Abstract
Background
Selective amygdalohippocampectomy (SAH) is an accepted surgical procedure for treatment of pharmacoresistant mesial temporal lobe epilepsy, but it may lead to postoperative visual field deficits (VFDs). Here we present a prospective randomised trial comparing the postoperative VFDs after either a trans-sylvian or temporobasal approach for SAH.
Method
Forty-eight patients were randomly assigned to trans-sylvian (n = 24) or temporobasal (n = 24) SAH. Postoperative VFD were quantitatively evaluated using automated static and kinetic perimetry. In 24 cases, diffusion tensor imaging-based deterministic fibre-tracking of the optic radiation was performed. The primary endpoint was absence of postoperative VFD. The secondary endpoint was seizure outcome and driving ability.
Results
Three patients (13 %) from the trans-sylvian group showed no VFD, compared to 11 patients (46 %) from the temporobasal group without VFD (p = 0.01, RR = 3.7; CI = 1.2–11.5). Fifteen patients from each group (63 %) became completely seizure-free (ILAE1). Among those seizure-free cases, five trans-sylvian (33 %) and ten temporobasal (66 %) patients could apply for a driving licence (NNT = 3) when VFDs were considered. Although the trans-sylvian group experienced more frequent VFDs, the mean functional visual impairment showed a tendency to be less pronounced compared with the temporobasal group. DTI-based tracking of the optic radiation revealed that a lower distance of optic radiation to the temporal base correlated with increased rate of VFD in the temporobasal group.
Conclusions
Temporobasal SAH shows significantly fewer VFDs and equal seizure-free rate compared with the trans-sylvian SAH. However, in patients in whom the optic radiation is close to the temporal base, the trans-sylvian approach may be a preferred alternative.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intractable epilepsy is a common neurological disease [29] leading to cognitive impairment, diminished quality of life and lower life expectancy [2, 31]. Surgery for drug-resistant epilepsy is an effective and well-accepted treatment option for seizures arising from the mesial temporal cortex (MTLE) with proven better results than drug treatment alone [34].
The main goal of epilepsy surgery is to achieve seizure freedom without causing neurological impairments [30]. However, a common problem after surgery for MTLE is the occurrence of visual field deficits (VFDs) after damaging the optic radiation and, more specifically, its most anterior part, “Meyer’s loop” [9, 38]. The Meyer’s loop shows a great anatomical variability between subjects and cannot be delineated on a conventional magnetic resonance imaging (MRI) [7, 28]. This explains the significant uncertainty about its exact location, thus making it difficult to preserve during surgery. Consequently, the reported rate of VFD in the literature varies widely from 3 to 91 % [13, 37, 38]. This is a major issue, as VFD can preclude driving in up to 50 % of the patients, depending on variable national regulations for driving with VFD [4, 19, 22, 26]. Recent advances in the visualisation of fibre tracts using DTI (diffusion tensor imaging) have achieved a better understanding of the optic radiation and Meyer’s loop, enabling the possibility to actively avoid their damage during surgery [36, 39].
Throughout the years, different procedures have been introduced for MTLE surgery. The most commonly used surgical procedure is the anterior temporal lobe resection (ATLR), initially developed by Penfield et al. [25], Bailey et al. [1] and Falconer et al. [10]. Selective amygdalohippocampectomy (SAH) represents an alternative to ATLR for treatment of MTLE, showing rather similar postoperative seizure outcome [11] although recently an advantage for ATLR concerning the seizure outcome was described [14]. Although initially hoped that the more “selective” nature of SAH would lead to less VFD, recent works could not confirm this assumption [8, 22]. Therefore, different approaches, hoping to be less harmful to the optic radiation [41], have been introduced. An example of such an attempt is the subtemporal approach described by Hori et al. [12], leading to a visual field impairment in 20 % of patients. The rationale of this approach is the idea that a surgeon may resect the mesial temporal structures going temporobasal, underneath the optic radiation, thus avoiding the highly variable extension of Meyer’s loop.
Despite the fact that VFD after MTLE surgery has been described for decades, it was only recently that prospective data concerning VFD after ATLR was presented [36, 37]. Unfortunately, in regard to VFD after SAH, most studies have been retrospective in nature and lack objective evaluation criteria. More importantly, to our knowledge, direct comparisons between the main approaches for SAH (transcortical, trans-sylvian and temporobasal/subtemporal) have mainly investigated neuropsychological or seizure outcome without regarding postoperative VFD [18, 24, 27].
