Abstract
Introduction
Head injury is the leading cause of accidental death in children. Recent reports have shown the benefit of decompressive craniectomy in children and the role of early timing has been emphasized. However, there is still a lack of data to determine the optimal time for performing craniectomy.
Case report
In contrast to most reports in the literature, this case report demonstrates successful bilateral decompressive craniectomy in a 10-year-old girl with multiple posttraumatic intracranial lesions and massive traumatic brain swelling on the 8th posttraumatic day.
Conclusions
Various pathophysiological mechanisms in the genesis of posttraumatic brain swelling make different treatment strategies necessary. Continuous monitoring of intracranial pressure (ICP), as well as serial cranial computed tomography (CCT), can help to differentiate between these mechanisms. Furthermore, repeated clinical and neurophysiological investigations are important for the timing of craniectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head injury is the leading cause of accidental death in children [14], and severe head injury is estimated to occur in approximately 5% of all children with head injury [22]. Children surviving primary brain damage are particularly in danger of developing secondary brain damage due to raised intracranial pressure (ICP). Despite various conservative management strategies such as osmodiuretics, hypothermia, barbiturates, hyperventilation, free-radical scavengers, or ventriculostomy, ICP does not always respond ; thus, decompressive craniectomy is the ultimate therapeutic approach. Recent reports have shown the benefit of decompressive craniectomy in children [12, 15, 29], and the role of early timing has been emphasized. However, there is still a lack of data to determine the optimal time for performing craniectomy.
This report is about progressive posttraumatic brain swelling with a subsequent rise in ICP that was resistant to conservative treatment (osmodiuretics, mild hyperventilation, barbiturates). Therefore, we performed a bilateral craniectomy on the 8th posttraumatic day to establish sufficient cerebral blood flow in both cerebral hemispheres and to decompress the midbrain and brainstem. Postoperative ICP values were within normal limits.
Case report
An initially comatose 10-year-old girl was admitted to the Department of Neurosurgery, University of Cologne, 1 h after a car accident with bilateral dilated and fixed pupils (Glasgow Coma Score = 3). Initial cranial computed tomography (CCT) showed an acute subdural hematoma with shift of the midline structures to the opposite side (Fig. 1). Evacuation of the hematoma was performed via a small craniectomy 150 min after the trauma, and an intraparenchymatous pressure probe (Codman) was placed into the right frontal lobe. Immediately after the operation, pupils returned to normal size and were reactive to light. ICP values ranged between 4 and 6 mmHg.
a Initial cranial computed tomography (CCT) showing an acute subdural hematoma with midline shift. b Postoperative CCT demonstrating hematoma evacuation and regression of the midline shift. c Control CCT due to therapy-resistant rise in ICP on the 8th day after the trauma, showing diffuse generalized brain edema. d CCT scan 2 days after surgery demonstrating the extent of the bilateral decompressive craniectomy and showing sufficient decompression of both cerebral hemispheres.
Electrophysiological evaluations on the first posttraumatic day revealed a cortical amplitude depression of the sensory evoked potential of the nervus medianus on the right side, as well as a transduction impairment of the acoustic evoked potential on the left. In blink reflex recordings, the oligosynaptic component R1 and the polysynaptically-mediated components R2 and R2′ were abolished. Analysis of glabella reflex recordings revealed a normal R1 component on both sides, whereas the component R2 was missing due to the use of midazolam and fentanyl for analgosedation. The masseter reflex was lost on the left side and showed a marked latency increase on the right side. These findings indicated a lesion of the right cerebral cortex, as well as bilateral brainstem dysfunction.
Follow-up CCT on day 1 revealed evacuation of the hematoma and regression of the midline shift (Fig. 1). On day 3, ICP values started to rise despite conservative therapy, and CCT showed progressive diffuse brain swelling.
