Abstract
Background
Many previous studies have reported that decompressive craniectomy has improved clinical outcomes in patients with intractable increased intracranial pressure (ICP) caused by various neurosurgical diseases. However there is no report that compares the effectiveness of the procedure in the different conditions. The authors performed decompressive craniectomy following a constant surgical indication and compared the clinical outcomes in different neurosurgical diseases.
Materials and methods
Seventy five patients who underwent decompressive craniectomy were analysed retrospectively. There were 28 with severe traumatic brain injury (TBI), 24 cases with massive intracerebral haemorrhage (ICH), and 23 cases with major infarction (MI). The surgical indications were GCS score less than 8 and/or a midline shift more than 6 mm on CT. The clinical outcomes were assessed on the basis of mortality and Glasgow Outcome Scale (GOS) scores. The changes of ventricular pressure related to the surgical intervention were also compared between the different disease groups.
Findings
Clinical outcomes were evaluated 6 months after decompressive craniectomy. The mortality was 21.4% in patients with TBI, 25% in those with ICH and 60.9% in MI. A favourable outcome, i.e. GOS 4–5 (moderate disability or better) was observed in 16 (57.1%) patients with TBI, 12 (50%) with ICH and 7 (30.4%) with MI. The change of ventricular pressure after craniectomy and was 53.2 (reductions of 17.4%) and further reduced by 14.9% (with dural opening) and (24.8%) after returning to its recovery room, regardless of the diseases group.
Conclusions
According to the mortality and GOS scores, decompressive craniectomy with dural expansion was found to be more effective in patients with ICH or TBI than in the MI group. However, the ventricular pressure change during the decompressive craniectomy was similar in the different disease groups. The authors thought that decompressive craniectomy should be performed earlier for the major infarction patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite highly developed medical and neurosurgical treatments, the mortality and morbidity for patients who have intractable increased intracranial pressure remains a challenge. The initial strategy for managing these patients is to repair the primary cause and to lower the intracranial pressure (ICP) to minimise subsequent brain damage.
Since ICP elevation is a major predictor of death in these patients, it is logical to conclude that a maximum effort aimed toward preventing intracranial hypertension is warranted [16, 72]. Many previous authors have reported the benefits as well as limitations of decompressive craniectomy in patients with hypertensive intracerebral haemorrhage [4, 5, 26, 29, 34, 74], severe traumatic brain injury [10, 11, 13, 16, 43, 45, 46, 59, 69, 70] and major infarction [12, 15, 20, 30, 31, 33, 43, 49, 50, 52, 55, 61, 66, 71, 72]. Some reports indicate that decompressive surgery might be more effective in patients with infarction, because the biomechanics of traumatic brain injury may be more diffuse than that of infarction [12, 49].
However, there are no reports in the literature that compare the effect of decompressive craniectomy on different neurosurgical diseases. Therefore, the authors performed decompressive craniectomy with dural expansions in severe traumatic bran injury (TBI), massive intracerebral haemorrhage (ICH) and major infarction (MI) patients following the same indications for the surgery. The patient outcomes in terms of mortality and Glasgow Outcome Scale (GOS) as well as the ventricular pressure changes during the decompressive craniectomy were compared between the different disease groups.
Methods and material
Patient population
Seventy-five patients who underwent decompressive craniectomy due to increased intracranial pressure due to severe TBI, massive ICH and MI were included in this retrospective analysis. Standard management included completion of a CT scan as rapidly as possible at the time of presentation to the emergency room or when the neurological deterioration was discovered. In all the patients, a pre-operative brain CT scan was performed within 3 hours of the decompression surgery. In patients whose neurological and radiological findings were better than our indications for decompression craniectomy, craniotomy was performed in TBI and ICH patients and other medical treatment such as intravenous or intraarterial thrombolysis was performed in major infarction patients. Thereafter, decompressive craniectomy was performed only if their neurological and radiological findings were appropriate for our decompression surgical criteria (Fig. 1).
Indications for surgery
The indications for decompressive craniectomy with dural expansion were (1) the appearance of definite unilateral or bilateral brain swelling on the CT scan e.g. midline shift of more than 6 mm and/or obliteration of the cisternal structures on the CT scan and/or a (2) patients with an initial Glasgow Coma Scale (GCS) score of less than 8 or worsening of the neurological status (GCS score less than 8). Patients with primary fatal brainstem failure, as indicated by a GCS score of 3 and had no spontaneous respiration did not undergo surgical intervention. The differential indication for either a hemicraniectomy or bilateral decompression where decided. Unilateral oedema/swelling and opening ventricular pressure less than 25 mmHg were treated by hemicraniectomy over the swollen hemisphere, whereas bilateral diffuse oedema/swelling or opening ventricular pressure more than 25 mmHg were treated by bilateral decompression. The above indications were constantly applied for all the patients in this study. For patients with a major infarction, if the initial neurological condition suited our surgical indications, decompressive craniectomy was performed as the first treatment (n = 9). If the neurological status was were better than our surgical indications, other medical treatments such as intravenous or intraarterial thrombolysis were administered before considering decompression surgery.