Here, we report a prospective randomised trial comparing two different approaches (trans-sylvian and temporobasal/subtemporal) for SAH and present comprehensive results concerning postoperative VFDs and final seizure outcome.
Materials and methods
Patient cohort, randomisation and study design
The purpose of this study was to compare VFD and seizure outcome after trans-sylvian or temporobasal approach for SAH in patients with MTLE. The study was part of a trans-regional collaborative research project (Sonderforschungsbereich SFB TR3). This part was to evaluate differences in cognition and VFDs after two different approaches for SAH. The randomised study was reviewed and approved by the reviewers of the German Research Council (Deutsche Forschungsgemeinschaft (DFG), http://gepris.dfg.de/gepris/projekt/5336202) and the local ethics committee. A total of four surgeons performed the procedures and all patients underwent surgery at the Department of Neurosurgery, University Hospital of Bonn, Germany, from August 2009 until December 2012.
Presurgical assessment was performed in all patients using a standard protocol.[15] Eligible patients were at least 18 years of age, had drug-resistant MTLE, and, after presurgical assessment, were recommended for resection of the mesial temporal structures. Prior to surgery, all patients underwent a visual acuity and visual field examination. Both approaches for resection of mesial temporal structures were explained. After informed consent, patients were then consecutively randomised to either the trans-sylvian or temporobasal approach. A computer-generated randomisation list was used and the randomised approach was communicated to the surgeon after the patient was brought to the operation room, just before surgery. A postoperative visual acuity and visual field examination were performed just prior to discharge in all patients. Postoperative follow-up was at least 1 year in all patients. Patients with other types of temporal resections or pre-existing VFD were excluded from the study.
The primary endpoint was the absence of VFD. Secondary endpoints were seizure outcome, driving ability and severity of the VFD. Thus, the main purpose was the analysis of VFDs present caused by direct or indirect surgical damage to the optic tract. A general review of the surgical techniques and associated problems was not intended.
DTI acquisition and visualisation of the optic radiation
MRI and DTI sequences were acquired on a Philips 3-T Intera MR System (Philips Medical Systems, Best, The Netherlands) with a standard epilepsy-specific protocol described elsewhere [32]. Deterministic tractography of the optic radiation was performed on the Brainlab Navigation Station (Brainlab, Feldkirchen, Germany). For that purpose, a seeding mask was selected in the beginning of the optic tract, just a behind the optic chiasm. Another seeding mask was placed to cover the lateral geniculate nucleus (LGN) [5]. A third, “way through” mask, lateral to the wall of the occipital horn of the lateral ventricle, was used to retain the passing fibres. The minimum fractional anisotropy threshold was 0.2 and a minimum fibre length was 50.
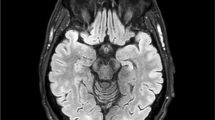
Surgical approach (Fig. 1)
The trans-sylvian approach was first described by Yasargil et al. in 1985. Briefly, after pterional trepanation and a trans-sylvian approach, the surgeon reaches the temporal horn of the lateral ventricle via the inferior limiting sulcus. The white matter of the anterior temporal stem was dissected about 1.5-1.7 cm. Once in the ventricle, the choroid plexus with the choroidal point was identified. After that, the uncus was emptied, and the amygdala and hippocampus were disconnected from surrounding structures and removed subpially as an en bloc specimen.
