Abstract
Background
Idiopathic intracranial hypertension (IIH) is characterised by an increased intracranial pressure (ICP) in the absence of any central nervous system disease or structural abnormality and by normal CSF composition. Management becomes complicated once surgical intervention is required. Venous sinus stenosis has been suggested as a possible aetiology for IIH. Venous sinus stenting has emerged as a possible interventional option. Evidence for venous sinus stenting is based on elimination of the venous pressure gradient and clinical response. There have been no studies demonstrating the immediate effect of venous stenting on ICP.
Methods
Patients with a potential or already known diagnosis of IIH were investigated according to departmental protocol. ICP monitoring was performed for 24 h. When high pressures were confirmed, CT venogram and catheter venography were performed to look for venous stenosis to demonstrate a pressure gradient. If positive, venous stenting would be performed and ICP monitoring would continue for a further 24 h after deployment of the venous stent.
Results
Ten patients underwent venous sinus stenting with concomitant ICP monitoring. Nine out of ten patients displayed an immediate reduction in their ICP that was maintained at 24 h. The average reduction in mean ICP and pulsatility was significant (p = 0.003). Six out of ten patients reported a symptomatic improvement within the first 2 weeks.
Conclusions
Venous sinus stenting results in an immediate reduction in ICP. This physiological response to venous stenting has not previously been reported. Venous stenting could offer an alternative treatment option in correctly selected patients with IIH.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Idiopathic intracranial hypertension (IIH) was first described in the 1890s by a German physician, Quincke, and was named ‘meningitis serosa’ [21]. It is described as a condition characterised by increased intracranial pressure (ICP) in the absence of any central nervous system disease or structural abnormality and by normal CSF composition. In the past decade several potential interacting causes have been identified [10], including venous sinus stenosis [5].
Venous sinus stenosis and raised venous pressure are frequently observed in patients diagnosed with IIH [15, 16]. The stenoses occur predominantly in the transverse sinus [6, 19]. The occlusion in venous outflow is believed to lead to a state of chronically raised CSF and intracranial pressure by resisting CSF absorption. This leads to a state of ‘self-sustained venous collapse’, which creates a cycle of increasing intracranial pressure and venous stenosis [5]. It is unclear in IIH, however, what is cause and what is effect. An iatrogenic cause of saggital sinus compression within our own institution resulted in a clinical picture of IIH that resolved with decompression [15]. Despite this, the relationship between venous stenosis and raised intracranial pressure remains unclear, particularly as to whether venous stenosis is a cause or consequence of raised intracranial pressure in IIH. Further work is required to understand the dynamic of the relationship between ICP and venous stenosis. Several other mechanisms to explain raised ICP in IIH have also been considered, such as increased CSF production and idiopathic brain swelling [1, 9, 11].
In patients who have demonstrated venous sinus stenosis and an associated pressure gradient across the stenosis there has been a growing body of evidence that endovascular stenting reduces this pressure gradient [10], but the correlation with clinical outcome remains unclear. Furthermore it has not yet been identified how long venous stenting takes to affect intracranial pressure, if at all.
Part of the assessment for suitability involves CT or MR imaging of the venous sinuses and a subsequent catheter venogram whereby pressure measurements are taken [11]. In cases of successful venous stenting, the pressure gradient resolves, and this improvement in venous pressure is taken as a surrogate metric for ICP [8]. Prior larger studies have used subjective markers to assess and quantify improvement. This includes patient-reported outcome measures such as headache scores [27, 29]. The duration in which symptoms of IIH improve or deteriorate is highly variable and not reported in the literature. A reliable time frame for assessment of improvement is not clear. The presence of papilloedema has also been used but this has been criticised as an inaccurate measure [20].
The venous pressure gradient can be seen to be obliterated immediately after stent insertion. To date there has been only one case described in the literature of concomitant intracranial pressure monitoring during venous sinus stenting using an intraparenchymal pressure monitor [8]. There was an immediate improvement in intracranial pressure that correlated to improved neurological function. Direct measurement of intracranial pressure provides an objective quantitative outcome that can be used to assess the efficacy of venous sinus stenting.
We describe a series of ten cases in which venous sinus stenting was performed with real-time intraparenchymal pressure monitoring. We investigated whether eliminating the pressure gradient across a cerebral venous stenosis in patients with IIH led to an immediate reduction in intracranial pressure.
