Abstract
This study was conducted with rats to determine the safety of long-term dietary supplementation with l-arginine. Beginning at 6 weeks of age, male and female rats were fed a casein-based semi-purified diet containing 0.61 % l-arginine and received drinking water containing l-arginine-HCl (0, 1.8, or 3.6 g l-arginine/kg body-weight/day; n = 10/group). These supplemental doses of l-arginine were equivalent to 0, 286, and 573 mg l-arginine/kg body-weight/day, respectively, in humans. After a 13-week supplementation period, blood samples were obtained from rats for biochemical analyses. Supplementation with l-arginine increased plasma concentrations of arginine, ornithine, proline, homoarginine, urea, and nitric oxide metabolites without affecting those for lysine, histidine, or methylarginines, while reducing plasma concentrations of ammonia, glutamine, free fatty acids, and triglycerides. l-Arginine supplementation enhanced protein gain and reduced white-fat deposition in the body. Based on general appearance, feeding behavior, and physiological parameters, all animals showed good health during the entire experimental period; Plasma concentrations of all measured hormones (except leptin) did not differ between control and arginine-supplemented rats. l-Arginine supplementation reduced plasma levels of leptin. Additionally, l-arginine supplementation increased l-arginine:glycine amidinotransferase activity in kidneys but not in the liver or small intestine, suggesting tissue-specific regulation of enzyme expression by l-arginine. Collectively, these results indicate that dietary supplementation with l-arginine (e.g., 3.6 g/kg body-weight/day) is safe in rats for at least 91 days. This dose is equivalent to 40 g l-arginine/kg body-weight/day for a 70-kg person. Our findings help guide clinical studies to determine the safety of long-term oral administration of l-arginine to humans.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
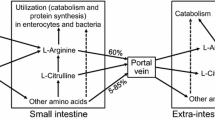
l-Arginine is synthesized in virtually all cell types from l-citrulline (Breuillard et al. 2015; Wu et al. 2007b), which is derived from l-glutamine/l-glutamate via pyrroline-5-carboxylate synthase (Blachier et al. 2011; Wu et al. 1994) and from l-proline via proline oxidase (Wu 1997) almost exclusively in enterocytes of most mammals, including humans, rats and pigs. l-Arginine is utilized by multiple metabolic pathways to produce protein, nitric oxide (NO), ornithine (the precursor of polyamines, proline, and glutamate), creatine, and agmatine (Wu and Morris 1998). Additionally, post-translational methylation of arginine residues in protein and its subsequent hydrolysis results in the production of asymmetrical dimethylarginine (ADMA), NG-monomethylarginine (NMMA), and symmetric dimethylarginine (SDMA). ADMA and NMMA are competitive inhibitors of NO synthases (NOS), whereas SDMA inhibits l-arginine transport by cells (Leiper and Vallance 1999). Although l-arginine was considered in the 1960s to be a substrate for the synthesis of l-homoarginine (hArg) by l-arginine:glycine amidinotransferase (AGAT) in rats (Ryan and Wells 1964; Ryan et al. 1968, 1969), little work had been done to examine mammalian hArg synthesis and catabolism until the 2010s. Emerging evidence shows that hArg may be a biomarker for risk for cardiovascular diseases (Atzler et al. 2015; Kayacelebi et al. 2015; Khalil et al. 2013; Michel 2013; Tsikas and Kayacelebi 2014).
Metabolites produced from l-arginine have enormous metabolic versatility (Blachier et al. 2011; Morris 2007; San Gabriel and Uneyama 2013). For example, NO regulates endothelium-dependent relaxation of blood vessels and energy metabolism in animals (Dai et al. 2013; Gornik and Creager 2004; Wu and Meininger 2009). Second, polyamines are required for the synthesis of DNA and protein as well as the proliferation and differentiation of all cell types (Agostinelli 2014). Third, proline is a major amino acid for collagen synthesis and, therefore, plays a key role in remodeling of the extracellular matrix (Phang and Liu 2012). Fourth, hArg is an inhibitor of l-arginine transport by cells (Greene et al. 1993), arginase (Hrabák et al. 1994), as well as liver and bone alkaline phosphohydrolases (Lin and Fishman 1972). Finally, creatine is an antioxidant and participates in energy metabolism in skeletal muscle and nerves (Brosnan and Brosnan 2007). Thus, there is growing interest in the use of l-arginine in improving health and treating various vascular diseases (Popolo et al. 2014; Wu 2014; Yang et al. 2015).
Although much is known about the biochemistry, physiology, and nutrition of l-arginine, the use of l-arginine as a dietary or beverage supplement has been limited due to the concerns of regulatory agencies, policymakers, and consumers over the safety of its long-term administration in humans (i.e., >2 months). This is due to (1) the lack of clinical data in the literature (e.g., concentrations of metabolites in the plasma) (Cicero and Colletti 2015; Shao and Hathcock 2008); and (2) a possible increase in the risk of adverse cardiovascular events in patients with acute myocardial infarction (Schulman et al. 2006). We have recently reported that long-term (91-day) supplementation of l-arginine does not adversely affect blood chemistry or general health status of pigs (Hu et al. 2015). The present study was conducted with rats to determine their physiological responses to long-term dietary supplementation with graded levels of l-arginine-HCl [i.e., 0, 1.8, and 3.6 g l-arginine/kg body-weight (BW)/day]. Availability of data from two animal models will help to guide future clinical studies (FDA 2005), such as those involving dietary supplementation with high doses of l-arginine to humans.