a A schematic visualisation of the optic tract based on Ebeling et al.[7] and Yamamoto et al. [40] The yellow dashed ovals represent areas at risk after trans-sylvian or temporobasal approach. While the trans-sylvian approach would mostly damage the Meyer’s loop, the damage inflicted by the temporobasal approach is more mesial and posterior and could affect the optic radiation bundle. b Trans-sylvian approach and c temporobasal approaches present the optic radiation (yellow), delineated in two different patients before surgery. After image fusion, the optic radiation has been transferred to the postoperative MRIs (coronal T2 images). The purple points on the axial images and their corresponding localisation on the coronal T2 images show the areas, where the optic radiation has been compromised by the resection cavity. CGL corpus geniculate laterale
The subtemporal approach for SAH has been described in various publications [12]. Thudium et al. [32] summarised the landmarks of this approach as used in our study. A 3.5 × 3-cm anterior basal temporal trepanation, followed by slight retraction of the temporal lobe, allowed entry into the anterior temporal horn of the lateral ventricle via a corticotomy of about 2 cm in the fusiform gyrus guided by a neuronavigation system. After that, the mesial structures of the temporal lobe were resected. In this study we have introduced the term of temporobasal approach because in a small subgroup of patients the entrance into the temporal horn of the ventricle could not be achieved purely subtemporally. The reason for this was the anatomy of large temporal basal veins, which did not allow sufficient elevation of the temporal lobe. In order to cope with this problem, the two following modifications of the subtemporal approach were used. (1) Subpial approach: after opening the dura, the basal pia of the inferior temporal gyrus was opened as well. Thereby, the pia remained together with the temporobasal veins detached to the dura of the temporal base. (2) If the elevation of the temporal lobe was still difficult, a small subpial corticectomy, maximally 8–10 mm high at the base of gyrus temporalis inferior, was performed. After that, neuronavigation was used to find the adequate trajectory for entering the ventricle. Thus, the term “temporobasal approach” includes the individualised approach, either purely subtemporal or with a subpial or even basal transcortical dissection to reach access to the temporal horn.
Visual field testing and evaluation of visual field deficits (VFD)
Preoperative and postoperative visual field testing was performed monocularly in all patients using automated perimetry. Until the year 2010, this was performed using the Humphrey Field Analyzer (Humphrey, Dublin, OH, USA) with a two-zone strategy on 120 test locations within the central 60° of the visual field. In 2011, recommendations for standardised perimetry in the framework of epilepsy surgery were published [17], which included the additional testing of kinetic stimuli corresponding to Goldmann stimuli III/4. According to these, visual field testing was then performed using a Twinfield perimeter (Oculus, Wetzlar, Germany), which is able to perform automated static and kinetic perimetry within one testing. The functional impairment of visual field defects is greater for defects located centrally and in the lower part of the visual field. A pure mathematical indication of the area of defect within the whole visual field would, therefore, not reflect the usefulness of the remaining visual field for the patient.
Therefore, we used a modified Estermann scheme to assess the functional impairment [23, 33]. This is widely used in Germany in experts’ opinions about visual field defects. The visual field area is divided into 100 score areas, which are smaller in the visual field centre and its lower region, respectively, to account for the greater functional importance of these areas. The functional impairment is then calculated as the sum of the areas, which have not been seen by the patient (scotomas). The higher the score, the more pronounced is the VFD. Therefore a complete homonymous hemianopia would give 50 % of functional visual impairment, a complete homonymous quadrantanopia of the upper quadrant 20 %, of the lower quadrant 30 %.
Last, the visual fields of the patients were rated according to the German driving criteria. When homonymous visual field defects are present (for Goldmann stimulus III/4), the central 20° of the visual field have to be normal with no scotoma. Therefore, patients with complete homonymous hemianopia or quadrantanopia are not allowed to drive. In patients with VFD with incomplete quadrantanopia where the central 20° are normal, the horizontal extent of the visual field has to be at least 120°, so that a horizontal area of 30°, at least 10° up and downwards of the horizontal meridian, has to be free of scotoma.
Seizure outcome
Seizure outcome was evaluated according to the ILAE classification [35]. The mean follow-up was 30 months (12–61 months).
Statistics
Statistical analysis was performed using a conventional chi-squared test for the categorical variables. Mean values of VFD (absolute values) as well as mean values of distance to the temporal base (millimetres) were compared using two sample t-tests. All tests were two-sided, and statistical significance was set at p ≤ 0.05; 95 % confidential intervals (CIs) were used. All analyses were performed with SPSS software (released 2011, IBM SPSS Statistics for Windows, Version 20.0; Armonk, IBM, NY, USA).
Results
A total of 63 patients underwent SAH for MTLE from August 2009 until December 2012. Fifty-four patients gave informed consent and were included in the study. Twenty-eight patients were randomised to the trans-sylvian and 26 to the temporobasal approach. Six patients (four from the trans-sylvian and two from the temporobasal group) were excluded from the study because they refused postoperative visual field examinations. Thus, 24 randomised patients were further evaluated from each group (Table 1).
VFDs after SAH (trans-sylvian versus temporobasal)
Three patients (13 %) from the trans-sylvian group showed no VFD after surgery, whereas the remaining 21 patients (87 %) had some visual field impairment. Among the temporobasal group, there were 11 patients without any VFDs (46 %) and 13 cases (54 %) with some VFDs (Fig. 2a). The difference between both groups was statistically significant: p = 0.01, RR = 3.7; CI = 1.2–11.5.
