Abstract
Exercise is reported to inhibit neuronal apoptotic cell death in the hippocampus and improve learning and memory. However, the effect of exercise on inhibition of neuronal apoptosis surrounding the area of damage after traumatic brain injury (TBI) and the improvement of cerebral dysfunction following TBI are unknown. Here, we investigate the effect of exercise on morphology and cerebral function following TBI in rats. Wistar rats received TBI by a pneumatic controlled injury device were randomly divided into two groups: (1) non-exercise group and (2) exercise group. The exercise group ran on a treadmill for 30 min/day at 22 m/min for seven consecutive days. Immunohistochemical and behavioral studies were performed following TBI. The number of single-stranded DNA (ssDNA)-positive cells around the damaged area early after TBI was significantly reduced in the exercise group compared with the non-exercise group (P < 0.05). Furthermore, most ssDNA-positive cells in the non-exercise group co-localized with neuronal cells. However, in the exercise group, a few ssDNA-positive cells co-localized with neurons. In addition, there was a significant increase in neuronal cell number and improvement in cerebral dysfunction after TBI in the exercise group compared with the non-exercise group (P < 0.05). These results indicate that exercise following TBI inhibits neuronal degeneration and apoptotic cell death around the damaged area, which results in improvement of cerebral dysfunction. In summary, treadmill running improved cerebral dysfunction following TBI, indicating its potential as an effective clinical therapy. Therefore, exercise therapy (rehabilitation) in the early phase following TBI is important for recuperation from cerebral dysfunction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain ischemia has been shown to induce excitotoxic cell death in the central nervous system (CNS) (Lyden and Wahlgren 2000; Zhang et al. 2002). Excitotoxic cell death is induced by the release of glutamate from neurons injured by ischemia, which subsequently leads to the over-activation of glutamate receptors resulting in the excessive influx of intracellular Ca2+ (Lyden and Wahlgren 2000; Zhang et al. 2002). Increased intracellular Ca2+ leads to the activation of caspase-3 and ultimately neuronal apoptosis and cell death (Lyden and Wahlgren 2000; Zhang et al. 2002).
In experimental focal ischemia in the rat brain, free radical production is increased by facilitation of the arachidonic acid cascade. Free radicals can induce lipid peroxidation in neuronal and glial cell membranes, and can directly cause DNA damage in neuronal and glial cells. These cascades of membrane peroxidation and DNA damage can induce neuronal and glial apoptotic cell death, which can be detected as immunopositive single-stranded DNA (ssDNA), and neuronal dysfunction (Chan et al. 1985; Lee et al. 2005). In addition, in neurons, the expression of bax, a pro-apoptotic protein, increases and the expression of bcl-2, an anti-apoptotic protein, decreases after ischemia, which results in apoptotic neuronal cell death (Sahin et al. 2010). These impairments progress automatically and induce brain edema, stroke and cerebral dysfunction (Hall and Braughler 1989; Clausen et al. 2004).
Traumatic brain injury (TBI) occurs as a result of a direct mechanical insult to the brain, and induces CNS degeneration and neuronal cell death (Chirumamilla et al. 2002; Rice et al. 2003). Following the initial mechanical insult, secondary effects including blood–brain barrier disruption, excitotoxic damage, neuronal degeneration and apoptotic cell death are induced due to the circulatory disturbance caused by ischemia (Kawamata et al. 1995; Azbill et al. 1997; Xiong et al. 1997). Moreover, in a recent study we reported that neurons and glial cells around the damaged brain region, at an early stage following TBI in the rat, induce apoptotic cell death (Itoh et al. 2009, 2010), and can contribute to cerebral dysfunction (Dressler and Vemuganti 2009).
Treadmill running exercise has been shown to increase cerebrovascular activity and the production of neurotrophic factors such as nerve growth factor (NGF), brain-derived neurotrophic factor (BDNF) and neurotrophin-3 in the brain (Wu et al. 2007; Chae and Kim 2009). In addition, studies have shown that treadmill-running exercise increases neuronal stem cell proliferation and neurogenesis in the hippocampus and cortex (Yi et al. 2009; Itoh et al. 2011). In an infarct and ischemic rat model, treadmill-running exercise was reported to inhibit apoptotic neuronal cell death in the hippocampus, and improve learning and memory (Sim et al. 2005). Moreover, in a rat brain injury model, treadmill-running exercise prevented lipid peroxidation in neuronal cell membranes, resulting in the inhibition of neuronal apoptotic cell death, and an improvement in learning and memory (Radak et al. 2001; Cechetti et al. 2008).
The effects of treadmill-running exercise on neuronal cell death in the hippocampus, and on learning, and memory following stroke and ischemia have been investigated; however, the effects of treadmill-running exercise on neuronal cell death around the damaged area and on cerebral dysfunction following TBI remain unknown. In this study, we used the rat TBI model to investigate the effects of treadmill running exercise on neuronal cell death around the damaged region and on cerebral dysfunction following TBI. We hypothesize that treadmill running exercise will inhibit neuronal apoptotic cell death around the damaged area and improve cerebral dysfunction following TBI.