On day 8, ICP increased to above 60 mmHg, and was resistant to conservative measures, and CCT showed a massive bilateral brain edema with compression of the ventricular system (Fig. 1). As neurophysiological re-evaluation showed no further impairment of brainstem function, we immediately performed a bilateral fronto-temporal decompressive craniectomy (13×9 cm) and an additional dura enlargement with periost on the right and with a synthetic dura substitute (Neuropatch; Aesculap, Tuttlingen, Germany) on the left side (Fig. 1). ICP values dropped immediately after decompression to normal values, and after a prolonged weaning phase, the patient was extubated on day 21. Neurological and neuropsychological examination showed severe spastic hemiparesis on the left, reduced vigilance, and an impairment in processing visual information. Therefore, neurological rehabilitation therapy was started 40 days after the trauma. After 3 months of continuous physio- and ergotherapeutic training, the patient was able to stand and walk alone. Attention deficits, as well as deficits in writing and analyzing visual information were improved by neuropsychological training, and after 6 months, the patient was able to reattend school. The 2-year follow-up examination showed a socially completely integrated child with no sensomotor deficit (Glasgow Outcome Score = 5).
Review of previous case reports
The vast majority of reports on decompressive craniectomies refer to adults. Reports on children are rare and are summarized in this section and in Table 1.
Dam Hieu et al. [12] reported the successful treatment of two children with acute posttraumatic intracranial hypertension by unilateral craniectomy within 12 h of the trauma. Both children had developed fixed and dilated pupils prior to decompression, which were unresponsive to mannitol infusion. In their opinion, craniectomy can be used as a salvage procedure in children with uncontrollable and rapidly worsening intracranial hypertension when performed within hours of the trauma.
Hejazi et al. [15] described seven cases of unilateral decompressive craniectomy performed within 55 min of the trauma, with complete neurological recovery. They concluded that craniectomy performed within the first 6 posttraumatic hours reduces mortality and improves outcome. Craniectomy later than 6 h can be life-saving but does not improve the neurological outcome.
Taylor et al. [29] performed the only randomized trial on this topic. Children who had sustained intracranial hypertension during the 1st day after admission or showed cerebral herniation were randomized to conventional medical management or decompressive craniectomy plus conventional medical management. Only 2 (14%) of the 14 children in the control group had a favorable outcome, whereas 12 patients (86%) had an unfavorable outcome. Seven (54%) of the 13 children in the decompressive group had a favorable and 6 (46%) had an unfavorable outcome (two-tailed Fisher’s exact test p=0.046; the p value required for significance following repeated significance testing was <0.0221) [20].
Kjellberg and Prieto [17] reported 4 pediatric cases treated via bifrontal craniectomy. Postoperatively, only 1 child suffered from severe neurological dysfunction.
Venes and Collins [31] treated 7 children via craniectomy with less promising results: only 1 child recovered without deficits, 5 children had permanent neurological disturbances, and 1 child died.
Discussion
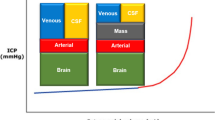
In adults, bilateral craniectomy is considered to be an appropriate procedure for controlling intracranial hypertension that is resistant to conservative treatment, resulting in a positive effect on both ICP levels and overall outcome [24]. This procedure disrupts the cascade of events that links primary to secondary brain damage by rebalancing the cerebral inflow–outflow regulation and by reducing the transmural pressure at the capillary bed. This results in a regression of blood congestion, a reduction in edema formation, and an increase in edema absorption [25].
The different physiological and pathophysiolgical conditions of an immature brain have to be considered for the indication for craniectomy to treat posttraumatic brain swelling in children. Brain water content in the pediatric population is higher than in adults [1], and the immature blood–brain barrier is much more vulnerable to injury from cerebral ischemia [10, 13]. These may be reasons for rapid and diffuse posttraumatic swelling, which is more common in children than in adults. Its incidence in children is nearly double that in adults and is associated with a high mortality rate.
Different pathophysiological processes, triggered by the size of the initial blood flow immediately after the trauma, contribute to the type of brain edema. One group shows almost normal blood flow values, and brain edema is mainly caused by hyperemia and vascular congestion. The other group shows low cerebral blood flow, reflecting ongoing ischemia and development of a cytotoxic brain edema due to insufficient oxygen supply. These two patterns of cerebral blood flow early after the trauma can be identified on initial CCT [32]. Clinical course and treatment strategies differ fundamentally in these two groups. Therefore, conservative treatment options, as well as the timing of the craniectomy, should be performed according to the basic pathophysiological process [2, 26].