Methods
Ethical approval for this protocol was obtained from the local ethics committee. The protocol was developed in response to patient feedback and in a service improvement project to streamline the assessment and eventual treatment for patients with IIH.
Patient selection
Patients referred or already known to the neurosurgical department with a diagnosis of IIH were assessed using a standardised protocol and other causes of their symptoms were excluded. This process included lumbar puncture for assessment of opening pressure and CSF constituents. All patients included in this study had been reviewed by a neuro-opthalmologist and were commenced on acetazolamide in the first instance.
CT or MR imaging was used to exclude enlarged ventricles and venous sinus thrombosis. Dedicated CT or MR venography was also performed for each of these patients to look for a possible venous sinus stenosis. In all ten cases there was a suspicion on non-invasive imaging that there was a point of stenosis. All patients were admitted for 24 h of ICP monitoring, which confirmed raised intracranial pressures. All patients with an average ICP of greater than 4.5 mmHg in a 24-h period were included. CSF constituents were checked and found to be normal in all subjects. Spiegelberg probes were used in all patients and inserted according to an agreed-upon protocol. A stab incision anterior to Kocher’s point on the right hand side was performed and a hand-twist drill was used to create the twist-drill hole. The dura was pierced through this hole and a Spiegleberg bolt screwed into place. The pressure monitor was then advanced to the pre-determined length. The probe was then plugged into the ICP monitor and the difference between systolic and diastolic ICP was checked prior to proceeding. An encircling silk purse string suture was used around the bolt entry site.
ICP monitoring continued until all patients underwent catheter venography and manometry to demonstrate venous sinus stenosis and a pressure gradient across the stenosis was confirmed. In cases with bilateral venous sinus stenosis pressure gradients were measured across both sides, and the the side with the greatest pressure gradient was stented in the first instance. Catheter venography was performed under local anaesthetic to confirm a pressure gradient existed prior to intervention under general anaesthetic. Pressure measurements were taken at the saggital sinus, transverse sinus, sigmoid sinus, internal jugular and within the inferior vena cava. The pressure gradient was calculated as the difference between the proximal and distal measurements to the stenosis.
All patients were discussed in a multi-disciplinary team meeting. If a pressure differential was identified on venography patients were given the choice of undergoing venous sinus stenting or CSF diversion surgery after explanation of the risks of each procedure. All patients who were offered sinus stenting chose this over CSF diversion therapy. The CSF diversion therapy that was offered was ventricular shunting surgery. All patients included in this study gave informed consent themselves.
Patients then underwent endovascular sinus stenting under general anaesthetic during the same admission. The ICP probe was kept in situ for all patients. ICP monitoring was recorded during the procedure and for the next 24 h. Recorded ICP data included: mean ICP during day and night, systolic and diastolic ICP means, and ICP pulsitility. Data were also collected on the frequency of spikes in ICP above 25 mmHg. All patients had another catheter venogram at a 3-month follow-up appointment. Data were processed using ICM and Excel. ICP was considered abnormal by assessing the pulsitility and mean over 24 h. A raised ICP was taken as 4.5 mmHg or above.
Ten patients were identified who underwent the complete selection process with an ICP bolt in situ. Three patients were excluded from this study because of incomplete data collection following stent insertion. In one case the ICP probe was removed at the end of the stenting procedure and in two cases the patient was not re-connected for data analysis immediately after the procedure.
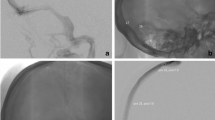
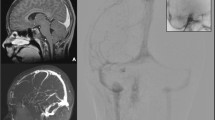
Stent placement technique and details
A 0.088″ Neuronmax long sheath was positioned in the distal sigmoid sinus. A venogram was then performed with a 0.027″ microcatheter and pre-stenting pressure measurements were performed. The length of the stent used was determined by measurement using a microcatheter.