Materials and methods
Animals and surgical procedures
Adult male Wistar rats (10 weeks of age, weighing 200–250 g, n = 64) were housed at 22°C under a 12:12-h light–dark cycle and had access to food and water ad libitum. All experiments were carried out with the approval of the Institutional Animal Experimentation Committee of Kinki University School of Medicine. Rats were anesthetized by intraperitoneal injection of pentobarbital (50 mg/kg). The scalp was incised along the midline and the skull was exposed. A 2 mm hole was drilled (1 mm posterior, +1 mm right lateral to bregma) in the right parietal calvaria (Itoh et al. 2005, 2007). Brain injury above the dura mater was inflicted with a pneumatic controlled injury device (Itoh et al. 2005, 2007) at an impact velocity of 4 m/s, with an impact tip diameter of 1 mm and a fixed impact deformation depth of 2 mm from the cerebral surface.
Following TBI, rats were randomly divided into two groups: (1) non treadmill running exercise group (non-exercise group, n = 26) and (2) treadmill running exercise group (exercise group, n = 26). The running protocol was performed according to a modification of Ueda’s method (Uda et al. 2006; Itoh et al. 2011). To minimize novelty stress, all rats were allowed to become familiarized with the treadmill by running on a motorized treadmill (Brain Science Idea, Osaka, Japan) for 15 min/day at 15 m/min for seven consecutive days. Electrical stimulation to encourage rats to run was disconnected to avoid pain stress after familiarization. The exercise group ran for 30 min/day at 22 m/min for seven consecutive days. The non-exercise group rats were put on the treadmill for 30 min/day for seven consecutive days without running.
Sham operation rats with no impact and non-exercise were used as controls for Morris water maze experiments (sham group, n = 12).
Morris water maze experiments
Morris water maze experiments were performed according to a modification of Elvander’s method (Itoh et al. 2009, 2010). A circular, thermostatically regulated, dark gray PVC-plastic water tank (180 cm wide, 45 cm deep; filled with tap water at 22 ± 1°C), located in the center of the testing room and surrounded by extra-maze cues, was used in the spatial learning task. A constant asymmetrical array of lamps and pictures served as cues for spatial orientation. A circular dark gray platform (15 cm wide) submerged 1 cm below the water surface served as a platform. The platform was placed in the center of the target quadrant of the water maze. Experiments were monitored using a digital TV system connected to a computer. Training took place between 8:00 am and 3:00 pm over seven consecutive days.
During the first 5 days, rats performed four swimming trials per day. The time taken to reach the platform, and the distance and speed travelled was monitored over a period of 120 s. If the platform was not noticed within 120 s, the recorded time was noted as 120 s. If the rat reached the platform within 120 s, it was allowed to remain on the platform for 30 s. A probe trial test was conducted at 6–7 days. The platform was removed on day 6–7 for a 30 s exploration test, which was recorded as the proportion of time rats were in the target quadrant.
Memory was tested in 12 animals from each of the non-exercise and exercise groups, and in 12 sham operation group animals, starting at day 1 and continuing up to 7 days after TBI/sham operation.
Immunohistochemistry
At 1 and 3 days following TBI, and after the last Morris water maze experiment at 7 days, seven rats in each of the non-exercise and exercise groups were deeply anesthetized by intraperitoneal pentobarbital (150 mg/kg), and then perfused intracardially with 300 ml of 0.1 M phosphate-buffered saline (PBS, pH 7.4–7.5) followed by 300 ml of 4% (w/v) paraformaldehyde (PFA) in PBS. The brains were removed and stored in PFA for 3 days. The maximum lesion size was sliced into 50 μm thick serial coronal sections using a microslicer (Dousaka EM, Kyoto, Japan). Each section was treated with 3% (v/v) H2O2 in Tris-buffered saline (TBS; 0.1 M Tris–HCl, pH 7.5, 0.15 M NaCl) for 30 min to block endogenous peroxidase activity. Sections were then washed three times with TBS containing 0.1% (v/v) Triton X-100 (TBS-T), blocked with 3% (v/v) bovine serum albumin (TBS-TB; BSA; Sigma, St. Louis, MO, USA) in TBS-T for 30 min, and incubated overnight at room temperature with the following primary antibodies in blocking solution: rabbit polyclonal anti-ssDNA antibody as a marker of apoptotic cell death (1:1000 dilution in TBS-TB; DAKO, Glostrup, Denmark), mouse anti-neuronal specific nuclear protein (NeuN) monoclonal antibody as a marker of neuronal cells (1:10000 dilution in TBS-TB; Millipore, Billerica, MA, USA), or mouse monoclonal anti-glial fibrillary acidic protein (GFAP) as a marker of astrocytes (1:10000 dilution in TBS-TB; BD Biosciences Pharmingen, CA, USA). Following extensive washing, the sections were further incubated with a HISTIFINE Rat-PO (mouse)-kit or HISTIFINE Rat-PO (rabbit)-kit (Nichirei, Osaka, Japan), comprised of peroxidase-conjugated anti-mouse or anti-rabbit secondary antibody, respectively, for 60 min at room temperature. The HISTIFINE Rat-PO kit contained pre-absorbed rat serum and exhibited negligible non-specific binding of rat serum in injured rat tissues. Labeling was visualized using diaminobenzidine (DAB; Vector Peroxidase Substrate Kit; Vector Laboratories, Burlingame, CA, USA) for 5 min, and only the GFAP stained sections were counterstained with hematoxylin to quantify the number of GFAP-positive cells. Negative control staining was performed with normal mouse serum instead of primary antibodies, following the procedure outlined above.
