Abstract
Increased cardiovascular risk associated with obesity cannot be fully explained by traditional risk markers. We therefore assessed plasma and interstitial concentrations of the novel cardiovascular risk biomarker homoarginine (hArg) in 18 individuals without signs of cardiovascular disease, including 4 morbidly obese subjects before and after bariatric surgery and subsequent weight reduction of 36 ± 7 kg. hArg concentrations were greater in skeletal muscle compared with adipose tissue. Plasma and tissue hArg concentrations did not correlate with BMI. Adipose tissue interstitial hArg concentrations were not affected by obesity, an oral glucose load, or dramatic weight loss. In conclusion, obesity seems not to have a major effect on hArg homeostasis, and hArg may not explain the added cardiovascular risk associated with obesity. Yet, given the small sample size of the study, the significance of hArg in obesity should be investigated in a larger population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The l-arginine homologue L-homoarginine (hArg) is a non-essential, non-proteinogenic amino acid. l-Arginine plays multiple physiological roles in nutrition, growth, health and disease (Wu et al. 2009). A small portion of free l-arginine (<0.1 %) serves as the substrate for nitric oxide (NO) synthesis by nitric oxide synthase (NOS) isoforms. hArg may inhibit NOS activity (Bretscher et al. 2003; Moali et al. 1998, 2000), and low plasma hArg concentrations were recently associated with cardiovascular and all-cause mortality in humans (Choe et al. 2013a; Kayacelebi et al. 2014b; März et al. 2010; Pilz et al. 2011). Importantly, plasma concentrations of arginine, asymmetric dimethylarginine (ADMA), and hArg do not necessarily reflect intracellular concentrations (Davids et al. 2012; Davids and Teerlink 2013). Obesity is an important predictor of overall and cardiovascular mortality (Prospective Studies Collaboration et al. 2009). The role of hArg in obesity and insulin resistance has not yet been explored and interstitial hArg concentrations in major target organs of obesity-associated pathophysiology, adipose tissue and skeletal muscle, are unknown. Plasma hArg was found to correlate with BMI in different populations (Atzler et al. 2014a; Pilz et al. 2014). Moreover, hArg may stimulate insulin secretion (Henningsson and Lundquist 1998) and a correlation to HOMA-IR was seen (Atzler et al. 2014a; Pilz et al. 2014). l-Arginine:glycine amidinotransferase (AGAT) is responsible for the synthesis of hArg (Choe et al. 2013a), and AGAT deficiency protects against the metabolic syndrome in mice (Choe et al. 2013b).
The aim of the present study was to determine plasma and interstitial hArg concentrations in relation to body mass index (BMI) and obesity-associated insulin resistance in humans. Because ADMA inhibits NOS activity, while hArg may serve both as an inhibitor and as a substrate for NO synthesis, hArg and ADMA may act antagonistically in the cardiovascular system (Tsikas and Kayacelebi 2014). As the hArg-to-ADMA (hArg/ADMA) molar ratio in the circulation may better evaluate the relative effects of hArg and ADMA on cardiovascular diseases (Tsikas and Kayacelebi 2014), we also explored the ratio of hArg/ADMA in our study.