Operative procedures
In all patients a ventricular puncture was performed at Kocher’s point on the side opposite the main lesion, before the craniectomy (at least 10 × 12 cm size). An external ventricular drein (EVD catheter; Yushin Medical, Seoul, Korea) was connected to the continuous cerebral perfusion pressure monitor (CPP-monitor; Spiegelberg, Hamburg, Germany) via a transducer device (Druckmesset; Smiths Industries, Kirchseeon, Germany). This monitoring system can continuously measure the mean ventricular pressure changes during the decompression surgery, bilateral decompression was performed using large bicoronal skin flaps. The skin flaps were placed just behind the parietal eminence, extending inferiorly to the zygoma on both sides and curving anteriorly towards the midline. This was reflected subperiosteally to the level of the supraorbital ridges. The reference points used for the bone flaps were at the pterion of frontal bone, the parietal eminence and in the temporal squamous areas. After the ventricular ICP was stabilised, the burr holes were connected using a pneumatic saw, with subsequent removal of the bone flap. A frontal median segment of the bone, measuring about 3 to 4 cm in width along the sagittal sinus, was saved to avoid damage to the sagittal sinus and to serve as a framework for later cranioplasty. Additional bone was removed at the temporal region to the floor of the middle fossa (Fig. 2). Ten or fifteen minutes after completion of the craniectomy, the ventricular pressure became stabilised. The dura was then opened with a large cruciated or curved Z-shaped incision, in the areas involving the frontal, temporal and parietal lobes. When the dura was opened, the underlying brain or haematoma typically herniated outwards. In MI patients, cortical resection was not performed. In TBI patients, the epidural or subdural haematoma was removed but haematoma mixed with contused brain parenchyma was not evacuated. In all patients, artificial dura (Lyoplant; B. Braun Melsungen AG, Melsungen, Germany) was placed underneath the incised dura, and secured with several sutures to allow the brain to herniated outward in a more controlled manner, and to prevent cortical adhesion. After insertion of an ICP sensor (Air-pouch system; Spiegelberg, Germany) at the posterior temporal bone margin for epidural ICP monitoring, the temporalis muscle and skin flap were then reapproximated with sutures. Thin large gel-foam (less than 5 mm thickness and 4 × 5 cm size) pieces were placed between the dura and muscle layer for post-operative bleeding control and prevention of adherence between the dura and temporalis muscle. This gel-foam layer facilitated the dissection plane for the cranioplasty to be performed later.
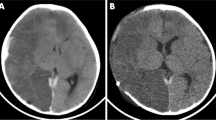
Representative axial head computed scans obtained in a patient with right middle cerebral artery infarction. a Pre-operative CT scan demonstrating the right middle cerebral artery infarction with midline shift. b Early post-operative CT scan demonstrating massive brain swelling. Radiolucent thin gel-foam layer can be seen between the dura and scalp. c Follow-up CT scan obtained 3 weeks postoperatively, when massive brain swelling had subsided. d Brain CT scan obtained after the autologous cranioplasty
Postoperative management and additional operation
After the decompressive surgery, conventional medical management, including hyperosmotic agents, and ventricular drainage (EVD), were initiated if the ventricular pressure exceeded 20 mmHg for 2 h. If the ventricular pressure exceeded 30 mmHg more than 2 h, regardless of previous mentioned medical therapy, mild hypothermia (rectal temperature, 32–34°C) a cold blanket and/or barbiturate coma therapy were initiated.
The bone flap was usually reimplanted 1–3 months after the craniectomy, having been stored under sterile conditions at −70°C (Fig. 3). A ventriculo-peritoneal shunt was performed if the diagnosis of hydrocephalus was confirmed.
Data collection
Ventricular pressure was monitored using the CPP-monitor and printed at a speed of 30 cm/hour during and after the decompression surgery in order to minimise the bias caused by cerebrospinal fluid (CSF) pulsation. The opening ICP readings, which were observed after ventricular tapping for 15 min were considered to be the highest sustained pressures. The ventricular pressure obtained after the craniectomy and opening of the dura were considered to be decompressive craniectomy and dura opening ICP, respectively. The ventricular pressure values were collected using continuous monitoring during surgery and the post-operative period (range 2-7 days).
