Abstract
Three historical phenobarbital-containing pharmaceutical preparations with an age of 36–57 years from the date of manufacture were analyzed. The analyzed preparations also differed in the type of dosage form: dragée, suppository, and solution. The aim was to evaluate the long-term stability of phenobarbital, within the systematic program aimed at studying the stability and degradation of active pharmaceutical ingredients in decades-old pharmaceutical products. The substances contained in the analyzed preparations were identified by reverse-phase HPLC with UV and high-resolution mass spectrometric detection, capillary zone electrolysis, and head-space solid-phase microextraction followed by GC–MS. The content of the main active ingredients was determined and compared with the values declared by the manufacturer. No degradation of phenobarbital was found in two preparations, dragée “Sedobelin” and suppository “Spasmoveralgin,” so phenobarbital is stable in these preparations even after 36, respectively 43, years since the production of a preparation. In contrast, two degradation products were identified in the 57-year-old solution “Sklerophyllin”: pheneturide and 3-aminopentanoic acid. The originally declared amount of phenobarbital was found to decrease by 12.5%. Thus, it is clear that phenobarbital is stable for many decades in solid dosage forms, whereas in liquid dosage forms it is partially degraded. In the second part of the work, ESI high-resolution mass spectra of four selected substances were interpreted: phenobarbital, pheneturide, 3-aminopentanoic acid, and 3,4-methylenedioxymethamphetamine. The latter substance was surprisingly found in the suppository “Spasmoveralgin,” probably as a degradation product of ephedrine contained in the product.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
For the purpose of establishing the shelf life of pharmaceutical products, the stability of their active ingredients is generally studied in the range of 1–5 years [1]. However, in recent years, the possibility of prolonging the shelf life of pharmaceutical products has been widely discussed, as it has significant economic [2,3,4], environmental [5], and also ethical impacts [6, 7]. The stability of the active ingredient of a pharmaceutical preparation generally depends both on its chemical structure and the dosage form used [8, 9]. This is because the active ingredient may be subject to a variety of degradation reactions, given both the chemical structure of the ingredient itself and other natural active substances or excipients that together form a particular dosage form.
In this work, we present the study of the long-term stability of phenobarbital in three different dosage forms, which were older than 36 years at the time of analysis. It is part of our systematic program aimed at studying the stability and degradation of active pharmaceutical ingredients in decades-old pharmaceutical products [10]. In this program, we studied the degradation of heroin and cocaine [11], quinine [12], ouabain [13], neosalvarsan [14], and several alkaloids [9] in various dosage forms.
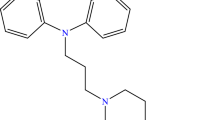
Phenobarbital (Fig. 1, CASRN [50-06-6]) is an important representative of barbiturates, drugs introduced into therapy in 1904 [15]. The parent compound of barbiturates, the barbituric acid itself, was synthesized by the famous German chemist Adolf von Bayer in 1864 [16]. In 1903, the German physician Joseph von Mering and the German chemist Emil Fischer discovered that 5,5-diethylbarbituric acid was hypnotic to animals [15]. Under the trade name Veronal, the substance was put into practice a year later. Phenobarbital was synthesized in 1911 by Fischer’s collaborator Heinrich Hörlein, as one of the results of the systematic preparation of new barbiturates. One year later, it was marketed under the trade name Luminal. Phenobarbital exhibited a more prolonged pharmacological action than its predecessors, and soon became the “king of barbiturates” and opened the way to another important therapeutic application of barbiturates. In February 1912, the German physician Alfred Hauptmann discovered that phenobarbital significantly helps in the treatment of epileptic seizures [17]. Although today it is rarely used for sedative and hypnotic effects, phenobarbital remains the oldest antiseizure medication still widely used and is still on the World Health Organization’s List of Essential Medicines [18].