As mentioned in “Methods”, visual impairment can be expressed in percent of visual field loss; therefore, we compared the mean amount of lost visual field areas between both groups. A complete homonymous quadrantanopia of the upper quadrant would therefore give a visual impairment of 20 %. The mean amount of functional visual impairment (lost visual field areas) was 15 % for the 21 patients with VFD in the trans-sylvian group and 20 % for the 13 patients in the temporobasal group. Thus the VFDs in the trans-sylvian group seemed to be less prominent; this difference, however, was not statistically significant (p = 0.2, two-sample t-test) (Fig. 3). The two outliers with more extended VFDs in the trans-sylvian group were patients, who developed postoperative temporal lobe infarctions (Fig. 3).
The functional visual impairment due to the surgical resection in percent (VFDs expressed as areas, which have not been recognised during the perimetric examination). The temporobasal group (13 patients with VFDs) shows a tendency for more severe VFDs (mean functional visual impairment 20 %) compared with the trans-sylvian group (21 patients with VFDs, mean functional visual impairment 15 %) (not statistically significant) (p = 0.2). The two outliers represent patients with postoperative temporal lobe infarctions, who developed a greater VFDs due to the ischaemic lesion. Box plots represent 50 % of the values, lines inside the boxes show median values; whiskers show the range (outliers excluded) and remaining 25 % of values
The qualitative evaluation of the severity of postoperative VFDs revealed in the 21 cases of the trans-sylvian group: 17 patients with VFDs in the upper and four patients with VFDs in the upper and lower contralateral quadrant. In the 13 cases of the temporobasal group with VFDs, there were nine patients with VFDs in the upper and four patients with VFDs in the upper and lower contralateral quadrant.
Seizure outcome and car driving
Fifteen patients from each group (63 %) were completely seizure-free (ILAE 1) on the last available outcome (LAO). A detailed comparison of the ILAE outcomes between both groups is presented in Table 1, showing no significant differences in seizure outcome. Five of 15 (33 %) seizure-free patients in the trans-sylvian group could obtain a driving licence (Fig. 2b), when the results from the visual field examination are considered. In contrast, 10 of the 15 (67 %) seizure-free patients from the temporobasal group would be allowed to apply for a driving licence. Thus, the relative risk reduction (RRR) was 50 % with a number needed to treat (NNT) of three, i.e. for every three patients operated on by the temporobasal approach, one additional patient would be allowed to apply for a driving licence. Although the difference between both groups was not significant (p = 0.07), a clear trend in favour of the temporobasal group could be shown.
DTI results (post hoc analysis)
Although DTI delineation of the optic radiation was not a study endpoint and DTI images were not used intraoperatively, the evaluation of the available data helped during the interpretation of the study results. Preoperative DTI examinations were available in 24 patients (10 trans-sylvian and 14 temporobasal). For the 24 cases, the mean distance between the most anterior extent of Meyers loop and temporal pole was 34 mm (23–48 mm).
In the temporobasal group, the optic radiation was localised higher above the temporal base in patients without VFDs (n = 8, 28.8 mm) compared to those who developed VFDs (n = 6, 21.6 mm); and this difference was statistically significant (p = 0.005, two-sample t-test). In the trans-sylvian group the localisation of the optic radiation did not influence the rate of VFD.
Discussion
Rationale of the study
VFDs are common complications after surgery for MTLE (e.g. 3-91 % after ATLR [13, 22]; 37-50 % after trans-sylvian SAH [42] and 79-89 % after transcortical SAH [8, 22]). If severe (e.g. hemianopia), they are a serious neurological impairment. However, even less prominent and not realised by the patient, VFDs affecting the central visual field may negatively impact postoperative quality of life, as they may preclude patients’ ability to acquire a driving licence—often considered the second most important benefit after seizure freedom. Although the risk for VFD is a well-known problem, being as old as epilepsy surgery itself [7, 9, 20], their reliable avoidance remains unsolved.
Recent reports have shown important improvements in VFD reduction after ATLR using DTI visualisation of the optic radiation [36]. VFD after selective amygdalohippocampectomy has been rarely examined [32]. By using the temporobasal approach as an alternative to the classic trans-sylvian approach, one can reach the mesial structures going beneath the optic radiation and thus potentially reduce the risk of VFD.