Area measurement of the damaged brain region
Area measurement of the damaged brain region was performed according to Itoh’s method (Itoh et al. 2009). To determine the area of the damaged region 7 days after TBI, five rats per group were collected after the last Morris water maze and the anteroposterior of the maximum size of the lesion was sliced into 40 serial coronal sections (50 μm thick). Anteroposterior sections 1–40 were stained with hematoxylin and eosin (HE). Images of the HE stain in the 40 anteroposterior serial sections were captured using a Nikon ECLIPSE E1000 microscope (Nikon, Tokyo, Japan) at 1× magnification and a CCD camera (Digital Sight DS-U1; Nikon, Tokyo, Japan). The area of the damaged region in each image was traced and measured by computer with ACT-2U image analysis software (Nikon, Japan), and the average area of the damaged region calculated over the 40 serial sections.
Quantification of ssDNA-, NeuN- and GFAP-positive cells
To determine the number of ssDNA-, NeuN- and GFAP-positive cells, all DAB-labeled cells within 500 μm of the edge of the damaged region (cortex), excluding the white matter, following TBI were counted in three serial sections under a Nikon E 1000 M microscope (Nikon, Japan) using a 20× objective. The number of DAB-labeled cells in three serial sections was averaged. An image of the measured area was captured at 20× magnification using the CCD camera, and the measured area and volume in each image was traced and measured by computer with ACT-2U image analysis software (Nikon, Japan). The number of DAB-labeled cells was calculated from the average number of DAB-positive cells and the volume of the tissue. Numbers of ssDNA-, NeuN- and GFAP-positive cells are expressed as the number of cells/100 μm3 (Itoh et al. 2009). To determine the number of DAB-positive cells, the area outside the damaged lesion was sliced into three serial coronal sections (50 μm thick) and the sections were stained with HE. The number of DAB-positive cells in each of the damaged sections was counted under a microscope with a 20× objective lens in four random fields. There was no significant difference in the density of cells in the measured area in the non-exercise and exercise group.
Double-immunofluorescence staining for ssDNA and NeuN
Sections collected at 3 days post-TBI were washed and blocked with 50 mM glycine in TBS for 2 h at 37°C to reduce non-specific fluorescence. The sections were washed with TBS-T, blocked with 3% (v/v) BSA in TBS-T, and incubated with the anti-ssDNA antibody (1:300) overnight at room temperature. Following extensive washing, the sections were incubated with Alexa Fluor 488 anti-rabbit IgG (1:300; BD Biosciences Pharmingen, San Diego, CA, USA) for 80 min at room temperature. Next, the sections were washed extensively and incubated with a mouse monoclonal anti-NeuN antibody (1:300) overnight at room temperature. Following extensive washing, the sections were further incubated with Alexa Fluor 555 anti-mouse IgG (1:300; BD Biosciences Pharmingen, USA) for 80 min at room temperature. The sections were subsequently observed using a confocal laser-scanning microscope (LSM5 PASCAL; Carl Zeiss Jena GmbH, Jena, Germany).
Statistical analysis
Water maze data were expressed as the mean ± SE. Data were analyzed using ANOVA and Fisher’s PLSD-test (Stat View®; SAS Institute Inc., Cary, NC, USA). Other data were expressed as the mean ± SD and analyzed using ANOVA p < 0.05 was considered statistically significant.
Results
Water maze experiments
The arrival time to the platform was significantly increased in the non-exercise group compared with the sham operation group (P ≤ 0.01, Fig. 1a). By contrast, the arrival time to the platform was significantly decreased in the exercise group compared with the non-exercise group (P < 0.05), and was not different from the sham operation group. The path length to the platform was significantly increased in the non-exercise group when compared to the sham operation group (P < 0.01, Fig. 1b). In contrast, the path length to the platform was significantly decreased in the exercise group compared with the non-exercise group (P < 0.01), and was not different from the sham operation group. The swim speed between groups was not different (Fig. 1c); however, the time spent in the target quadrant was significantly decreased in the non-exercise group compared with the sham operation group (P < 0.01, Fig. 1d). By contrast, the time spent in the target quadrant was significantly increased in the exercise group compared with the non-exercise group (P < 0.01), and did not differ from the sham operation group.