Materials and methods
l-Arginine-HCl and l-alanine were products of Ajinomoto Inc. (Tokyo, Japan). Their purity was >99.9 %, as analyzed by high-performance liquid chromatography (Wu and Meininger 2008). The sources of other chemicals were the same as described previously (Hou et al. 2015; Hu et al. 2015).
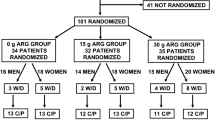
Experiment 1: effects of long-term dietary l-arginine-HCl supplementation on male rats
Animals and diets
Male Sprague–Dawley rats (5 weeks of age) were purchased from Harlan Laboratories (Indianapolis, IN). Upon arrival at the Texas A&M University Kleberg animal facilities, all rats were housed individually in carbonate cages in a temperature-controlled (25 °C) and humidity-controlled (60 % relative humidity) room on a 12-h light:12-h dark cycle. During a 1-week period of adaptation, the animals were fed a regular rodent diet (Product Cat #8604, Harlan Teklad) and had free access to drinking water (double-distilled and deionized water).
At 6 weeks of age, rats were assigned randomly to one of three treatment groups (0, 2.18, or 4.35 g l-arginine-HCl/kg BW/day). These doses of l-arginine-HCl provided 0, 1.8, or 3.6 g l-arginine/kg BW/day, respectively. Isonitrogenous amounts of l-alanine were added to the drinking water (Table 1). The dosages of l-arginine and l-alanine were chosen on the basis of previous studies with rats (Tsubuku et al. 2004; Fu et al. 2005) and pigs (Hu et al. 2015). l-Alanine was used as the isonitrogenous control primarily because of its extensive catabolism in the body, its safety, and its inability to serve as a precursor for endogenous synthesis of arginine (Jobgen et al. 2009a; Kohli et al. 2004). There were 10 rats per group. During the entire period of the experiment, rats were fed a casein-based semi-purified diet containing 4.3 % fat (Jobgen et al. 2009a) and had free access to their respective drinking water (double-distilled and deionized water). This enteral diet contained 0.61 % l-arginine and 0.44 % l-alanine, as analyzed by HPLC (Dai et al. 2014). Concentrations of l-arginine-HCl in drinking water were adjusted according to the volume of water consumed by rats to provide intake of 0, 2.18, and 4.35 g l-arginine-HCl/kg BW/day. Mean concentrations of l-arginine-HCl in drinking water were 0, 2.57, and 5.08 g/100 ml for male rats in the 0, 2.18, and 4.35 g l-arginine-HCl/kg BW/day groups, respectively.
Because our pilot studies showed that arginine-supplemented rats tended to eat more food than control rats, arginine-supplemented rats were individually pair-fed with rats in the control group (no supplemental l-arginine-HCl) on a kg BW basis to ensure similar intakes of all nutrients (except for arginine and alanine) among the three groups. Body weight, food intake, and water intake of each rat were recorded on a daily basis throughout the study. No spillage of food (pellet form) was noted for any group of rats. Urine glucose and ketone bodies were tested every 4 weeks using Chemstrip.up, as described previously (Wu 1995a).
During the 13th week of arginine supplementation, oxygen consumption, CO2 production, and energy expenditure were measured between 9:00 and 11:00 AM using a computer-controlled Oxymas instrument (Columbus Instruments, OH, USA), as we described previously (Tekwe et al. 2013). Furthermore, non-invasive tail-cuff measurement of systolic blood pressure was performed, as described by Wu (1995a). After the 13 weeks of arginine supplementation, rats (19 weeks or 133 days of age) were food deprived for 5 h to obtain blood samples (100 µL) from the tail vein using a microhematocrit (Jobgen et al. 2009a) for analyses of serum glucose and amino acids (except for methylarginines and hArg). On the day of euthanasia, after rectal temperatures of the rats were recorded using a thermometer designed for rats, the animals were immediately anesthetized with CO2 and killed by cervical dislocation. Cardiac blood samples were collected into heparinized tubes and centrifuged immediately to obtain plasma for analyses of lipids, hormones, methylarginines, and hArg, whereas liver, kidney and jejunum samples (approximately 0.5 g) were immediately obtained and placed in liquid nitrogen (Jobgen et al. 2009a). In addition, retroperitoneal, epididymal, subcutaneous (inguinal), and mesenteric adipose tissues, as well as brown adipose tissue (located in the interscapular region), extensor digitorum longus (EDL) and soleus muscles, brain, liver, kidney, and other tissues were dissected and weighed. Intestinal lumen content was removed before the gut was weighed.
Determination of body composition
After tissues of euthanized rats were weighed, the whole body of each animal (including the empty gastrointestinal tract) was homogenized using a Seydelmann Cutter K64 (Strasser; Stuttgart, Germany), as described by Satterfield et al. (2012, 2013). The content of water, crude protein, crude fat, ash, and carbohydrate was determined, as we described (Jobgen et al. 2009a; Wu et al. 1999).