Materials and methods
Human studies
hArg was measured in 18 individuals: 10 healthy non-obese subjects from a previously reported dietary intervention study (Engeli et al. 2012), 4 obese subjects before and after bariatric surgery, and 4 healthy age-matched controls. There was no overlap between the study populations. BMI was calculated from the ratio of body weight (kg)/body height (m2) and subjects were classified according to WHO classification (WHO 2000). HOMA-IR was calculated with the formula: HOMA-IR = (glucose[mM] × insulin[mU/L])/22.5) to quantify insulin resistance (Matthews et al. 1985). Glucose and insulin were measured by standard procedures in a certified Clinical Chemistry laboratory. Individuals’ characteristics are listed in Table 1. In 10 healthy individuals, two of which were overweight, blood samples were taken after 2 weeks on an isocaloric reduced-fat diet in the fasting state. Subjects did not take any drugs and were weight-stable for at least 3 months prior to study participation. To determine interstitial hArg concentrations in subcutaneous adipose tissue and skeletal muscle by microdialysis (MD), we also studied four morbidly obese patients before and after substantial weight loss through bariatric surgery, as well as four healthy, non-obese, and age-matched individuals as controls. These participants were also subjected to oral glucose tolerance testing (75 g glucose in 300 mL water). We included only non-smokers without history of allergy, gastrointestinal, endocrinological or psychiatric disorders, and with normal blood pressure and electrocardiograms. MD catheters (CMA 60, CMA/µDialysis, Stockholm, Sweden) were inserted into abdominal subcutaneous adipose tissue and into the vastus lateralis muscle, and were connected to mini-pumps (CMA 107) as described elsewhere (May et al. 2013). After probe insertion, catheters were perfused at a flow rate of 1 µL/min with Ringer solution containing 50 mM ethanol (Fellander et al. 1996). After 30 min of equilibration, MD samples were collected every 15 min during 30 min baseline and 2 h glucose challenge as described elsewhere (May et al. 2014). MD samples were placed on ice after collection and stored at −80 °C until analysis. All subjects provided written informed consent prior to study participation. Study protocols were approved by the Ethics Committees of Charité University Medicine and Hannover Medical School (MD study).
Processing of biological samples
EDTA blood samples were centrifuged (1,500 × g, 4 °C, 15 min) and resulting plasma was analysed immediately or stored at –80 °C until analysis. Ultrafiltrates from 0.5-mL plasma aliquots were obtained by centrifugation (15,000 × g, 4 °C, 30 min) using Vivaspin 2 Hydrosart cartridges (cut-off 10 kDa; Sartorius, Göttingen, Germany). In 10-µL plasma aliquots, hArg, arginine and ADMA were derivatized first to their methyl esters using 2 M HCl in CH3OH for endogenous amino acids and 2 M HCl in CD3OD for the de novo synthesized trideutero (d3)-internal standards; then pentafluoropropionyl derivatives were produced (Kayacelebi et al. 2014a; Tsikas et al. 2003).
Chemicals
The hydrochloride salts of hArg, arginine and ADMA were purchased from Sigma (Deisenhofen, Germany). Pentafluoropropionic anhydride was obtained from Pierce (Rockford, IL, USA). CD3OD (99 % at 2H) was supplied by Aldrich (Steinheim, Germany). All other chemicals were obtained from Merck (Darmstadt, Germany).
Measurement of homoarginine and ADMA
hArg (Kayacelebi et al. 2014a) and ADMA (Tsikas et al. 2003) were measured in plasma and native MD samples by previously reported, fully-validated gas chromatography-tandem mass spectrometry (GC–MS/MS) methods using the triple-stage quadrupole mass spectrometer ThermoQuest TSQ 7000 (Finnigan MAT, San Jose, CA) directly interfaced with a Trace 2000 series gas chromatograph equipped with an autosampler AS 2000 (CE Instruments, Austin, TX). Other instrumental conditions were described elsewhere (Kayacelebi et al. 2014a; Tsikas et al. 2003). Quantification of hArg was performed by selected-reaction monitoring (SRM) of the mass transition m/z 600 → m/z 366 for hArg and m/z 603 → m/z 366 for the internal standard d3-hArg. Quantification of ADMA was performed by SRM of the mass transition m/z 634 → m/z 378 for ADMA and m/z 637 → m/z 378 for the internal standard d3-ADMA.
Statistical analysis
All data are shown as mean and standard error. Statistical analysis was performed using IBM SPSS Statistic 22. Intra-individual differences were compared by Students t test for paired or unpaired samples, as appropriate. ANOVA testing for repeated measures was used for multiple comparisons. Univariate correlation was calculated by the method of Pearson. In all analyses, P < 0.05 was considered to be statistically significant.