By using a stiff 0.014″ microwire (usually a Platinum Plus microwire), the chosen carotid Wallstent was navigated past the stenosis and then deployment began. The carotid Wallstent was felt to offer the greatest degree of flexibility without compromising radial force. It was sometimes required to advance the Neuronmax long sheath past the stenosis if the carotid Wallstent could not pass the stenosis. A post-stenting venogram was performed to check apposition of the stent to the vessel wall. A balloon angioplasty is rarely required. Post-stenting venogram is then performed to check resolution of the pressure gradient. The patient is usually given IV 500 mg aspirin after deployment of the stent and then lifelong oral aspirin 75 mg daily from the next day. No patient in this study experienced complications from this procedure.
Figures 1, 2 and 3 show venous stent insertion.
Results
All patients in this study had the pressure gradient across the venous sinus stenosis obliterated. In all ten patients obliteration of the venous pressure gradient resulted in a sustained drop in their mean intracranial pressure for the 24 h of measurement that followed stenting in nine out of the ten cases. Similarly, there was a drop in the ICP pulse amplitude in all but one case.
Table 1 shows the venous pressures and ICP data for each patient before and after stenting.
Table 2 outlines the ten patients included in this study. These were consecutive patients undergoing venous sinus.
Figure 4 displays the mean ICP for each patient pre- and post-insertion of the venous stent.
Figure 5 displays the pulse amplitude ICP for each patient pre- and post-insertion of the venous stent.
Figure 6 displays the pre- and post-stenting mean ICP, pulsitility and number of ICP peaks for all ten patients.
Paired two-tailed T-test was performed to assess for statistical significance. Change in mean ICP following stenting was significant (p = 0.00393). Similarly, the change in ICP pulsitility was also found to be statistically significant (p = 0.00445).
Discussion
This is the first case series of patients who have undergone venous sinus stenting for IIH with real time ICP monitoring. In nine of the ten patients in this series there was a significant reduction in mean ICP, pulse amplitude and number of ICP spikes in the first 24 h following stent insertion. Such a clear physiological response to sinus stent insertion has only been reported in one case previously [8]. This study displays clearly that this phenomenon is reproducible in correctly selected patients.
In our case series, one patient did not see an improvement in their mean ICP. In addition to this there was an insignificant rise in ICP pulsitility. This patient was of a similar age as other patients and had a pressure gradient that was significant and seen to be obliterated following insertion of the venous stent. However, this patient, subject nine, was phenotypically different. The average BMI in this group was 34. Patient nine had a BMI of 26. Although this is still considered overweight it raises the possibility of alternative mechanisms causing high intracranial pressure. The venous stenosis seen may be a secondary phenomenon. It is likely that IIH is a common end point with more than one aetiology. In our study 90% of our patient cohort experienced an immediate drop in their ICP. The implication is that venous sinus stenosis is the primary cause of raised ICP in the majority of patients with IIH. Further studies evaluating other potential causes of IIH may allow us to further refine the selection criteria for venous sinus stenting in IIH.
The average BMI of our patient cohort was 34: 20% (2 patients) had a BMI greater than 40. Bariatric services have been used for IIH patients at our institution in the past, with some good outcomes; however bariatric surgery remains surgically challenging with higher complication rates. In this cohort no patients underwent bariatric intervention. The relationship between raised ICP and BMI is likely to be as a result of impeding venous drainage. Patients with raised BMIs at our institution have also been shown to have raised inferior vena-caval pressures. Other studies have also shown raised pleural and cardiac filling pressures associated with raised BMI in patients with IIH [24]. One possible explanation for the patient who failed to show a significant reduction in mean ICP and pulsitility is the underlying pathological process leading to the phenotype of IIH. Whereas every other patient in this study had a grossly elevated BMI, this patient did not. A grossly elevated BMI can explain the reduced venous outflow and subsequent rise in ICP that is seen in IIH and that is amenable to venous stenting. If BMI is not contributing to the raised venous pressures then it is likely the elevated ICP is driving the raised venous pressures rather than the other way around. There are also other factors to consider with regard to the aetiology of venous stenosis or obstruction. IIH is mimicked by venous sinus thrombosis. Post-infective changes and scarring may also cause a long-term stenosis. However within this study no patients had any convincing clinical or radiological features of this. In the absence of any primary venous pathology, however, CSF diversion is more likely to have an effect on reducing ICP than improving venous outflow. Of course, further research is required into the exact pathogenesis of the raised ICP in these patients.