The presence of a midline shift was measured by a neuroradiologist, on CT scans obtained within 3 hours prior to decompressive craniectomy. This was measured by observation of the distance of the anterior septum that deviated from the line between the anterior and posterior edges of the falx at its attachment to the inside of the calvarium.
Statistical analysis
All data are presented as the mean ± SD. Comparisons between data groups were computed using the ANOVA or Chi-square tests. And if the ANOVA test showed a statistical difference, the unpaired T-test was performed for further analysis. Statistical significance was defined as a probability value of less than 0.05.
Results
From March 2002 to February 2007, a total of 135 patients had undergone decompressive craniectomy. Of these, 60 patients were excluded from this study. They included six patients lost to follow up, four who did not have ventricular pressure monitoring during and after the decompression surgery, five of paediatric age (less than 16 years) and 45 having other diseases such as brain abscess or vasospasm after the aneurysmal subarachnoid haemorrhage. The remaining 75 patients were included in this retrospective analysis; 28 patients had severe traumatic brain injury, 24 had a massive hypertensive intracerebral haematoma, and 23 patients have suffered major infarction (Table 1). There were 52 males and 23 females with a mean age of 54.9 years (range 40–82 years). The age distribution and gender in each group showed no statistical difference.
Ventricular ICP changes seen in accordance with decompression steps
The opening ventricular pressures were variable from 13.5 to 85 mmHg. After craniectomy with intact dura, the ventricular pressure decreased to 53.2 (17.4% of the opening ICP. After the dura was opened, the ventricular ICP decreased further to 20.5 (14.9% of the opening ventricular ICP). Finally the ventricular pressure being measured in the recovery room was down to 28.2 (24.8% of the opening ventricular ICP (Table 2 and Fig. 4). Intracerebral haematoma removal in the ICH group showed a further decrease in the ventricular pressure, ranging from 0 mmHg to 9.5 mmHg.
The amount of ventricular pressure change during decompression surgery was similar in all study groups. The opening ventricular ICP did not correlate with the amount of midline shift, but the amount of ventricular ICP changes from opening ICP to dura opening ICP was correlated with the GOS scores. (T = −2.87, p = 0.01)
Neurological outcome
The pre-operative clinical condition according to GCS was similar in all study groups. The clinical outcomes were evaluated at 6 months after the decompressive surgery by other neurosurgeons who had no information about the patients. Mortality was 21.4% in TBI, 25% in ICH and 60.9% in the MI group. A favourable outcome of GOS 4–5 (moderate disability or better) was observed in 16 patients with TBI, 12 with ICH and seven in the MI group. A poor outcome was a GOS of 1–3 (death, vegetative state, or severe disability) and was observed in 12 patients with TBI, 12 with ICH and 16 with MI groups (Table 3).
Time lapse from the symptom onset and decompressive surgery
The mean time between onset of symptoms and surgery was 9.6 ± 6.9 and 8.3 ± 5.0 h in TBI and ICH, respectively whereas for infarction patients it was 33.3 ± 22.5. The correlation between the time lapse and clinical outcome shows no statistical significance, in the three groups.
Post-operative complications
A consistent finding was the presence of cerebral oedema significant enough to result in bulging out of the craniectomy site and some degree of hygroma both conditions improving spontaneously. (Fig. 2). Five patients (10.2%) had wound infection after reimplantation of the bone flap (n = 49). There were ten patients (13.3%) who required a ventriculo-peritoneal shunt for hydrocephalus (Table 1).
Discussion
Over the past two decades, many studies have shown that decompressive craniectomy is an effective treatment strategy in patients with intractable increased intracranial pressure caused by a variety of neurosurgical diseases [2, 17, 19, 20, 24, 29, 44, 51, 53, 58, 60, 70, 75].
Since the brain is encased in the unyielding vault of the skull, the increased volume of brain and blood result in increased ICP [10, 11, 35, 57]. Decompressive craniectomy with dura expansion involves removing a defined portion of the skull with loose closure of the dura and skin layers. The surgery is intended to increase the volume of the space available for expansion of oedematous brain tissue and thereby increase compliance which will result in a shift to the right of the pressure-volume curve [10, 16, 18, 35, 39, 43]. This results in effective lowering of the increased ICP, improvement in cerebral oxygenation and prevention of secondary brain damage [10, 20, 24, 25, 30, 39, 40, 43, 48, 55, 62, 63].
