Abstract
Cross-sectional studies indicate that menstrual problems are related to poorer mental health; however, longitudinal studies are limited. This longitudinal study aimed to determine whether baseline menstrual characteristics were risk factors for incident and persistent mental health problems. The study was conducted among Chinese adolescent girls. Menstrual characteristics including menarche, menstrual cycle and menstrual pain were assessed at baseline, whereas mental health problems including PTSD, depression, anxiety, ADHD, insomnia, psychotic-like experiences, non-suicidal self-injury, suicide ideation, suicide plan, and suicide attempt were assessed at baseline (n = 1039) and at the 1-year follow-up (n = 946) by self-administered, structured questionnaires. Multiple logistic regressions were performed to examine whether menstrual characteristics were associated with incident (e.g., PTSD at follow-up but not baseline) and persistent (e.g., PTSD at both time points) mental health problems. The results demonstrated that early menarche was related to persistence of psychotic-like experiences; irregular menstruation was associated with higher rates of incident anxiety and insomnia, and persistent depression, anxiety, ADHD, insomnia, non-suicidal self-injury, suicide ideation, and suicide plan; menstrual pain was associated with elevated rates of incident PTSD and depression, and persistent depression, insomnia, psychotic-like experiences, non-suicidal self-injury, suicidal ideation, suicide plan, and suicide attempt. In conclusion, irregular menstruation and menstrual pain specifically contributed to the development of emotional problems and insomnia, and were associated with maintenance of the most mental health problems in early adolescence. The long-term effects of menstrual problems on mental health need further study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As an integral part of females’ overall health, menstruation can have a significant impact on their physical, mental, and social well-being [1]. For girls, puberty is a unique and critical period, in which they experience their first menstruation in response to ovarian hormones such as estrogen [2]. Menarche, the onset of menstruation, denotes the start of reproductive capacity [3]. Age at menarche can be influenced by complex factors such as genetics, body mass index, nutrition levels, environment and socio-economic conditions [4, 5]. The median age of the first menstruation in most developed countries is 12–13 years [6]. In China, a recent study has demonstrated that the mean age at menarche declined from 12.8 years in 2005 and 12.3 years in 2014 [7]. With the arrival of menstruation, various menstruation-related complaints such as menstrual pain and related menstrual symptoms (diarrhea, nausea, sweating, vomiting, backaches, headaches, fatigue and related somatic complaints) are often observed [8,9,10,11]. A study of Hong Kong, for example, revealed that 68.7% of girls aged between 11.2 and 20.0 years reported dysmenorrhea [9]. In a study of Turkey, the prevalence of menstrual irregularity and dysmenorrhea among females aged between 9 and 17 years were 31.2% and 89.5%, respectively [12]. The menstruation-related complaints mentioned above are often the causes of girls’ school absenteeism and poor concentration. To a large extent, this may lead to impaired quality of life [2, 10, 13, 14].
Adolescents, especially girls, are vulnerable to some mental health problems due to rapid physical and hormonal changes in puberty. Recent research has revealed that early menstruation (years < 11) and menstrual problems may contribute to mental health problems [10, 13]. A prior study has proposed that girls with early menarche are more prone to have emotional distress compared to those with on-time and late menarche [15]. More specifically, two studies based on large UK cohorts with longitudinal designs reported early timing of menarche was related to higher levels of depression in mid-adolescence [16, 17]; another study with genetic risk demonstrated that the early menarche was causally linked to depression [18]. Further, several cross-sectional studies have demonstrated that adolescent girls with irregular menstrual cycles and menstrual pain are at elevated risk for suffering from mental health problems. For instance, evidence from both China and South Korea suggested that menstrual irregularity was correlated with suicide ideation and non-suicidal self-injury [2, 10, 19]. Besides, irregular menstrual cycles may influence girls’ sleep and increase the likelihood of daytime sleepiness and sleep disorders [20, 21], for both sleep and menstruation are related to the hypothalamic-pituitary axis activities [22, 23]. In addition, girls with menstrual pain were more likely to have sleep disorders, PTSD, non-suicidal self-injury, depression and anxiety [2, 21, 24,25,26].
Indeed, there is considerable evidence for the positive correlation between menstruation and mental health problems in adolescents by cross-sectional studies. However, the longitudinal studies are very limited. Only a few longitudinal studies based on the western population have been conducted to investigate the association between early menarche and depression symptoms to date [16, 17]. To our knowledge, no studies have yet employed a longitudinal design to explore whether menstrual characteristics at baseline are predictive of the development of multiple mental health problems. A focus on the longitudinal association of menstruation with mental health conditions may provide crucial information for theory and clinical applications, for understanding the predictors of psychiatric problems could provide clues on how to prevent the onset of mental health disorders and improve the management of adolescents with these disorders.
