychiatry 52(6):591–598 e592
Liu X, Buysse DJ (2006) Sleep and youth suicidal behavior: a neglected field. Curr Opin Psychiatry 19(3):288–293
Liu X, Guo CQ, Liu LQ, Sun LM (1997) Reliability and validity of the youth self-report (YSR) of Achenbach’s child behavior checklist (CBCL) [in Chinese]. Chin Ment Health J 11(4):200–203
Liu X, Tein JY, Zhao Z, Sandler IN (2005) Suicidality and correlates among rural adolescents of China. J Adolesc Health 37(6):443–451
Liu X, Chen H, Bo QG, Fan F, Jia CX (2017a) Poor sleep quality and nightmares are associated with non-suicidal self-injury in adolescents. Eur Child Adolesc Psychiatry 26(3):271–279
Liu XC, Chen H, Liu Z, Fan F, Jia CX (2017b) Early menarche and menstrual problems are associated with sleep disturbance in a large sample of Chinese adolescent girls. Sleep
Liu XC, Chen H, Liu ZZ, Jia CX (2017c) Prevalence of suicidal behavior and associated factors in a large sample of Chinese adolescents. Epidemiology and Psychiatric Sceince In Press
Liu X, Chen H, Liu ZZ, Jia CX (2018) Insomnia and psychopathological features associated with restless legs syndrome in Chinese adolescents. J Clin Psychiatry 79(1):16m11358
Maciejewski DF, Creemers HE, Lynskey MT, Madden PA, Heath AC, Statham DJ, Martin NG, Verweij KJ (2014) Overlapping genetic and environmental influences on nonsuicidal self-injury and suicidal ideation: different outcomes, same etiology? JAMA Psychiatry 71(6):699–705
Nur Azurah AG, Sanci L, Moore E, Grover S (2013) The quality of life of adolescents with menstrual problems. J Pediatr Adolesc Gynecol 26(2):102–108
Owens C, Hansford L, Sharkey S, Ford T (2015) Needs and fears of young people presenting at accident and emergency department following an act of self-harm: secondary analysis of qualitative data. Br J Psychiatry
Pigeon WR, Pinquart M, Conner K (2012) Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry 73(9):e1160–e1167
Pilver CE, Libby DJ, Hoff RA (2013) Premenstrual dysphoric disorder as a correlate of suicidal ideation, plans, and attempts among a nationally representative sample. Soc Psychiatry Psychiatr Epidemiol 48(3):437–446
Sequeira ME, Lewis SJ, Bonilla C, Smith GD, Joinson C (2017) Association of timing of menarche with depressive symptoms and depression in adolescence: Mendelian randomisation study. Br J Psychiatry 210(1):39–46
Shek DT, Yu L (2012) Self-harm and suicidal behaviors in Hong Kong adolescents: prevalence and psychosocial correlates. Sci World J 2012:932540
Song Y, Ma J, Agardh A, Lau PW, Hu P, Zhang B (2015) Secular trends in age at menarche among Chinese girls from 24 ethnic minorities, 1985 to 2010. Glob Health Action 8:26929
Steiner M, Dunn E, Born L (2003) Hormones and mood: from menarche to menopause and beyond. J Affect Disord 74(1):67–83
Swannell SV, Martin GE, Page A, Hasking P, St John NJ (2014) Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life Threat Behav 44(3):273–303
Wan YH, Hu CL, Hao JH, Sun Y, Tao FB (2011) Deliberate self-harm behaviors in Chinese adolescents and young adults. Eur Child Adolesc Psychiatry 20(10):517–525
Wan Y, Chen J, Sun Y, Tao F (2015) Impact of childhood abuse on the risk of non-suicidal self-injury in mainland Chinese adolescents. PLoS One 10(6):e0131239
Weiss EL, Longhurst JG, Mazure CM (1999) Childhood sexual abuse as a risk factor for depression in women: psychosocial and neurobiological correlates. Am J Psychiatry 156(6):816–828
Williams CE, Creighton SM (2012) Menstrual disorders in adolescents: review of current practice. Horm Res Paediatr 78(3):135–143
Yu M, Han K, Nam GE (2016) The association between mental health problems and menstrual cycle irregularity among adolescent Korean girls. J Affect Disord 210:43–48
Zetterqvist M (2015) The DSM-5 diagnosis of nonsuicidal self-injury disorder: a review of the empirical literature. Child Adolesc Psychiatry Ment Health 9:31
Zetterqvist M, Lundh LG, Dahlstrom O, Svedin CG (2013) Prevalence and function of non-suicidal self-injury (NSSI) in a community sample of adolescents, using suggested DSM-5 criteria for a potential NSSI disorder. J Abnorm Child Psychol 41(5):759–773
Acknowledgements
The authors would like to thank staffs at the Yanggu County Center for Disease Control and Prevention, Lijin County Center for Disease Control and Prevention, and Zoucheng City Center for Disease Control and Prevention, Shandong Province, China, and all participating school teachers for their help with data collection and all students for their voluntarily participating in the study.
Funding
This work was funded by the National Natural Science Foundation of China (Grant number 81573233) and Shandong University School of Public Health Third Level Discipline Infrastructure Project Fund (Grant number 2017-08).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
We obtained permission to conduct the study from the principals in the target schools and informed consent from participants in the target classes before the survey. Participants were asked to get permission from their parents to participate in the survey. The study was approved by the research ethics committee of Shandong University School of Public Health and target schools.
Rights and permissions
About this article
Cite this article
Liu, X., Liu, ZZ., Fan, F. et al. Menarche and menstrual problems are associated with non-suicidal self-injury in adolescent girls. Arch Womens Ment Health 21, 649–656 (2018). https://doi.org/10.1007/s00737-018-0861-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-018-0861-y