Abstract
Purpose
Intraductal tubulopapillary neoplasm is a rare pancreatic tumor. The purpose of this study was to clarify the recurrence type and prognosis in recurrent cases after intraductal tubulopapillary neoplasm resection.
Methods
PubMed was searched for previous reports on surgical resection of intraductal tubulopapillary neoplasm of the pancreas that were published from 2009 to July 2020. The clinical features obtained from these reports were summarized and analyzed.
Results
The clinicopathological data of 35 intraductal tubulopapillary neoplasm cases were obtained. Of these, 21 were males, and 14 were females, with an average age of 57.9 years old. Invasive findings were observed in 21 of 35 patients (60%). Recurrence was observed in 11 of the 35 cases (31.4%), including remnant pancreatic recurrence in 6 cases (17.1%) and liver metastasis in 5 cases (14.3%). The tumor size was significantly larger in the liver metastasis group than in the remnant pancreas recurrence group (P = 0.04), and patients with liver metastases tended to have a poorer prognosis than those with remnant pancreas recurrence.
Conclusions
The recurrence type of intraductal tubulopapillary neoplasm resection was mainly remnant pancreatic recurrence and liver metastasis recurrence. Total pancreatectomy for remnant pancreatic recurrence may be suitable because of its good prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intraductal tubulopapillary neoplasm (ITPN) was proposed as a new disease concept by Yamaguchi et al. [1] in 2009 and was categorized as a new entity in the pancreatic intraductal neoplasm family in the 2010 World Health Organization (WHO) classification of tumors of the digestive system [2]. ITPN is rare, with an incidence rate of 0.9% among exocrine pancreatic tumors and 3% among pancreatic tumors. ITPN is a solid tumor that fills the pancreatic duct and is non-mucus-producing. It grows as a tubulopapillary neoplasm in the pancreatic duct, with scattered small necrotic foci that have a tendency to differentiate into gland ducts (positive expression of pancreatic duct epithelial markers cytokeratin [CK]-7 and CK-19) but not into acinar cells (negative expression of trypsin, a marker for acinar differentiation). An immunohistochemical assessment of the mucin core protein expression in tumors shows negative findings for MUC2, MUC5AC, and fascin (differentiation from intraductal papillary mucinous neoplasm [IPMN]) and no KRAS or BRAF mutations.
Several systematic reviews of ITPN have been reported thus far. Basturk et al. [3] reported that ITPN had a better prognosis than normal pancreatic cancer, even with invasive findings. Furthermore, they compared the overall survival rates with and without invasive findings and found no significant difference. Date et al. [3] also analyzed 58 cases of ITPN resection and reported their clinicopathological features and surgical outcomes. The overall survival rates was 81.5% in patients with an invasive component and 77.8% in those with a non-invasive component. Kuan et al. [4] reported the latest clinical and pathological findings in both ITPN of the pancreas and the rarer ITPN of the bile duct. There have been no reports concerning recurrence of ITPN, although ITPN is a relatively newly identified and rare disease that is gradually being elucidated as a result of the accumulation of cases and seems to have a favorable prognosis.
We herein report our analysis of the recurrence types and prognosis of recurrent ITPN resection cases based on a systematic review.
Materials and methods
Literature search
PubMed (URL: https://www.ncbi.nlm.nih.gov) was searched for reports on surgical resection of ITPN of the pancreas. The search was performed using the term “intraductal tubulopapillary neoplasm”. The final search was completed in July 2020. All English-language articles related to reports on surgical resection of ITPN of the pancreas were analyzed. Cases were extracted from the selected articles. The extracted cases were further sorted by postoperative course and recurrence type. The entire process of this study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [5].