Analysis of amino acids, glucose, creatinine, ammonia, urea, NOx, and enzymes in plasma
For analysis of metabolites, plasma (0.1 ml) was deproteinized with an equal volume of 1.5 M HClO4, followed by addition of 0.05 ml 2 M K2CO3 (Wu et al. 1994). Amino acids (including methylarginines and hArg) in the neutralized extract were determined by fluorometric HPLC methods involving precolumn derivatization with o-phthaldialdehyde, as described previously (Hou et al. 2015; Wu and Meininger 2008). The integration of chromatographic peaks was performed using the Millenium-32 Software (Waters, Milford, MA, USA). Glucose was determined enzymatically by a spectrophotometric method involving hexokinase and glucose-6-phosphate dehydrogenase (Satterfield et al. 2013). Creatinine was determined using a kit from Sigma Chemicals (St. Louis, MO, USA). Ammonia and urea were determined using glutamate dehydrogenase and urease plus glutamate dehydrogenase, respectively (Wu 1995b). Nitrate and nitrite (NOx) levels were determined by an HPLC method involving the enzymatic conversion of nitrate into nitrite and the derivatization of nitrite with 2,3-diaminonaphthalene (DAN) to form 2,3-naphthotriazole, as we described previously (Jobgen et al. 2007). Activities of alanine transaminase and aspartate transaminase in plasma were measured as described by Wu et al. (2000), whereas alkaline phosphatase and lactate dehydrogenase activities were determined using assay kits from Sigma Chemicals.
Analysis of free fatty acids, triglycerides, and hormones in plasma
Free fatty acids and triglycerides in plasma were analyzed using assay kits from Wako Chemicals (Richmond, VA, USA), as we previously described (Jobgen et al. 2009a). Plasma insulin, growth hormone, insulin-like growth factor-I, adiponectin, leptin, corticosterone, total triiodothyronine, and total thyroxine were determined using radioimmunoassay kits for rats (Linco, St. Louis, MO), as we previously described (Jobgen et al. 2009a).
Concentrations of hArg and AGAT activity in tissues
To provide an explanation for our observation that plasma concentrations of hArg were increased in arginine-supplemented rats, we determined concentrations of hArg and AGAT activity in the liver and kidney (which are likely major tissues for hArg synthesis in animals), as we described previously (Hou et al. 2015). Because the enteral diet directly provides arginine and lysine to the lumen of the small intestine, we also measured concentrations of hArg and AGAT activity in the jejunum. AGAT activity in tissue homogenates was measured at 37 °C for 15 min in the presence of 80 mM sodium phosphate buffer (pH 7.5) containing 15 mM l-arginine plus 15 mM l-lysine. Under the enzyme assay conditions used, addition of protease inhibitors (Wu 1997) to tissue homogenates had no effect on AGAT activity in the liver, kidney or small intestine.
Experiment 2: effects of long-term dietary l-arginine-HCl supplementation on female rats
Experiment 2 was conducted as Experiment 1, except that female rats were used instead of male rats. Per kg BW, female rats consumed more water than male rats. Thus, concentrations of l-arginine-HCl in drinking water were adjusted according to the volume of water consumption by female rats to provide intake of 0, 2.18, and 4.35 g l-arginine-HCl/kg BW/day. Mean concentrations of l-arginine-HCl in drinking water were 0, 2.06, and 3.92 g/100 ml for female rats in the 0, 2.18, and 4.35 g l-arginine-HCl/kg BW/day groups, respectively.
Statistical analyses
Results are expressed as mean ± SEM. Statistical analyses of data were performed by one-way analysis of variance using the General Linear Models procedures (Assaad et al. 2014b). Differences among treatment means were determined using the Student–Newman–Keuls multiple comparison method (Assaad et al. 2014a, b). A probability value ≤0.05 was taken to indicate statistical significance.
Results
Overall observations
Feeding behavior, water consumption, hair, general appearance, body-weight gain, rectal temperature, urination, and defecating were normal for all the male and female rats throughout the 13-week period of l-arginine supplementation (Table 2). Rats in all the groups were alert and vivacious. Blood pH did not differ between control and arginine-supplemented rats. Urine tests for glucose and ketone bodies were negative for all rats. No sickness (including diarrhea) or injury was observed for any animals. All internal organs of the male and female rats appeared normal upon gross examination.
Food intakes and water consumption of rats
Dietary supplementation with 1.8 and 3.6 g l-arginine/kg BW/day did not affect (P > 0.05) either food intake or water consumption by male (Exp. 1) or female (Exp. 2) rats (Table 2). Food intakes by male and female rats were approximately 45.6 and 49.5 g/kg BW/day, respectively (Table 2). These levels of food intake supplied 278 and 302 mg l-arginine/kg BW/day in the basal diet to male and female rats, respectively. In either male or female rats, arginine supplementation did not affect their water consumption, which was approximately 86 and 109 ml/kg BW/day, respectively (Table 2). Through adjusting l-arginine-HCl concentrations in drinking water, both male and female rats received supplementation of l-arginine in the amounts of 0, 1.8, and 3.6 g/kg BW/day, which were approximately 0, 6, and 12 times the l-arginine intake from the basal diet, respectively. Based on the conversion ratio of 1:0.16 (rats vs. humans; FDA 2005), the human-equivalent doses of the supplemental l-arginine were 0, 286, and 573 mg l-arginine/kg body-weight/day, respectively, or 20, and 40 g l-arginine/day for a 70-kg person, respectively.