The effect of exercise on cerebral function 7 days after TBI. The effect of treatment on arrival time a path length b and swim speed c to the platform and time spent in the target quadrant d. Values represent the mean ± SE (n = 12/group). a The exercise group versus. the non-exercise group. *P < 0.05, **P < 0.01. The non-exercise group versus sham operation group. # P < 0.01. b, c The exercise group versus the non-exercise group versus sham operation group. *P < 0.05, **P < 0.01
Area of the damaged brain region after TBI
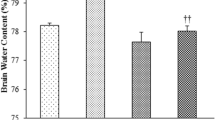
HE images of the damaged brain region 7 days after TBI (Fig. 2a–b) revealed a significant reduction in the area of the damaged brain region in the exercise group (3.53 ± 1.41 mm2) versus the non-exercise group (7.82 ± 1.69 mm2) (P < 0.001, Fig. 2c).
Size of damaged brain region 7 days after traumatic brain injury. Hematoxylin and eosin staining shows the non-exercise group a and the exercise group b. Scale bar = 1 mm. c Measurement results of each group (n = 5/group). The results are shown as the mean ± SD. The exercise group versus the non-exercise group. ***P < 0.001
Quantification of ssDNA-immunopositive cells following TBI
At 1, 3 and 7 days following TBI in the non-exercise group, many ssDNA-immunopositive cells were present around the damaged area, and possessed an ssDNA-immunopositive cytoplasm morphologically similar to those of neurons or small astrocytes (Fig. 3a). By contrast, at 1, 3 and 7 days following TBI in the exercise group, only a few ssDNA-immunopositive cells were present around the damaged area (Fig. 3b), with a significant reduction in the number of ssDNA-immunopositive cells at 1, 3 and 7 days following TBI in the exercise group (45.3 ± 15.2, 147 ± 37.1, 24.1 ± 7.6, respectively) compared with the non-exercise group (67.2 ± 13.6, 299.2 ± 16.9, 60.1 ± 16.2; P < 0.05) (Fig. 3c). The number of ssDNA-immunopositive cells 3 days after TBI in the non-exercise group was markedly higher than at 1 and 7 days after TBI (P < 0.001).
Immunostaining for single-stranded DNA (ssDNA) around the damaged cerebral cortex following traumatic brain injury in the rat. At 3 days after injury in the non-exercise group, abundant ssDNA immunoreactivity was present mainly in the nuclei a, but in the exercise group, there were only a few ssDNA immunoreactive nuclei b. Scale bars = 50 μm. Graph showing the ssDNA immunopositive cell number around the damaged cerebral cortex following traumatic rat brain injury c. The results are shown as the mean ± SD. The exercise group versus the non-exercise group. * P < 0.05; **P < 0.01; ***P < 0.001; n = 7
Quantification of NeuN- immunopositive cells following TBI
At 7 days following TBI in the non-exercise group, there were NeuN-positive cells present around the damaged area, which possessed a nuclear staining pattern (Fig. 4a). By contrast, at 7 days following TBI in the exercise group, there were many NeuN-positive cells present around the damaged area (Fig. 4b). There was a significant increase in the number of NeuN-positive cells 7 days following TBI in the exercise group (825 ± 82.6) compared with the non-exercise group (397.8 ± 18.2, P < 0.001) (Fig. 4c).
Neuronal specific nuclear protein (NeuN) expression around the damaged region 7 days following traumatic brain injury in the rat. The NeuN-positive cells were observed in the non-exercise group a, while numerous large NeuN-positive cells and fibers were observed in the exercise group b. Scale bar = 50 μm. c The number of NeuN-positive cells in each group (n = 7/group). The exercise group versus the non-exercise group. ***P < 0.001
Quantification of GFAP-immunopositive cells following TBI
At 7 days following TBI in the non-exercise group, there were many GFAP-positive fibers that formed glial scars (Fig. 5a), and these fibers were enriched at the site of damage (Fig. 5a). In contrast, in the exercise group, there were small GFAP-positive cells, which possessed a small GFAP-positive cytoplasm and a few projections (Fig. 5b). There was a significant decrease in the number of GFAP-positive cells 7 days following TBI in the exercise group (311.5 ± 27.3) compared with the non-exercise group (508.7 ± 33, P < 0.001) (Fig. 5c).
Glial fibrillary acidic protein (GFAP) expression around the damaged region following TBI in the rat. At 7 days after injury, there were many glial scars a and many GFAP-positive cells and projections a in the non-exercise group, there were few glial scars b, many GFAP-positive cells, and many projections were observed in the exercise group b. Scale bar = 50 μm. *Damaged region. c Size of GFAP-positive area in each group (n = 7/group). **P < 0.01
Double-immunofluorescence staining for ssDNA with NeuN or GFAP
There were many NeuN-immunopositive cells around the damaged area 3 days after TBI in both the non-exercise and exercise group (Fig. 6). The majority of NeuN-immunopositive cells (Fig. 6a) were also immunopositive for ssDNA (Fig. 6b) in the non-exercise group after TBI (Fig. 6c). By contrast, only a few NeuN-positive cells (Fig. 6d) co-localized with ssDNA (Fig. 6e) in the exercise group (Fig. 6f).