The phenobarbital stability has been studied by a number of authors under various conditions. As early as 1927, Steenhauer [19] discovered the thermal instability of phenobarbital solutions when heated to 100 °C during autoclaving of injectable solutions, leading to the formation of a substituted acetylurea derivative and carbon dioxide. According to Colombo et al. [20], this degradation can be suppressed by adding 28% glycerol and 10% ethanol to the solution. In 1949, Dunker [21] found that the decomposition of phenobarbital aqueous solutions occurs in the alkaline region (pH = 9.2–10.8), even at room temperature. Pheneturide (Fig. 1, CASRN [90-49-3]) was identified as the major degradation product. The detailed mechanism of phenobarbital degradation has been studied by several authors [22,23,24,25], and it was found that its hydrolysis occurs in the pH range of 6.01 to 12.05 and results in the opening of the ring and formation of two main degradation products. For the non-ionized form of barbiturate, the ring opens at the 1,2- or equivalent 2,3-position to yield a substituted diamide. However, for ionized barbiturate, the ring opens at the 1,6- or equivalent 3,4-position to produce a substituted acetylurea derivative. This is consistent with the findings of Dietz et al. [26], who demonstrated that phenobarbital is stable in an elixir, an emulsion, and a propylene glycol solution for 56 weeks. On the contrary, in the aqueous solution of pH = 8, the phenobarbital concentration decreased to 76%. The long-term stability of phenobarbital was investigated by Cantrell et al. [5], who measured the content of phenobarbital in tablets, which expired 28 years before the analysis. They found 94% of the declared amount; it can be caused by both degradation and manufacturing error. With the exception of this single publication, no information on the long-term stability of phenobarbital is known.
For our analysis, we had three samples of historical pharmaceutical products containing phenobarbital as the main active ingredient (Fig. 2). The first specimen was representative of solid dosage forms. It was “Sedobelin” dragées, manufactured by the company Spofa (former Czechoslovakia) in 1978, so 43 years have passed since its production at the time of analysis. The declared content of one dragée was: 50 mg phenobarbital, 20 mg papaverine hydrochloride, 0.25 mg radobelin (a mixture of belladonna alkaloids, especially atropine), and 100 mg extractum crataegi (hawthorn leaf extract, the main components of which are procyanidin and hyperoside). The product was used to treat spastic conditions, especially asthma and cholestasis. It was introduced into therapy in 1942 by the company Eko (former Czechoslovakia); the product is no longer manufactured.
The second analyzed pharmaceutical product, the suppositories “Spasmoveralgin,” was representative of semisolid dosage forms. The product was manufactured by the company Spofa (former Czechoslovakia) in 1985, so 36 years have passed since its production at the time of analysis. The declared content of a suppository was: 300 mg bromisoval, 200 mg aminophenazone, 50 mg caffeine, 25 mg phenobarbital, 25 mg papaverine hydrochloride, 15 mg codeine dihydrogen phosphate, 5 mg ephedrine hydrochloride, and 0.5 mg atropine methyl bromide. The product was used to treat spastic conditions and pain and was introduced into use by the company Spolek pro chemickou a hutní výrobu (former Czechoslovakia) in 1949; at present, it is no longer manufactured.
The “Sklerophyllin” solution was the oldest analyzed pharmaceutical product and belonged to liquid dosage forms. It was introduced into therapy in 1938 by the company Interpharma (former Czechoslovakia), later production was taken over by Galena (former Czechoslovakia), and the manufacture was ceased in 1964. The analyzed sample was therefore at least 57 years old at the time of analysis (the exact date of production could not be determined for the missing lot number). The declared content in 200 cm3 of solution was: 300 mg methacholine bromide, 400 mg theophylline, 200 mg phenobarbital, and 200 mg sodium iodide. The solution also contains a chlorophyll-based dye, known in the literature as chlorophyllinpurin [27], with a concentration of 1 mg cm−3. As indicated on the bottle label, some excipients are not explicitly listed by the manufacturer. The product was used to treat arteriosclerosis, high blood pressure, and to relieve symptoms of senescence.
Results and discussion
Study of the composition of analyzed preparations
The composition of the analyzed historical phenobarbital-containing pharmaceutical products was studied by RP-HPLC with UV and high-resolution tandem mass spectrometry (HRMS2) detection. Because all three analyzed preparations are multicomponent with a content of tens to hundreds of milligrams, two different methods were used for the separation of individual components of the analyzed preparations on the basis of the literature. For both methods, the gradient programs and the flow rate of the mobile phase were subsequently adapted by monitoring changes in the peak retention times and the resolution of consecutive peaks. For the separation of the analytes, a Supelcosil™ LC-18 (250 × 4.5 mm, 5 μm) column was used for all three analyzed preparations.