Body weight, whole-body energy expenditure, blood pressure, and body composition of rats
In either male (Exp. 1) or female (Exp. 2) rats, supplementing 1.8 and 3.6 g l-arginine/kg BW/day did not affect (P > 0.05) the body weight of the animals (Table 2). However, weights of skeletal muscle, brown adipose tissue, and thymus were increased (P < 0.05) but weights of white adipose tissue were decreased (P < 0.05) in both male and female rats in response to dietary supplementation with arginine (Table 3). Weights of other tissues did not differ between control and arginine-supplemented rats. l-Arginine supplementation enhanced (P < 0.05) oxygen consumption, CO2 production, and energy expenditure [expressed per kg non-fat mass (Assaad et al. 2014a)] (Table 4), while reducing (P < 0.05) systolic blood pressure (Table 2), in both male and female rats. Compared with the control group, supplementing 1.8 and 3.6 g l-arginine/kg BW/day to male or female rats decreased (P < 0.05) the percentage of fat and increased (P < 0.05) the percentage of protein in the body (Table 5).
Concentrations of amino acids, other metabolites, hormones, and enzymes in the plasma of rats
Plasma concentrations of amino acids and related metabolites in control and arginine-supplemented male or female rats are summarized in Table 6. Dietary supplementation with 1.8 and 3.6 g l-arginine/kg BW/day dose dependently increased (P < 0.05) plasma concentrations of arginine, ornithine, proline, hArg, and urea, while reducing plasma concentrations of glutamine, ammonia, free fatty acids, and triglycerides in both males and females. Dietary supplementation with arginine did not affect (P > 0.05) concentrations of lysine, histidine, citrulline, ADMA, NMMA, SDMA, other amino acids, creatinine, or glucose in the plasma of male or female rats (Table 6). Concentrations of all measured hormones (except leptin), as well as the activities of alanine transaminase, aspartate transaminase, and lactate dehydrogenase in the plasma did not differ (P > 0.05) between control and arginine-supplemented rats (Table 7). l-Arginine supplementation reduced (P < 0.05) the concentration of leptin but increased (P < 0.05) the activity of alkaline phosphatase in the plasma of both male and female rats in a dose-dependent manner (Table 7).
Concentrations of hArg and AGAT activity in tissues of rats
The concentrations of hArg and AGAT activity were highest in the liver, followed by the kidneys and the small intestine in descending order (Table 8). Supplementing 1.8 and 3.6 g l-arginine/kg BW/day to male and female rats increased (P < 0.05) concentrations of hArg and AGAT activity in the kidney, but had no effect (P > 0.05) in the liver or the small intestine (Table 8).
Discussion
l-Arginine is an abundant amino acid in animals, representing 14 % of total nitrogen in body protein (Wu et al. 1999; Wu 2014). Besides serving as a major substrate for synthesis of proteins, l-arginine is actively utilized via multiple pathways to generate low-molecular-weight bioactive substances (e.g., NO, creatine, polyamines, hArg, and agmatine). Thus, mammals, birds, and fish have high requirements for l-arginine, which may be increased in certain physiological (e.g., pregnancy, lactation, exercise, and exposure to a cold environment) and pathological (e.g., injury, burns, obesity, and diabetes) situations (Wu et al. 2013). In addition, l-arginine can regulate multiple metabolic pathways [e.g., the hepatic urea cycle and tetrahydrobiopterin synthesis (Wu and Morris 1998; Shi et al. 2004)], gene expression [e.g., peroxisome proliferator-activated receptor γ coactivator-1α and AMP-activated protein kinase (Fu et al. 2005; Jobgen et al. 2009b)], and cell signaling pathways [e.g., the mammalian target of rapamycin (mTOR) and focal adhesion kinase (Rhoads and Wu 2009; Yao et al. 2008)]. Thus, l-arginine has been employed in clinical studies to improve cardiovascular function, reduce obesity, and treat a variety of diseases associated with inadequate production of NO (Hurt et al. 2014; Li et al. 2014; Lucotti et al. 2006; Wu et al. 2009). Despite its versatile metabolic functions, the use of l-arginine as a dietary or beverage supplement has been limited due to the concerns of regulatory agencies, policymakers, and consumers over the safety of its long-term supplementation in humans (i.e., >2 months), primarily because of the lack of clinical data (Boger and Bode-Boger 2001; Cicero and Colletti 2015; Cynober 2007; Shao and Hathcock 2008).
Mean arginine intake by the U.S. adult population is ~5 g/day (Flynn et al. 2002). Approximately 40 % of l-arginine in the diet is catabolized in the first pass by the small intestine, and the remaining 60 % (namely, 3 g arginine/day) enters the portal circulation (Castillo et al. 1993; Dai et al. 2011). Results of previous short-term studies indicate the absence of a systematic pattern of adverse effects of oral l-arginine administration in adult humans, which precludes the selection of “No Observed Adverse Effect Level” or “Lowest Observed Adverse Effect Level” as the usual approach to identify a tolerable Upper Level of intake for this dietary supplement (Hayashi 2003; Shao and Hathcock 2008). Thus, investigators have developed a newer method for risk assessment, named the Observed Safe Level (OSL) or the Highest Observed Intake, which is defined as the highest intake level with sufficient evidence of safety (FAO/WHO 2006). In a double-blind, placebo-controlled trial with 16 healthy adult males, oral administration of 20 g l-arginine/day for 4 weeks did not result in any adverse effect as determined by standard clinical chemistry indices (Chin-Dusting et al. 1996). Likewise, healthy adults could tolerate oral administration of 40 g l-arginine/day for 1 week (duration of the study; Beaumier et al. 1995). Similarly, results from other trials indicated no side effects of oral administration of 21 and 42 g l-arginine/day to patients with hypercholesterolemia (Clarkson et al. 1996) and cystic fibrosis (Grasemann et al. 2005) for 4 and 6 weeks, respectively. Based on these findings, an OSL value for oral administration of l-arginine to healthy adults has been suggested to be 20 g/day (Shao and Hathcock 2008). However, the published studies with healthy subjects involved a short duration of l-arginine supplementation (1 to 4 weeks) and a very small number of subjects (5–16) (Beaumier et al. 1995; Chin-Dusting et al. 1996). These concerns limit our confidence in the 20 g/day dose as the OSL value for oral administration of l-arginine to healthy adults and underscore the need for larger and longer studies. To date, it is unknown how much dietary arginine can be tolerated by humans for a prolonged period of time (Cicero and Colletti 2015; Evans et al. 2004; McKnight et al. 2010; McNeal et al. 2010). This question can only be answered by doing clinical trials with humans. However, such studies must be based first on long-term animal experiments.