Double-immunofluorescence staining of single-stranded DNA (ssDNA) and neuronal specific nuclear protein (NeuN) around the damaged area 3 days after traumatic brain injury. At 3 days after the injury, many NeuN-immunopositive (a, green) and ssDNA-immunopositive (b, red) cells were observed in the non-exercise group. The ssDNA-immunopositive cells were double-immunopositive for NeuN (c, arrows, yellow). However, in the exercise group, many NeuN-immunopositive (d, green) and a few ssDNA-immunopositive (e, red) cells were observed. Only a few cells stained positive for both ssDNA and NeuN (f, arrow). Scale bar = 50 μm
Discussion
Previous studies provide strong evidence that signaling pathways can cause cellular damage and even apoptotic cell death during brain injury. For example, activation of mitochondrial pathways (Sugawara et al. 2002) and kinase signaling pathways (Irving and Bamford 2002), both of which can occur after a variety of injuries including focal cerebral ischemia and TBI, have been demonstrated. Activation of caspase-3 was also increased in hippocampal CA1 neurons 3 days after an ischemic insult, following which the release of cytochrome c from the mitochondria to the cytosol induced neural and glial apoptotic cell degeneration and death (Sugawara et al. 2002). In the present study, the peak in apoptotic ssDNA-positive cells 3 days after TBI in the exercise group (Fig. 3) is consistent with these data.
Following TBI, the number of ssDNA-positive cells in the exercise group decreased compared with the non-exercise group (Fig. 3). In addition, fewer NeuN-positive cells co-localized with ssDNA-positive cells in the exercise group compared with the non-exercise group following TBI (Fig. 6), and there were many more NeuN-positive cells around the damaged area during the chronic phase after TBI in the exercise group (Fig. 4).
Studies have shown that in a rat ischemic model, basic fibroblast growth factor (bFGF) (Wei et al. 2000), NGF (Kim et al. 2004; Nguyen et al. 2010), BDNF (Kim et al. 2004; Nguyen et al. 2010), insulin-like growth factor 1 (IGF-1) (Wine et al. 2009) and growth hormone (GH) (Shin et al. 2004) inhibit neuronal apoptotic cell death in the hippocampus and cortex by inhibiting the activation of caspase-9 and -3 after brain injury. In addition, NGF and BDNF activate the phosphatidylinositol 3 kinase (PI3K)/Akt pathway, an anti-apoptotic signaling pathway, via TrkA or TrkB receptors, resulting in a reduction in neural and glial apoptotic cell degeneration and death (Nguyen et al. 2010). Furthermore, in an in vitro Parkinson’s disease model, bFGF and IGF-1 inhibit neurotoxicity-induced apoptotic cell death of dopaminergic neurons via the extracellular signal-regulate kinase 1/2 (ERK1/2) and PI3K pathways (Hsuan et al. 2006; Sun et al. 2010). In addition, an ischemic model using diabetic rats, showed a reduction in IGF-1 and an increase in neuronal apoptotic cell death in the hippocampus, in contrast to an ischemic model using non-diabetic rats (Rizk et al. 2007). On the other hand, exercise increases the production of bFGF in the hippocampus in the rat brain, and bFGF enhances and accelerates proliferation, cell division and neuronal survival (Wu et al. 2007). In addition, exercise also increases the production of IGF-1 (Llorens-Martin et al. 2010) and GH (Blackmore et al. 2009) in the rat brain, both of which enhance neuronal survival in the hippocampus.
In the rat ischemic model, exercise after brain injury has also been shown to increase the production of NGF and BDNF in the hippocampus and cortex, and neuronal apoptotic cell death is inhibited by exercise in the hippocampus and cortex after brain injury (Hennigan et al. 2007). Moreover, exercise after brain injury increases the production of NGF, BDNF and TrkA or TrkB receptor activity, which subsequently activates the PI3K/Akt pathway leading to the inhibition of neuronal apoptotic cell death in the hippocampus (Nguyen et al. 2010).
Bcl-2 inhibits the release of cytochrome c from the mitochondria to the cytosol and blocks the activation of caspase-3, resulting in the inhibition of neuronal apoptotic cell death (Hockenbery et al. 1990). In a bcl-2-overexpressing ischemic mouse model, overexpression of bcl-2 has been shown to be neuroprotective in the hippocampus after brain injury when compared with bcl-2 deficient mice (Martinou et al. 1994; Hata et al. 1999). Interestingly, in a rat ischemic model, exercise increases the expression of bcl-2 after brain injury compared with non-exercise rats, and exercise decreases the expression of bax, which induces apoptotic cell death, resulting in the prevention of neuronal and glial apoptotic cell death and the protection of neurons in the hippocampus (Liebelt et al. 2010). Furthermore, exercise has been shown to reduce oxidative stress induced by hydroxyl radicals (·OH) and super oxide (O2 −), which induce neuronal apoptotic cell death after ischemia, and exercise after brain injury blocks neuronal apoptotic cell death and improves learning and memory (Radak et al. 2001; Cechetti et al. 2008).
These results indicate that exercise increases the number of NeuN-positive cells and decreases apoptotic cell death, and thereby alleviates neuron damage and decreases the area of damage after TBI.