Based on a large sample of Chinese adolescent girls, the purpose of this study was to investigate the longitudinal association between menstrual characteristics (early menarche, menstrual irregularity, and menstrual pain) and mental health problems (PTSD, depression, anxiety, ADHD, insomnia, psychotic-like experiences, non-suicidal self-injury, and suicide). We specifically examined: (a) whether the menstrual characteristics at baseline were associated with the incidence of mental health problems (e.g., PTSD only at follow-up but not baseline); and (b) whether the menstrual characteristics at baseline were associated with the persistence of mental health problems (e.g., PTSD at both time points). Thus, the aims were to explore whether the menstrual characteristics at baseline were associated with increased risks of developing and maintaining mental health problems during 1-year follow-up.
Methods
Participants
This study is part of a school-based study project on the development course of children and adolescents’ mental health. One of the student’s family members was surveyed at baseline, while a portion of the students would be assessed three times. The present study focused on data from Time 1 (baseline) and Time 2 (1-year follow-up) only. The detailed sampling was described in our previous studies [27, 28]. Briefly, the data were obtained from the girls (mean age 12.49 years, SD = 0.97) of five schools in Hunan and Jiangxi, China. The girls were in 4th, 5th, 6th, 7th, 8th grades at Time 1 and 5th, 6th, 7th, 8th, 9th grades at Time 2. The two provinces are located in the southeast area of the country and are moderately developed in China. The five schools included three primary schools, one middle school, and one school consisting of primary school and middle school. Three of them were located in urban areas and two in rural areas; four were public schools and one was a private school.
In the present study, 3101 girls were enrolled, of whom 1488 girls had experienced menarche. 449 girls were excluded from data analysis because they were about to finish primary school and entered junior high school, making it difficult to follow-up. Therefore, the final sample at time 1 included n = 1039 participants. At time two, 93 girls were lost to follow-up due to transferring to new schools; thus, 946 (91%) participants were followed.
Procedure
With approval and support of the principals and class teachers of the five target schools, participants were invited to complete the self-administered, structured questionnaires to assess their menstrual characteristics and mental health problems at baseline. One year later, 936 participants completed the follow-up assessment of mental health problems. The time interval between the baseline assessment and the follow-up is 1 year. The data collection of both time points was done in the classrooms during regular school hours. Before filling out the questionnaires, the students were required to read the instructions carefully and complete the questionnaires independently. In addition, all the data were collected by trained psychological professionals and teachers. Written informed consent was obtained from all the participants and their parents or caretakers. The study received approval from the Moral & Ethics Committee of the School of Psychology, Jiangxi Normal University (Nanchang, China).
Measures
Menstrual characteristics
One question was used to indicate whether the girls had experienced menarche (yes or no). Girls who responded “yes” were further asked about menstrual characteristics through the following five questions: (1) age at menarche: “How old were you when you had your first menstrual period?”; (2) menstrual cycle: “How regular is your menstrual cycle? 1 for regular, 2 for sometimes irregular, 3 for very irregular”. To display the findings briefly, the data were dichotomized into regular and irregular (1 = regular, 2 and 3 = irregular); (3) menstruation interval: “How many days is it from the first day of your period to the first day of your next period?”; (4) bleeding duration: “How many days do you usually bleed on your period?” (5) menstrual pain: “How about your menstrual pain? 1 for no pain, 2 for mild pain, 3 for moderate pain, 4 for severe pain”. Finally, these variables were converted to dichotomous variables (1 and 2 = no pain, 3 and 4 = pain).
Mental health problems
The Life Events Checklist for DSM-5 (LEC-5) was administered to measure lifetime traumatic events. The LEC-5 is a self-report measure used to assess Criterion A for PTSD. There are 17 categories of traumatic events involving actual or threatened death, serious injury, or sexual violence. Each type of event has six choices: “happened to me”, “witnessed it”, “learned about it happened to a close family member or close friend”, “part of my job”, “not sure” and “does not apply”. The participants would be regarded as exposed to specific trauma if they selected any one of the first four choices. In the current study, Cronbach’s α was 0.795 and 0.805 for baseline and follow-up, respectively.
PTSD symptoms in the past month were assessed with the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) [29]. The PLC-5 includes 20 items rated on a 0–4 (not at all to extremely) Likert scale. A PTSD diagnosis based on the DSM-5 diagnostic criteria requires participants to score two or more on each of the items. Following the DSM-5, participants may be screened for PTSD if at least one re-experiencing symptom, one avoidance symptom, two negative alterations in cognitions and mood, and two hyperarousal symptoms are endorsed. In the current study, Cronbach’s α of the total scale was 0.942 and 0.949 for baseline and follow-up, respectively.
The Patient Health Questionnaire-9 (PHQ-9) was used for the assessment of depression over the past 2 weeks [30]. It contains 9 items, which are rated from 0 = not at all to 3 = nearly every day. The total score can range from 0 to 27. A cutoff score of 10 has been recommended to diagnose depression symptoms. In the current study, Cronbach’s α was 0.882 and 0.888 for baseline and follow-up, respectively.