In the immediate posttraumatic period, cerebral autoregulation can be lost and can lead to profound cerebral hyperemia and vascular congestion. Initial CCT scans show a hyperdense brain due to the increased cerebral blood volume, which is responsible for a rise in ICP, as supported by experimental and clinical studies [4, 6]. As CO2 responsivity is often preserved in the absence of pressure autoregulation hyperventilation is the most effective conservative measure [9] to control ICP. If these children develop a loss of CO2 responsivity, cerebral blood flow will rise excessively over the next few days. The prolonged loss of CO2 responsivity is considered to be a severe sign [23], followed by an increase in ICP. Morbidity among this group is high because it is difficult to control ICP using conservative treatment modalities [18, 19]. Cerebral vessels do not respond to hypocapnia, and mannitol does not act against the basic pathophysiology, but can elevate ICP due to an increase in cerebral blood volume. As these pathophysiological events usually develop between the 3rd and 5th posttraumatic day, late decompressive craniectomy may be indicated to maintain adequate cerebral blood flow. As the CCT in our case showed a swollen and hyperdense brain on the 8th posttraumatic day (Fig. 1), we explained the rise in ICP by an increase in cerebral blood volume and, therefore, performed bilateral craniectomy.
On the other hand, if early ischemia and hypoxia occurs, the time course of brain swelling will be different. Low brain density on the initial CCT suggests a lack of blood in the brain. The rise in ICP is typical, but difficult to control due to an increase in cerebral water content [16] caused by the cytotoxic brain edema. Cerebral blood flow in these patients remains low, and mortality is high despite maximal conservative treatment. The best conservative therapy would be the use of barbiturates, which decrease the cerebral metabolic rate and permit a degree of ischemia without cellular damage. These children seem to be the best candidates for early decompressive craniectomy within hours of the trauma to normalize ICP in order to restitute adequate cerebral blood flow and to prevent the cascade of events that leads to further cytotoxic swelling.
In addition to these mechanisms, further pathophysiological events lead to a breakdown of the blood–brain barrier and to the development of a vasogenic brain edema with increased water content, especially in the white matter. In general, blood–brain barrier disruption reaches its maximum during the first few hours after an injury and can be promoted by secondary insults like hypoxia and ischemia [28]. Other inflammatory factors that occur after traumatic brain injury, like complement activation [8], formation of free radicals [11], nitric oxide [27], and cytokines [3], may also contribute to the genesis of blood–brain barrier breakdown. In these cases, serial CCT investigations show a progressive loss of gray to white matter differentiation. A rise in ICP due to vasogenic brain edema should be treated using hyperoncotic solutions like mannitol, but mannitol is less effective in children than in adults as this agent had been found to increase cerebral blood flow in the pediatric population [21].
Our literature review revealed 33 cases of posttraumatic craniectomy in children. In 27 cases (82%), operation was performed within 6 h of the trauma. In 22 patients (67%), no conservative treatment had been attempted. Outcome was favorable in 12 patients (36%), and 8 patients (24%) recovered completely (Table 1).
The selection of patients and the determination of the ideal time point for craniectomy are still debatable. The answer should be individualized for each patient and can only be given by continuous monitoring of ICP and cerebral perfusion pressure (CPP), as well as by serial clinical, neurophysiological, and radiographic examinations. Additional monitoring techniques like online measurement of brain tissue partial pressure of oxygen (PtiO2) would be desirable as oxygen supply of the brain is the critical issue in secondary damage. Bardt et al. [5] observed that frequent episodes of brain hypoxia (PtiO2<10 mmHg) correlated with death and poor neurological outcome. They suggested that PtiO2 monitoring is more sensitive than saturation of jugular venous oxygen and, thus, should be the method of choice in monitoring cerebral oxygenation after traumatic brain injury. Van Santbrink et al. [30] demonstrated that PtiO2 values <5 mmHg within 24 h of the trauma negatively correlated with outcome and concluded that PtiO2 monitoring is a safe and clinically applicable method in patients with severe head injury.