For the analysis of the preparation “Sedobelin,” or “Spasmoveralgin,” gradient elution, hereinafter referred to as Gradient I, was selected on the basis of the literature [28, 29] and appropriately adjusted. The binary mobile phase consisting of aqueous 20 × 10–3 mol dm−3 acetate buffer (CH3COOH/CH3COONH4) of pH = 3.50 (solvent A) and acetonitrile (solvent B) was used with a flow rate of 1.0 cm3 min−1. The adapted gradient program started with 70% of A which was maintained constant for 7.5 min, then linearly decreased to 55% of A within 8.5 min, then linearly decreased to 10% of A within 6 min, then maintained constant for 2 min, then linearly increased to 70% of A within 2 min, and finally maintained constant for 4 min; the total analysis time was 30 min.
For the analysis of the preparation “Sklerophyllin,” gradient elution, hereinafter referred to as Gradient II, was selected on the basis of the literature [30, 31] and appropriately adjusted. The binary mobile phase consisted of aqueous 10–2 mol dm−3 acetate buffer (CH3COOH/CH3COONH4) of pH = 2.50 (solvent A) and methanol (solvent B), and the flow rate was 1.0 cm3 min−1. The adapted gradient program started with 75% of A which was maintained constant for 8 min, then linearly decreased to 45% of A within 8 min and then maintained constant for 1 min, then increased to 75% of A within 1 min and finally maintained constant for 12 min; thus, the total analysis time was 30 min.
The identification of substances in the analyzed pharmaceutical preparations was based on HRMS2 measurements and comparison of the spectra obtained with the spectra of the standards (for most of the substances identified) and, at the same time, with data from the literature. An overview of the substances found and identified is given in Table 1. The representative chromatogram of the analysis of the preparation “Sklerophyllin” is shown in Fig. 3. It is obvious that the separation of the compounds is satisfactory; the tailing peak of β-methylcholine is the result of the high concentration of this substance in the analyzed preparation.
HPLC analysis of the preparation “Sklerophyllin” (a) chromatogram with UV detection at 280 nm, (b) extracted ion chromatogram with ESI in positive mode, (c) extracted ion chromatogram with ESI in negative mode at m/z = 231.0777. Identification of the substances: 1 3-aminopentanoic acid, 2 theophylline, 3 β-methylcholine, 4 phenobarbital, 5 ethyl 4-hydroxybenzoate, 6 green colorant, 7 pheneturide, 8 O-acetyl-β-methylcholine. Measurement conditions: Supelcosil™ LC-18 (250 × 4.5 mm, 5 μm) column, gradient elution with aqueous 10–2 mol dm−3 acetate buffer of pH = 2.50 and methanol (for details see text, Gradient II), and flow rate 1.0 cm3 min−1
Selected components (especially main active ingredients) were quantified mainly by HPLC–MS based on calibration dependences constructed from peak areas. Because the determination of aminophenazone was not possible from HPLC measurements (its peak was tailing), a spectrophotometric method based on reaction with phosphomolybdic acid [49] was used for its quantification in “Spasmoveralgin” preparation. The determination of inorganic ions in “Sklerophyllin” preparation was performed by capillary zone electrophoresis (CZE). The determination of ethanol in the “Sklerophyllin” preparation was performed by head-space solid-phase microextraction followed by GC–MS (SPME–GC–MS). Table 2 provides an overview of the results of the determination of selected substances and their comparison with the content declared by the manufacturer (if possible).
The analysis of the “Sedobelin” preparation identified, in addition to the declared substances, quinic acid, whose source is the hawthorn leaf extract contained in the preparation [50], and sucrose, a common excipient in the production of dragée. No phenobarbital degradation product was found. The determination of the main active ingredients in the preparation showed that the phenobarbital content found was 48% higher than declared by the manufacturer. A probable explanation is a manufacturing error since the papaverine content practically corresponds to the declared amount. In this case, phenobarbital is therefore stable and undegraded even after 43 years of production of this preparation.