Key findings
The temporobasal approach helped to minimise the risk of damaging the optic radiation (p = 0.01). There was no difference in the seizure outcome between both groups. In each group, 63 % of the patients were completely seizure free (ILAE1; Engel Class IA) at last available outcome.
Another important result was the number of seizure-free patients who could apply for a driving licence after surgery. Sixty-seven percent of the seizure-free patients were able to drive again after temporobasal SAH compared with only 33 % of the seizure-free patients after trans-sylvian SAH, when the German driving guidelines were applied. The importance of this difference is highlighted by the fact that every three seizure-free patients treated by temporobasal SAH, result in one additional patient, who would be able to drive (NNT = 3). Although this difference did not reach statistical significance, this is a positive trend concerning one of the dearest desires of epilepsy patients with a great impact on quality of life and deserves further study.
Patients in the temporobasal group had less frequent VFDs overall, but showed a trend to more pronounced functional visual impairment (20 % vs 15 %, Fig. 3). Additionally, the proportion of patients with lower quadrant visual field loss was worse in the temporobasal group, which is a clinically important outcome. This observation implies that although impairment of the optic radiation in the temporobasal group is more unlikely, such damage could harm it more severely, even resulting in more pronounced VFD. The impact of such “strategic lesions” of the optic radiation can be explained by the nature of the approach. The optic radiation may be damaged more mesially and posteriorly during the temporobasal approach, where the visual information of the branches has already been bundled together (Fig. 1a, c), thus causing a VFD including both the upper and lower quadrant. In contrast, the trans-sylvian approach would often damage the Meyer’s loop of optic radiation, mostly resulting in an upper quadrantanopia (Fig. 1a, b). However, the trans-sylvian approach may lead to a vascular event causing a temporal ischaemic lesion [21], thus resulting in greater VFD (more than just the upper quadrant), as it was the case in two of our patients. Our experience, based on more than 600 trans-sylvian SAH surgeries, shows that such large ischaemic lesions are very uncommon. These two events together with the rather large rate of VFDs may have been a consequence of the “learning curve” of two new neurosurgeons being introduced to the epilepsy programme during the time when the study was conducted. The rate of other surgical complications did not differ between the groups and was similar to earlier published results [3, 6].
Finally, in the temporobasal group, the occurrence of VFD was associated with closer distance of the optic radiation to the temporal base (p = 0.005, two-sample t-test), implying that the smaller distance to the temporal base could represent a greater risk of damaging the optic radiation if temporal basal approach is used.
Comparison to other VFD results after SAH
There have been only two small retrospective patient series reporting VFD after temporobasal SAH: Thudium et al. [32] with 25 % VFD (3 of 12 patients) and Hori et al. [12] with 20 % VFD (2 of 10 patients). The difference to the VFD rate reported here (58 %) can be best explained by the larger number of operated-on patients, the learning curves of the two new neurosurgeons and the more rigorous quantitative and standardised evaluation of the visual fields. In order to deliver a clear statement concerning the postoperative VFDs, we assigned only those with an absolutely unimpaired postoperative visual field examination to the group of patients without VFDs. The postoperative VFDs after trans-sylvian SAH in this cohort (88 %) were similar to those reported by Mengesha et al. [22] (89 %) and Egan et al. [8] (79 %).
The evaluation of the VFDs with respect to the driving ability after epilepsy surgery has been examined less frequently.[37] In the studies of Ray et al. [26] and Manji et al. [19], patients were operated on by ATLR, whereas in the study of Beisse et al. [4] a trans-sylvian SAH was performed. Of note, the first two studies are not fully comparable to our data, as the British criteria for obtaining a driving licence are not completely identical to those in Germany. The three studies reported that 54 % [26], 58 % [19] and 50 % [4] of the patients fulfilled the visual field criteria for acquiring a driving licence. These results are better than the one reported here for the trans-sylvian group (33 % of the seizure-free patients), but worse compared to the seizure-free patients from the temporobasal group, of whom 67 % were able to apply for a driving licence after surgery.
Strengths and limitations
To our knowledge, this is the first prospective randomised study examining VFDs after SAH with respect to two of the three most commonly used approaches. By using automated static and kinetic perimetry, an exact and proper evaluation of the visual field was possible. The randomisation of the patients involved only the two approaches and was not influenced or biased by tractography results, which were unknown to the surgeon at surgery, thus providing genuine data concerning the surgical procedures themselves.