In the adult CNS, TBI results in a rapid response from resident astrocytes, a process often referred to as reactive astrocytosis or glial scarring (McGraw et al. 2001; Itoh et al. 2007). This process can be identified by GFAP immunoreactivity, which appears around the damaged area after brain injury (McGraw et al. 2001; Itoh et al. 2007). and glial scar separated no damaged area from damaged area in the chronic phase after brain injury (McGraw et al. 2001; Itoh et al. 2007). In this study, the number of GFAP-positive cells 7 days following TBI in the chronic phase in the non-exercise group showed a significant increase compared with the number of cells in the exercise group. The number of GFAP-positive cells appeared to decrease in the exercise group, which could be due to the inhibitory effect of exercise on apoptosis and degeneration of neural and glial cells following TBI.
Although the Morris water maze is typically used to evaluate memory and learning, it has recently been used to evaluate cortical brain dysfunction after TBI (Xiong et al. 2008; Itoh et al. 2009). In the present study, the arrival time and path length to the platform was significantly reduced in the exercise group compared with the non-exercise group after TBI, to levels similar to the sham operation group. In addition, the time spent in the target quadrant was significantly increased in the exercise group compared with the non-exercise group after TBI to levels similar to the sham operation group, indicating that the neuroprotective effects of exercise resulted in an improvement in cerebral dysfunction following TBI (Fig. 1).
In addition, it is reported that exercise blocks neuronal apoptosis in the hippocampus and induces improvement of learning and memory (Uysal et al. 2005). Exercise increases the production of NGF and BDNF, and subsequently facilitates the expression TrkA and TrkB receptors, which promote neurogenesis and inhibit neuronal apoptotic cell death in the hippocampus resulting in an improvement of learning and memory (Wu et al. 2007; Chae and Kim 2009). Furthermore, exercise increases the expression of bFGF and IGF-1 in the hippocampus, and improves memory and learning (Wu et al. 2007; Llorens-Martin et al. 2010). Moreover, in a rat ischemic model, exercise also prevents neuronal apoptotic cell death in the hippocampus after stroke and improves learning and memory (Sim et al. 2005). These results also indicate that exercise might show an improvement in cerebral dysfunction following TBI. Furthermore, in a recent report, forced exercise was shown to effectively induce neuroprotection compared to voluntary exercise in a rat stroke model (Hayes et al. 2008). A possible explanation for this result is that forced exercise has a stressful component in contrast to voluntary exercise, and therefore, is better able to induce neuroprotection. In addition, our recent report has indicated that neurogenesis occurs around the damaged area after TBI in rats; however, it is unclear if neural stem cells migrate to the damaged area from the subventricular zone, or if de novo neurogenesis in the damaged area occurs (Itoh et al. 2007). Although cerebral function may be improved by neurogenesis after TBI, 30 days is necessary for newly born neurons to become mature following TBI (Itoh et al. 2007). In the present study, neurogenesis was monitored 7 days after TBI, and we identified that newly born neurons and neural stem cells around the damaged area following TBI did not contribute to the results of this study.
In conclusion, treadmill exercise at early phases following TBI inhibited neuronal degeneration and apoptotic cell death around the damaged area, and improved cerebral dysfunction. Thus, treadmill exercise has potential as an effective therapy following TBI. Therefore, exercise therapy (rehabilitation) in the early phase following TBI may be important for recuperation of induced cerebral dysfunction.
References
Azbill RD, Mu X, Bruce-Keller AJ, Mattson MP, Springer JE (1997) Impaired mitochondrial function, oxidative stress and altered antioxidant enzyme activities following traumatic spinal cord injury. Brain Res 765:283–290
Blackmore DG, Golmohammadi MG, Large B, Waters MJ, Rietze RL (2009) Exercise increases neural stem cell number in a growth hormone-dependent manner, augmenting the regenerative response in aged mice. Stem Cells 27:2044–2052
Cechetti F, Fochesatto C, Scopel D, Nardin P, Goncalves CA, Netto CA, Siqueira IR (2008) Effect of a neuroprotective exercise protocol on oxidative state and BDNF levels in the rat hippocampus. Brain Res 1188:182–188