Analysis of the “Spasmoveralgin” preparation confirmed all declared active substances except atropine, whose declared concentration was low and probably below the detection limit of the HPLC method used. Somewhat surprising was the finding of 3,4-methylenedioxymethamphetamine, commonly known as ecstasy. The plausible explanation is that it is the product of the degradation of ephedrine, which is contained in the “Spasmoveralgin” preparation [51]. Adipic acid amide is the second substance identified in the preparation compared to the declared content. Its presence is easily explained because this substance is a common excipient in dosage forms. The phenobarbital content in the “Spasmoveralgin” preparation was determined to be significantly lower than the declared amount. This is probably due to a manufacturing error, as no phenobarbital degradation products were found. The reason may also be the dosage form of the preparation. It is known that the manufacturing of suppositories has often resulted in inhomogeneity of the active substance content in the individual piece of the dosage form [52].
Only in the third specimen analyzed, solution “Sklerophyllin,” the degradation of phenobarbital was detected and it was proved that pheneturide is the main degradation product of phenobarbital. 3-Aminopentanoic acid, found in the preparation, is a probable other product of phenobarbital degradation. Both findings correspond to the measured phenobarbital content of 87.5% compared to the declared content. After more than 57 years since the manufacture of the analyzed product “Sklerophyllin,” phenobarbital has degraded from 12.5% to the two degradation products mentioned above. The weakly acidic environment of the preparation may have contributed to the relatively low degree of degradation of phenobarbital; the measured value of the solution was pH = 5.34. Ethanol, which has been determined to be 20% in solution, may also contribute to the stability of phenobarbital [20]. The determined content of theophylline, O-acetyl-β-methylcholine bromide, and sodium iodide corresponds to the values declared by the manufacturer. The green dye, defined by the manufacturer as “chlorophyllinpurin,” has not been accurately identified. It is probably one of a wide variety of chlorophyll dyes [53]. It is most likely to be hypothesized that this dye is chlorophyllin (known also as chlorin e6, CASRN [19660-77-6]), its complex with magnesium ions—chlorophyllin A (CASRN [15611-43-5]), or its degradation product, pheophorbide a5 (CASRN [15664-29-6]). This is also indicated by the measured concentration of magnesium ions, which could come from chlorophyllin A, because in a slightly acidic environment, magnesium ions dechelate [54]. In addition, according to Kephart [55], a number of chlorophyll derivatives can be formed from plant material in the preparation of chlorophyll-based green dyes. Ethyl 4-hydroxybenzoate, which is widely used as an antimicrobial preservative in pharmaceutical preparations [56, 57], was also found in the sample as an excipient unspecified by the manufacturer. Its determined concentration corresponds to the concentrations used for antimicrobial purposes. Finally, the finding of β-methylcholine can be explained as an impurity or degradation product of O-acetyl-β-methylcholine bromide.
High-resolution mass spectrometry of selected compounds
For all analyzed preparations, high-resolution tandem mass spectra were used to identify the substances present. The obtained HRMS2 spectra were compared with both the spectra measured for the standards and with the literature (Table 1). The HRMS2 spectra for four selected substances, including the design of the corresponding ion structures, are presented in Fig. 4, to enrich the hitherto insufficiently published data.
High-resolution tandem mass spectra of selected compounds found in the analyzed historical phenobarbital-containing pharmaceutical products (precursor ion is marked by the diamond): (a) ESI−-MS2 spectrum of the product ions of phenobarbital, (b) ESI+-MS2 spectrum of the product ions of pheneturide, (c) ESI+-MS2 spectrum of the product ions of 3-aminopentanoic acid, and (d) ESI+-MS2 spectrum of the product ions of 3,4-methylenedioxymethamphetamine
Phenobarbital is the target molecule studied in this work. Its obtained spectrum (Fig. 4a) is analogous to the spectra obtained by other methods of ionization, especially collision-induced dissociation [36, 58] chemical ionization [59], or electron impact ionization [60]. However, the structures of ESI fragments have not yet been proposed in the literature.
According to our best knowledge, the HRMS2 of pheneturide, the main product of phenobarbital degradation, has not yet been published in the literature. Its measured mass spectrum, including the design of the corresponding ion structures, is therefore shown in Fig. 4b. The situation is similar also in the case of the second probable product of degradation of phenobarbital, which is 3-aminopentanoic acid. Its measured mass spectrum is shown in Fig. 4c.