Therefore, additional monitoring of brain tissue PtiO2 indicates whether a rise in cerebral blood flow satisfies the higher oxygen demand of the traumatized brain or is caused by the loss of cerebral autoregulation with little effect on cerebral tissue oxygenation. When PtiO2 values indicate adequate brain oxygen supply, children can be treated conservatively, despite a rise in ICP, as adequate brain oxygenation seems to be much more important than absolute ICP values [7]. On the other hand, initial low PtiO2 values indicate that the brain is ischemic and that an impending cytotoxic brain edema may lead to a rise in ICP and a further reduction in cerebral oxygen supply. Thus, early craniectomy may be necessary to restore adequate cerebral blood flow in those cases.
Conclusion
Different pathophysiological mechanisms in the genesis of posttraumatic brain swelling require different treatment strategies. Continuous ICP monitoring and serial CCT scanning are important and routinely available techniques for the differentiation between these mechanisms and, in consequence, indicate the appropriate therapy. Furthermore, clinical and neurophysiological investigations can help in timing craniectomy. For exact timing, additional online monitoring techniques like continuous PtiO2 monitoring may help to identify prolonged periods of compromised cerebral oxygen extraction. However, it has to be considered that threshold values for PtiO2 have so far been defined only for the adult population. Further studies are necessary to evaluate the benefit of continuous PtiO2 monitoring in timing decompressive craniectomy in children.
References
Agrawal HC, Davis JM, Himwich WA (1968) Water content of dog brain parts in relation to maturation of the brain. Am J Physiol 215:846–848
Aldrich EP, Eisenberg HM, Saydjari C (1992) Diffuse brain swelling in severely head-injured children. J Neurosurg 76:450–453
Baba T, Black KL, Ikezaki K (1991) Intracarotid infusion of leukotriene C4 selectively increases blood–brain barrier permeability after focal ischemia in rats. J Cereb Blood Flow Metab 11:638–643
Baigas KV, Grundi PD, Kochanek PM, Schiding JK, Nemoto EM (1996) Posttraumatic hyperemia in immature, mature, and aged rats: autoradiographic determination of cerebral blood flow. J Neurotrauma 13:189–200
Bardt TF, Unterberg AW, Hartl R, Kiening KL, Schneider GH, Lanksch WR (1998) Monitoring of brain tissue PO2 in traumatic brain injury: effect of cerebral hypoxia on outcome. Acta Neurochir Suppl 71:153–156
Barie AJ, Ghajar JB, Firlik AD, Chang VA, Hariri RJ (1993) Contribution of increased cerebral blood volume to post traumatic intracranial hypertension. J Trauma 35:69–71
Beaumont A, Marmarou A (1999) Treatment of raised intracranial pressure following traumatic brain injury. Crit Rev Neurosurg 9:207–216
Bellander B-M, von Holst H, Fredman P (1996) Activation of the complement cascade and increase of clusterin in the brain following a cortical contusion in the adult rat. J Neurosurg 85:468–475
Bruce DA, Alavi A, Bilaniuk L (1981) Diffuse cerebral swelling following head injuries in children: the syndrome of “malignant brain edema.” J Neurosurg 54:170
Caley DW, Maxwell DS (1970) Development of the blood vessels and extracellular space during postnatal maturation of rat cerebral cortex. J Comp Neurol 138:31–48
Chan PH, Schmidley JW, Fishman RA (1984) Brain injury, edema and vascular permeability changes induced by oxygen-derived free radicals. Neurology 34:315–320
Dam Hieu P, Sizun J, Person H, Besson G (1996) The place of decompressive surgery in the treatment of uncontrollable post-traumatic intracranial hypertension in children. Childs Nerv Syst 12:270–275