However, this study has its limitations, one of them being the small sample size, which may allow for unrecognised statistical uncertainty. Although the difference between both groups concerning the possibility of obtaining a driving licence was presented (showing a statistical trend, p = 0.07), it did not reach statistical significance, most probably due to the relatively small patient number. Despite this fact, an NNT analysis (NNT = 3) was presented demonstrating a potential advantageous trend of the temporobasal approach. However, the limitations caused by the lack of statistical significance should be taken into consideration.
Additional kinetic visual field testing up to 85° was only implemented in 2011; patients examined before were only tested up to 60° eccentricity. None of the patients in the 85° group had isolated VFDts outside 60°. We, therefore, do not think that we missed relevant VFDs in the first patients, which may have influenced study outcome. Furthermore the VFDs were tested in a rather early time-point after surgery, where a postoperative oedema may still be present. Therefore, an examination, performed several months later, would have been more useful.
DTI delineation of the optic radiation was not the primary goal of the study and was not available in all patients. This was also the reason why the DTI evaluation was performed as post hoc analysis. The routine use of probabilistic algorithms was established at our institution after the beginning of the study. Therefore we used a deterministic algorithm to obtain the optic radiation and Meyer’s loop, which has been shown recently to be inferior to probabilistic algorithms [16]. Further limitation was the delineation of optic radiation on the preoperative MRI, which was then transferred to the postoperative MRI, potentially leading to an error, if the image fusion algorithm was not precise enough. The small patient number, in whom DTI was available, does not allow generalisation of the results. Keeping those limitations in mind, the DTI visualisation of the optic radiation should not be stressed as a central aspect of this study. It rather represents an opportunity to discuss a possible explanation of the VFD outcome. However, the availability of DTI visualisation of the optic radiation could have changed the surgical management of the patients in two ways. Firstly, one could be more confident in choosing the adequate trajectory to the ventricle beneath the optic radiation. Secondly, even in a rather small patient number, there was an association between VFD occurrence and shorter distance of the optic radiation to the temporal base, implying the use of a trans-sylvian approach in this subgroup of patients.
Conclusions and result implications
This prospective study shows that a temporobasal approach can contribute to reducing the number of postoperative VFDs after SAH. This consequently results in a positive trend for patient’s driving perspective. However, if a visual impairment occurs, it tends to be more severe in the temporobasal group. In cases with close optic radiation-temporal base distance, the use of a trans-sylvian approach may be a preferred alternative.
References
Bailey P, Gibbs F (1951) The surgical treatment of psychomotor epilepsy. J Am Med Assoc 145(6):365–370
Baker GA, Jacoby A, Buck D, Stalgis C, Monnet D (1997) Quality of life of people with epilepsy: a European study. Epilepsia 38(3):353–362
Behrens E, Schramm J, Zentner J, König R (1997) Surgical and neurological complications in a series of 708 epilepsy surgery procedures. Neurosurgery 41(1):1–10
Beisse F, Lagrèze WA, Schmitz J, Schulze-Bonhage A (2014) Visual field defects after epilepsy surgery. Ophthalmologe 111(10):942–947
Benjamin CFA, Singh JM, Prabhu SP, Warfield SK (2012) Optimization of tractography of the optic radiations. Hum Brain Mapp 35(2):683–697
Clusmann H, Kral T, Gleissner U, Sassen R, Urbach H, Blumcke I, Bogucki J, Schramm J (2004) Analysis of Different Types of Resection for Pediatric Patients with Temporal Lobe Epilepsy. Neurosurgery 54(4):847–860