Early reports of craniectomy, performed as a salvage procedure for the relief of increased ICP after TBI, were not promising [9, 27]. According to the Traumatic Coma Data Bank (TCDB) study, patients with a GCS score of 8 or less on admission have an overall mortality of 33%, with 14% in the vegetative state, and only 7% achieving a good outcome [10, 11, 16, 37].
Recent studies have reported an improved outcome using decompressive craniectomy after the development of refractory intracranial hypertension. One to two thirds of the surviving patients have been reported to have a favourable outcome and the mortality has been reported as less than 20% [1, 6, 10, 11, 13, 22, 25, 32, 40, 45, 46, 53, 65, 69, 70].
In our study, decompressive craniectomy was performed as the first treatment, if the patients had our specific criteria indicating surgery. The mortality was 21.4% and favourable outcome was 57.1% in the TBI patients.
Despite the improved control of systemic hypertension, massive ICH is still one of the most devastating forms of cerebrovascular disease [4, 74]. Maria et al. reported that ICP increases again, a few hours after removal of the haematoma because the heamorrhage itself triggers a series of negative pathogenic mechanisms, the final result of which is the loss of cerebral autoregulation and development of oedema [34].
The role of surgery in the management of primary supratentorial ICH has been the subject of controversy for many years [26, 34, 56, 67, 74]. The aim of surgery is to reduce the mass effect on the brain resulting from both haematoma as well as post-haemorrhagic oedema [34].
In our study, the mortality and favourable outcome in massive ICH patients were 25% and 50%, respectively. The authors feel that early decompressive craniectomy in massive ICH patients could improve the mortality and clinical outcome.
“Malignant or major” middle cerebral artery (MCA) infarction is defined as an infarction of at least two thirds or more of the MCA territory [15, 52, 61]. These complete MCA infarctions are life-threatening and occur in up to 10% of all stroke patients. Most of these patients will experience associated unilateral brain swelling and brain distortion which may lead to transtentorial herniation and has an 80% mortality rate [3, 8, 15, 20, 28, 55, 61, 70].
Surgical decompression accompanied by removal of infarcted brain areas or mass lesions has previously been shown to be effective in selected patients with cerebellar lesions [23, 29, 30, 33, 47, 67]. A recent literature review concluded that the significant mortality rate reduction (studies reporting a 40–50% reduction in mortality rate), a wide therapeutic window (2–5 days), and a low incidence of intraoperative complications make decompressive craniectomy a relevant treatment in patients with a major infarction [15, 17, 20, 21, 28, 48, 52, 54, 55, 61, 70]. The recent reports on this subject have found that most clinical series have a more favourable surgical outcome [8, 21, 42, 48, 52, 55, 61, 70, 72]. A displacement of brain tissue caused by increased ICP is probably the most likely cause of the initial decrease in consciousness and further neurologic deterioration [20]. Decompressive craniectomy increase the space available for upward and outward brain shift and prevents brain stem compression [20, 43, 46]. This surgical procedure has been shown to reduce the patient mortality from 80% in conservatively treated patients to between 20%-35% in surgically treated patients [30, 52, 54, 66, 71, 75]. Schwab et al. [55], showed that severe handicap occurred in only 13% of patients, and Carter et al. [7], reported a favourable outcome in 72% at 1 year follow up. Another recent report, emphasises that decompressive craniectomy within 48 h of the onset of malignant MCA infarction increased the number of patients with a favourable functional outcome [68].
In our study, mortality was 60.9% and favourable outcome was only 30.4% in patients with major infarction. The authors thought that in our study, decompressive craniectomy was delayed until the neurological condition matched the surgical indication (GCS less than 8) and this delayed surgical time may have resulted in a poor clinical outcome than prior studies that performed decompressive surgery earlier [15, 20, 21, 30, 52, 55, 66].
In our opinion, the surgical indication which was followed in this study (GCS score less than 8) caused delay and earlier surgical intervention should be performed for the better neurologic outcome in major infarction patients. A well planned prospective study is needed to established the optimum surgical timing and avoid unnecessary operation in major infarction patients.
The ventricular ICP changes during decompression surgery were similar with our previous report [73]. There are many controversies concerning the correlation between the ICP and midline shift [10, 21, 28, 43, 54, 75]. According to the data reported by Eisenberg et al. [14], midline shift is a very strong predictor of abnormal ICP, and the risk of death is greater as the midline shift becomes larger. Conversely, the investigations of Miller et al. [41] and Tabaddor et al. [64], found no correlation or only a poor correlation between midline shift and ICP. In our study, the opening ventricular ICP was not correlated with the amount of midline shift and the clinical outcomes.