Results
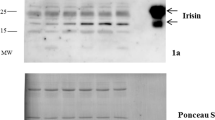
The plasma hArg concentrations measured in the present study are within the range reported for healthy humans, Plasma hArg concentration and BMI were not correlated in the healthy individuals examined after 2 weeks on reduced-fat diet (n = 10; r 2 = 0.02; P = 0.73). The same was true for the correlation between hArg/ADMA ratio and BMI (r 2 = 0.0; P = 0.95) (Fig. 1a). However, when looking only at the seven subjects within the normal BMI range (18.5–25 kg/m2), we found a strong correlation between BMI and plasma hArg (r 2 = 0.8; P = 0.006), as well as between BMI and the hArg/ADMA ratio (r 2 = 0.82; P = 0.005). Furthermore, plasma hArg concentrations did not differ between lean individuals and morbidly obese patients before weight loss (1.74 ± 0.25 vs. 1.97 ± 0.36 µM; n = 4 each) in the second set of the studied individuals. Mean weight loss of 36 ± 7 kg over 6 months had no influence on hArg plasma concentration (1.97 ± 0.36 vs. 2.02 ± 0.26 µM; n = 4). When combining all data sets (n = 18), no correlation between plasma hArg and BMI was observed, but the correlation within the normal BMI range (n = 9) persisted. A correlation between plasma hArg and HOMA-IR was not found, despite significant HOMA-IR differences between lean and obese subjects (P < 0.01) and a trend to lower HOMA-IR indices after massive weight reduction (P = 0.1).
a Correlation of plasma hArg and ADMA with BMI in individuals after 2 weeks of reduced-fat diet (n = 10). b Adipose tissue and skeletal muscle interstitial hArg and ADMA concentrations in lean individuals (n = 4) during an oral glucose tolerance test. c Interstitial hArg and ADMA concentrations during an oral glucose tolerance test in healthy individuals and in morbidly obese patients before and after massive weight reduction. d Changes of interstitial glucose concentration from mean baseline values during an oral glucose load in healthy individuals and in morbidly obese patients before and after massive weight reduction
Plasma values of homoarginine did not correlate to adipose tissue homoarginine values but tended to correlate to skeletal muscle homoarginine (r 2 = 0.2; P = 0.7 and r 2 = 0.7; P = 0.1 respectively). Interstitial hArg (1.25 ± 0.21 vs. 0.75 ± 0.16 µM, P = 0.02) and ADMA concentrations (0.27 ± 0.02 vs. 0.17 ± 0.03 µM, P = 0.02) in skeletal muscle were significantly higher compared to adipose tissue in four lean subjects (Fig. 1b). The hArg/ADMA ratio did not differ between skeletal muscle and adipose tissue (4.4 ± 0.8 vs. 4.8 ± 1.0, P = 0.09). Oral glucose challenge did not change skeletal and adipose tissue hArg and ADMA concentrations (Fig. 1b). When comparing adipose tissue interstitial hArg concentrations between lean and morbidly obese subjects (n = 4 each, Fig. 1c), we observed significantly higher hArg concentrations in lean subjects (0.75 ± 0.16 vs. 0.39 ± 0.03 µM; P = 0.03; each n = 4), whereas interstitial ADMA concentrations were similar (0.17 ± 0.03 vs. 0.15 ± 0.02 µM; P = 0.3). The hArg/ADMA ratio was about four in lean individuals and about three in obese patients. Massive weight loss did not affect interstitial hArg and ADMA concentrations in adipose tissue (Fig. 1c). During an oral glucose challenge, interstitial adipose tissue hArg and ADMA concentrations did not change upon oral administration of glucose, unlike the interstitial glucose concentrations (Fig. 1c, d).