Ebeling U, Reulen HJ (1988) Neurosurgical topography of the optic radiation in the temporal lobe. Acta Neurochir (Wien) 92(1–4):29–36
Egan RA, Shults WT, So N, Burchiel K, Kellogg JX, Salinsky M (2000) Visual field deficits in conventional anterior temporal lobectomy versus amygdalohippocampectomy. Neurology 55(12):1818–1822
Falconer MA, Wilson JL (1958) Visual field changes following anterior temporal lobectomy: their significance in relation to Meyer’s loop of the optic radiation. Brain 81(1):1–14
Falconer MA, Meyer A, Hill D, Mitchell W, Pond DA (1955) Treatment of temporal-lobe epilepsy by temporal lobectomy; a survey of findings and results. Lancet 268(6869):827–835
Helmstaedter C, Elger CE, Hufnagel A, Zentner J, Schramm J (1996) Different effects of left anterior temporal lobectomy, selective amygdalohippocampectomy, and temporal cortical lesionectomy on verbal learning, memory, and recognition. J Epilepsy 9:39–45
Hori T, Yamane F, Ochiai T, Kondo S, Shimizu S, Ishii K, Miyata H (2007) Selective subtemporal amygdalohippocampectomy for refractory temporal lobe epilepsy: operative and neuropsychological outcomes. J Neurosurg 106(1):134–141
Jeelani NUO, Jindahra P, Tamber MS, Poon TL, Kabasele P, James-Galton M, Stevens J, Duncan J, McEvoy AW, Harkness W, Plant GT (2010) ‘Hemispherical asymmetry in the Meyer’s Loop’: a prospective study of visual-field deficits in 105 cases undergoing anterior temporal lobe resection for epilepsy. J Neurol Neurosurg Psychiatr 81(9):985–991
Josephson CB, Dykeman J, Fiest KM, Liu X, Sadler RM, Jetté N, Wiebe S (2013) Systematic review and meta-analysis of standard vs selective temporal lobe epilepsy surgery. Neurology 80(18):1669–1676
Kral T, Clusmann H, Urbach J, Schramm J, Elger CE, Kurthen M, Grunwald T (2002) Preoperative evaluation for epilepsy surgery (Bonn Algorithm). Zentralbl Neurochir 63(3):106–110
Lilja Y, Ljungberg M, Starck G, Malmgren K, Rydenhag B, Nilsson DT (2014) Visualizing Meyer’s loop: a comparison of deterministic and probabilistic tractography. Epilepsy Res 108(3):481–490
Lutz MT, Mayer T, Schiefer U (2011) Recommendations for a standardized perimetry within the framework of epilepsy surgery. Ophthalmologe 108(7):628–636
Lutz MT, Clusmann H, Elger CE, Schramm J, Helmstaedter C (2004) Neuropsychological outcome after selective amygdalohippocampectomy with transsylvian versus transcortical approach: a randomized prospective clinical trial of surgery for temporal lobe epilepsy. Epilepsia 45(7):809–816
Manji H, Plant GT (2000) Epilepsy surgery, visual fields, and driving: a study of the visual field criteria for driving in patients after temporal lobe epilepsy surgery with a comparison of Goldmann and Esterman perimetry. J Neurol Neurosurg Psychiatr 68(1):80–82
Marino R, Rasmussen T (1968) Visual field changes after temporal lobectomy in man. Neurology 18(9):825–835
Martens T, Merkel M, Holst B, Brückner K, Lindenau M, Stodieck S, Fiehler J, Westphal M, Heese O (2014) Vascular events after transsylvian selective amygdalohippocampectomy and impact on epilepsy outcome. Epilepsia 55(5):763–769
Mengesha T, Abu-Ata M, Haas KF, Lavin PJ, Sun DA, Konrad PE, Pearson M, Wang L, Song Y, Abou-Khalil BW (2009) Visual field defects after selective amygdalohippocampectomy and standard temporal lobectomy. J Neuroophthalmol 29(3):208–213
Mills RP, Drance SM (1986) Esterman disability rating in severe glaucoma. Ophthalmology 93(3):371–378
Olivier A (2000) Transcortical selective amygdalohippocampectomy in temporal lobe epilepsy. Can J Neurol Sci 27(Suppl 1):S68–96
Penfield W, Baldwin M (1952) Temporal lobe seizures and the technic of subtotal temporal lobectomy. Ann Surg 136(4):625–634
Ray A, Pathak-Ray V, Walters R, Hatfield R (2002) Driving after epilepsy surgery: effects of visual field defects and epilepsy control. Br J Neurosurg 16(5):456–460
von Rhein B, Nelles M, Urbach H, von Lehe M, Schramm J, Helmstaedter C (2012) Neuropsychological outcome after selective amygdalohippocampectomy: subtemporal versus transsylvian approach. J Neurol Neurosurg Psychiatr 83(9):887–893