Data from animal studies are much needed before clinical trials are started with humans. We reported that healthy adult pigs and rats can tolerate large amounts of supplemental l-arginine, which are at least 0.21 g/kg body-weight/day (Mateo et al. 2007, 2008) and 2.1 g/kg body-weight/day (Jobgen et al. 2009a, b) for 84 days, respectively (Wu et al. 2007a). Based on standard hematology and clinical chemistry tests, growth, general health status, plasma concentrations of amino acids, other metabolites, hormones (e.g., insulin, growth hormone, and IGF-1), as well as plasma activities of alanine transaminase, aspartate transaminase, and lactate dehydrogenase (indicators of integrity of cells, particularly hepatocytes), we found that dietary supplementation with l-arginine (315, 473, and 630 mg/kg BW/day) was safe in pigs for at least 91 days (Hu et al. 2015). These doses of supplemental arginine are equivalent to 286, 430, and 573 mg l-arginine/kg BW/day, respectively, in humans (Hu et al. 2015). Likewise, Tsubuku et al. (2004) reported that adult male rats can tolerate at least 3.6 g l-arginine/kg BW/day for 13 weeks. Similar results from measurements of various physiological parameters were obtained in the present student involving both male and female rats. Based on the conversion factor adopted by the Food and Drug Administration of the United States (2005), the human-equivalent doses of the supplemental l-arginine from our rat study (1.8 and 3.6 g l-arginine/kg BW/day) were equivalent to 20 and 40 g l-arginine/day for a 70-kg person, respectively.
Dietary supplementation with l-arginine increased plasma concentrations of arginine, ornithine, and proline, while reducing plasma concentrations of ammonia, glutamine, free fatty acids, and triglycerides without any adverse effect on plasma concentrations of other proteinogenic amino acids (e.g., lysine, histidine, glycine, tryptophan, and methionine) in male or female rats (Table 6). This is consistent with the beneficial roles for l-arginine in activating the hepatic urea cycle and enhancing muscle protein synthesis in mammals (Wu and Morris 1998; Yao et al. 2008), while stimulating the oxidation of fatty acids to water and CO2 and inhibiting the synthesis of both long-chain fatty acids and triglycerides in a tissue-specific manner (McKnight et al. 2010; Wu et al. 2012). Accordingly, l-arginine-supplemented rats had a higher rate of energy expenditure (Table 4) and gained more protein but less fat in the body (Table 5), as compared with the control group. In addition, our results indicate that dietary supplementation with 1.8 and 3.6 g l-arginine/kg BW/day does not cause either antagonism among basic amino acids or an imbalance between amino acids in male or female rats. The observation that the plasma activity of alkaline phosphatase (an indicator of its release by both the liver and bone) was higher in arginine-supplemented rats than in the control group, as reported previously for pigs (Hu et al. 2015), may suggest a stimulatory effect of l-arginine on bone growth. Collectively, our results indicate that dietary supplementation with l-arginine (at least 3.6 g/kg BW/day) is safe in both male and female rats for at least 91 days. Our findings help guide clinical studies to determine the safety of long-term oral administration of l-arginine to humans.
Finally, plasma concentrations of methylarginines and hArg in control and arginine-supplemented rats warrant comments. Because the experimental diet did not contain these amino acids, changes in their plasma levels are determined by the balance between production and utilization/excretion (Wu 2013). Although l-arginine had long been identified to be the precursor of ADMA, NMMA, and SDMA (Leiper and Vallance 1999), as well as hArg (Davids et al. 2012; Ryan et al. 1969) in animals, little is known about effects of arginine supplementation on plasma concentrations of these amino acids or about the nutritional regulation of their synthesis in animals or humans. We found that supplementing 1.8 and 3.6 g arginine/kg BW/day for 13 weeks did not affect the concentrations of ADMA, NMMA, and SDMA in the plasma of male or female rats (Table 6). Thus, substantial increases in the ratios of arginine to ADMA, NMMA, and SDMA can overcome inhibitory effects of the methylarginines on NOS and the uptake of arginine by cells (Tsikas et al. 2000), thereby promoting NO production by various tissues and cells (including vascular endothelial cells) and reducing blood pressure (Table 2) in both male and female rats. Similarly, hArg concentrations or AGAT activities in the liver or the small intestine did not differ between control and arginine-supplemented rats. In contrast, both hArg concentrations and AGAT activity in the kidney were enhanced in response to l-arginine supplementation (Table 8). Thus, it is likely that the kidneys, but not the liver or the gut, contribute to an increase in the circulating level of hArg in arginine-supplemented rats. Additionally, our results suggest tissue-specific regulation of AGAT expression by l-arginine.