Discussion
This is the first study reporting interstitial hArg concentrations assessed by serial MD sampling and GC–MS/MS analysis in human subjects. hArg is a naturally occurring amino acid derived from lysine (Ryan and Wells 1964) and may be involved in the NOS-catalysed generation of the vasodilator NO (Valtonen et al. 2008), as well as in the inhibition NOS activity (Bretscher et al. 2003; Moali et al. 1998, 2000). hArg can be formed through reactions homologous to those of the urea cycle (März et al. 2010). Furthermore, hArg generation is catalysed by AGAT (Choe et al. 2013a; Kleber et al. 2003), which is the rate limiting enzyme in skeletal muscle creatinine synthesis (Wyss and Kaddurah-Daouk 2000). AGAT seems to protect against the metabolic syndrome in mice (Choe et al. 2013b). Previously, we demonstrated that adipose tissue ADMA does not play a major role in NO-dependent regulation of adipose tissue blood flow and metabolism, and is not subject to regulation by glucose challenges in humans (May et al. 2014). Our current study extends this finding to hArg, because rapid increases in plasma and tissue glucose concentrations did not elicit significant increases in tissue hArg concentrations. Glucose and the associated increase in insulin therefore appear not to play a major role in hArg biosynthesis or degradation.
Larger population-based studies have found a positive correlation between hArg and BMI or HOMA-IR (Atzler et al. 2014a; Pilz et al. 2014). In our admittedly small study cohort, plasma hArg concentrations did not differ between lean and obese individuals, and only in subjects within the normal BMI range plasma hArg correlated with BMI. Furthermore, despite lower HOMA-IR indices after weight reduction and significant differences in HOMA-IR between the examined study groups, hArg and HOMA-IR did not correlate at all. The lack of correlation might be accounted to the small sample size of our study, especially when the small differences seen in larger population studies are considered (Atzler et al. 2014a; Pilz et al. 2014). Nevertheless, a significant negative correlation between plasma ADMA and weight reduction was observed in only 29 patients after bariatric surgery, with a decrease of 45 % in patients after 18 kg weight loss (Patle et al. 2012). Despite a larger mean weight reduction in our study (36 ± 7 kg), we did not observe significant changes in our 4 morbidly obese subjects. However, plasma hArg is higher in men compared to women (Pilz et al. 2014), which might have biassed our results as our study populations were not equally distributed with regard to gender.
Interstitial adipose tissue hArg concentrations were about two times higher in lean individuals compared to morbidly obese patients, but substantial weight loss did not change hArg concentrations, neither in plasma nor in adipose tissue. Interstitial hArg concentrations in healthy subjects were two-fold higher in skeletal muscle compared to adipose tissue, which might reflect the mentioned connection to creatinine metabolism (Choe et al. 2013a). However, MD results are depending on the recovery rate of the targeted molecule, and recovery rates are influenced by local blood flow (Plock and Kloft 2005) which is higher in skeletal muscle than in adipose tissue, even under resting conditions. Thus, differences in MD results for hArg between skeletal muscle and adipose tissue are possibly explained by different MD recovery rates. The same may be true for the difference in adipose tissue hArg between groups, as adipose tissue blood flow is inversely related to adiposity.