Results
From the 86 articles identified, 1 that was not written in English (n = 1), those of obvious irrelevance (n = 45), and 1 for which detailed information was not available (n = 1) were excluded, leaving 39 articles [1], 4, 6, 39. Seventy-nine cases were extracted from these 39 articles, and from these 79, we excluded 44 cases for which the postoperative course was not reported (n = 19), cases with no recurrence that were not followed for more than 12 months after surgery (n = 8), cases with the recurrence type not reported (n = 16), and there were cases in which pre-recurrence and post-recurrence were reported, and such cases were counted as one case. These findings are summarized in Fig. 1. We, therefore, finally analyzed 35 ITPN cases extracted by the algorithm (Fig. 1); Table 1 shows the clinicopathological summary of these cases. Table 2 shows characteristic of patients according to the recurrence patterns of ITPN.
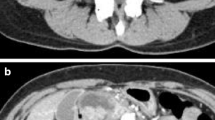
Of the 35 analyzed cases, 21 were males, and 14 were females, with an average age of 57.9 years. Invasive findings were observed in 21 of the 35 patients (60%). Recurrence was observed in 11 of the 35 cases (31.4%), including remnant pancreatic recurrence in 6 cases (17.1%) and liver metastasis in 5 cases (14.3%) (Fig. 2). Regarding the tumor diameter, the median size was 3.5 (range 0.5–12.0) cm in the no-recurrence group, 1.7 (range 1.0–2.2) cm in the remnant pancreas recurrence group, and 8.0 (range 3.3–15.0) cm in the liver metastasis group. The tumor size was significantly larger in the liver metastasis group than in the remnant pancreas recurrence group. One case each in the remnant pancreatic recurrence and liver metastasis groups with an unknown tumor diameter was excluded (P = 0.04). Invasive findings were observed in four of the five cases of recurrence of liver metastasis. Three cases showed lymph node metastasis, and all had recurrence of liver metastasis. [6, 20, 35] There was one case in which the surgical margin was considered positive, and that case had recurrence of liver metastasis. [35] No surgical treatment was performed for recurrence of liver metastasis, while chemotherapy was performed in two cases [6, 20]. One case had recurrence of the remnant pancreas 192 months after surgery. After recurrence, total pancreatectomy (TP) was performed in five of the six cases with remnant pancreatic recurrence, and no further recurrence has since been reported in any of these cases at the time of publication.
No cases of neoadjuvant therapy were reported. Adjuvant therapy was performed in seven patients. [6, 9, 21, 28, 29, 31, 33] Four cases received tegafur-gimeracil-oteracil potassium (S-1) (one case was after TP for remnant pancreatic recurrence). [10, 28, 29, 31] One case was treated with gemcitabine (GEM) and had liver and lymph node metastases [6]. Two cases were treated with GEM and capecitabine [21, 33]. One of these two cases had recurrence of liver metastasis [33]. Remnant pancreatic recurrence was observed in two patients who received S-1 as adjuvant treatment [29, 31]. Only one patient developed multiple liver metastases 4-months after surgery and died 3-months later [1]. Figure 3 shows the recurrence-free and overall survival rates of ITPN according to the recurrence type. In Figs. 3 and 4, one case of liver metastasis recurrence in the non-invasive group was excluded because the survival recurrence period was unknown. Figure 3a shows the recurrence-free survival rate of ITPN according to the recurrence pattern. Patients with liver metastases tended to have a poorer prognosis than those with remnant pancreas recurrence, but this was not statistically significant (P = 0.07). Figure 3b shows the overall survival rate of ITPN according to the recurrence pattern. No significant difference was found here either (P = 0.15).
Figure 4 shows the recurrence-free and overall survival rates of ITPN according to the invasion type. There was no significant difference in the recurrence-free survival rate (P = 0.25) or overall survival rate (P = 0.40) between the two groups.
Discussion
ITPN is a relatively newly identified rare disease whose concept was first established in 2009, and details of its treatment and prognosis remain unclear, even after 10 years. Although characteristic image findings and pathological findings have been reported, the preoperative diagnosis is relatively difficult at present, and most cases are diagnosed after resection. The 5-year survival rates of ITPN were reported to be 71%–80.7%, [3, 3] showing a better prognosis than pancreatic cancer, but there are no reports concerning the recurrence of ITPN, making ours the first to examine ITPN recurrence. The recurrence type was found to be mainly remnant pancreatic recurrence and liver metastasis recurrence, which may be accompanied by lymph node metastasis. The tumor size was significantly larger in the liver metastasis group than in the remnant pancreas recurrence group (P = 0.04). The recurrence-free survival rates tended to be poorer in patients with liver metastases than in those with remnant pancreas recurrence.
