Abstract
Background
Although cervical laminoplasty is a frequently utilized surgical intervention for cervical spondylotic myelopathy, it is primarily performed using conventional open surgical techniques. We attempted the minimally invasive cervical laminoplasty using biportal endoscopic approach.
Methods
Contralateral lamina access is facilitated by creating space through spinous process drilling, followed by lamina hinge formation. Subsequently, the incised lamina is elevated from ipsilateral aspect, and secure metal plate fixation is performed.
Conclusion
We successfully performed the cervical open door laminoplasty using biportal endoscopic approach. Biportal endoscopic cervical open-door laminoplasty may be a minimally invasive technique that can prevent complications related with open surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Relevant surgical anatomy
The creation of a contralateral laminar hinge from the ipsilateral side and the elevation of the laminar flap are fundamental steps in biportal endoscopic cervical laminoplasty. The length of the laminae in the cervical region is shorter than that in the lumbar region, facilitating easier access to the contralateral cervical laminae. When exposing the opposite side of the lamina, the spinous process may obstruct the view. In such instances, the spinous process is partially removed or trimmed at its base using a drill. Endoscopy, alongside specialized instruments, enables access to the contralateral laminar lateral border by utilizing the space acquired by drilling out the spinous process. By establishing portals close to the midline, an endoscopic drill can efficiently reach the contralateral lamina with a stiffer approach angle, facilitating effective drilling to create a hinge [4, 5]. The advantages of biportal endoscopic surgery, which involves independent manipulation using two hands, contribute to technical advancements, making endoscopic laminoplasty a viable option for treating cervical spondylotic myelopathy [2, 4, 5, 8].
Description of the technique
Surgical instruments
The standard biportal endoscopic systems, a toolkit set for biportal endoscopic spine surgery, radiofrequency (RF) systems, working cannula, and a scope retractor (MD company, South Korea) were utilized for this technique [5, 6].
Additionally, the CenterpieceTM Open Door Plate fixation system (Medtronic, Minnesota, USA) which features a "laminar shelf" and "kickstand" design, is utilized for lamina fixation [1].
Positioning and portal creation
Under general endotracheal anesthesia, the patient was positioned prone with neck flexion secured using skin tape [7]. The surgical procedure is detailed herein using a case example of biportal endoscopic cervical laminoplasty targeting cervical spondylotic myelopathy at the C5-6–7 levels from the patient's left side (Fig. 1). Three linear skin incisions were made at midpoints between the pedicle and spinous process at the affected level (Fig. 2a). The central incision served for metal plate fixation and was directly made on the target lamina (Fig. 2b).
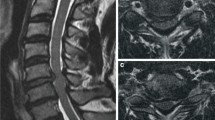
Preoperative images from a 72-year-old man who presented with symptoms of cervical spondylotic myelopathy. (a) Severe spinal cord compression and signal changes (red arrowheads) were observed on the sagittal section of a T2-weighted magnetic resonance image (MRI) at the C5-6–7 levels. (b, c) Axial sections of the MRI revealed severe stenosis of the spinal canal and neuroforamen (yellow arrowheads) at the C5-6 and C6-7 levels. (d)The lateral X-ray view demonstrated cervical kyphosis
Making portals and initial laminotomy during the biportal endoscopic cervical laminoplasty at the C5-C6-C7 left. (a) The locations of the portals (colored oval circles) are shown, situated between the pedicle (white dotted circle) and midline (white longitudinal line). The central portal (blue oval circle) is utilized for metal plate fixation and facilitates water outflow. (b) Intraoperative C-arm image. The instruments access the target lamina perpendicular to the midline axis (white asterisk) through the central working portal (blue oval circle). Scope retractors were applied at every portal. (c) Initial marginal laminotomy (areas marked with red) was performed before creating the hinge."
Craniocaudal laminotomy for ligamentum flavum detachment (Video 1)
Following soft tissue dissection, clear exposure of the spinous process, ipsilateral lamina, and interlaminar space was achieved. The interlaminar border of adjacent upper and lower-level laminae (C5 and C7) was drilled to detach the ligamentum flavum from bony structures, facilitating smooth elevation of the laminar flap (Fig. 2c).
Contralateral laminar hinge creation (Video 2)
The mid and spinolaminar junctional portion of the spinous process was drilled out while preserving the interspinous ligament to establish a surgical tract for the contralateral side (Fig. 3a). A scope retractor was used to elevate soft tissue, creating a secure contralateral working space. Through this space, the endoscopic drill accessed the contralateral lamina with a stiffer approach angle, drilling the contralateral lamina under endoscopic guidance (Fig. 3b). Finally, the contralateral gutter was created under endoscopic guidance Following the creation of the contralateral hinge, two portals were transitioned to the ipsilateral laminae.