The incidence of hydrocephalus after severe head trauma or in patients with major infarction, who underwent decompressive surgery, has been reported to range from 0.75% to 20%. However, the diagnosis of true hydrocephalus is not always simple [18, 36, 38]. In our study, the over all incidence of shunt surgery for hydrocephalus after decompressive craniectomy was 13.3%.
Conclusions
In patients with a comparable neurological status, decompressive craniectomy with dural expansion was more effective in patients with traumatic brain injury and massive intracerebral haemorrhage than those with major infarction. For patients with severe traumatic brain injury or massive intracerebral haemorrhage, decompressive craniectomy was a good first treatment modality. For patients with major infarction, surgical management should be attempted as early as possible.
References
Albanèse J, Leone M, Allies JR, Kaya JM, Antonini F, Alliez B, martin C (2003) Decompressive craniectomy for severe traumatic brain injury: evaluation of the effects at one year. Crit Care Med 31:2535–2538
Bayir H, Clark RSB, Kochanek PM (2003) Promising strategies to minimise secondary brain injury after head trauma. Crit Care Med 31(Suppl):S112–S117
Berrouschot J, Sterker M, Bettin S, Köster J, Schneider D (1998) Mortality of space-occupying (‘malignant’) middle cerebral artery infarction under conservative intensive care. Intensive Care Med 24:620–623
Broderick JP, Adams HP, Barsan W, Feinberg W, Feldmann E, Grotta J, Kase C, Krieger D, Mayberg M, Tilley B, Zabramski JM, Zuccarello M (1999) Guideline for the management of spontaneous intracerebral haemorrhage. A statement for healthcare professionals from a special writing group of the stroke council, American Heart Association. Stroke 30:905–915
Broderick JP, Brott TG, Duldner JE, Tomsick T, Huster F (1993) Volume of intracerebral haemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke 24:987–993
Caroli M, Locatelli M, Campanella R, Balbi S, Martinelli F, Arienta C (2001) Multiple intracranial lesions in head injury: clinical considerations, prognostic factors, management, and results in 95 patients. Surg Neurol 56:82–88
Carter B, Ogilvy CS, Candia GJ, Rosas HD, Buonanno F (1997) One-year outcome after decompressive surgery for massive non-dominant hemispheric infarction. Neurosurgery 40:1168–1176
Cho DY, Chen TC, Lee HC (2003) Ultra-early decompressive craniectomy for malignant middle cerebral artery infarction. Surg Neruol 60:227–233
Clark K, Nash TM, Hutchison GC (1968) The failure of circumferential craniotomy in acute traumatic cerebral swelling. J Neurosurg 29:367–371
Coplin WM, Cullen NK, Policherla PN, Vinas FC, Wilseck JM, Zafonte RD, Rengachary SS (2001) Safety and feasibility of craniectomy with duraplasty as the initial surgical intervention for severe traumatic brain injury. J Trauma 50:1050–1059
Coplin WM (2001) Intracranial pressure and surgical decompression for traumatic brain injury: biological rationale and protocol for a randomised clinical trial. Neurol Res 23:277–290
Delashaw JB, Broaddus WC, Kassell NF, Haley EC, Pendleton GA, Vollmer DG, Maggio WW, Grady MS (1990) Treatment of right hemispheric cerebral infarction by hemicraniectomy. Stroke 21:874–881
DE Luca GP, Volpin L, Fornezza U, Cervellini P, Zanusso M, Casentini L, Curri D, Piacentiono M, Bozzato G, Colombo F (2000) The role of decompressive craniectomy in the treatment of uncontrollable post-traumatic intracranial hypertension. Acta Neurochir Supple 76:401–404
Eisenberg HM, Gary HE Jr, Aldrich EF, Saydjari C, Turner B, Foulkes MA, Jane JA, Marmarou A, Marshall LF, Young HF (1990) Initial CT findings in 753 patients with severe head injury. A report from the NIH Traumatic Coma Data Bank. J Neurosurg 73:688–698
Fandino J, Keller E, Barth A, Landolt H, Yonekawa Y, Seiler RW (2004) Decompressive craniectomy after middle cerebral artery infarction. Swiss Med Wkly 134:423–429
Figaji AA, Fieggen AG, Peter JC (2003) Early decompressive craniotomy in children with severe traumatic brain injury. Child’s Nerv Syst 19:666–673