Many cases of remnant pancreatic recurrence have been reported in recent years. For remnant pancreatic recurrence, several factors, such as tumor cell-positive excision sections, multifocal lesions, and intrapancreatic micrometastasis, are considered. The resection margins were reported to be negative in all six cases of remnant pancreatic recurrence, and tumor remnants are unlikely to be the cause of recurrence. The pathological findings of recurrent tumors indicate that the tumor is basically located in the main pancreatic duct but may also be located in the pancreatic parenchyma. There were multiple recurrences in two cases [30, 33]. One non-invasive case experienced recurrence with new invasive findings, [30] but the histological findings, immunostaining, and molecular characteristics were similar to those of the primary tumor. In one case of recurrent tumor, the Ki-67 labeling index increased, and the risk of malignancy may also increase with recurrence. However, there was a case in which invasive findings were observed in primary tumors but not in recurrent tumors.
Saeki et al. [30] noted that if the remnant pancreatic tumor is metachronous and multicentric, it develops mainly in the main pancreatic duct. Similarities should be confirmed by comparing the pathological findings of the original and recurrent tumors, which may help predict recurrence mechanisms. Regarding the mechanism underlying remnant pancreatic recurrence, the clinicopathological findings were similar to those of the original tumor in previous reports, and micrometastases were predominant in the original tumor in contrast to cases of metachronous or multicentric recurrence [30, 32]. As a new possibility, Ko et al. [33] pointed out the possibility of the implantation of tumor cells, as a recurrent tumor was found in the pancreatic duct in a resected specimen of total pancreatectomy, but no clear malignant tumor was found in the pancreatic duct epithelium, and tumor cells were floating in the pancreatic duct. The true mechanism of remnant pancreatic recurrence is unknown and requires further study. One case of recurrence developed 192 months after surgery, so long-term follow-up is required. After remnant pancreas recurrence, TP was performed in five of six cases, and a good prognosis was established. TP may be suitable, depending on the patient’s status, as there were no cases of remnant pancreas recurrence after TP. However, since one case of liver metastasis recurrence was reported in a patient who underwent TP as the initial surgery, [1] it is necessary to conduct careful follow-up after TP.
Recurrence of liver metastases tends to occur in large tumors and is often associated with invasive findings. In our review, recurrence of liver metastasis was observed in all three cases with lymph node metastasis in the resected specimen, and lymph node metastasis may be a risk factor for recurrence of liver metastasis. Cases of recurrence of liver metastasis often have invasive findings, but one case did not show invasive findings. The cause of liver metastasis recurrence may be due to either preoperative or intraoperative iatrogenic factors. A strict pathological examination with fine slices may be required to search for invasive findings. This case showed high-grade dysplasia and had a high Ki-67 labeling index of 70% and high malignancy, so it would not have been strange for liver metastasis recurrence to occur.
The basic treatment of ITPN is resection. In addition, neoadjuvant therapy and adjuvant therapy may be considered. However, there were no cases of neoadjuvant treatment. Adjuvant treatment was performed in seven cases [6, 9, 21, 28, 29, 31, 33]. However, five of them experienced a relapse. It is hoped that viable neoadjuvant and adjuvant therapy strategies will be established with the accumulation of more cases. Chemotherapy is often selected as a treatment for recurrence of liver metastases, and GEM, S-1, and 5-Fluorouracil, Leucovorin and Oxaliplatin (FOLFOX) are routinely administered for pancreatic cancer; however, their effects are unclear. Chemotherapy was administered in two cases [6, 20]. Bhuva et al. [6] reported that the combination of FOLFOX and integrated Yttrium-90 radioembolization was partially successful for managing recurrence of liver metastasis. Regarding the treatment strategy for recurrence of liver metastases, there is no consensus chemotherapy regimen, and marked efficacy cannot be expected, so resection should be considered when possible. However, liver metastases are often unresectable, in which case chemotherapy or radiation therapy, similar to the approach with normal pancreatic cancer, may be a suitable option. Palliative care is selected if treatment is not possible or desired. The prognosis is poor if recurrence of liver metastasis occurs. It is, therefore, important to prevent such recurrence.