Chae CH, Kim HT (2009) Forced, moderate-intensity treadmill exercise suppresses apoptosis by increasing the level of NGF and stimulating phosphatidylinositol 3-kinase signaling in the hippocampus of induced aging rats. Neurochem Int 55:208–213
Chan PH, Fishman RA, Longar S, Chen S, Yu A (1985) Cellular and molecular effects of polyunsaturated fatty acids in brain ischemia and injury. Prog Brain Res 63:227–235
Chirumamilla S, Sun D, Bullock MR, Colello RJ (2002) Traumatic brain injury induced cell proliferation in the adult mammalian central nervous system. J Neurotrauma 19:693–703
Clausen F, Lundqvist H, Ekmark S, Lewen A, Ebendal T, Hillered L (2004) Oxygen free radical-dependent activation of extracellular signal-regulated kinase mediates apoptosis-like cell death after traumatic brain injury. J Neurotrauma 21:1168–1182
Dressler J, Vemuganti R (2009) Apoptosis and gene expression after TBI. Leg Med (Tokyo) 11(Suppl 1): S54–S55
Hall ED, Braughler JM (1989) Central nervous system trauma and stroke II. Physiological and pharmacological evidence for involvement of oxygen radicals and lipid peroxidation. Free Radic Biol Med 6:303–313
Hata R, Gillardon F, Michaelidis TM, Hossmann KA (1999) Targeted disruption of the bcl-2 gene in mice exacerbates focal ischemic brain injury. Metab Brain Dis 14:117–124
Hayes K, Sprague S, Guo M, Davis W, Friedman A, Kumar A, Jimenez DF, Ding Y (2008) Forced, not voluntary, exercise effectively induces neuroprotection in stroke. Acta Neuropathol 115:289–296
Hennigan A, O’Callaghan RM, Kelly AM (2007) Neurotrophins and their receptors: roles in plasticity, neurodegeneration and neuroprotection. Biochem Soc Trans 35:424–427
Hockenbery D, Nunez G, Milliman C, Schreiber RD, Korsmeyer SJ (1990) Bcl-2 is an inner mitochondrial membrane protein that blocks programmed cell death. Nature 348:334–336
Hsuan SL, Klintworth HM, Xia Z (2006) Basic fibroblast growth factor protects against rotenone-induced dopaminergic cell death through activation of extracellular signal-regulated kinases 1/2 and phosphatidylinositol-3 kinase pathways. J Neurosci 26:4481–4491
Irving EA, Bamford M (2002) Role of mitogen- and stress-activated kinases in ischemic injury. J Cereb Blood Flow Metab 22:631–647
Itoh T, Satou T, Hashimoto S, Ito H (2005) Isolation of neural stem cells from damaged rat cerebral cortex after TBI. Neuroreport 16:1687–1691
Itoh T, Satou T, Hashimoto S, Ito H (2007) Immature and mature neurons coexist among glial scars after rat traumatic brain injury. Neurol Res 29:734–742
Itoh T, Satou T, Nishida S, Tsubaki M, Hashimoto S, Ito H (2009) Improvement of cerebral function by anti-amyloid precursor protein antibody infusion after traumatic brain injury in rats. Mol Cell Biochem 324:191–199
Itoh T, Satou T, Nishida S, Tsubaki M, Imano M, Hashimoto S, Ito H (2010) Edaravone protects against apoptotic neuronal cell death and improves cerebral function after traumatic brain injury in rats. Neurochem Res 35:348–355
Itoh T, Imano M, Nishida S, Tsubaki M, Hashimoto S, Ito A, Satou T (2011) Exercise increases neural stem cell proliferation surrounding the area of damage following rat traumatic brain injury. J Neural Trans 118:193–202
Kawamata T, Katayama Y, Hovda DA, Yoshino A, Becker DP (1995) Lactate accumulation following concussive brain injury: the role of ionic fluxes induced by excitatory amino acids. Brain Res 674:196–204
Kim DH, Zhao X, Tu CH, Casaccia-Bonnefil P, Chao MV (2004) Prevention of apoptotic but not necrotic cell death following neuronal injury by neurotrophins signaling through the tyrosine kinase receptor. J Neurosurg 100:79–87
Lee EJ, Lee MY, Chen HY, Hsu YS, Wu TS, Chen ST, Chang GL (2005) Melatonin attenuates gray and white matter damage in a mouse model of transient focal cerebral ischemia. J Pineal Res 38:42–52
Liebelt B, Papapetrou P, Ali A, Guo M, Ji X, Peng C, Rogers R, Curry A, Jimenez D, Ding Y (2010) Exercise preconditioning reduces neuronal apoptosis in stroke by up-regulating heat shock protein-70 (heat shock protein-72) and extracellular-signal-regulated-kinase 1/2. Neuroscience 166:1091–1100
Llorens-Martin M, Torres-Aleman I, Trejo JL (2010) Exercise modulates insulin-like growth factor 1-dependent and -independent effects on adult hippocampal neurogenesis and behaviour. Mol Cell Neurosci 44:109–117
Lyden P, Wahlgren NG (2000) Mechanisms of action of neuroprotectants in stroke. J Stroke Cerebrovasc Dis 9:9–14
Martinou JC, Dubois-Dauphin M, Staple JK, Rodriguez I, Frankowski H, Missotten M, Albertini P, Talabot D, Catsicas S, Pietra C et al (1994) Overexpression of BCL-2 in transgenic mice protects neurons from naturally occurring cell death and experimental ischemia. Neuron 13:1017–1030
McGraw J, Hiebert GW, Steeves JD (2001) Modulating astrogliosis after neurotrauma. J Neurosci Res 63:109–115