ADHD symptoms in the past 6 months were assessed by the World Health Organization Adult ADHD Self-Report Scale (ASRS) [31]. The ASRS includes two subscales (inattention and hyperactivity-impulsivity), each of them consisting of 9 items. All items on the measure are rated on a 0–4 Likert scale from 0 = never to 4 = very often. The participants with 17 or higher scores on either subscale are screened as high likelihood of having ADHD [32]. In the current study, Cronbach’s α was 0.909 and 0.928 for baseline and follow-up, respectively.
To screen for anxiety disorders in the past 3 months, the Screen for Child Anxiety Related Emotional Disorders (SCARED), a self-report instrument containing 41 items, was administered [33]. Items are rated on a 3-point scale with 0 for not true or hardly ever true, 1 for sometimes true, and 2 for true or often true. The range of possible total scores varies between 0 and 82. Participants with a total score of 25 or above have higher chance of screening for an anxiety disorder. Cronbach’s α in the current study was 0.938 and 0.945 for baseline and follow-up, respectively.
The Youth Self-Rating Insomnia Scales (YSIS) is a self-administered questionnaire used to measure the severity of insomnia symptoms and impaired daytime functioning within the past month [34]. It contains 8 items, with each item rated on a 5-point scale. A higher total score ranging from 8 to 40 indicates more insomnia problems. A cutoff score of 22 is recommended to screen for insomnia symptoms. Cronbach’s α of the total scale in the current study was 0.851 and 0.866 for baseline and follow-up, respectively.
Psychotic-like experiences in the past month were measured using seven items from the MINI-International Neuropsychiatric Interview for psychotic disorders [35]. Participants responded either “yes” or “no” to each item. The number of psychotic-like experiences was classified into 0–3 and 4–7 (0–3 = symptom absent and 4–7 = symptom present). In the current study, Cronbach’s α was 0.736 and 0.774 for baseline and follow-up, respectively.
To assess the participants’ self-injurious thoughts and suicide behaviors, four questions from previous studies were administered [36]: (1) “Have you ever hurt yourself but not intended to die?”; (2) “ Have you ever had any thoughts about killing yourself?”; (3) “Have you ever made a plan for committing suicide?”; and (4) “Have you ever carried out your plan?”. There were six types of responses to the questions: no, 1, 2, 3, 4, and 5 or more. Finally, these variables were categorized into 0 or 1(0 = no and 1 = one or more times).
Sociodemographic characteristics
Characteristics including location (urban, rural), age, siblings (yes, no), income (low, middle, high), parents’ education (less than high school, high school or above), self-perceived physical health (good, fair, poor) and self-perceived physical exercise (less than once a week, once or twice a week, more than twice a week) were considered as sociodemographics.
Statistical analysis
Descriptive statistics were used to analyze the frequency for categorical variables and means (SD) for continuous variables. According to participants’ status of mental health, we defined our outcome variables as four groups: none (e.g., no PTSD at both time points), recovery (e.g., PTSD at baseline but not follow-up), incident (e.g., PTSD at follow-up but not at baseline) and persistent (e.g., PTSD at both time points). Multiple logistic regression analyses were conducted to explore the longitudinal associations of menstrual characteristics (early menarche, menstrual irregularity, and menstrual pain) and mental health problems (PTSD, depression, anxiety, ADHD, insomnia, psychotic-like experiences, non-suicidal self-injury, and suicide) while adjusting for sociodemographic variables. Since there were no significant associations of mental health problems with menstrual interval and bleeding in our cross-sectional study, the present study did not focus on the duration of menstrual interval and bleeding. Furthermore, in consideration of the length of the paper and the size of the tables, the present study mainly focused on the association of early menarche, menstrual irregularity and pain with mental health problems. The results of menstrual bleeding and intervals are shown in the supplementary material (see Supplementary Material Table 4 and 5). Odds ratios (ORs) and 95% confidence intervals (CIs) were reported.
The percentages of missing data for mental health problems were from 9.0 to 9.5%. Chi-square tests for category variables and t-tests for continuous variables were used to compare the differences in baseline demographics, menstrual characteristics, and mental health problems between students who completed both survey and those who completed only at baseline. The results showed that the two group were not different in demographics, most menstrual characteristics, and mental health problems. However, students who were screened as early menarche (χ2 = 13.31, p < 0.001) were less likely to be flowed up. Missing data were imputed using the expectation–maximization algorithm. Sensitive analyses were also conducted with full data without missing data. The findings of the two methods are similar, and results of imputed data are reported. Data analysis was performed using Statistical Product and Service Solutions version 25.0 (SPSS 25.0). The 0.05-level 2-sided test was used to assess statistical significance.
Results
Sample characteristics
Sociodemographic characteristics and prevalence of early menarche, menstrual irregularity and pain are shown in Table 1.
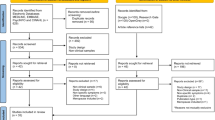
The prevalence rates of the incident and persistent mental health outcomes are presented in Fig. 1. The incidence and the persistence of insomnia, NSSI, and suicide ideation were the highest, whereas the rates of incident and persistent suicide attempt and PTSD were lowest.