In conclusion, supplementing 1.8 and 3.6 g l-arginine/kg BW/day for 91 days did not have any adverse effects on the measured physiological variables or general health status of male or female rats. Our results also indicate a promising effect of l-arginine on improving lean tissue mass and metabolic profiles in the plasma, while beneficially reducing plasma concentrations of ammonia, free fatty acids, and triglycerides, as well as white adipose tissue in the body. l-Arginine supplementation enhanced AGAT activity in the kidneys but not in the liver or the small intestine, suggesting a tissue-specific difference in AGAT expression to regulate arginine metabolism in the body. Collectively, the findings from the present study are helpful for predicting a safe upper limit for oral administration of l-arginine to healthy adults and in guiding clinical studies to determine long-term safety of l-arginine supplementation in humans.
Abbreviations
- ADMA:
-
Asymmetrical dimethylarginine
- AGAT:
-
l-Arginine:glycine amidinotransferase
- Arg:
-
l-Arginine
- BW:
-
Body weight
- hArg:
-
l-Homoarginine
- HPLC:
-
High-performance liquid chromatography
- NMMA:
-
NG-monomethylarginine
- NO:
-
Nitric oxide
- NOS:
-
Nitric oxide synthase
- NOx:
-
Nitrate plus nitrite
- SDMA:
-
Symmetrical dimethylarginine
References
Agostinelli E (2014) Polyamines and transglutaminases: biological, clinical, and biotechnological perspectives. Amino Acids 46:475–485
Assaad H, Yao K, Tekwe CD et al (2014a) Analysis of energy expenditure in diet-induced obese rats. Front Biosci 19:967–985
Assaad H, Zhou L, Carroll RJ et al (2014b) Rapid publication-ready MS-Word tables for one-way ANOVA. Springer Plus 3:474
Atzler D, Schwedhelm E, Choe CU (2015) l-homoarginine and cardiovascular disease. Curr Opin Clin Nutr Metab Care 18:83–88
Beaumier L, Castillo L, Ajami AM et al (1995) Urea cycle intermediate kinetics and nitrate excretion at normal and “therapeutic” intakes of arginine in humans. Am J Physiol Endocrinol Metab 269:E884–E896
Blachier F, Davila AM, Benamouzig R et al (2011) Channelling of arginine in NO and polyamine pathways in colonocytes and consequences. Front Biosci (Landmark Ed) 16:1331–1343
Boger RH, Bode-Boger SM (2001) The clinical pharmacology of l-arginine. Annu Rev Pharmacol Toxicol 41:79–99
Breuillard C, Cynober L, Moinard C (2015) Citrulline and nitrogen homeostasis: an overview. Amino Acids 47:685–691
Brosnan JT, Brosnan ME (2007) Creatine: endogenous metabolite, dietary, and therapeutic supplement. Annu Rev Nutr 27:241–261
Castillo L, Chapman TE, Yu YM et al (1993) Dietary arginine uptake by the splanchnic region in adult humans. Am J Physiol Endocrinol Metab 265:E532–E539
Chin-Dusting JP, Alexander CT, Arnold PJ et al (1996) Effects of in vivo and in vitro l-arginine supplementation on healthy human vessels. J Cardiovasc Pharmacol 28:158–166
Cicero AF, Colletti A (2015) Nutraceuticals and blood pressure control: results from clinical trials and meta-analyses. High Blood Press Cardiovasc Prev. doi:10.1007/s40292-015-0081-8
Clarkson P, Adams MR, Powe AJ et al (1996) Oral l-arginine improves endothelium-dependent dilation in hypercholesterolemic young adults. J Clin Invest 97:1989–1994
Cynober L (2007) Pharmacokinetics of arginine and related amino acids. J Nutr 137:1646S–1649S
Dai ZL, Wu G, Zhu WY (2011) Amino acid metabolism in intestinal bacteria: links between gut ecology and host health. Front Biosci 16:1768–1786
Dai ZL, Wu ZL, Yang Y et al (2013) Nitric oxide and energy metabolism in mammals. Biofactors 39:383–391
Dai ZL, Wu ZL, Jia SC et al (2014) Analysis of amino acid composition in proteins of animal tissues and foods as pre-column o-phthaldialdehyde derivatives by HPLC with fluorescence detection. J Chromatogr B 964:116–127
Davids M, Ndika JD, Salomons GS et al (2012) Promiscuous activity of arginine:glycine amidinotransferase is responsible for the synthesis of the novel cardiovascular risk factor homoarginine. FEBS Lett 586:3653–3657
Evans RW, Fernstrom JD, Thompson J et al (2004) Biochemical responses of healthy subjects during dietary supplementation with l-arginine. J Nutr Biochem 15:534–539
Flynn NE, Meininger CJ, Haynes TE et al (2002) The metabolic basis of arginine nutrition and pharmacotherapy. Biomed Pharmacother 56:427–438
Food and Agriculture Organization/World Health Organization (FAO/WHO) (2006) A model for establishing upper levels of intake for nutrients and related substances. Technical Workshop on Nutrient Risk Assessment, Geneva
Food and Drug Administration (FDA), Center for Drug Evaluation and Research (CDER), U.S. Department of Health and Human Services (2005) Guidance for Industry: Estimating the Maximum Safe Starting Dose in Initial Clinical Trials for Therapeutics in Adult Healthy Volunteers, Bethesda, MD