Nguyen TL, Kim CK, Cho JH, Lee KH, Ahn JY (2010) Neuroprotection signaling pathway of nerve growth factor and brain-derived neurotrophic factor against staurosporine induced apoptosis in hippocampal H19–7 cells. Exp Mol Med 42:583–595
Radak Z, Kaneko T, Tahara S, Nakamoto H, Pucsok J, Sasvari M, Nyakas C, Goto S (2001) Regular exercise improves cognitive function and decreases oxidative damage in rat brain. Neurochem Int 38:17–23
Rice AC, Khaldi A, Harvey HB, Salman NJ, White F, Fillmore H, Bullock MR (2003) Proliferation and neuronal differentiation of mitotically active cells following traumatic brain injury. Exp Neurol 183:406–417
Rizk NN, Myatt-Jones J, Rafols J, Dunbar JC (2007) Insulin like growth factor-1 (IGF-1) decreases ischemia-reperfusion induced apoptosis and necrosis in diabetic rats. Endocrine 31:66–71
Sahin S, Alkan T, Temel SG, Tureyen K, Tolunay S, Korfali E (2010) Effects of citicoline used alone and in combination with mild hypothermia on apoptosis induced by focal cerebral ischemia in rats. J Clin Neurosci 17:227–231
Shin DH, Lee E, Kim JW, Kwon BS, Jung MK, Jee YH, Kim J, Bae SR, Chang YP (2004) Protective effect of growth hormone on neuronal apoptosis after hypoxia-ischemia in the neonatal rat brain. Neurosci Lett 354:64–68
Sim YJ, Kim H, Kim JY, Yoon SJ, Kim SS, Chang HK, Lee TH, Lee HH, Shin MC, Shin MS, Kim CJ (2005) Long-term treadmill exercise overcomes ischemia-induced apoptotic neuronal cell death in gerbils. Physiol Behav 84:733–738
Sugawara T, Noshita N, Lewen A, Gasche Y, Ferrand-Drake M, Fujimura M, Morita-Fujimura Y, Chan PH (2002) Overexpression of copper/zinc superoxide dismutase in transgenic rats protects vulnerable neurons against ischemic damage by blocking the mitochondrial pathway of caspase activation. J Neurosci 22:209–217
Sun X, Huang L, Zhang M, Sun S, Wu Y (2010) Insulin like growth factor-1 prevents 1-mentyl-4-phenylphyridinium-induced apoptosis in PC12 cells through activation of glycogen synthase kinase-3beta. Toxicology 271:5–12
Uda M, Ishido M, Kami K, Masuhara M (2006) Effects of chronic treadmill running on neurogenesis in the dentate gyrus of the hippocampus of adult rat. Brain Res 1104:64–72
Uysal N, Tugyan K, Kayatekin BM, Acikgoz O, Bagriyanik HA, Gonenc S, Ozdemir D, Aksu I, Topcu A, Semin I (2005) The effects of regular aerobic exercise in adolescent period on hippocampal neuron density, apoptosis and spatial memory. Neurosci Lett 383:241–245
Wei OY, Huang YL, Da CD, Cheng JS (2000) Alteration of basic fibroblast growth factor expression in rat during cerebral ischemia. Acta Pharmacol Sin 21:296–300
Wine RN, McPherson CA, Harry GJ (2009) IGF-1 and pAKT signaling promote hippocampal CA1 neuronal survival following injury to dentate granule cells. Neurotox Res 16:280–292
Wu CW, Chen YC, Yu L, Chen HI, Jen CJ, Huang AM, Tsai HJ, Chang YT, Kuo YM (2007) Treadmill exercise counteracts the suppressive effects of peripheral lipopolysaccharide on hippocampal neurogenesis and learning and memory. J Neurochem 103:2471–2481
Xiong Y, Gu Q, Peterson PL, Muizelaar JP, Lee CP (1997) Mitochondrial dysfunction and calcium perturbation induced by traumatic brain injury. J Neurotrauma 14:23–34
Xiong Y, Mahmood A, Lu D, Qu C, Kazmi H, Goussev A, Zhang ZG, Noguchi CT, Schallert T, Chopp M (2008) Histological and functional outcomes after traumatic brain injury in mice null for the erythropoietin receptor in the central nervous system. Brain Res 1230:247–257
Yi SS, Hwang IK, Yoo KY, Park OK, Yu J, Yan B, Kim IY, Kim YN, Pai T, Song W, Lee IS, Won MH, Seong JK, Yoon YS (2009) Effects of treadmill exercise on cell proliferation and differentiation in the subgranular zone of the dentate gyrus in a rat model of type II diabetes. Neurochem Res 34:1039–1046
Zhang C, Shen W, Zhang G (2002) N-methyl-D-aspartate receptor and L-type voltage-gated Ca(2+) channel antagonists suppress the release of cytochrome c and the expression of procaspase-3 in rat hippocampus after global brain ischemia. Neurosci Lett 328:265–268
Acknowledgments
This work was supported by Grant-in-Aid for Scientific Research (20500472 and 21500803) and ZENRYOKEN. The authors thank Mari Yachi for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Grant information
(1) Grants-in-Aid for Scientific Research, numbers 20500472 and 21500803. (2) ZENRYOKEN.
Rights and permissions
About this article
Cite this article
Itoh, T., Imano, M., Nishida, S. et al. Exercise inhibits neuronal apoptosis and improves cerebral function following rat traumatic brain injury. J Neural Transm 118, 1263–1272 (2011). https://doi.org/10.1007/s00702-011-0629-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-011-0629-2