In conclusion, this is the first report to examine ITPN recurrence. The recurrence type of ITPN resection is mainly remnant pancreatic recurrence and liver metastasis recurrence, but the type may be affected by the tumor size. TP for remnant pancreatic recurrence may be a suitable treatment approach because of its good prognosis.
References
Yamaguchi H, Shimizu M, Ban S, Koyama I, Hatori T, Fujita I, et al. Intraductal tubulopapillary neoplasms of the pancreas distinct from pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am J Surg Pathol. 2009;33:1164–72.
Adsay NV, Fukushima N, Furukawa T, Hruban RH, Klimstra DS, Klöppel G, et al. Intraductal neoplasm of the pancreas. In: Boston FT, Carneiro F, Hruban RH, Heise ND, et al., editors. World Health Organization classification of 14 tumours of the digestive system. Lyon: IARC Press; 2010; p. 304–13.
Basturk O, Adsay V, Askan G, Dhall D, Zamboni G, Shimizu M, et al. Intraductal tubulopapillary neoplasm of the pancreas: a clinicopathologic and immunohistochemical analysis of 33 cases. Am J Surg Pathol. 2017;41(3):313–25.
Date K, Okabayashi T, Shima Y, Iwata J, Sumiyoshi T, Kozuki A, et al. Clinicopathological features and surgical outcomes of intraductal tubulopapillary neoplasm of the pancreas: a systematic review. Langenbeck’s Arch Surg. 2016;401:439–47.
Kuan LL, Dennison AR, Garcea G. Intraductal tubulopapillary neoplasm of the pancreas and bile duct: a review. Pancreas. 2020;49(4):498–502.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. https://doi.org/10.1136/bmj.b2535.
Bhuva N, Wasan H, Spalding D, Stamp G, Harrison M. Intraductal tubulopapillary neoplasm of the pancreas as a radiation induced malignancy. BMJ Case Rep. 2011. https://doi.org/10.1136/bcr.09.2011.4777.
Tajiri T, Tate G, Matsumoto K, Hoshino H, Iwamura T, Kodaira Y, et al. Diagnostic challenge: intraductal neoplasms of the pancreatobiliary system. Pathol Res Pract. 2012;208(11):691–6.
Jokoji R, Tsuji H, Tsujimoto M, Shinno N, Tori M. Intraductal tubulopapillary neoplasm of pancreas with stromal osseous and cartilaginous metaplasia; a case report. Pathol Int. 2012;62:339–43.
Urata T, Naito Y, Nagamine M, Izumi Y, Tonaki G, Iwasaki H, et al. Intraductal tubulopapillary neoplasm of the pancreas with somatic BRAF mutation. Clin J Gastroenterol. 2012;5:413–20.
Guan H, Gurda G, Lennon AM, Hruban RH, Erozan YS. Intraductal tubulopapillary neoplasm of the pancreas on fine needle aspiration: case report with differential diagnosis. Diagn Cytopathol. 2014;42(2):156–60.
Kasugai H, Tajiri T, Takehara Y, Mukai S, Tanaka J, Kudo SE. Intraductal tubulopapillary neoplasms of the pancreas: case report and review of the literature. J Nippon Med Sch. 2013;80:224–9.
Someya Y, Nakamoto Y, Nakatani K, Kawaguchi M, Minamiguchi S, Togashi K. 18F-FDG uptake in intraductal tubulopapillary neoplasm of the pancreas. Clin Nucl Med. 2014;39(4):e277–80.