Finally, in Fig. 4d, the measured spectrum of 3,4-methylenedioxymethamphetamine is documented, as its presence in the analyzed “Spasmoveralgin” preparation was very surprising. Fragmentation ions agree with the data reported in the literature [40], but the proposals of probable structures of individual ions, given in this work, are much richer.
Conclusions
Analysis of three historical pharmaceutical preparations containing phenobarbital, which differ in the type of dosage form, revealed that phenobarbital is stable in solid and semisolid preparations even after decades of its manufacture. On the other hand, the phenobarbital concentration decreased to 87.5% in the 57-year-old solution of “Sklerophyllin” and two degradation products were found: pheneturide, 3-aminopentanoic acid. When determining the content of the main active ingredients in the analyzed preparations, relatively large manufacturing errors were found in their production. Furthermore, the mass spectra of four selected substances (phenobarbital, pheneturide, 3-aminopentanoic acid, and 3,4-methylenedioxymethamphetamine) were measured and interpreted, which so far have not been sufficiently published in the literature.
Experimental
Analyzed samples, chemicals
The historical pharmaceutical products analyzed (Fig. 2) came from the collection of the Department of Analytical Chemistry, Faculty of Science, Charles University (Czech Republic). The storage conditions of the samples are not known; it is assumed that they have been stored in the dark at room temperature. Sample dating was performed on the basis of a lot number. In the case of the “Sklerophyllin” sample, the dating was only approximately estimated according to the information on the packaging and the data from the literature. The composition of the samples is given above in the section Introduction.
The following substances were used as standards of active pharmaceutical ingredients or excipients: O-acetyl-β-methylcholine bromide (≥ 98%, Merck), aminophenazone (reagent grade, Merck), atropine (≥ 99%, Merck), caffeine (p.a., Sigma-Aldrich), codeine (according to Ph. Eur., Zentiva, Czech Republic), ephedrine (p.a., Lachema, Czech Republic), ethanol 96% (p.a., Lach-Ner, Czech Republic), ethyl 4-hydroxybenzoate (ReagentPlus, Merck), magnesium chloride (p.a., Lach-Ner, Czech Republic), papaverine hydrochloride (p.a., collection of the Department of Analytical Chemistry, Faculty of Science, Charles University), phenobarbital (p.a., Lach-Ner, Czech Republic), potassium bromide (p.a., Lach-Ner, Czech Republic), potassium iodide (p.a., Lach-Ner, Czech Republic), D-(-)-quinic acid (98%, Merck), sodium chloride (p.a., Lach-Ner, Czech Republic), sucrose (p.a., Lach-Ner, Czech Republic), and theophylline (≥ 99%, Merck).
The other chemicals used were: acetic acid 99% (p.a, Lach-Ner, Czech Republic), acetonitrile (HPLC Supra-Gradient, Biosolve Chimie, France), ammonium acetate (p.a, Lach-Ner, Czech Republic), 18-crown-6 ether (99%, Merck), ethanol 96% (p.a., Penta, Czech Republic), formic acid 98% (p.a, Lach-Ner, Czech Republic), imidazole (ACS Reagent, Merck), methanol (HPLC Supra-Gradient, Biosolve Chimie, France), phosphomolybdic acid hydrate (ACS reagent, Merck), and sodium hydroxide (p.a., Lachema, Czech Republic). Deionized water, prepared on a Milli-Q instrument (Millipore, USA), with a specific conductivity < 0.05 μS cm−1 was used (unless otherwise stated).
Procedures, instrumentation
Prior to analysis, a weighed formulation of the studied pharmaceutical product was dissolved in a defined amount of methanol in a volumetric flask (50.00 cm3 for “Sedobelin,” 100.0 cm3 for “Spasmoveralgin”) using ultrasound. The resulting suspension was filtered through a 0.20 μm syringe filter (Whatman). In the case of “Sklerophylline,” a volume of 1.00 cm3 was pipetted from the liquid sample, diluted in a 5.00 cm3 volumetric flask by methanol and filtered through a 0.20 μm syringe filter.