Early menarche and mental health problems
Early menarche had no significant association with rates of all kinds of incident mental problems; early menarche was significantly associated with elevated rates of persistent psychotic-like experiences (OR = 2.31, 95% CI 1.01–5.27) (see Tables 2 and 3).
Menstrual irregularity and mental health problems
Menstrual irregularity was significantly associated with increased rates of incident anxiety (OR = 1.77, 95% CI 1.03–3.06) and insomnia (OR = 1.69, 95% CI 1.08– 2.64); menstrual irregularity was significantly associated with increased rates of persistent depression (OR = 5.88, 95% CI 2.10–16.51), anxiety (OR = 3.39, 95% CI 1.85–6.20), ADHD (OR = 3.40, 95% CI 1.67–6.93), insomnia (OR = 2.03, 95% CI 1.20–3.42), psychotic-like experiences (OR = 5.21, 95% CI 1.59–17.05), non-suicidal self-injury (OR = 2.90, 95% CI 1.61–5.26), suicidal ideation (OR = 2.15, 95% CI 1.41–3.29) and suicide plan (OR = 2.27, 95% CI 1.10–4.71) (see Tables 2 and 3).
Menstrual pain and mental health problems
Menstrual pain was significantly associated with elevated rates of incident PTSD (OR = 1.90, 95% CI 1.08–3.32) and depression (OR = 1.99, 95% CI 1.23–3.21); menstrual pain had significant associations with increased rates of persistent depression (OR = 1.79 95% CI 1.08–2.97), insomnia (OR = 1.97 95% CI 1.33–2.93), psychotic-like experiences (OR = 1.79 95% CI 1.00–3.20), non-suicidal self-injury (OR = 2.00 95% CI 1.34–3.00), suicidal ideation (OR = 1.70 95% CI 1.20–2.42), suicide plan (OR = 2.06 95% CI 1.25–3.40) and suicide attempt (OR = 3.20 95% CI 1.32–7.76) (see Tables 2 and 3).
Discussion
The purpose of this comprehensive study with a longitudinal design was to investigate the roles of menarche, menstrual cycles, and menstrual pain as risk factors for incident and persistent mental health problems including PTSD, depression, ADHD, anxiety, insomnia, psychotic-like experiences, and suicide in a 1-year follow-up study of a large sample of Chinese girls. Since menarche, menstrual cycles, and menstrual pain are very discriminative menstrual characteristics and have different roles in development and maintenance of various mental health problems, the findings are discussed separately as follows.
Early menarche
Inconsistent with previous cross-sectional studies [2, 10, 21] and longitudinal studies [15,16,17,18, 37] that reported early menarche as an important risk factor for various mental health problems, particularly depression and suicidal-related behaviors, there were no significant associations of early menarche with all the incident outcomes and most of persistent mental health problems in this study. Differences in samples, assessment methods, study designs, and follow-up periods may contribute to the controversial findings across studies. It is worth mentioning that most significant reports of early menarche and depression are from one UK group [17,18,19] and studies of suicidal-related behaviors are almost from one Chinese group [2, 10, 21]. More studies are needed, especially those from different cultures and independent groups, to clarify the controversy. Notably, age might be one key variable in studies of menarche. For example, in a longitudinal UK cohort study, Sequeira et al. found that early menarche was associated with higher risks of depression at 14 years but not at 17, 18, and 19 years [19]. In the current sample, the population was likely rather young, and the follow-up period was very short. This may be related to the negative findings.
Interestingly, our study for the first time revealed that early menarche was a risk factor for persistent psychotic-like experiences. The finding is in contrast to the “estrogen hypothesis” that suggests that estrogen could be a protective factor against psychosis. Although the “estrogen hypothesis” has been supported by observations that females with early puberty tend to present fewer psychosis symptoms [38, 39], some studies also found no significant association between the timing of menarche and the age of psychosis onset [40, 41]. The moderators and conditions of the adaptation of the hypothesis should be further explored.
Menstrual irregularity
A wide array of studies with cross-sectional designs have shown a link between irregular periods and mental health problems such as suicide behavior, non-suicidal self-injury, sleep problems, anxiety and depression [2, 10, 13, 42,43,44,45,46,47,48]. Our findings further demonstrated that menstrual irregularity was prospectively associated with onsets of anxiety and insomnia, but not with incident PTSD, depression, ADHD, psychotic-like experiences, and suicide. On one hand, specific psychiatric problems (e.g., sleep disturbances) might be more sensitive to the fluctuations of hormone levels; on the other hand, irregularity may occur during the sensitive period of onset anxiety [49], which would trigger anxiety easily. Although there were no significant relations between menstrual irregularity and incident PTSD, depression, ADHD, psychotic-like experiences, and suicide, irregular menstrual cycles did contribute to the maintenance of these mental health problems except for PTSD. The findings echo earlier cross-sectional studies and several case–control studies which have revealed that clinical symptoms of ADHD and schizophrenia are likely to fluctuate between menstrual periods [42,43,44]. Contrary to our expectation [50, 51], irregular menstruation was neither related to incident PTSD nor persistent PTSD. This may be due to the symptoms of PTSD pertaining to specific traumatic events.