Del Chiaro M, Mucelli RP, Blomberg J, Segersvärd R, Verbeke C. Is intraductal tubulopapillary neoplasia a new entity in the spectrum of familial pancreatic cancer syndrome? Fam Cancer. 2014;13(2):227–9.
Ahls MG, Niedergethmann M, Dinter D, Sauer C, Lüttges J, Post S, et al. Case report: intraductal tubulopapillary neoplasm of the pancreas with unique clear cell phenotype. Diagn Pathol. 2014;9:11.
Furuhata A, Minamiguchi S, Mikami Y, Kodama Y, Sumiyoshi S, Adachi S, et al. Intraductal tubulopapillary neoplasm with expansile invasive carcinoma of the pancreas diagnosed by endoscopic ultrasonography-guided fine needle aspiration: a case report. Diagn Cytopathol. 2014;42(4):314–20.
Tajima S. Intraductal tubulopapillary neoplasm of the pancreas suspected by endoscopic ultrasonography-fine-needle aspiration cytology: report of a case confirmed by surgical specimen histology. Diagn Cytopathol. 2015;43(12):1003–6.
Takayama S, Maeda T, Nishihara M, Kanazawa A, Chong HS, Oka H, et al. A case of intraductal tubulopapillary neoplasm of pancreas with severe calcification, a potential pitfall in diagnostic imaging. Pathol Int. 2015;65(9):501–6.
Yoshida Y, Matsubayashi H, Sasaki K, Kanemoto H, Uesaka K, Ono H, et al. Intraductal tubulopapillary neoplasm of the pancreatic branch duct showing atypical images. J Dig Dis. 2015;16:357–61.
Kitaguchi K, Kato Y, Kojima M, Okuobo S, Takahashi D, Okada R, et al. A resected case of intraductal tubulopapillary neoplasm of the pancreas: report of a case. Int Surg. 2015;100(2):281–6.
Matthews Y, McKenzie C, Byrne C, Kench JG. Intraductal tubulopapillary neoplasm of pancreas with associated invasive carcinoma, lymph node, rectal and hepatic metastases. Pathology. 2015;47(2):169–71.
Kölby D, Thilén J, Andersson R, Sasor A, Ansari D. Multifocal intraductal tubulopapillary neoplasm of the pancreas with total pancreatectomy:report of a case and review of literature. Int J Clin Exp Pathol. 2015;8(8):9672–80.
Savant D, Lee L, Das K. Intraductal tubulopapillary neoplasm of the pancreas masquerading as pancreatic neuroendocrine carcinoma: review of the literature with a case report. Acta Cytol. 2016;60(3):267–74.
Fujimoto Y, Tomimaru Y, Tamura H, Noguchi K, Nagase H, Hamabe A, et al. Pancreatic intraductal tubulopapillary neoplasm with associated invasive cancer successfully treated by total pancreatectomy: a case report. Oncol Lett. 2017;14(1):153–8.
Kuscher S, Steinle H, Soleiman A, Öfner D, Schneeberger S, Oberhuber G. Intraductal tubulopapillary neoplasm (ITPN) of the pancreas associated with an invasive component: a case report with review of the literature. World J Surg Oncol. 2017;15(1):203.
Kovacevic B, Añó PL, Toxværd A, Vilmann P, Kalaitzakis E. Intraductal tubulopapillary neoplasm of the pancreas diagnosed by endoscopic ultrasonography-guided fine needle aspiration. Endoscopy. 2017;49(11):E266–7.
Maghrebi H, Makni A, Rhaeim R, Zehani A, Bensafta Z. Intraductal tubulopapillary neoplasm: a new entity in the spectrum of pancreatic intraductal neoplasms. J Clin Diagn Res. 2017;11(9):PD14–6. https://doi.org/10.7860/JCDR/2017/28596.10663.
Niu L, Xu Z, Liu H, Cao H, Yang G. Intraductal tubulopapillary neoplasm accompanied by invasive carcinoma of the pancreas: a case report and review of the literature. Mol Clin Oncol. 2017;6(5):676–82.