Georgiadis D, Schwarz S, Aschoff A, Schwab S (2002) Hemicraniectomy and moderate hypothermia in patients with severe ischaemic stroke. Stroke 33:1584–1588
Guerra WKW, Gaab MR, Dietz H, Mueller JU, Piek J, Fritsch MJ (1999) Surgical decompression for traumatic brain swelling: indications and results. J Neurosurg 90:187–196
Hejazi N, Witzmann A, Fae P (2002) Unilateral decompressive craniectomy for children with severe brain injury. Report of seven cases and review of the relevant literature. Eur J Pediatr 161:99–104
Hofmeijer J, van der Worp HB, Kappelle LJ (2003) Treatment of space-occupying cerebral infarction. Crit Care Med 31:617–625
Holtkamp M, Buchheim K, Unterberg A, Hoffmann O, Schielke E, Weber JR, Masuhr F (2001) Hemicraniectomy in elderly patients with space occupying media infarction: improved survival but poor functional outcome. J Neurol Neurosurg Psychiatry 70:226–228
Hutchinson PJ, Kirkpatrick PJ (2004) Decompressive craniectomy in head injury. Curr Opin Crit Care 10:101–104
Ivamoto HS, Numoto M, Donaghy RMP (1974) Surgical decompression for cerebral and cerebellar infarcts. Stroke 5:365–370
Jaeger M, Soehle M, Meixensberger J (2003) Effects of decompressive craniectomy on brain tissue oxygen in patients with intracranial hypertension. J Neurol Neurosurg Psychiatry 74:513–515
Jiang JY, Xu W, Li WP, Xu WH, Zhang J, Bao YH, Ying YH, Luo QZ (2005) Efficacy of standard traumatic craniectomy for refractory intracranial hypertension with severe traumatic brain injury: a multicenter, prospective, randomised controlled study. J Neurotrauma 22:623–628
Juvela S, Heiskanen O, Poranen A, Valtonen S, Kuurne T, Kaste M, Troupp H (1989) The treatment of spontaneous intracerebral haemorrhage. A prospective randomised trial of surgical and conservative treatment. J Neurosurg 70:755–758
Kerr FWL (1963) Radical decompression and dural grafting in severe cerebral oedema. Mayo Clin Proc 43:852–864
Kilincer C, Asil T, Utku U, Hamamcioglu MK, Turgut N, Hicdonmez T, Simsek O, Ekuklu G, Cobanoglu S (2005) Factors affecting the outcome of decompressive craniectomy for large hemispheric infarction: a prospective cohort study. Acta Neurochir (Wien) 147:587–594
Kobayashi S, Sato A, Kageyama Y, Nakamura H, Watanabe Y, Yamaura A (1994) Treatment of hypertensive cerebellar hemorrhage-surgical or conservative management? Neurosurgery 34:246–251
Koh MS, Goh KYC, Tung MYY, Chan C (2000) Is decompressive craniectomy for acute cerebral infarction of any benefit? Surg Neurol 53:225–230
Kondziolka D, Fazl M (1988) Functional recovery after decompressive craniectomy for cerebral infarction. Neurosurgery 23:143–147
Kontopoulos V, Foroglou N, Patsalas J, Magras J, Foroglon G, Yiannakou-Pephtoulidou M, Sofianos E, Anastassiou H, Tsaoussi G (2002) Decompressive craniectomy for the management of patients with refractory hypertension: should it be reconsidered? Acta Neurochir 144:791–796
Macdonell RAL, Kalnins RM, Donnan GA (1987) Cerebellar infarction: natural history, prognosis, and pathology. Stroke 18:849–855
Maira G, Anile C, Colosimo C, Rossi GF (2002) Surgical treatment of primary supratentorial intracerebral haemorrhage in stuporous and comatose patients. Neurol Res 24:54–60
Marmarou A, Beaumont A (2004) Physiology of the cerebrospinal fluid and intracranial pressure. In: Richard Winn H (ed) Youmans neurological surgery, Vol 4. 5th edn. WB Saunders, Philadelphia, pp 175–193
Marmarou A, Abd-Elfattah MA, Bandoh K, Yoshihara M, Yamamoto T, Tsuji O, Zasler N, Ward JD, Young HF (1996) Post-traumatic ventriculomegaly: hydrocephalus or atrophy? A new approach for diagnosis using CSF dynamics. J Neurosurg 85:1026–1035
Marshall LF, Marshall SB, Klauber MR, Van Berkum Clark M (1991) A new classification of head injury based on computerised tomography. J Neurosurg 75:S14–S20
Mazzini L, Campini R, Angelino E, Rognone F, pastore I, Oliveri G (2003) Post-traumatic hydrocephalus: a clinical, neuroradiologic, and neuropsychologic assessment of long-term outcome. Arch Phys Med Rehabil 84:1637–1641
Meier U, Zeilinger FS, Henzka O (2000) The use of decompressive craniectomy for the management of severe head injuries. Acta Neurochir Suppl 76:475–478