Menstrual pain
In the current study, reporting menstrual pain at baseline was significantly associated with incident PTSD and depression. Evidence from previous studies reported dysmenorrhea was linked to an increased risk of developing PTSD in Iraq and Afghanistan veterans and earthquake-exposed high school students [25, 52]. The possible mechanism between them remains unclear, but there is one possible explanation. PTSD has been reported in association with elevated levels of cytokines TNF-a and IL-1. These cytokines could lead to the further release of prostaglandin E2, which has an indirect effect on menstrual pain by inducing hyperactivity of uterine muscle [53]. Also, the association between dysmenorrhea and depression has been revealed in previous research [24]. The pain as a stressor appears to affect mood [54]. Extending previous research, our study further established a longitudinal association between menstrual pain and PTSD and depression. We observed no association between menstrual pain and incident anxiety, ADHD, insomnia, psychotic-like experiences, NSSI, and suicide behaviors, which indicated that the effect of dysmenorrhea at baseline only applied to specific mental health problems.
With regard to the persistent mental health problems, our results demonstrated that menstrual pain at baseline was significantly associated with persistent depression, insomnia, psychotic-like experiences, NSSI, and suicide. As previously described, monthly repeated menstrual pain could be a stressor that had a lasting impact on specific mental health problems [55]. The underlying mechanism has been explored and clarified by researchers. Latthe et al. found that dysmenorrhea was one of the risk factors for chronic pelvic pain, and females with pelvic pain had more chance of suffering from psychological problems such as depression, neuroticism, and somatization than those without pain [56]. However, despite the advance in the underlying mechanism between dysmenorrhea and psychological problems, there was no significant association between dysmenorrhea and persistent PTSD, anxiety, and ADHD.
Strengths and limitations
This is the first exploratory study to examine the longitudinal association of baseline menstrual characteristics with the incidence and persistence of mental health problems. Significantly, our study makes up for the deficiency of cross-sectional research and provides evidence for the importance of menstruation for the development and maintenance of certain psychiatric disorders. This is noteworthy, as we find evidence for a longitudinal association between menstruation and certain mental health problems in early adolescence. However, several limitations need to be noted. First, the measurements depending on participant self-reporting may give rise to recalling bias. Second, in terms of the measure of regularity of the cycle, only subjective evaluations were made by participants. Adding an objective measure (e.g., asking the participants to report the exact cycle lengths of their previous three to six cycles) would make the variables more reliable. Third, a reverse longitudinal relationship may also exist. Mental health problems at baseline may be also related to increased risks of menstrual problems. Further studies could focus on this point and obtain a non-confounding assessment of the relationship. Fourth, in the present study, the age range of the population in the present study was 9–19 years and girls under the age of 11 accounted for 2.7 percent. Although a previous study showed good reliability and validity of PHQ 9 in children aged 11–17 years [57], the reliability and validity of PHQ 9 in children under the age of 11 need further investigation. Fifth, the mental health history before baseline assessment is unknown. Sixth, the generalizability of the results is limited by the short follow-up time. In the present study, we have examined only a 1-year time window. The effects of menstrual characteristics in late adolescence and even adulthood are unknown. Finally, assessments were performed at a 1-year interval. We did not collect more information about how those mental health disorders fluctuated over the whole 12-month timespan. More frequent assessments of psychiatric problems are needed in future studies to figure out how those psychological problems change or persist over time.
Conclusions
Irregular menstrual cycles and menstrual pain may affect the girls’ mood, leading to the incidence of emotional problems as well as insomnia, and have lasting effects on most mental disorders. Identifying the risk factors for females’ mental health problems helps differentiate adolescents who are more likely to suffer from specific psychiatric disorders and provide appropriate prevention and interventions targeting specific risk factors. In clinical practice, treatment of abnormal menstruation could be a way of improving the mental health condition.