An Agilent 1200 HPLC System with a binary pump was used for HPLC–MS. The detection was performed using an internal diode-array detector and with a connected mass spectrometer. Separation was performed on a Supelcosil™ LC-18 (250 × 4.5 mm, 5 μm; Supelco) column with a temperature maintained at 30 °C. To analyze the preparation “Sedobelin” or “Spasmoveralgin,” the binary mobile phase consisting of aqueous 20 × 10–3 mol dm−3 acetate buffer (CH3COOH/CH3COONH4) of pH = 3.50 (solvent A) and acetonitrile (solvent B) was used with a flow rate of 1.0 cm3 min−1. The gradient program started with 70% of A which was maintained constant for 7.5 min, then linearly decreased to 55% of A within 8.5 min, then linearly decreased to 10% of A within 6 min, then maintained constant for 2 min, then linearly increased to 70% of A within 2 min, and finally maintained constant for 4 min; the total analysis time was 30 min. The volume of injected sample was 3 mm3. In the case of preparation “Sklerophyllin,” the binary mobile phase consisted of aqueous 10–2 mol dm−3 acetate buffer (CH3COOH/CH3COONH4) of pH = 2.50 (solvent A) and methanol (solvent B). The flow rate was 1.0 cm3 min−1. The gradient program started with 75% of A that was maintained constant for 8 min, then linearly decreased to 45% of A within 8 min and then maintained constant for 1 min, then increased to 75% of A within 1 min, and finally maintained constant for 12 min; thus, the total analysis time was 30 min. The volume of injected sample was 5 mm3.
High-resolution tandem mass spectrometry detection was performed on a Bruker QqTOF compact instrument operated with Compass otofControl 4.0 software (Bruker Daltonics, Germany). For data processing software Compass DataAnalysis 4.4 (Build 200.55.2969; Bruker Daltonics, Germany) was used. ESI-MS2 data were collected in both positive and negative mode, the scan range was m/z = 50–1000. The drying gas temperature was set at 220 °C, and its flow rate was 3.0 dm3 min−1. The cone voltage was 2800 V. Measured mass spectra were analyzed using Compass CompoundCrawler 3.0 software (Bruker, Germany). The calibration method was employed for the quantification of analytes.
The determination of aminophenazone in the preparation “Spasmoveralgin” was carried out using a spectrophotometric method based on a reaction with phosphomolybdic acid, according to Ghimicescu et al. [49]. Measurement was done on a single-beam diode-array spectrophotometer HP-8453 (Agilent, USA) in a quartz cuvette with an absorption layer thickness of 1 cm at wavelength 630 nm. The quantification was based on a calibration method.
All electrophoretic measurements were performed on an Agilent 7100 capillary electrophoresis instrument (Agilent Technologies, Germany) equipped with a diode array and a contactless conductivity detector. The measurement temperature was maintained at 25 °C. The calibration method was used for the quantification of ions. The determination of bromide and iodide was carried out in a 20 µm i.d., 375 µm o.d. fused-silica capillary (Polymicro Technologies, USA), 110.0 cm total length, 95.0 cm effective length. Prior to the first use, the capillary was flushed 10 min with 1.0 mol dm−3 aqueous solution of sodium hydroxide and then 10 min with deionized water. Between individual runs, the capillary was flushed 3 min with the background electrolyte consisting of 1.0 mol dm−3 aqueous solution of formic acid. The sample was introduced by a pressure of 5 kPa for 10 s. During separation, the voltage was set at − 25 kV (current was 4 µA) and a pressure of 45 mbar was applied to the outlet vial. Contactless conductivity detection was used. Determination of magnesium and sodium cations was carried out in a 50 µm i.d., 375 µ.m. o.d. capillary, 80.0 cm total length, 71.5 cm effective length. Prior to the first use, the capillary was treated as previously described. Between individual runs, the capillary was flushed 3 min with the background electrolyte consisting of 10–2 mol dm−3 aqueous solution of imidazole adjusted to pH = 4.5 (set using acetic acid) and with the addition of 4.0 × 10–3 mol dm−3 18-crown-6 ether. The sample was introduced by a pressure of 5 kPa for 10 s. During separation, the voltage was set at 30 kV (current was 6 µA). UV detection at 200 nm wavelength was employed.