Meier U, Gräwe A (2003) The importance of decompressive craniectomy for the management of severe head injuries. Acta Neurochir Suppl 86:367–371
Miller JD, Becker DP, Ward JD, Sullivan HG, Adams WE, Rosner MJ (1977) Significance of intracranial hypertension in severe head injury. J Neurosurg 47:503–516
Mori K, Nakao Y, Tamamoto T, Maeda M (2004) Early external decompressive craniectomy with duraplasty improves functional recovery in patients with massive hemispheric embolic infarction. Timing and indication of decompressive surgery for malignant cerebral infarction. Surg Neurol 62:420–430
Münch E, Horn P, Schürer L, Piepgra A, Paul T, Schmiedek P (2000) Management of severe traumatic brain injury by decompressive craniectomy. Neurosurgery 47:315–323
Ong YK, Goh KYC, Chan C (2002) Bifrontal decompressive craniectomy for acute subdural empyema. Child’s Nerv Syst 18:340–343
Polin RS, Shaffrey ME, Bogaev CA, Tisdale N, Germanson R, Bocchicchio B, Jane JA (1997) Decompressive bifrontal craniectomy in the treatment of severe refractory post-traumatic cerebral oedema. Neurosurgery 42:84–94
Piek J (2002) Decompressive surgery in the treatment of traumatic brain injury. Curr Opin Crit Care 8:134–138
Raco A, Caroli E, Isidori A, Vangelista T, Salvati M (2003) Management of acute cerebellar infarction: one institution’s experience. Neurosurgery 53:1061–1066
Teithmeier T, Speder B, Pakos P, Brinker G, Löhr M, Klug N, Ernestus RI (2005) Delayed bilateral craniectomy for treatment of traumatic brain swelling in children: case report and review of the literature. Child’s Nerv Syst 21:249–253
Rengachary SS, Batnitzky S, Morantz RA, Arjunan K, Jeffries B (1981) Hemicraniectomy for acute massive cerebral infarction. Neurosurgery 8:321–328
Rieke K, Schwab S, Krieger D, von Kummer R, Aschoff A, Schuchardt V, Hacke W (1995) Decompressive surgery in space-occupying hemispheric infarction: results of an open, prospective trial. Crit Care Med 23:1576–1587
Robertson C (2004) Critical care management of traumatic brain injury. In: Richard Winn H (ed) Youmans neurological surgery, Vol 4. 5th edn. WB Saunders, Philadelphia, pp 5103–5144
Robertson SC, Lennarson P, Hasan DM, Traynelis VC (2004) Clinical course and surgical management of massive cerebral infarction. Neurosurgery 55:55–62
Ruf B, Heckmann M, Schroth I, Hugens-Penzel M, Reiss I, Borkhard A, Gortner L, Jődicke A (2003) Early decompressive craniectomy and duraplasty for refractory intracranial hypertension in children: results of a pilot study. Crit Care 7:R133–R138
Sakai K, Iwahashi K, Terada K, Gohda Y, Sakurai M, Matsumoto Y (1998) Outcome after external decompression for massive cerebral infarction. Neuro Med Chir (Tokyo) 38:131–136
Schwab S, Steiner T, Aschoff A, Schwarz S, Steiner HH, Jansen O, Hacke W (1998) Early hemicraniectomy in patients with complete middle cerebral artery infarction. Stroke 29:1888–1893
Schwarz S, Jauss M, Krieger D, Dörfler A, Albert F, Hacke W (1997) Haematoma evacuation does not improve outcome in spontaneous supratentorial intracerebral haemorrhage: a case-control study. Acta Neurochir (Wien) 139:879–904
Schwab S, Aschoff A, Spranger M, Albert F, Hacke W (1996) The value of intracranial pressure monitoring in acute hemispheric stroke. Neurology 47:393–398
Smith ER, Carter BS, Ogilvy CS (2002) Proposed use of prophylactic decompressive craniectomy in poor-grade aneurysmal subarachnoid haemorrhage patients presenting with associated larger Sylvian haematomas. Neurosurgery 51:117–124
Soukiasian H, Hui T, Avital I, Eby J, Thompson R, Kleisli T, Margulies DR, Cunneen S (2002) Decompressive craniectomy in trauma patients with severe brain injury. Am Surg 68:1066–1071
Stefini R, Latronico N, Cornali C, Rasulo F, Bollati A (1999) Emergent decompressive craniectomy in patients with fixed dilated pupils due to cerebral venous and dural sinus thrombosis: report of three cases. Neurosurgery 45:626–630
Steiner T, Ringleb P, Hacke W (2001) Treatment option for larger hemispheric stroke. Neurology 57(Suppl 2):S61–S68
