Abstract
Background
The unilateral biportal endoscopic (UBE) technique is less invasive and has a faster recovery time than open surgery. Compared with the uniportal technique, the biportal technique has a larger field of vision and a wider operation range.
Method
We attempted the posterior UBE approach for cervical stenosis at the C4–C6 levels. UBE decompression of C4–C6 with unilateral lateral mass screw fixation at the C4–C5 levels was performed under general anesthesia.
Conclusions
We successfully performed cord decompression at the C4–C6 levels using the UBE technique. This approach could be used as an alternative method to treat cervical stenosis with instability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Relevant surgical anatomy
Osteophytes, intervertebral space collapse, ligamentum flavum hypertrophy, and ossification of the posterior longitudinal ligament (OPLL) all lead to the narrowing of the cervical canal. In most cases, cervical myelopathy with posterior compression necessitates posterior decompressive surgery. Total laminectomy often requires auxiliary internal fixation to prevent segmental instability, and extensive paraspinal muscle release and retraction during posterior open surgery may result in axial neck pain and kyphotic deformity during long-term follow-up [4]. Endoscopic unilateral laminectomy for bilateral decompression (ULBD) needs to be performed in the narrow cervical canal, which requires a high level of technical skill and a steep learning curve [2].
The unilateral biportal endoscopic (UBE) approach has a large surgical area and a wide operation range, allowing for total laminectomy and lateral mass screw fixation while minimizing damage to the posterior tension band (PTB).
Description of the technique
Operative case presentation
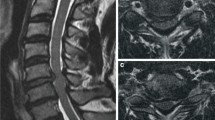
A 72-year-old woman presented with gait disturbance and numbness in both the upper and lower extremities. A physical examination revealed tendon hyperreflexia, ankle clonus, and the presence of the Babinski sign. The patient’s history included hypertension, hyperlipidemia, and coronary stent implantation. Magnetic resonance imaging (MRI) revealed central cervical stenosis at the C4-C5-C6 levels, compressing the spinal cord due to ligamentum flavum (LF) hypertrophy and disk herniation at the C4-C5-C6 levels (Fig. 1). The diagnosis of cervical myelopathy was confirmed by cervical canal stenosis with a pincer mechanism. The patient expressed strong opposition to conventional open surgeries, such as anterior fusion and posterior open-door laminoplasty, because of a previous history of cardiovascular diseases.
Surgical instruments
We used the same lateral mass screws and rods as in the conventional posterior approach. A high-speed burr (Guizhou Zirui Technology, China), conventional arthroscopic facilities, a tool-kit of radiofrequency (RF) systems (Jiangsu BONSS Medical Technology, China), and open spine surgical equipment, such as pituitary forceps and Kerrison rongeurs, were used.
Position and creation of portals
The patient was placed in the prone position under general anesthesia with mild flexion of the cervical spine. The head was placed in a horseshoe-shaped cushion and fixed with tape, and the shoulders were held down by plasters. The head of the operation table was lifted until the cervical intervertebral space was perpendicular to the ground.
Two horizontal lines were drawn along the C4 and C6 pedicles, while a vertical line was drawn in the midline of the left lateral mass in the anteroposterior view. The cranial intersection point served as a viewing portal, while the caudal intersection point served as a working portal. Two incisions were made on the right side of the spinous processes of C5 and C6, and the screw portals were formed with serial dilators at 30 degrees laterally and parallel to the adjacent facet to implant the lateral mass screws at C4 and C5 (Fig. 2).
Tip sparing and lateral mass screw fixation
First, the “sliding technique” was used to dissect and expose the left laminae of C4–C6, the interlaminar space, and the medial border of the facet joint using RF probe. The interlaminar spaces between C4–C5 and C5–C6 were clearly identified. Second, the tip of the spinous process of C4–C5 was cut and floated automatically due to the PTB function. After moving from the stump of the spinous process to the contralateral side, the lateral masses at C4 and C5 and the laminae at C4–C6 on the right side were exposed using RF. Third, we used a 2-mm diamond burr to locate the correct screw entry point, which was confirmed by fluoroscopy. Two 3.5-mm polyaxial screws with lengths of 12 mm were inserted through the screw portals according to the Magerl technique [1]. An appropriately sized rod was selected, and bent to match the contours of the lateral masses. During the installation of locking nuts, a hemi-cannula can be used to prevent the nuts losing into the soft tissue (Fig. 3).
The tip of the spinous process was cut, and RF probe could reach the contralateral lamina (a). A diamond burr was used to determine the entry point of the screw (b) and confirmed by fluoroscopy (c). The screw was placed in the lateral mass evenly (d). The screws were connected by a curved rod (e) and secured by locking nuts (f)
Total laminectomy
First, the remnant spinous processes were removed with a grinding drill. Then, starting at the dorsal cortex of C5, the laminae were gradually thinned until only the ventral cortical bone remained. The ventral laminae were then excised with 1-mm Kerrison rongeurs. The lower part of the C4 lamina was removed with a diamond burr until the proximal insertion of C4–C5 LF was exposed. Similarly, the upper part of the C6 lamina was removed until the distal insertion of C5–C6 LF was exposed, and the LFs between C4–C5 and C5–C6 were dissociated and gradually resected. The full decompression of the cervical canal was confirmed by direct visualization (Video 1). A drainage tube was inserted through the working portal (Fig. 4). The incisions were closed with absorbable sutures. The surgery was conducted without complications. The estimated blood loss during the surgery was 100 mL, and the operation time was 175 min.