Other possible causes for failure to resolve elevated ICP with venous sinus stenting is the morphology of the stenosis. In our series, patient 9 had bilateral transverse sinus stenosis, and failure to resolve may have been due to an insufficient increase in venous outflow with unilateral stenting. The stenosis also extended across a greater length of the transverse sinus. This again may signify the rise in ICP to be generated from an intraparenchymal pathology rather than a primary venous abnormality.
Until now, the argument behind venous sinus stenting for IIH was based on an elimination of the venous pressure gradient associated with variable improvement in symptoms in these patients. Presence of papilloedema and reduction in reported symptoms of IIH have also been used as measures of symptomatic improvement [1]. Our study has investigated the relationship between a reduced venous pressure gradient and its correlation with ICP. The timing of change in ICP was previously not known following reduction in venous pressure. We have demonstrated that the ICP change is immediate and sustained for at least 24 h.
The time span in which ICP is reduced by venous sinus stenting has not previously been reported in the literature. The rapid reduction in ICP seen in these patients may provide a unique insight into the unanswered question of the relationship between ICP and venous stenosis. If there is an immediate reduction in ICP, this may suggest that it is the venous stenosis itself that has lead to a raised intracranial pressure in that individual. When there is no drop in ICP with stenting it may be the case that venous stenosis is a secondary phenomenon, as seen in patient 9. Studies have shown, using dedicated MRI imaging techniques, that venous sinus calibre is associated with ICP [7]. This adds to the argument that ICP and venous stenosis are related and proportional. This creates a cycle, and we believe the key to breaking this cycle is to understand the pathogenesis behind it.
The prevalence of venous sinus stenosis in patients diagnosed with IIH is widely variable in the literature, with rates ranging from 23 to 80% [4, 13]. Within our own practice, the incidence of venous sinus stenosis in patients with IIH is currently 30%; however this only accounts for patients under the neurosurgical team. Those assessed prior to 2011 were rarely investigated for venous stenosis. It is likely that the percentage of IIH patients with venous stenosis is much higher than our own data would suggest. Investigating patients with CT and MR venography could offer a successful treatment option for a significant proportion of patients with IIH.
There is a potential haemorrhagic risk with performing catheter venous angiography and stenting with an intraparenchymal ICP bolt in situ as a result of the heparinisation or intraprocedural IV aspirin that is often required. This is a theoretical risk but in practice has not been observed. Our protocol did not necessitate pre-medication with anti-platelets for this reason. Patients undergoing endovascular coiling following aneurysmal subarachnoid haemorrhage are frequently heparinised and have been done with ICP bolts in situ, with no such complications. A previously reported complication from venous sinus stenting is an ipsilateral frontal headache. This is thought to be secondary to dural stretching from the stent and has been observed in our patient population. This can be successfully managed with neuropathic pain medication, such as gabapentin, and we now use this prophylactically [1].
Stenting procedures are done under general anaesthetic. The use of sedation and paralysis leads to significantly reduced intracranial and venous pressures during the procedure. For this reason the diagnostic venography should be done under local anaesthesia to avoid the risk of a false-negative investigation. A pressure gradient can still be demonstrated under general anaesthesia and this gradient is reduced once the stent is deployed.
In the majority of patients with IIH maximal medical therapy and repeated lumbar punctures are enough to control symptoms. Surgical intervention including CSF diversion, optic nerve sheath fenestration or sub-temporal decompression has been reserved for patients where maximal medical management has failed to control their symptoms. First-line surgical intervention has traditionally been with CSF diversion therapy (i.e. ventriculo-peritoneal or lumbo-peritoneal shunting). This is associated with numerous complications including: shunt migration, dislocation, infection, intracerebral haemorrhage and acquired Chiari malformation [25, 28]. Patients frequently require repeated admissions and further operations for shunt complications. Complications and shunt failure rates within 6 months have been reported as high as 64% [23]. Optic nerve sheath fenestration has complication rates as high as 40% [3]. Venous sinus stenting is a viable alternative that has repeatedly reported reduced complication rates [1]. This has been echoed in our own experience by patient choice; every patient that was offered venous stenting in this study consented to this over surgical intervention.