Low plasma and serum hArg concentrations are supposed to be associated with cardiovascular morbidity and mortality (Atzler et al. 2014b; Choe et al. 2013a; Drechsler et al. 2013; Tomaschitz et al. 2014). This was recently confirmed in two large population-based studies (Atzler et al. 2014a; Pilz et al. 2014). Low hArg concentrations were also detected in plasma of male smokers compared to male non-smokers, both groups being without overt cardiovascular disease (Sobczak et al. 2014a). In the same study, smoking was associated with higher ADMA plasma concentrations (Sobczak et al. 2014a). We hypothesized that the hArg/ADMA molar ratio rather than the individual circulating concentrations of hArg and ADMA would be more useful to improve cardiovascular disease risk prediction (Tsikas and Kayacelebi 2014). In accordance with this proposal, cardiovascular disease risk would be the higher, the lower the hArg/ADMA would be. Thus, healthy smokers with a hArg/ADMA ratio of 5.7 would have a higher cardiovascular disease risk than non-smokers with a hArg/ADMA ratio of 4.2 (Tsikas and Kayacelebi 2014; Sobczak et al. 2014b). Higher circulating hArg concentrations were measured in normal pregnancy and in preeclampsia, while circulating ADMA concentrations are rather normal (Khalil et al. 2013; Valtonen et al. 2008). Based on these reports and since obesity is an important cardiovascular risk factor, we reasoned that plasma hArg concentrations could be lower in obese subjects. The results of the present study argue against this assumption. However, we acknowledge the small sample size and the preliminary nature of our study, which are major limitations of our study. Evaluation of hArg and ADMA in a sufficiently large population of obese and lean individuals is warranted. In the present study we report for the first time interstitial concentrations for hArg, and ADMA and their hArg/ADMA ratio which was lower in morbidly obese subjects compared to healthy subjects (i.e., about 3 vs. 4). Yet, the significance of the interstitial hArg/ADMA ratio as a predictor of cardiovascular risk also remains to be evaluated in larger populations.
Abbreviations
- ADMA:
-
N G,N G-Dimethyl-l-arginine
- BMI:
-
Body mass index
- hArg:
-
L-Homoarginine
- HOMA-IR:
-
Homeostasis model assessment-insulin resistance (index)
- MD:
-
Microdialysis
- NO:
-
Nitric oxide
- NOS:
-
Nitric oxide synthase
- SRM:
-
Selected-reaction monitoring
References
Atzler D, Gore MO, Ayers CR, Choe CU, Böger RH, de Lemos JA, McGuire DK, Schwedhelm E (2014a) Homoarginine and cardiovascular outcome in the population-based Dallas Heart Study. Arterioscler Thromb Vasc Biol 34:2501–2507
Atzler D, Schwedhelm E, Nauck M, Ittermann T, Böger RH, Friedrich N (2014b) Serum reference intervals of homoarginine, ADMA, and SDMA in the Study of Health in Pomerania. Clin Chem Lab Med 52:1835–1842
Bretscher LE, Li H, Poulos TL, Griffith OW (2003) Structural characterization and kinetics of nitric-oxide synthase inhibition by novel N5-(iminoalkyl)- and N5- (iminoalkenyl)-ornithines. J Biol Chem 278:46789–46797
Choe CU, Atzler D, Wild PS, Carter AM, Böger RH, Ojeda F, Simova O, Stockebrand M, Lackner K, Nabuurs C, Marescau B, Streichert T, Muller C, Luneburg N, De Deyn PP, Benndorf RA, Baldus S, Gerloff C, Blankenberg S, Heerschap A, Grant PJ, Magnus T, Zeller T, Isbrandt D, Schwedhelm E (2013a) Homoarginine levels are regulated by l-arginine:glycine amidinotransferase and affect stroke outcome: results from human and murine studies. Circulation 128:1451–1461