References
Critchley HOD, Babayev E, Bulun SE, Clark S, Garcia-Grau I, Gregersen PK, Kilcoyne A, Kim J-YJ, Lavender M, Marsh EE, Matteson KA, Maybin JA, Metz CN, Moreno I, Silk K, Sommer M, Simon C, Tariyal R, Taylor HS, Wagner GP, Griffith LG (2020) Menstruation: science and society. Am J Obstet Gynecol 223:624–664. https://doi.org/10.1016/j.ajog.2020.06.004
Liu X, Liu Z-Z, Fan F, Jia C-X (2018) Menarche and menstrual problems are associated with non-suicidal self-injury in adolescent girls. Arch Womens Ment Health 21:649–656. https://doi.org/10.1007/s00737-018-0861-y
Esen İ, Oğuz B, Serin HM (2016) Menstrual characteristics of pubertal girls: a questionnaire-based study in Turkey. J Clin Res Pediatr Endocrinol 8:192–196. https://doi.org/10.4274/jcrpe.2026
Paffenbarger RSJ, Kampert JB, Lee IM, Hyde RT, Leung RW, Wing AL, Hsieh CC (1994) Age at menarche. Med Sci Sports Exerc 314:605–613
Ersoy B, Balkan C, Gunay T, Egemen A (2005) The factors affecting the relation between the menarcheal age of mother and daughter. Child Care Health Dev 31:303–308. https://doi.org/10.1111/j.1365-2214.2005.00501.x
Diaz A, Laufer MR, Breech LL (2006) Menstruation in girls and adolescents: using the menstrual cycle as a vital sign. Pediatrics 118:2245–2250. https://doi.org/10.1542/peds.2006-2481
Lei Y, Luo D, Yan X, Zhang J, Hu P, Ma J, Song Y, Lau PWC (2021) The mean age of menarche among Chinese schoolgirls declined by 6 months from 2005 to 2014. Acta Paediatr Int J Paediatr 110:549–555. https://doi.org/10.1111/apa.15441
French L (2008) Dysmenorrhea in adolescents. Pediatr Drugs 10:1–7. https://doi.org/10.2165/00148581-200810010-00001
Chan SSC, Yiu KW, Yuen PM, Sahota DS, Chung TKH (2009) Menstrual problems and health-seeking behaviour in Hong Kong Chinese girls. Hong Kong Med J 15:18–23
Chen H, Wang XT, Bo QG, Zhang DM, Qi ZB, Liu X, Jia CX (2017) Menarche, menstrual problems and suicidal behavior in Chinese adolescents. J Affect Disord 209:53–58. https://doi.org/10.1016/j.jad.2016.11.027
Ravi R, Shah P, Palani G, Edward S, Sathiyasekaran BWC (2016) Prevalence of menstrual problems among adolescent school girls in rural Tamil Nadu. J Pediatr Adolesc Gynecol 29:571–576. https://doi.org/10.1016/j.jpag.2015.10.016
Cakir M, Mungan I, Karakas T, Girisken I, Okten A (2007) Menstrual pattern and common menstrual disorders among university students in Turkey. Pediatr Int 49:938–942. https://doi.org/10.1111/j.1442-200X.2007.02489.x
Yu M, Han K, Nam GE (2017) The association between mental health problems and menstrual cycle irregularity among adolescent Korean girls. J Affect Disord 210:43–48. https://doi.org/10.1016/j.jad.2016.11.036
Williams CE, Creighton SM (2012) Menstrual disorders in adolescents: review of current practice. Horm Res Paediatr 78:135–143. https://doi.org/10.1159/000342822
Ge X, Conger RD, Elder GH (1996) Coming of age too early: pubertal influences on girls’ vulnerability to psychological distress. Child Dev 67:3386–3400. https://doi.org/10.1111/j.1467-8624.1996.tb01919.x
Joinson C, Heron J, Lewis G, Croudace T, Araya R (2011) Timing of menarche and depressive symptoms in adolescent girls from a UK cohort. Br J Psychiatry 198:17–23. https://doi.org/10.1192/bjp.bp.110.080861
Joinson C, Heron J, Araya R, Lewis G (2013) Early menarche and depressive symptoms from adolescence to young adulthood in a UK cohort. J Am Acad Child Adolesc Psychiatry 52:591-598.e2. https://doi.org/10.1016/j.jaac.2013.03.018
Sequeira ME, Lewis SJ, Bonilla C, Smith GD, Joinson C (2017) Association of timing of menarche with depressive symptoms and depression in adolescence: Mendelian randomisation study. Br J Psychiatry 210:39–46. https://doi.org/10.1192/bjp.bp.115.168617
Kim T, Nam GE, Han B, Cho SJ, Kim J, Eum DH, Lee SW, Min SH, Lee W, Han K, Park YG (2018) Associations of mental health and sleep duration with menstrual cycle irregularity: a population-based study. Arch Womens Ment Health 21:619–626. https://doi.org/10.1007/s00737-018-0872-8
Liu X, Chen H, Liu Z-Z, Fan F, Jia C-X (2017) Early menarche and menstrual problems are associated with sleep disturbance in a large sample of chinese adolescent girls. Sleep 40:1–30. https://doi.org/10.1093/sleep/zsx107
Wang ZY, Liu ZZ, Jia CX, Liu X (2019) Age at menarche, menstrual problems, and daytime sleepiness in Chinese adolescent girls. Sleep 42:1–8. https://doi.org/10.1093/sleep/zsz061