Rubino PA, Rhoton AL Jr, Tong X, de Oliveira E (2005) Three-dimensional relationships of the optic radiation. Neurosurgery 57(Suppl 4):219–227
Sander JW, Shorvon SD (1996) Epidemiology of the epilepsies. J Neurol Neurosurg Psychiatr 61(5):433–443
Spencer S, Huh L (2008) Outcomes of epilepsy surgery in adults and children. Lancet Neurol 7(6):525–537
Sperling MR, Feldman H, Kinman J, Liporace JD, O’Connor MJ (1999) Seizure control and mortality in epilepsy. Ann Neurol 46(1):45–50
Thudium MO, Campos AR, Urbach H, Clusmann H (2010) The basal temporal approach for mesial temporal surgery: sparing the Meyer loop with navigated diffusion tensor tractography. Neurosurgery 67(ONS Suppl 2):385–390
Weber J, Schiefer U, Kolling G (2004) Proposed scoring system for assessment of functional impairment due to visual field defects. Ophthalmologe 101(10):1030–1033
Wiebe S, Blume WT, Girvin JP, Eliasziw M, Effectiveness and Efficiency of Surgery for Temporal Lobe Epilepsy Study Group (2001) A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med 345(5):311–318
Wieser HG, Blume WT, Fish D, Goldensohn E, Hufnagel A, King D, Sperling MR, Lüders H, Pedley TA, Commission on Neurosurgery of the International League Against Epilepsy (ILAE) (2001) ILAE Commission Report. Proposal for a new classification of outcome with respect to epileptic seizures following epilepsy surgery. Epilepsia 42(2):282–286
Winston GP, Daga P, White MJ, Micaleff C, Miserocchi A, Mancini L, Modat M, Stretton J, Sidhu MK, Symms MR, Lythgoe DJ, Thornton J, Yousry TA, Ourselin S, Duncan JS, McEvoy AW (2014) Preventing visual field deficits from neurosurgery. Neurology 83(7):604–611
Winston GP (2013) Epilepsy surgery, vision, and driving: What has surgery taught us and could modern imaging reduce the risk of visual deficits? Epilepsia 54(11):1877–1888
Winston GP, Daga P, Stretton J, Modat M, Symms MR, McEvoy AW, Ourselin S, Duncan JS (2012) Optic radiation tractography and vision in anterior temporal lobe resection. Ann Neurol 71(3):334–341
Winston GP, Yogarajah M, Symms MR, McEvoy AW, Micallef C, Duncan JS (2011) Diffusion tensor imaging tractography to visualize the relationship of the optic radiation to epileptogenic lesions prior to neurosurgery. Epilepsia 52(8):1430–1438
Yamamoto T, Yamada K, Nishimura T, Kinoshita S (2005) Tractography to depict three layers of visual field trajectories to the calcarine gyri. Am J Ophthalmol 140(5):781–785
Yaşargil MG, Krayenbühl N, Roth P, Hsu SPC, Yaşargil DCH (2010) The selective amygdalohippocampectomy for intractable temporal limbic seizures. J Neurosurg 112(1):168–185
Yeni SN, Tanriover N, Uyanik Ö, Ulu MO, Özkara Ç, Karaağaç N, Ozyurt E, Uzan M (2008) Visual field defects in selective amygdalohippocampectomy for hippocampal sclerosis: the fate of Meyer’s loop during the transsylvian approach to the temporal horn. Neurosurgery 63(3):507–515
Acknowledgments
We thank R.D. Ormond MD for language editing of the manuscript. We thank R. Fimmers MD for providing the randomisation list. We wish to acknowledge the contribution of other colleagues who maintained the epilepsy surgery database in the past at the Department of Neurosurgery: T. Kral MD and E. Behrens MD.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J.S. received reimbursement for congress costs from several scientific societies. C.E.E. is consultant for Desitin and Novartis and received honoraria for talks from Pfizer and Eisai. The funding sources had no role in the design of the study, interpretation of the results, or in the writing of the manuscript. None of the other authors has any conflict of interest to disclose.
Funding
Patients’ follow-up was funded as part of the transregional collaborative research consortium SFB-TR3 “Mesial temporal lobe epilepsies” of the Deutsche Forschungsgemeinschaft (DFG).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Delev, D., Wabbels, B., Schramm, J. et al. Vision after trans-sylvian or temporobasal selective amygdalohippocampectomy: a prospective randomised trial. Acta Neurochir 158, 1757–1765 (2016). https://doi.org/10.1007/s00701-016-2860-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2860-y