Choe CU, Nabuurs C, Stockebrand MC, Neu A, Nunes P, Morellini F, Sauter K, Schillemeit S, Hermans-Borgmeyer I, Marescau B, Heerschap A, Isbrandt D (2013b) l-arginine:glycine amidinotransferase deficiency protects from metabolic syndrome. Hum Mol Genet 22:110–123
Collaboration Prospective Studies, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R (2009) Body-mass index and cause-specific mortality in 900000 adults: collaborative analyses of 57 prospective studies. Lancet 373:1083–1096
Davids M, Teerlink T (2013) Plasma concentrations of arginine and asymmetric dimethylarginine do not reflect their intracellular concentrations in peripheral blood mononuclear cells. Metab Clin Exp 62:1455–1461
Davids M, Ndika JD, Salomons GS, Blom HJ, Teerlink T (2012) Promiscuous activity of arginine:glycine amidinotransferase is responsible for the synthesis of the novel cardiovascular risk factor homoarginine. FEBS Lett 586:3653–3657
Drechsler C, Kollerits B, Meinitzer A, März W, Ritz E, König P, Neyer U, Pilz S, Wanner C, Kronenberg F (2013) Homoarginine and progression of chronic kidney disease: results from the mild to moderate kidney disease study. PLoS One 8:e63560
Engeli S, Tsikas D, Lehmann AC, Böhnke J, Haas V, Strauß A, Janke J, Gorzelniak K, Luft FC, Jordan J (2012) Influence of dietary fat ingestion on asymmetrical dimethylarginine in lean and obese human subjects. Nutr Metab Cardiovasc Dis 22:720–726
Fellander G, Linde B, Bolinder J (1996) Evaluation of the microdialysis ethanol technique for monitoring of subcutaneous adipose tissue blood flow in humans. Int J Obes Relat Metab Disord 20:220–226
Henningsson R, Lundquist I (1998) Arginine-induced insulin release is decreased and glucagon increased in parallel with islet NO production. Am J Physiol 275:E500–E506
Kayacelebi AA, Beckmann B, Gutzki FM, Jordan J, Tsikas D (2014a) GC-MS and GC-MS/MS measurement of the cardiovascular risk factor homoarginine in biological samples. Amino Acids 46:2205–2217
Kayacelebi AA, Nguyen TH, Neil C, Horowitz JD, Jordan J, Tsikas D (2014b) Homoarginine and 3-nitrotyrosine in patients with takotsubo cardiomyopathy. Int J Cardiol 173:546–547
Khalil AA, Tsikas D, Akolekar R, Jordan J, Nicolaides KH (2013) Asymmetric dimethylarginine, arginine and homoarginine at 11-13 weeks’ gestation and preeclampsia: a case-control study. J Hum Hypertens 27:38–43
Kleber ME, Seppälä I, Pilz S, Hoffmann MM, Tomaschitz A, Oksala N, Raitoharju E, Lyytikäinen LP, Mäkelä KM, Laaksonen R, Kähönen M, Raitakari OT, Huang J, Kienreich K, Fahrleitner-Pammer A, Drechsler C, Krane V, Boehm BO, Koenig W, Wanner C, Lehtimäki T, März W, Meinitzer A (2003) Circ Cardiovasc Genet 6:505–513
März W, Meinitzer A, Drechsler C, Pilz S, Krane V, Kleber ME, Fischer J, Winkelmann BR, Böhm BO, Ritz E, Wanner C (2010) Homoarginine, cardiovascular risk, and mortality. Circulation 122:967–975
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
May M, Batkai S, Zoerner AA, Tsikas D, Jordan J, Engeli S (2013) Enhanced human tissue microdialysis using hydroxypropyl-ss-cyclodextrin as molecular carrier. PLoS One 8:e60628
May M, Ahrens J, Menne J, Haller H, Beige J, Eckert S, Jordan J, Engeli S (2014) Limited acute influences of electrical baroreceptor activation on insulin sensitivity and glucose delivery: a randomized, double-blind, cross-over clinical study. Diabetes 63:2833–2837
Moali C, Boucher JL, Sari MA, Stuehr DJ, Mansuy D (1998) Substrate specificity of NO synthases: detailed comparison of l-arginine, homo-L-arginine, their N omega-hydroxy derivatives, and N omega-hydroxynor-L-arginine. Biochemistry 37:10453–10460