Inomata K, Kitago M, Obara H, Fuji-Nishimura Y, Shinoda M, Yagi H, et al. Conncurrent presentation of an intraductal tubulopapillary neoplasm and intraductal papillary mucinous neoplasm in the branch duct of the pancreas, with a superior mesenteric artery aneurysm: a case report. World J Surg Oncol. 2018;16:83.
Sakamoto S, Tsuruga Y, Fujii Y, Shomura H, Hattori A, Kazui K, et al. Intraductal tubulopapillary neoplasm of the pancreas presenting as recurrent acute pancreatitis: a case report. Int J Surg Case Rep. 2018;48:122–5.
Saeki K, Miyasaka Y, Ohishi Y, Yamamoto T, Matsuda R, Mochidome N, et al. Intrapancreatic recurrence of intraductal tubulopapillary neoplasm (ITPN) 16 years after the initial surgery for noninvasive ITPN: a case report. Surg Case Rep. 2018;4:96.
Umemura A, Ishida K, Nitta H, Takahara T, Hasegawa Y, Makabe K, et al. A rare case of intraductal tubulopapillary neoplasm of the pancreas rupturing and causing acute peritonitis. Case Rep Gastroenterol. 2017;11(3):661–6.
Umemura A, Ishida K, Nitta H, Takahara T, Hasegawa Y, Makabe K, et al. An extremely rare case who underwent total remnant pancreatectomy due to recurrent pancreatic metastasis of intraductal tubulopapillary neoplasm. Clin J Gastroenterol. 2019;12(2):153–9.
Ko K, Nishida Y, Sasahara K, Kishimoto H, Noriaki O, Tauchi K, et al. A resected case of recurrent ITPN in the remnant pancreas after pancreatoduodenectomy. Surg Case Rep. 2019;5(1):33.
Fritz S, Küper-Steffen R, Feilhauer K, Sommer CM, Richter GM, Bosse A, et al. Intraductal tubular papillary neoplasm (ITPN), a novel entity of pancreatic epithelial neoplasms and precursor of cancer: a case report and review of the literature. Int J Surg Case Rep. 2019;55:187–91.
Zhang J, Ren S, Wang J, Ye D, Zhang H, Qiu W, et al. Imaging findings of intraductal tubulopapillary neoplasm (ITPN) of the pancreas: two case reports and literature review. Medicine (Baltimore). 2019;98(6):e14426. https://doi.org/10.1097/MD.0000000000014426.
Zhou PC, Chen XP, Li B, Xie YC, Zhou TJ, Wang JM, et al. Intraductal tubulopapillary neoplasm (ITPN) of the pancreas with invasive cancer misdiagnosed as a mesenteric cyst for 12 years: a case report and literature review. Int J Clin Exp Pathol. 2019;12(3):1041–6.
Dalal A, Patil G, Vadgaonkar A, Maydeo A. A rare case of intraductal tubulopapillary neoplasm of the pancreas—case report (with video). Postgrad Med. 2020;132(3):270–3. https://doi.org/10.1080/00325481.2019.1669058.
Nabrinsky E, Baste CL, Gonzalez M, James E. Intraductal tubulopapillary neoplasm of the pancreas presenting as a localized pancreatic tumor in a 52-year-old woman: focusing on a rare pancreatic malignancy and contrasting to intrapapillary mucinous neoplasm. Cureus. 2020;12(6):e8548. https://doi.org/10.7759/cureus.8548.
Ohno A, Kaku T, Kawabe K. Fine-needle-aspiration using forward-viewing echoendoscope for the recurrence of intraductal tubulopapillary neoplasm. Dig Endosc. 2020;32(5):e102–3.
Acknowledgements
We thank H. Nikki March, PhD, from Edanz Group (https://en-author-services.edanzgroup.com/ac) for editing a draft of this manuscript.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Seki, T., Watanabe, A., Harimoto, N. et al. Systematic review of resectable intraductal tubulopapillary neoplasm with special reference to recurrence patterns. Surg Today 52, 532–541 (2022). https://doi.org/10.1007/s00595-021-02324-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02324-3