Fu WJ, Haynes TE, Kohli R et al (2005) Dietary l-arginine supplementation reduces fat mass in Zucker diabetic fatty rats. J Nutr 135:714–721
Gornik HL, Creager MA (2004) Arginine and endothelial and vascular health. J Nutr 134:2880S–2887S
Grasemann H, Grasemann C, Kurtz F et al (2005) Oral l-arginine supplementation in cystic fibrosis patients: a placebo-controlled study. Eur Respir J 25:62–68
Greene B, Pacitti AJ, Souba WW (1993) Characterization of L-arginine transport by pulmonary artery endothelial cells. Am J Physiol 264:L351–L356
Hayashi Y (2003) Application of the concept of risk assessment to the study of amino acid supplements. J Nutr 133:2021S–2024S
Hou YQ, Jia SC, Nawaratna G et al (2015) Analysis of L-homoarginine in biological samples by HPLC involving pre-column derivatization with o-phthalaldehyde and N-acetyl-L-cysteine. Amino Acids. doi:10.1007/s00726-015-1962-9
Hrabák A, Bajor T, Temesi A (1994) Comparison of substrate and inhibitor specificity of arginase and nitric oxide (NO) synthase for arginine analogues and related compounds in murine and rat macrophages. Biochem Biophys Res Commun 198:206–212
Hu SD, Li XL, Rezaei R et al (2015) Safety of long-term dietary supplementation with l-arginine in pigs. Amino Acids 47:925–936. doi:10.1007/s00726-015-1921-5
Hurt RT, Ebbert JO, Schroeder DR et al (2014) l-Arginine for the treatment of centrally obese subjects: a pilot study. J Diet Suppl 11:40–52
Jobgen WS, Jobgen SC, Li H et al (2007) Analysis of nitrite and nitrate in biological samples using high-performance liquid chromatography. J Chromatogr B 851:71–82
Jobgen WJ, Meininger CJ, Jobgen SC et al (2009a) Dietary l-arginine supplementation reduces white-fat gain and enhances skeletal muscle and brown fat masses in diet-induced obese rats. J Nutr 139:230–237
Jobgen W, Fu WJ, Gao H et al (2009b) High fat feeding and dietary l-arginine supplementation differentially regulate gene expression in rat white adipose tissue. Amino Acids 37:187–198
Kayacelebi AA, Willers J, Pham VV et al (2015) Plasma homoarginine, arginine, asymmetric dimethylarginine and total homocysteine interrelationships in rheumatoid arthritis, coronary artery disease and peripheral artery occlusion disease. Amino Acids. doi:10.1007/s00726-015-1915-3
Khalil AA, Tsikas D, Akolekar R et al (2013) Asymmetric dimethylarginine, arginine and homoarginine at 11–13 weeks’ gestation and preeclampsia: a case-control study. J Hum Hypertens 27:38–43
Kohli R, Meininger CJ, Haynes TE et al (2004) Dietary l-arginine supplementation enhances endothelial nitric oxide synthesis in streptozotocin-induced diabetic rats. J Nutr 134:600–608
Leiper J, Vallance P (1999) Biological significance of endogenous methylarginines that inhibit nitric oxide synthases. Cardiovasc Res 43:542–548
Li XL, Bazer FW, Johnson GA et al (2014) Dietary supplementation with l-arginine between days 14 and 25 of gestation enhances embryonic development and survival in gilts. Amino Acids 46:375–384
Lin CW, Fishman WH (1972) L-Homoarginine. An organ-specific, uncompetitive inhibitor of human liver and bone alkaline phosphohydrolases. J Biol Chem 247:3082–3087
Lucotti P, Setola E, Monti LD et al (2006) Beneficial effect of a long-term oral l-arginine treatment added to a hypocaloric diet and exercise training program in obese, insulin-resistant type 2 diabetic patients. Am J Physiol Endocrinol Metab 291:E906–E912
Mateo RD, Wu G, Bazer FW et al (2007) Dietary l-arginine supplementation enhances the reproductive performance of gilts. J Nutr 137:652–656
Mateo RD, Wu G, Moon HK et al (2008) Effects of dietary arginine supplementation during gestation and lactation on the performance of lactating primiparous sows and nursing piglets. J Anim Sci 86:827–835
McKnight JR, Satterfield MC, Jobgen WS et al (2010) Beneficial effects of l-arginine on reducing obesity: Potential mechanisms and important implications for human health. Amino Acids 39:349–357
McNeal C, Wu G, Vasquez S et al (2010) The role of arginine for treating obese youth. In: Bagchi D (ed) Global Perspectives on Childhood Obesity. Elsevier, New York, pp 433–442
Michel T (2013) R is for arginine: metabolism of arginine takes off again, in new directions. Circulation 128:1400–1404
Morris SM Jr (2007) Arginine metabolism: boundaries of our knowledge. J Nutr 137:1602S–1609S
Phang JM, Liu W (2012) Proline metabolism and cancer. Front Biosci (Landmark Ed) 17:1835–1845
Popolo A, Adesso S, Pinto A et al (2014) l-Arginine and its metabolites in kidney and cardiovascular disease. Amino Acids 46:2271–2286
Rhoads JM, Wu G (2009) Glutamine, arginine, and leucine signaling in the intestine. Amino Acids 37:111–122
Ryan WL, Wells IC (1964) Homocitrulline and homoarginine synthesis from lysine. Science 144:1122–1123
Ryan WL, Barak AJ, Johnson RJ (1968) Lysine, homocitrulline, and homoarginine metabolism by the isolated perfused rat liver. Arch Biochem Biophys 123:294–297