Moali C, Brollo M, Custot J, Sari MA, Boucher JL, Stuehr DJ, Mansuy D (2000) Recognition of alpha-amino acids bearing various C = NOH functions by nitric oxide synthase and arginase involves very different structural determinants. Biochemistry 39:8208–8218
Patle R, Dubb S, Alaghband-Zadeh J, Sherwood RA, Tam F, Frankel A, Moniz C, Bueter M, Vincent RP, le Roux CW (2012) Improved blood pressure, nitric oxide and asymmetric dimethylarginine are independent after bariatric surgery. Ann Clin Biochem 49:589–594
Pilz S, Tomaschitz A, Meinitzer A, Drechsler C, Ritz E, Krane V, Wanner C, Bohm BO, März W (2011) Low serum homoarginine is a novel risk factor for fatal strokes in patients undergoing coronary angiography. Stroke 42:1132–1134
Pilz S, Teerlink T, Scheffer PG, Meinitzer A, Rutters F, Tomaschitz A, Drechsler C, Kienreich K, Nijpels G, Stehouwer CD, März W, Dekker JM (2014) Homoarginine and mortality in an older population: the Hoorn study. Eur J Clin Invest 44:200–208
Plock N, Kloft C (2005) Microdialysis–theoretical background and recent implementation in applied life-sciences. Eur J Pharm Sci 25:1–24
Ryan WL, Wells IC (1964) Homocitrulline and homoarginine synthesis from lysine. Science 144:1122–1127
Sobczak A, Prokopowicz A, Radek M, Szula M, Zaciera M, Kurek J, Goniewicz ML (2014a) Tobacco smoking decreases plasma concentration of the emerging cardiovascular risk marker, L-homoarginine. Circ J 78:1254–1258
Sobczak A, Prokopowicz A, Radek M, Szula M, Zaciera M, Kurek J, Goniewicz ML (2014b) Do homoarginine and asymmetric dimethylarginine act antagonistically in the cardiovascular system? Circ J 78:2096
Tomaschitz A, Meinitzer A, Pilz S, Rus-Machan J, Genser B, Drechsler C, Grammer T, Krane V, Ritz E, Kleber ME, Pieske B, Kraigher-Krainer E, Fahrleitner-Pammer A, Wanner C, Boehm BO, März W (2014) Homoarginine, kidney function and cardiovascular mortality risk. Nephrol Dial Transplant 29:663–671
Tsikas D, Kayacelebi AA (2014) Do homoarginine and asymmetric dimethylarginine act antagonistically in the cardiovascular system? Circ J 78:2094–2095
Tsikas D, Schubert B, Gutzki FM, Sandmann J, Frölich JC (2003) Quantitative determination of circulating and urinary asymmetric dimethylarginine (ADMA) in humans by gas chromatography-tandem mass spectrometry as methyl ester tri(N-pentafluoropropionyl) derivative. J Chromatogr B 798:87–99
Valtonen P, Laitinen T, Lyyra-Laitinen T, Raitakari OT, Juonala M, Viikari JS, Heiskanen N, Vanninen E, Punnonen K, Heinonen S (2008) Serum L-homoarginine concentration is elevated during normal pregnancy and is related to flow-mediated vasodilatation. Circ J 72:1879–1884
WHO (2000) Obesity: preventing and managing the global epidemic, Report of a WHO consultation. World Health Organ Tech Rep Ser 894(i–xii):1–253
Wu G, Bazer FW, Davis TA, Kim SW, Li P, Marc Rhoads J, Carey Satterfield M, Smith SB, Spencer TE, Yin Y (2009) Arginine metabolism and nutrition in growth, health and disease. Amino Acids 37:153–168
Wyss M, Kaddurah-Daouk R (2000) Creatine and creatinine metabolism. Physiol Rev 80:1107–1213
Acknowledgments
The laboratory assistance of Bibiana Beckmann, Anja Mitschke and Maria-Theresia Suchy is gratefully acknowledged. We thank Frank-Mathias Gutzki for performing GC–MS/MS analyses of homoarginine and ADMA in plasma and microdialysate samples.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
May, M., Kayacelebi, A.A., Batkai, S. et al. Plasma and tissue homoarginine concentrations in healthy and obese humans. Amino Acids 47, 1847–1852 (2015). https://doi.org/10.1007/s00726-015-1922-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-015-1922-4