Making hinge and laminectomy is described with illustrations during biportal endoscopic cervical laminoplasty. (a) Drilling out the spinous process to obtain space for contralateral access. (b) Making a hinge in the contralateral lamina by crossing the midline. (c) Ipsilateral laminectomy. (d) Elevating the laminar flap from the ipsilateral laminectomy edge. In all surgical steps, the tip of the scope retractor created working space at every corner by pulling and pushing the soft tissue
Ipsilateral laminectomy (Video 2)
Ipsilateral laminectomy, the final bony drilling step, involved linear laminectomy along the medial border of the facet joint using a 4 mm diameter diamond drill (Fig. 3c). The laminectomy width corresponded to the size of the drill.
Laminar flap elevation (Video 3)
Before elevating the laminar flap, proximal and distal ends of the ligamentum flavum were released from the drilled laminar border using hooks and dissectors. The laminar flap was then carefully elevated from the ipsilateral edge of the laminectomy using the two-hands technique, with a scope retractor on the left hand and a dissector on the right hand, applying gradual pressure to prevent hinge fracture (Fig. 3d).
Metal plate fixation (Video 4)
The metal plate size was determined using a customized ruler under endoscopic vision and the laminar shelf height on preoperative computed tomography axial images. The plate was inserted into the working space through the central portals using forceps. Initially, the plate laminar shelf was fitted onto the lamina, followed by tucking the kickstand onto the edge of the lateral mass (Fig. 4a). Plate manipulation was executed using curved forceps due to the impossibility of assembling the plate holder within the narrow working space. While the scope retractor held the plate in place, holes for screw fixation were drilled using a 2 mm diameter drill, and the plate was fixed with premeasured screws from the lateral mass to the lamina (Figs. 4b, c, d). Following fixation, the integrity of the hinge site was confirmed through endoscopic inspection, and closed suction drainage was placed over the plate and lamina to prevent epidural hematoma.
Surgical steps of metal plate fixation during biportal endoscopic cervical laminoplasty. The laminar shelf and kickstand of the metal plate were fitted in the lamina and lateral mass, sequentially. A scope retractor held the laminectomy edge, facilitating the insertion of the metal plate. (c) Screw fixation was performed first in the lateral mass. (d) Subsequently, the laminar flap was fixed using premeasured screws. (e) Illustration after a successful operation
The postoperative images demonstrate a decompressed spinal cord and a properly positioned metal plate (Fig. 5).
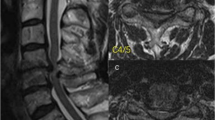
Postoperative radiological results and surgical wound after biportal endoscopic cervical laminoplasty and laminectomy at the C5-C6-C7 left. (a) Sufficiently expanded spinal canal was observed on the sagittal section of the magnetic resonance image (MRI). (b, c) Axial cuts of MRI showed a decompressed spinal canal and ipsilateral neuroforamen (yellow arrowheads) at the C5-6 and C6-7 levels. Minimal muscle injury was found along the ipsilateral surgical tract (blue triangle); however, contralateral extensor muscles were intact (red asterisks). (d) Axial image of computed tomography (CT) six months postoperatively. The metal plate was placed in the appropriate position and firmly fixed with screws. The lamina hinge was also well preserved without fracture. (e) Three-dimensional reconstruction CT images showed the contour of the marginal laminotomy (white dotted lines) and the appropriate position of the metal plate (asterisk). A laminar hinge was also found at the contralateral lamina (red arrowheads). (f) Surgical wound one month after surgery
Indications
The indications for this technique are similar to those of endoscopic decompression laminectomy for the treatment of cervical spondylotic myelopathy [4]. However, due to technical intricacies, this approach is particularly recommended for cases involving a single lamina located between two consecutive interlaminar spaces, necessitating two-segment decompression laminectomy. This recommendation is particularly relevant in patients with cervical kyphosis. Additionally, this technique offers the advantage of resolving combined foraminal stenosis simultaneously [4].
Limitations
Conventional instruments are impractical in narrow working spaces; therefore, alternative instruments are essential for manipulating metal plates, and using a scope retractor is indispensable for successful plate fixation. Patients with osteoporotic and thin laminae are unsuitable candidates due to the heightened risk of hinge fracture and instrumentation failure. Performing multi-segmental laminoplasty is likely to be technically challenging and time-consuming.
How to avoid complications
This surgical procedure should be undertaken by surgeons with abundant experience in both endoscopic cervical surgery and conventional laminoplasty. During the procedure of plate fixation, it is crucial to manage the water pressure carefully to prevent compression of the dura and potential injury to the spinal cord [3]. Verification of proper discharge of continuous saline irrigation must be ensured during surgery. Plate fixation is time-consuming, particularly for beginners, and performing multiple-level endoscopic laminoplasty may increase the risk of irreversible spinal cord injury. Therefore, we recommend considering conventional laminoplasty for patients requiring multiple-level laminoplasty. In cases where diffuse epidural bleeding obscures the endoscopic view during laminar flap elevation, achieving hemostasis using a foamy agent should be prioritized to ensure clear vision before proceeding further.