Buckley TM, Schatzberg AF (2005) On the Interactions of the Hypothalamic-Pituitary-Adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J Clin Endocrinol Metab 90:3106–3114. https://doi.org/10.1210/jc.2004-1056
Adams Hillard PJ (2008) Menstruation in adolescents: what’s normal, what’s not. Ann N Y Acad Sci 1135:29–35. https://doi.org/10.1196/annals.1429.022
Uçar T, Timur Taşhan S, Aksoy Derya Y, Nacar G (2018) An analysis of dysmenorrhoea and depressive symptoms in university students: a case-control study. Int J Nurs Pract 24:1–7. https://doi.org/10.1111/ijn.12678
Takeda T, Tadakawa M, Koga S, Nagase S, Yaegashi N (2013) Relationship between dysmenorrhea and posttraumatic stress disorder in Japanese high school students 9 months after the Great East Japan earthquake. J Pediatr Adolesc Gynecol 26:355–357. https://doi.org/10.1016/j.jpag.2013.06.020
Gagua T, Tkeshelashvili B, Gagua D, Mchedlishvili N (2013) Assessment of anxiety and depression in adolescents with primary dysmenorrhea: a case-control study. J Pediatr Adolesc Gynecol 26:350–354. https://doi.org/10.1016/j.jpag.2013.06.018
Zhan N, Xie D, Zou J, Wang J, Geng F (2021) The validity and reliability of benevolent childhood experiences scale in Chinese community adults. Eur J Psychotraumatol. https://doi.org/10.1080/20008198.2021.1945747
Geng F, Li S, Yang Y, Zou J, Tu L, Wang J (2021) Trauma exposure and posttraumatic stress disorder in a large community sample of Chinese adults. J Affect Disord 291:368–374. https://doi.org/10.1016/j.jad.2021.05.050
Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL (2015) The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress 28:489–498. https://doi.org/10.1002/jts.22059
Kroenke K, Spitzer RL, Williams JBW (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16:606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, Howes MJ, Jin R, Secnik K, Spencer T, Ustun TB, Walters EE (2005) The World Health Organization adult ADHD self-report scale (ASRS): a short screening scale for use in the general population. Psychol Med 35:245–256. https://doi.org/10.1017/S0033291704002892
Schuetz CG (2008) Psychometric properties of the Chinese version of the adult ADHD Self-report Scale. Int J Methods Psychiatr Res 17(Suppl 1):S78–S82. https://doi.org/10.1002/mpr
Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M (1999) Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry 38:1230–1236. https://doi.org/10.1097/00004583-199910000-00011
Liu X, Yang Y, Liu ZZ, Luo Y, Fan F, Jia CX (2019) Psychometric properties of Youth Self-Rating Insomnia Scale (YSIS) in Chinese adolescents. Sleep Biol Rhythms 17:339–348. https://doi.org/10.1007/s41105-019-00222-3
Lecrubier Y, Sheehan D, Hergueta T, Weiller E (1998) The mini international neuropsychiatric interview. Eur Psychiatry 13:198S-198S. https://doi.org/10.1016/s0924-9338(99)80239-9
Nock MK, Holmberg EB, Photos VI, Michel BD (2007) Self-injurious thoughts and behaviors interview: development, reliability, and validity in an adolescent sample. Psychol Assess 19:309–317. https://doi.org/10.1037/1040-3590.19.3.309
Stice E, Presnell K, Bearman SK (2001) Relation of early menarche to depression, eating disorders, substance abuse, and comorbid psychopathology among adolescent girls. Dev Psychol 37:608–619. https://doi.org/10.1037/0012-1649.37.5.608
Seeman MV, Lang M (1990) The role of estrogens in schizophrenia gender differences. Schizophr Bull 16:185–194. https://doi.org/10.1093/schbul/16.2.185
Castle DJ, Abel K, Noriyoshi T, Murray RM (1995) Gender differences in schizophrenia: hormonal effect or subtypes? Schizophr Bull 21:1–12. https://doi.org/10.1093/schbul/21.1.1
Rubio-Abadal E, Usall J, Barajas A, Carlson J, Iniesta R, Huerta-Ramos E, Baños I, Dolz M, Sánchez B, Ochoa S, Araya S, Arranz B, Arteaga M, Asensio R, Autonell J, Baños I, Bañuelos M, Barajas A, Barceló M, Blanc M, Borrás M, Busquets E, Carlson J, Carral V, Castro M, Corbacho C, Coromina M, Cuevas J, Dachs I, Dolz M, Domenech MD, Elias M, Espezel I, Falo E, Fargas A, Foix A, Fusté M, Godrid M, Gómez D, González O, Granell L, Gumà L, Haro JM, Herrera S, Huerta-Ramos E, Lacasa F, Mas N, Martí L, Martínez R, Matalí J, Miñambres A, Miquel L, Muñoz D, Muñoz V, Nogueroles R, Ochoa S, Ortiz J, Pardo M, Planella M, Pelaez T, Peruzzi S, Rivero S, Rodriguez MJ, Rubio E, Sammut S, Sánchez M, Sánchez B, Serrano E, Solís C, Stephanotto C, Tabuenca P, Teba S, Torres A, Urbano D, Usall J, Vilaplana M, Villalta V (2016) Relationship between menarche and psychosis onset in women with first episode of psychosis. Early Interv Psychiatry 10:419–425. https://doi.org/10.1111/eip.12194