The ethanol concentration in the preparation “Sklerophyllin” was determined by head-space solid-phase microextraction (SPME) [61]. The analyzed preparation was diluted 1:20 with distilled water. A 1.00 cm3 of the diluted solution was dispensed into a 4 cm3 glass vial with the septum. The solution in the vial was stirred using a magnetic stirrer, and a SPME fiber Carboxen-PDMS 75 μm was placed in the headspace using a SPME Holder (both Supelco, USA). The sorption on the fiber took place at room temperature for 30 min. Next, the fiber was placed into the injection port of the GC–MS. The GC–MS measurements were performed on a Shimadzu QP-2010 instrument. The injection was performed in splitless mode, and the injector temperature was 250 °C. Separation was achieved using an Agilent J&W DB-WAX column (30 m × 0.25 mm; the film thickness 0.25 μm). The oven temperature was initially set at 35 °C for 3 min and then increased at a rate of 15.0 °C min−1 to 250 °C and then held for 10 min. The pressure of the carrier gas (helium) was 60 kPa. Electron ionization with an electron energy of 70 eV and a quadrupole mass analyzer in scan mode in the range of m/z = 25–350 was used. The retention time of ethanol was 4.11 min, and the standard addition method was used for its quantitation.
References
Sengupta P, Chatterjee B, Tekade RK (2018) Int J Pharm 543:328
Zilker M, Sörgel F, Holzgrabe U (2018) J Pharm Biomed Anal 150:318
Zilker M, Sörgel F, Holzgrabe U (2019) Drug Test Anal 11:1065
Zilker M, Sörgel F, Holzgrabe U (2019) J Pharm Biomed Anal 166:222
Cantrell L, Suchard JR, Wu A, Gerona RR (2012) Arch Intern Med 172:1685
Alnahas F, Yeboah P, Fliedel L, Abdin AY, Alhareth K (2020) Int J Environ Res Public Heal 17:787
Iserson KV (2021) J Emerg Med 60:669
Lyon RC, Taylor JS, Porter DA, Prasanna HR, Hussain AS (2006) J Pharm Sci 95:1549
Nesměrák K, Kudláček K, Kozlík P, Štícha M, Vašíčková P, Babica J (2020) Chem Listy 114:52
Nesměrák K, Kudláček K, Babica J (2017) Monatsh Chem 148:1557
Nesměrák K, Štícha M, Čvanšarová M (2010) Anal Lett 43:2572
Kudláček K, Nesměrák K, Štícha M, Kozlík P, Babica J (2017) Monatsh Chem 148:1613
Kudláček K, Nesměrák K, Štícha M, Kozlík P, Babica J (2018) Monatsh Chem 149:1555
Nesměrák K, Kudláček K, Štícha M, Kozlík P, Babica J (2019) Monatsh Chem 150:1611
López-Muñoz F, Ucha-Udabe R, Alamo C (2005) Neuropsychiatr Dis Treat 1:329
de Meijere A (2005) Angew Chemie Int Ed 44:7836
Yasiry Z, Shorvon SD (2012) Epilepsia 53:26
World Health Organization (2021) World health organization model list of essential medicines: 22nd list. World Health Organization, Geneva
Steenhauer AJ (1927) Pharm Weekbl 64:1154
Colombo BM, Primavera P, Lojodice D (1970) Farmaco Ed Prat 25:241
Dunker MFW (1949) J Am Pharm Assoc Sci Ed 38:409
Hasegawa J, Ikeda K, Matsuzawa T (1958) Chem Pharm Bull 6:36
Tishler F, Sinsheimer JE, Goyan JE (1962) J Pharm Sci 51:214
Garrett ER, Bojarski JT, Yakatan GJ (1971) J Pharm Sci 60:1145
Gardner LA, Goyan JE (1973) J Pharm Sci 62:1026
Dietz NJ, Cascella PJ, Houglum JE, Chappell GS, Sieve RM (1988) Pharm Res 5:803