Specific perioperative considerations
The laminoplasty plate is affixed to the bone using small screws, and it is advisable to employ a type of plate that can be temporarily secured to the lamina even before complete fixation with screws. We utilized the Open-door plate type of Centerpiece, featuring a "Laminar shelf" designed for easy fixation to the lamina and a "Kickstand" to enhance stability on the lateral mass. It is important to note that using a graft plate without a laminar shelf and kickstand is not recommended due to associated technical difficulties.
Specific information to give the patient about surgery and potential risks
While laminoplasty offers advantages in preventing restenosis and epidural adhesions, it is essential to inform patients about the potential risks, including the possibility of plate fixation failure during surgery. In such cases, conversion of the laminoplasty procedure to total laminectomy may become necessary. Additionally, if an endoscopic approach proves to be technically challenging, transitioning to open surgery should be contemplated.
Data availability
The data and materials used in this study are available upon request from the corresponding author.
Code availability
Applicable.
References
Chen H, Liu H, Zou L, Li T, Gong Q, Song Y, Zeng J, Liu L, Kong Q (2016) Effect of mini-plate fixation on hinge fracture and bony fusion in unilateral open-door cervical expansive laminoplasty. Clin Spine Surg 29:E288-295. https://doi.org/10.1097/bsd.0000000000000131
Heo DH, Ha JS, Jang JW (2023) Biportal endoscopic posterior cervical foraminotomy for adjacent 2-level foraminal lesions using a single approach (sliding technique). Neurospine 20:92–98. https://doi.org/10.14245/ns.2346144.072
Kang MS, Park HJ, Hwang JH, Kim JE, Choi DJ, Chung HJ (2020) Safety evaluation of biportal endoscopic lumbar discectomy: assessment of cervical epidural pressure during surgery. Spine (Phila Pa 1976) 45:E1349-e1356. doi:https://doi.org/10.1097/brs.0000000000003585
Kim J, Heo DH, Lee DC, Chung HT (2021) Biportal endoscopic unilateral laminotomy with bilateral decompression for the treatment of cervical spondylotic myelopathy. Acta Neurochir (Wien) 163:2537–2543. https://doi.org/10.1007/s00701-021-04921-0
Kim J, Heo DH, Lee DC, Park CK, Chung H (2022) Surgical removal of cervical extradural cysts using the biportal endoscopic approach. World Neurosurg 164:228–236. https://doi.org/10.1016/j.wneu.2022.05.034
Kim JY, Ha JS, Lee CK, Lee DC, Hong HJ, Choi SY, Park CK (2023) Biportal endoscopic posterior thoracic laminectomy for thoracic spondylotic myelopathy caused by ossification of the ligamentum flavum: technical developments and outcomes. Neurospine 20:129–140. https://doi.org/10.14245/ns.2346060.030
Song KS, Lee CW (2020) The biportal endoscopic posterior cervical inclinatory foraminotomy for cervical radiculopathy: technical report and preliminary results. Neurospine 17:S145-s153. https://doi.org/10.14245/ns.2040228.114
Zhu C, Deng X, Pan H, Zhang W (2022) Unilateral biportal endoscopic laminectomy with lateral mass screw fixation for treating cervical spinal stenosis. Acta Neurochir (Wien) 164:1529–1533. https://doi.org/10.1007/s00701-022-05212-y
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
Corresponding Author (DH Heo): Conceived and designed the study, conducted data analysis and interpretation, drafted the manuscript, critically reviewed it for important intellectual content.
First Author (JY Kim): Contributed to data collection, analysis, and interpretation, critically reviewed the manuscript for important intellectual content.
Co Authors (HS Kim, SY Choi, KM Kim): Contributed to study design, provided technical or material support, critically reviewed the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
Applicable.
Consent for publication
Applicable.
Conflicts of interest/Competing interests
The authors declare no conflicts and competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Video 1 Endoscopic video demonstrating biportal endoscopic cervical laminoplasty and foraminotomy performed at the C5-6-7 levels on the left side of the patient. Surgical techniques include marginal laminotomy and ipsilateral foraminotomy. (MP4 25305 KB)
Video 2 Creation of the contralateral laminar hinge and ipsilateral laminectomy. (MP4 90682 KB)
Video 3 Completion of the foraminotomy and detachment of the laminar flap. (MP4 52426 KB)
Video 4 Fixation of the metal plate. (MP4 78194 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, J.Y., Heo, D.H. Biportal endoscopic cervical open-door laminoplasty to treat cervical spondylotic myelopathy. Acta Neurochir 166, 182 (2024). https://doi.org/10.1007/s00701-024-06076-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-06076-0