Ryan WL, Johnson RJ, Dimari S (1969) Homoarginine synthesis by rat kidney. Arch Biochem Biophys 131:521–526
San Gabriel A, Uneyama H (2013) Amino acid sensing in the gastrointestinal tract. Amino Acids 45:451–461
Satterfield MC, Dunlap KA, Keisler DH et al (2012) Arginine nutrition and fetal brown adipose tissue development in diet-induced obese sheep. Amino Acids 43:1593–1603
Satterfield MC, Dunlap KA, Keisler DH et al (2013) Arginine nutrition and fetal brown adipose tissue development in nutrient-restricted sheep. Amino Acids 45:489–499
Schulman SP, Becker LC, Kass DA et al (2006) l-Arginine therapy in acute myocardial infarction: the Vascular Interaction With Age in Myocardial Infarction (VINTAGE) randomized clinical trial. JAMA 295:58–64
Shao A, Hathcock JN (2008) Risk assessment for the amino acids taurine, l-glutamine and l-arginine. Regul Toxicol Pharmacol 50:376–399
Shi W, Meininger CJ, Haynes TE et al (2004) Regulation of tetrahydrobiopterin synthesis and bioavailability in endothelial cells. Cell Biochem Biophys 41:415–433
Tekwe CD, Lei J, Yao K et al (2013) Oral administration of interferon tau enhances oxidation of energy substrates and reduces adiposity in Zucker diabetic fatty rats. Biofactors 39:552–563
Tsikas D, Kayacelebi AA (2014) Do homoarginine and asymmetric dimethylarginine act antagonistically in the cardiovascular system? Circ J 78:2094–2095
Tsikas D, Böger RH, Sandmann J et al (2000) Endogenous nitric oxide synthase inhibitors are responsible for the l-arginine paradox. FEBS Lett 478:1–3
Tsubuku S, Hatayama K, Mawatari K et al (2004) Thirteen-week oral toxicity study of l-arginine in rats. Int J Toxicol 23:101–105
Wu G (1995a) Nitric oxide synthesis and the effect of aminoguanidine and NG-monomethyl-l-arginine on the onset of diabetes in the spontaneously diabetic BB rat. Diabetes 44:360–364
Wu G (1995b) Urea synthesis in enterocytes of developing pigs. Biochem J 312:717–723
Wu G (1997) Synthesis of citrulline and arginine from proline in enterocytes of postnatal pigs. Am J Physiol Gastrointest Liver Physiol 272:G1382–G1390
Wu G (2013) Amino acids: biochemistry and nutrition. CRC Press, Boca Raton
Wu G (2014) Dietary requirements of synthesizable amino acids by animals: A paradigm shift in protein nutrition. J Anim Sci Biotechnol 5:34
Wu G, Meininger CJ (2008) Analysis of citrulline, arginine, and methylarginines using high-performance liquid chromatography. Methods Enzymol 440:177–189
Wu G, Meininger CJ (2009) Nitric oxide and vascular insulin resistance. Biofactors 35:21–27
Wu G, Morris SM Jr (1998) Arginine metabolism: nitric oxide and beyond. Biochem J 336:1–17
Wu G, Knabe DA, Flynn NE (1994) Synthesis of citrulline from glutamine in pig enterocytes. Biochem J 299:115–121
Wu G, Ott TL, Knabe DA et al (1999) Amino acid composition of the fetal pig. J Nutr 129:1031–1038
Wu G, Haynes TE, Li H et al (2000) Glutamine metabolism in endothelial cells: ornithine synthesis from glutamine via pyrroline-5-carboxylate synthase. Comp Biochem Physiol A 126:115–123
Wu G, Bazer FW, Cudd TA et al (2007a) Pharmacokinetics and safety of arginine supplementation in animals. J Nutr 137:1673S–1680S
Wu G, Collins JK, Perkins-Veazie P et al (2007b) Dietary supplementation with watermelon pomace juice enhances arginine availability and ameliorates the metabolic syndrome in Zucker diabetic fatty rats. J Nutr 137:2680–2685
Wu G, Bazer FW, Davis TA et al (2009) Arginine metabolism and nutrition in growth, health and disease. Amino Acids 37:153–168
Wu ZL, Satterfield MC, Bazer FW, Wu G (2012) Regulation of brown adipose tissue development and white fat reduction by l-arginine. Curr Opin Clin Nutr Metab Care 15:529–538
Wu G, Bazer FW, Satterfield MC et al (2013) Impacts of arginine nutrition on embryonic and fetal development in mammals. Amino Acids 45:241–256
Yang Y, Wu ZL, Meininger CJ et al (2015) l-Leucine and NO-mediated cardiovascular function. Amino Acids 47:435–447
Yao K, Yin YL, Chu WY et al (2008) Dietary arginine supplementation increases mTOR signaling activity in skeletal muscle of neonatal pigs. J Nutr 138:867–872
Acknowledgments
This research was supported by a grant from the International Council of Amino Acid Science (Brussels, Belgium). We thank our graduate students and technicians for assistance in this work. Ying Yang was supported by a Fellowship from the China Scholarship Council.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The use of animals for this research was approved by the Institutional Animal Care and Use Committee of Texas A&M University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, Y., Wu, Z., Jia, S. et al. Safety of long-term dietary supplementation with l-arginine in rats. Amino Acids 47, 1909–1920 (2015). https://doi.org/10.1007/s00726-015-1992-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-015-1992-3