Within our patient cohort, two patients (5 and 6) had pre-operative ICP readings of 7.1 and 6.9 mmHg respectively. Pre-operative ICP was considered high if mean ICP after 24 h of monitoring was greater than 4.5 mmHg. The value of 4.5 mmHg is derived from our experience of elective ICP monitoring in over 400 patients, and furthermore recently published data have shown that a 24-h period of monitoring using this protocol gives an accurate representation of ICP and pulse amplitude when compared to longer periods of monitoring [26].
More recent studies have shown that in elective ICP monitoring in mobile patients (who spend much of the day in the upright position and ambulatory), the mean ICP is often much lower over 24 h when compared to supine patients undergoing ICP monitoring or ICP as derived from lumbar puncture. This has resulted in fewer patients returning to theatre [16]. For patients 5 and 6, we still see a reduction in mean ICP as well as pulsitility. The decision to treat required a multidisciplinary team approach and consideration of symptoms in conjunction with ICP.
The monitoring of ICP in a repeated fashion is essential in the assessment of many neurosurgical disorders [2]. Current views on raised ICP and what is considered ‘normal’ are based almost entirely on data in supine patients [17]. Furthermore, ICP has been traditionally derived from lumbar punctures or intracranial ICP monitoring in hospital [22]. These patients are invariably supine when it seems clear that posture clearly plays a role in altering ICP. This has been elucidated in studies on patients with head injury in neuro-intensive care [18] as well as in patients with shunts [14] or undergoing intracerebral surgery [12]. The relationship between ICP and posture, however, has rarely been considered in patients with IIH or normal controls. Current studies on the management of IIH still largely derive their ICP from lumbar punctures.
Conclusion
Nine out of ten patients with IIH who completed the full assessment process showed a decrease in their ICP measurements immediately following stenting of a venous sinus stenosis. This was sustained over a further 24 h of monitoring. This reduction in ICP shows that eliminating a venous sinus pressure gradient in patients with IIH immediately reduces the intraparenchymal pressure in the short term. The ability to reproduce the effect of immediate reduction in ICP following venous stenting in a series of patients has not been previously reported in the literature and provides insights into the pathophysiology of the condition.
References
Ahmed RM, Wilkinson M, Parker GD, Thurtell MJ, Macdonald J, McCluskey PJ, Allan R, Dunne V, Hanlon M, Owler BK, Halmagyi GM (2011) Transverse sinus stenting for idiopathic intracranial hypertension: a review of 52 patients and of model predictions. Am J Neuroradiol 32(8):1408–1414
Andresen M, Hadi A, Petersen LG, Juhler M (2015) Effect of postural changes on ICP in healthy and ill subjects. Acta Neurochir 157:109–113
Brazis PW (2009) Clinical review: the surgical treatment of idiopathic pseudo tumour cerebri (idiopathic intracranial hypertension). Cephalgia 28:1361–1373
De Simone R, Ranieri A, Montella S, Marchese M, Persico P, Bonavita V (2012) Sinus venous stenosis, intracranial hypertension and progression of primary headaches. Neurol Sci 33 Suppl 1:S21–5
De Simone R, Ranieri A (2010) Advancement in idiopathic intracranial hypertension pathogenesis: focus on sinus venous stenosis. Neurol Sci 31:S33–S39
Donaldson JO (1981) Pathogenesis of pseudotumor syndromes. Neurology 31:877–880
Farb RI, Vanek I, Scott JN, Mikulis DJ, Willinsky RA, Tomlinson G, terBrugge KG (2003) Idiopathic intracranial hypertension the prevalence and morphology of sinovenous stenosis. Neurology 60(9):1418–1424
Fargen KM, Velat GJ, Lewis SB, Hoh BL, Mocco J, Lawson MF (2013) Concomitant intracranial pressure monitoring during venous sinus stenting for intracranial hypertension secondary to venous sinus stenosis. J Neurointervent Surg 5:e22. doi:10.1136/neurintsurg-2012-010371