Evans AN, Reynolds JM, Reynolds ML (1974) Development of a blood–brain barrier mechanism in foetal sheep. J Physiol 238:371–386
Graham D, Adam J, Doyle D, Lawrence A, McLellan D, Ng H (1989) Fatal head injury in children. J Clin Pathol 42:18–22
Hejazi N, Witzmann A, Fae P (2002) Unilateral decompressive craniectomy for children with severe brain injury. Report of seven cases and review of the relevant literature. Eur J Pediatr 161:99–104
Kita H, Marmarou A (1994) The cause of acute brain swelling after closed head injury in rats. Acta Neurochir Suppl (Wien) 60:452–455
Kjellberg RN, Prieto A Jr (1971) Bifrontal decompressive craniectomy for massive cerebral edema. J Neurosurg 34:488–493
Lang DA, Teasdale GM, Macpherson P, Lawrence A (1994) Diffuse brain swelling after head injury: more often malignant in adults than in children. J Neurosurg 80:675–680
McBride DQ, Shalmon E, Herman D, Becker DP (1997) Cerebral blood flow as a predictor of outcome following traumatic brain injury. J Neurosurg 86:633–641
McPherson K (1974) Statistics: the problem of examining accumulating data more than once. N Engl J Med 290:501–502
Miller JD (1992) Evaluation and treatment of head injury in adults. Neurosurg Q 2:28–43
Murgio A, Andrade FA, Sanchez Munoz MA, Boetto S, Leung KM (1999) International multicenter study of head injury in children. Childs Nerv Syst 15:318–321
Paolin A, Rodriguez G, Betetto M (1998) Cerebral hemodynamic response to CO2 after severe head injury: clinical and prognostic implications. J Trauma 44:495
Polin RS, Shaffrey ME, Boagaev CA, Tisdale N, Germanson T, Bocchicchio B, Jane JA (1997) Decompressive bifrontal craniectomy in the treatment of severe refractory posttraumatic cerebral edema. Neurosurgery 41:84–94
Rinaldi A, Mangiola C, Anile C, Maira G, Amante P, Ferraresi A (1990) Hemodynamic effects of decompressive craniectomy in cold induced brain oedema. Acta Neurochir Suppl 51:394–396
Sahuquillo J, Poca MA, Garnacho A (1993) Early ischemia after severe head injury. Preliminary results in patients with diffuse brain injuries. Acta Neurochir 122:204–214
Salvemini D, Wang Z-Q, Wyatt PS (1996) Nitric oxide: a key mediator in the early and late phase of carrageenan-induced rat paw inflammation. Br J Pharmacol 118:829–838
Tanno H, Nockels RP, Pitts LH (1992) Breakdown of the blood–brain barrier after fluid percussive brain injury in the rat. I. Distribution and time course of protein extravasation. J Neurotrauma 9:21–32
Taylor A, Butt W, Rosenfeld J, Shann F, Ditchfield M, Lewis E, Kulg G, Wallace D, Henning R, Tibballs J (2001) A randomized trial of very early decompressive craniectomy in children with traumatic brain injury and sustained intracranial hypertension. Childs Nerv Syst 17:154–162
Van Santbrink H, Maas A, Avezaat CJJ (1996) Continuous monitoring of partial pressure of brain tissue oxygen in patients with severe head injury. Neurosurgery 38:21–31
Venes JL, Collins WR (1975) Bifrontal decompressive craniectomy in the management of head trauma. J Neurosurg 42:429–433
Yoshino E, Yamaki T, Higuchi T, Horikawa Y, Hirakawa K (1985) Acute brain edema in fatal head injury: analysis by dynamic CT scanning. J Neurosurg 63:830–839
Author information
Authors and Affiliations
Corresponding author
Additional information
A commentary on this paper is available at http://dx.doi.org/10.1007/s00381-004-1045-9
Rights and permissions
About this article
Cite this article
Reithmeier, T., Speder, B., Pakos, P. et al. Delayed bilateral craniectomy for treatment of traumatic brain swelling in children: case report and review of the literature. Childs Nerv Syst 21, 249–253 (2005). https://doi.org/10.1007/s00381-004-1044-x
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-004-1044-x