Stiefel MF, Heuer GG, Smith MJ, Bloon S, Maloney-Wilensky E, Gracias VH, Grady MS, LeRoux PD (2004) Cerebral oxygenation following decompressive hemicraniectomy for the treatment of refractory intracranial hypertension. J Neurosurg 101:241–247
Strege RJ, Lang EW, Stark AM, Scheffner H, Fritsch MJ, Barth H, Mehdorn M (2003) Cerebral oedema leading to decompressive craniectomy: an assessment of the preceding clinical and neuromonitoring trends. Neurol Res 25:510–515
Tabaddor K, Danziger A, Wisoff HS (1982) Estimation of intracranial pressure by CT scan in closed head trauma. Surg Neurol 18:212–215
Uhl E, Kreth FW, Elias B, Goldammer A, Hempelmann RG, Liefner M, Nowak G, Oertel M, Schmieder K, Schneider G-H (2004) Outcome and prognostic factors of hemicraniectomy for space occupying cerebral infarction. J Neurol Neurosurg Psychiatry 75:270–274
Unwin DH, Batjer HH, Greenlee RG Jr (1992) Management controversy. Medical versus surgical therapy for spontaneous intracerebral haemorrhage. Neurosurg Clin N Am 3:533–537
Vahedi K, Hofmeijer J, Juettler E, Vicaut E, George B, Algra A, Amelink GJ, Schmiedeck P, Schwa S, Rothwell PM, Bousser MG, van der Worp HB, Hacke W, DECIMAL, DESTINY, and HAMLET investigators (2007) Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trial. Lancet 6:215–222
Whitfield PC, Patel H, Hutchinson PJA, Czosnyka M, Parry D, Menon D, Pickard JD, Kirkpatrick PJ (2001) Bifrontal decompressive craniectomy in the management of post-traumatic intracranial hypertension. Br J Neurosurg 15:500–507
Winter CD, Adamides AA, Rosenfeld JV (2005) The role of decompressive craniectomy in the management of traumatic brain injury: a critical review. J Clin Neurosci 12:619–623
Woertgen C, Erban P, Rothoerl RD, Bein T, Horn M, Brawanski A (2004) Quality of life after decompressive craniectomy in patients suffering from supratentorial brain ischaemia. Acta Neurochir (Wien) 146:691–695
Yao Y, Liu W, Yang X, Hu W, Li G (2005) Is decompressive craniectomy for malignant middle cerebral artery territory infarction of any benefit for elderly patients? Surg Neurol 64:165–169
Yoo DS, Kim DS, Cho KS, Huh PW, Park CK, Kang JK (1999) Ventricular pressure monitoring during bilateral decompression with dural expansion. J Neurosurg 91:953–959
Zazulia AR, Diringer MN, Derdeyn CP, Powers WJ (1999) Progression of mass effect after intracerebral haemorrhage. Stroke 30:1167–1173
Ziai WC, Port JD, Cowan JA, Garonzik IM, Bhardwaj A, Rigamonti D (2003) Decompressive craniectomy for intractable cerebral oedema: experience of a single center. J Neurosurg Anesthesiol 15:25–32
Zuccarelo M, Brott T, Derex L, Kothari R, Sauerbeck L, Tew J, Von Loveren H, Yeh H-S, Tomsick T, Pancioli A, Khoury J, Broderick J (1999) Early surgical treatment for supratentorial intracerebral haemorrhage. A randomised feasibility study. Stroke 30:1833–1839
Acknowledgement
The author wish to acknowledge the financial support of the Catholic Institute of Cell Therapy Basic Science Programs Foundation made in the program year of 2007.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
“This study aims to add to the now extensive literature on observational series following decompressive craniectomy. It provides further data with good numbers but does attempt to pool results from three different indications with concerns over pooling of ICP data. While the indications for this operation following malignant middle cerebral artery infarction have become more clearly defined following the publication of the combined results of the DESTINY, DECIMAL and HAMLET studies in Lancet Neurology (March 2008), the randomised studies addressing the role of decompressive craniectomy following traumatic brain injury are on-going (www.RESCUEicp.com, DECRA)”
Dr. Hutchinson
Rights and permissions
About this article
Cite this article
Kim, KT., Park, JK., Kang, SG. et al. Comparison of the effect of decompressive craniectomy on different neurosurgical diseases. Acta Neurochir (Wien) 151, 21–30 (2009). https://doi.org/10.1007/s00701-008-0164-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-008-0164-6