Fishman RA (1984) Pathophysiology of pseudotumour cerebri. An unsolved puzzle [editorial]. Arch Neurol 41:257–258
Friedman DI, Jacobson DM (2004) Idiopathic intracranial hypertension. J Neuroophthalmol 24:138–145
Higgins JNP, Cousins C, Owler BK, Sarkese N, Pickard JD (2003) Idiopathic intracranial hypertension: 12 cases treated by venous sinus stenting. J Neurol Neurosurg Psychiatry 74(12):1662–1666
Hung OR, Hare GM, Brien S (2000) Head elevation reduces head-rotation associated increased ICP in patients with intracranial tumours. Can J Anaesth 47(5):415–420
Ibrahim MH, Zeid SHA, Elbar AA (2014) Prevalence of venous sinus stenosis in Pseudotumour cerebri (PTC) using digital subtraction angiography (DSA). Egypt J Radiol Nucl Med 45:519–522
Kajimoto Y, Ohta T, Miyake H, Matsukawa M, Ogawa D, Nagao K, Kuroiwa T (2000) Posture related changes in the pressure environment of the ventriculoperitoneal shunt system. J Neurosurg 93(4):614–617
Karahalios DG, Rekate HL, Khayata MH, Apostolides PJ (1996) Elevated intracranial venous pressure as a universal mechanism in pseudotumour cerebri of varying etiologies. Neurology 46:198–202
King JO, Mitchell PJ, Thomson KR, Tress BM (1995) Cerebral venography and manometry in idiopathic intracranial hypertension. Neurology 45:2224–2228
Lilja A, Andresen M, Hadi A, Christoffersen D, Juhler M (2014) Clinical experience with telemetric intracranial pressure monitoring in a Danish neurosurgical center. Clin Neurol Neurosurg 120:36–40
Ng I, Lim J, Wong HB (2004) Effects of head posture on cerebral haemodynamics: its influences on intracranial pressure, cerebral perfusion pressure, and cerebral oxygenation. Neurosurgery 54(3):593–597
Owler BK, Parker G, Halmagyi GM, Johnston IH, Besser M, Pickard JD, Higgins JN (2005) Cranial venous outflow obstruction and pseudotumour cerebri syndrome. Adv Tech Stand Neurosurg 30:107–174
Padhye LV, Van Stavern GP, Sharma A, Viets R, Huecker JB, Gordon MO (2013) Association between visual parameters and neuroimaging features of idiopathic intracranial hypertension. J Neurol Sci 332(1–2):80–85
Quincke H (1893) Meningitis serosa. Sammlung Klinischer Vortrage 67:655
Raboel PH, Bartek J, Andersen M, Bellander BM, Romner B (2012) Intracranial pressure monitoring: invasive versus non-invasive methods—a review. Crit Care Res Pract
Rosenberg ML, Corbett JJ, Smith C, Goodwin J, Sergott R, Savino P, Schatz N (1993) Cerebrospinal fluid diversion procedures in pseudotumour cerebri. Neurology 43:1071–1072
Sugerman HJ, DeMaria EJ, Felton WL 3rd, Nakatsuka M, Sismanis A (1997) Increased intra-abdominal pressure and cardiac filling pressure in obesity-associated pseudotumour cerebri. Neurology 49(2):507–511
Suri A, Pandey P, Mehta VS (2002) Subarachnoid hemorrhage and intracerebral haematoma following lumboperitoneal shunt for pseudotumour cerebri: a rare complication. Neurol India 50:508–510
Thompson SD, Coutts A, Craven CL, Toma AK, Thorne LW, Watkins LD (2017) Elective ICP monitoring: how long is long enough? Acta Neurochir. doi:10.1007/s00701-016-3074-z
Thurtell MJ, Bruce BB, Newman NJ, Biousse V (2010) An update on idiopathic intracranial hypertension. Rev Neurol Dis 7:e56–e68
Wang VY, Barbaro NM, Lawton MT, Pitts L, Kunwar S, Parsa AT, Gupta N, McDermott MW (2007) Complications of lumboperitoneal shunts. Neurosurgery 60:1045–1048
Yri HM, Ronnback C, Wegener M, Hamann S, Jensen RH (2014) The course of headache in idiopathic intracranial hypertension: a 12-month prospective follow-up study. Eur J Neurol 21(12):1458–1464
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflicts of interest
All authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licencing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Matloob, S.A., Toma, A.K., Thompson, S.D. et al. Effect of venous stenting on intracranial pressure in idiopathic intracranial hypertension. Acta Neurochir 159, 1429–1437 (2017). https://doi.org/10.1007/s00701-017-3229-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3229-6