Nachtrag I zur 7. Auflage von Gehes Codex. Schwarzec, Dresden, 1938
El-Gindy A (2005) Farmaco 60:745
Abdel Salam RA, Hadad GM, Abdel Hameed EA (2013) J Liq Chromatogr 36:384
Franeta JT, Agbaba D, Eric S, Pavkov S, Aleksic M, Vladimirov S (2002) Farmaco 57:709
Alvi SU, Castro F (1986) J Liq Chromatogr 9:2269
Domínguez-Rodríguez G, Marina ML, Plaza M (2022) Food Chem 385:132688
Taylor VF, March RE, Longerich HP, Stadey CJ (2005) Int J Mass Spectrom 243:71
Gu L, Kelm MA, Hammerstone JF, Zhang Z, Beecher G, Holden J, Haytowitz D, Prior RL (2003) J Mass Spectrom 38:1272
Su J, Fu P, Shen Y, Zhang C, Liang M, Liu R, Li H, Zhang W (2008) J Pharm Biomed Anal 46:342
Spell JC, Srinivasan K, Stewart JT, Bartlett MG (1998) Rapid Commun Mass Spectrom 12:890
John H, Binder T, Höchstetter H, Thiermann H (2010) Anal Bioanal Chem 396:751
Nesměrák K, Kudláček K, Štícha M, Kozlík P, Červený V, Kunešová J (2019) Monatsh Chem 150:1593
Bogusz MJ, Hassan H, Al-Enazi E, Ibrahim Z, Al-Tufail M (2006) J Pharm Biomed Anal 41:554
Pihlainen K, Aalberg L, Tepponen M, Clark CR, Kostiainen R (2005) J Chromatogr Sci 43:92
Dembitsky VM, Shkrob I, Rozentsvet OA (2000) Phytochemistry 54:965
Zhang Z, Yan B, Liu K, Bo T, Liao Y, Liu H (2008) Rapid Commun Mass Spectrom 22:2851
Jeong ES, Kim SH, Cha EJ, Lee KM, Kim HJ, Lee SW, Kwon OS, Lee J (2015) Rapid Commun Mass Spectrom 29:367
Marciniec B (1985) Pharmazie 40:110
Kokatsu J, Yomoda R, Suwa T (1992) Chem Pharm Bull 40:1517
Guo C, Gong L, Wang W, Leng J, Zhou L, Xing S, Zhao Y, Xian R, Zhang X, Shi F (2020) Int J Mass Spectrom 447:116250
Shi X, Yang Y, Ren H, Sun S, Mu LT, Chen X, Wang Y, Zhang Y, Wang LH, Sun C (2020) Phytochem Lett 35:175
Han C, Xia B, Chen X, Miao Q, Shen Y (2016) Food Chem 194:1199
Ghimicescu C, Stan M, Dorneanu V (1975) Farmacia (Bucharest, Rom.) 23:147
Kuczkowiak U, Petereit F, Nahrstedt A (2014) Sci Pharm 82:835
Stojanovska N, Fu S, Tahtouh M, Kelly T, Beavis A, Kirkbride KP (2013) Forensic Sci Int 224:8
Setnikar I, Fontani F (1970) J Pharm Sci 59:1319
Gross J (1991) Pigments in vegetables: chlorophylls and carotenoids. Springer Science, New York
Suzuki T, Shioi Y (2002) Photosynth Res 74:217
Kephart JC (1955) Econ Bot 9:3
Piao C, Chen L, Wang Y (2014) J Chromatogr B 969:139
Kosová M, Hrádková I, Mátlová V, Kadlec D, Šmidrkal J, Filip V (2015) J Clin Pharm Ther 40:436
Werner E, Croixmarie V, Umbdenstock T, Ezan E, Chaminade P, Tabet JC, Junot C (2008) Anal Chem 80:4918
Perchalski RJ, Yost RA, Wilder BJ (1982) Anal Chem 54:1466
Lauritsen FR, Nielsen K (2010) Int J Mass Spectrom 295:119
Mateus D, Ferreira IMPLVO, Pinho O (2011) Food Chem 126:1387
Acknowledgements
The financial support by the project “Cooperatio” of Charles University is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nesměrák, K., Štícha, M., Belianský, M. et al. Long-term stability of phenobarbital in various pharmaceutical products. Monatsh Chem 153, 735–744 (2022). https://doi.org/10.1007/s00706-022-02950-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00706-022-02950-8