Hochman KM, Lewine RR (2004) Age of menarche and schizophrenia onset in women. Schizophr Res 69:183–188. https://doi.org/10.1016/S0920-9964(03)00176-2
Riecher-rössler A, Häfner H, Stumbaum M, Maurer K, Schmidt R (1994) Can estradiol modulate schizophrenic symptomatology? Schizophr Bull 20:203–214. https://doi.org/10.1093/schbul/20.1.203
Choi SH, Kang SB, Joe SH (2001) Changes in premenstrual symptoms in women with schizophrenia: a prospective study. Psychosom Med 63:822–829. https://doi.org/10.1097/00006842-200109000-00016
Roberts B, Eisenlohr-Moul T, Martel MM (2018) Reproductive steroids and ADHD symptoms across the menstrual cycle. Psychoneuroendocrinology 88:105–114. https://doi.org/10.1016/j.psyneuen.2017.11.015
Mahon JN, Rohan KJ, Nillni YI, Zvolensky MJ (2015) The role of perceived control over anxiety in prospective symptom reports across the menstrual cycle. Arch Womens Ment Health 18:239–246. https://doi.org/10.1007/s00737-014-0456-1
Dorn LD, Negriff S, Huang B, Pabst S, Hillman J, Braverman P, Susman EJ (2009) Menstrual symptoms in adolescent girls: association with smoking, depressive symptoms, and anxiety. J Adolesc Heal 44:237–243. https://doi.org/10.1016/j.jadohealth.2008.07.018
Kiesner J, Poulin F (2012) Developmental associations between adolescent change in depressive symptoms and menstrual-cycle-phase-specific negative affect during early adulthood. J Youth Adolesc 41:1325–1338. https://doi.org/10.1007/s10964-011-9722-y
Gleeson PC, Worsley R, Gavrilidis E, Nathoo S, Ng E, Lee S, Kulkarni J (2016) Menstrual cycle characteristics in women with persistent schizophrenia. Aust N Z J Psychiatry 50:481–487. https://doi.org/10.1177/0004867415590459
Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, Il Shin J, Kirkbride JB, Jones P, Kim JH, Kim JY, Carvalho AF, Seeman MV, Correll CU, Fusar-Poli P (2022) Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry 27:281–295. https://doi.org/10.1038/s41380-021-01161-7
Pineles SL, Nillni YI, Patton SC, Mostoufi SM, Hauger R, Rasmusson AM, King MW, Bauer MR, Gerber MR, Resick PA, Orr SP (2016) Brief report: extinction retention and the menstrual cycle: different associations for women with posttraumatic stress disorder. J Abnorm Psychol 125:349–355. https://doi.org/10.1037/abn0000138
Nillni YI, Pineles SL, Patton SC, Rouse MH, Sawyer AT, Rasmusson AM (2015) Menstrual cycle effects on psychological symptoms in women with PTSD. J Trauma Stress 28:1–7. https://doi.org/10.1002/jts.21984
Cohen BE, Maguen S, Bertenthal D, Shi Y, Jacoby V, Seal KH (2012) Reproductive and other health outcomes in Iraq and Afghanistan women veterans using VA health care: association with mental health diagnoses. Women’s Health Issues 22:e461–e471. https://doi.org/10.1016/j.whi.2012.06.005
Wu MH, Lu CW, Chuang PC, Tsai SJ (2010) Prostaglandin E2: the master of endometriosis? Exp Biol Med 235:668–677. https://doi.org/10.1258/ebm.2010.009321
Balik G, Üstüner I, Kağitci M, Şahin FK (2014) Is there a relationship between mood disorders and dysmenorrhea? J Pediatr Adolesc Gynecol 27:371–374. https://doi.org/10.1016/j.jpag.2014.01.108
Wang L, Wang X, Wang W, Chen C, Ronnennberg AG, Guang W, Huang A, Fang Z, Zang T, Wang L, Xu X (2004) Stress and dysmenorrhoea: a population based prospective study. Occup Environ Med 61:1021–1026. https://doi.org/10.1136/oem.2003.012302
Dutton P (2006) Factors predisposing women to chronic pelvic pain: systematic review. J Fam Plan Reprod Health Care 32:244–244. https://doi.org/10.1783/147118906778586732
Leung DYP, Mak YW, Leung SF, Chiang VCL, Loke AY (2020) Measurement invariances of the PHQ-9 across gender and age groups in Chinese adolescents. Asia Pac Psychiatry 12:1–6. https://doi.org/10.1111/appy.12381
Funding
The present study was funded by National Natural Science Foundation of China (Grant numbers: 31700987, 32260210). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yuan, D., Li, Q., Zhan, N. et al. Longitudinal associations of menstrual characteristics with mental health problems among Chinese girls. Eur Child Adolesc Psychiatry 33, 2547–2556 (2024). https://doi.org/10.1007/s00787-023-02345-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-023-02345-y