Intraoperative endoscopic images during endoscopic decompression. A diamond burr was used to remove the dorsal cortical bone of the laminae (a), and LFs between C4–5 (white arrow) and C5–6 (black arrow) were exposed (b). The C4-C5-C6 levels were completely decompressed after endoscopic decompression, and a drainage tube was inserted (c)
Postoperative course
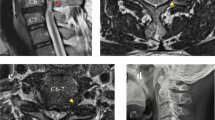
Numbness and gait dysfunction were significantly improved postoperatively. Postoperative 3D-CT and radiograph confirmed that the internal fixation was in good condition, and the MRI results revealed that the central canal was completely decompressed at the C4–C5 levels (Fig. 5).
Indications
The indications for UBE laminectomy with lateral mass screw fixation were central cervical stenosis requiring total laminectomy and degenerative cervical stenosis with segmental cervical instability. This procedure can also be performed if previous posterior hemilaminectomy, multilevel anterior corpectomy, or discectomy with support grafting has been performed. We do not recommend the procedure in patients with infectious, traumatic, or tumoral cervical spine disorders.
Limitations
Lateral masses in the upper cervical area are usually small. Therefore, we suggest that this technique be used at the lower cervical level (C3–C7). This approach is usually possible at the lower cervical levels (C3–C7) but not at the upper cervical levels (C1–C2). Dysplasia or congenital absent lateral masses should not be ignored before undergoing surgery. Abnormally distributed vertebral arteries make safe screw placement difficult or impossible and thus deserve special attention.
How to avoid complications
Intraoperative neuroelectrophysiological monitoring has been shown to considerably reduce the risk of neurological injury. The myofascial in the working portal must be completely incised to maintain outflow patency and prevent epidural hypertension. If endoscopic visualization or an appropriate screw trajectory proves difficult, the surgery must be converted to an open procedure.
Specific information for the patient
Although posterior decompression is thorough, second-stage anterior decompression may be necessary in some situations. There have been no long-term follow-up reports on the clinical and radiologic outcomes of posterior UBE decompression with lateral mass fixation in the treatment of cervical stenosis. The patient should be informed preoperatively that the procedure may be converted to a standard open surgery if there is insufficient endoscopic decompression or severe dural adhesions.
Specific perioperative considerations
A reasonable anti-osteoporosis treatment can effectively improve bone mineral density while preventing screw loosening and displacement.
References
Magerl F, Grob D, Seemann P (1987). Stable dorsal fusion of the cervical spine (C2-Th1) using hook plates[J]. In: Kehr P, Weidner A (eds) Cervical spine I. Springer, New York, pp 217–221. https://doi.org/10.1007/978-3-7091-8882-8_38
Song KS, Lee CW (2020) The biportal endoscopic posterior cervical inclinatory foraminotomy for cervical radiculopathy: technical report and preliminary results [J]. Neurospine 17(Suppl 1):S145–S153. https://doi.org/10.14245/ns.2040228.114
Su N, Fei Q, Wang BQ, Kang N, Zhang QM, Tang HH et al (2019) Comparison of clinical outcomes of expansive open-door laminoplasty with unilateral or bilateral fixation and fusion for treating cervical spondylotic myelopathy: a multi-center prospective study. BMC Surg 19:116. https://doi.org/10.1186/s12893-019-0583-8
Wang M, Luo XJ, Deng QX, Li JH, Wang N (2016) Prevalence of axial symptoms after posterior cervical decompression: a meta analysis. Eur Spine J 25:2302–2310. https://doi.org/10.1007/s00586-016-4524-2
Funding
This work was supported by the National Key R&D Program of China (2019YFC0121400).
This study protocol was approved by the Research Ethics board in our hospital. The patient signed a written informed consent form that she will be enrolled in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Key points
• We successfully performed total laminectomy for cervical stenosis with unilateral lateral mass screw fixation using a biportal endoscopic posterior approach.
• The benefits of the endoscopic approach included the preservation of the paraspinal muscles and ligaments, a minimal amount of estimated blood loss, fast postoperative recovery, and a short hospital stay.
• The portals were designed based on the lesion site, and the endoscopic instruments moved across the surface of the lamina; thus, two incisions were sufficient for multilevel decompression.
• Imaging data should be analyzed meticulously, and the course of the vertebral artery and any aberrant anatomy should be recognized.
• Dissection should not exceed the lateral margin of the lateral mass; otherwise, significant bleeding can occur, obscuring the operation field.
• A 2-mm diamond burr can be used to locate the screw entry points under fluoroscopy.
• It is slightly difficult to insert the rod into the polyaxial screws under endoscopy, and more patience is needed.
• The locking nuts can be implanted with the aid of a hemi-cannula to ensure that the locking nuts are not lost in soft tissue.
• Unilateral and bilateral lateral mass screw fixation can produce similar results in terms of cervical curvature maintenance and clinical outcomes [3].
• The dorsal cortex of the lamina can be removed with a grinding drill, and the ventral cortical bone can be carefully removed with a 1-mm Kerrison rongeur to ensure that the cord is not injured.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spine degenerative
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 282793 KB)
Rights and permissions
About this article
Cite this article
Zhu, C., Deng, X., Pan, H. et al. Unilateral biportal endoscopic laminectomy with lateral mass screw fixation for treating cervical spinal stenosis. Acta Neurochir 164, 1529–1533 (2022). https://doi.org/10.1007/s00701-022-05212-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05212-y