Abstract
Purpose
Lysophosphatidylcholine (LPC), which is generated from phosphatidylcholine (PC) and metabolized by autotaxin (ATX), modulates immune responses via its anti-inflammatory property. We investigated the association between LPC and postoperative complications (POCs) after colorectal cancer surgery (CRC).
Methods
The subjects of this study were 43 patients who underwent surgery for CRC. Peripheral blood samples were collected preoperatively and immediately after surgery, and on postoperative days (PODs) 1, 3, 5, and 7. Patients were divided into a No-POC group (n = 33) and a POC group (n = 10). Blood LPC, IL-6, PC, and ATX levels were measured by specific enzymatic assays or ELISA.
Results
The postoperative to preoperative LPC ratios were lowest on POD 1 in both groups. The POC group had significantly lower LPC ratios throughout the perioperative period than the No-POC group. The LPC ratios were inversely correlated with IL-6. The predictive impact of LPC ratios on POCs was demonstrated by ROC analysis (cut-off 51.2%, AUC 0.798) and multivariate analysis (OR 15.1, P = 0.01). The postoperative PC ratios decreased more after surgery in the POC group. ATX levels did not change significantly in either group.
Conclusions
Decreased postoperative LPC is associated with increased postoperative inflammatory response and POCs. The decreased PC supply to the circulation is a mechanism of the postoperative LPC decrease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of colorectal cancer (CRC) continues to increase in Japan. Since 2015, it has been the most common cancer in this country, accounting for over 50,000 deaths annually [1]. Although mortality associated with CRC has decreased by 14% over the last decade, about 40% of patients with diagnosed CRC will die from their disease [2]. Surgery continues to form the cornerstone of its management, but is itself associated with significant morbidity and mortality despite improvements in techniques and perioperative care [3]. The postoperative complication (POC) rates after CRC surgery remain high at about 30% and the postoperative mortality rate is still 3–4% [4, 5]. POCs, particularly infective complications such as anastomotic leakages, are clearly associated with both an increased risk of cancer recurrence and poorer long-term oncological survival, in addition to their adverse effects on quality of life and medical resources [6,7,8,9]. Thus, there is an urgent need for surgeons to understand the background mechanism of POC occurrence in individual patients and overcome it. Early identification of patients at high risk of POCs may aid clinical decision-making and possibly improve outcomes.
Lysophosphatidylcholine (LPC) is a lipid mediator, derived from membrane phospholipids, which has been suggested to regulate excessive immune response [10]. LPC is generated through the action of phospholipase A2 on phosphatidylcholine (PC), and has a potent proinflammatory effect that is mediated by up-regulation of the endothelial cell adhesion molecule, growth factors, and various immune cells in vitro [11,12,13]. Some studies also suggest that LPC may function as an immunosuppressor. Previous studies demonstrated that LPC has a high affinity for the immunoregulatory G protein-coupled receptor G2A, expressed in immature T- and B-cells [14]: G2A-deficient mice developed an autoimmune disease characterized by the activation of lymphocytes and hyper-responsive T-cells [15]. Based on the immunosuppressive potential of LPC, patients with sepsis show significantly decreased LPC blood levels [16,17,18]. LPC supplementation in an experimental sepsis model had a beneficial anti-inflammatory effect [19]. Thus, LPC depletion is closely related to sepsis development through the promotion of an exaggerated immune response.
Numerous studies suggest that exaggerated post-surgical systemic inflammation; specifically, higher levels of interleukin-(IL) 6 and C-reactive protein (CRP), has a negative effect on short- and long-term outcomes [20,21,22,23]. The magnitude of this inflammatory response varies widely among individuals and depends on type, duration, and extent of surgery; type of anesthesia; and perioperative blood transfusion; among other factors [24,25,26,27]. However, the influence of immunomodulating lipid mediator LPC on clinical outcomes after elective cancer surgery is undetermined. Therefore, this study examined the associations between postoperative LPC changes and postoperative inflammatory response with respect to POC occurrence, and their predictive value for POCs after elective CRC surgery.
Materials and methods
Patients
We conducted a prospective single-institutional observational study at the Department of Surgery at Nippon Medical School Chiba Hokusoh Hospital from January, 2014 to December, 2015. Forty-three patients with CRC who underwent elective surgery with primary tumor resection were included in this study. All patients received antibiotic prophylaxis as per local protocols, but not oral antibiotic prophylaxis. The surgical approach (open or laparoscopic) and extent of resection were decided by the surgeon, taking patient factors into consideration. Patients who were younger than 18 years old, those with a history of preoperative chemotherapy or radiation, those with clinical symptoms of infection, and those with chronic liver dysfunction and cirrhosis, chronic renal failure, or gastrointestinal obstructions, were excluded from the analysis.
The 43 patients were divided into two groups at the end of their individual follow-up periods, according to whether they had suffered POCs (n = 10; POC group), or not (n = 33; No-POC group). All POCs were recorded daily by attending physicians during the patients’ hospital stay and at the first visit to the outpatient clinic, approximately 30 days after surgery. POCs were classified based on the Clavien–Dindo grading system [28]. Complications with Clavien–Dindo grades ≥ I were defined as POCs in this study. We evaluated the association between changes in blood LPC levels and postoperative inflammatory response and the predictive value for the occurrence of POCs.
Relevant patient and clinical variables were recorded at the time of chart review. The specific intake variables for each patient included sex, age, body mass index (BMI), comorbidity, American Society of Anesthesiologists (ASA) score, tumor location, pathological stage, surgical approach (laparoscopic or open), resection of other organs, duration of surgery, intraoperative blood loss, preoperative blood white blood cell count (WBC), CRP, and albumin concentrations.
This study was conducted in accordance with the Helsinki Declaration. The study protocol was approved by the Ethics Committee of Nippon Medical School Chiba Hokusoh Hospital (Chiba, Japan) (Approval no. 562).
Blood sampling and assays
Peripheral venous blood samples were collected before (pre) and immediately after surgery (post) and on the mornings of postoperative days (PODs) 1, 3, 5, and 7. The WBC, CRP, and albumin levels were routinely measured immediately, at a central laboratory. The limit of detection for the CRP assay was 0.02 mg/dL. The remaining samples were separated immediately by centrifugation at 4 °C for 10 min at 2000×g and stored at − 80 °C until assays. Blood LPC and IL-6 levels were analyzed using commercially available assay kits (LPC: AZWELL LPC Assay kit; Alfresa Pharma, Osaka, Japan; IL-6: Human IL-6 DuoSet ELISA, R&D Systems, Minneapolis, MN, USA). Blood phosphatidylcholine (PC) and lysophospholipase D/autotaxin (ATX) levels were measured using commercially available kits (Phosphatidylcholine assay kit; Cayman Chemical, Ann Arbor, MI; Human ENPP-2/Autotaxin DuoSet ELISA, R&D Systems), before and after surgery, and on POD1.
Statistical analysis
Data are presented as means ± standard error (SE). Postoperative LPC changes are expressed as comparisons with baseline levels before surgery. The two-tailed Student’s t test and Mann–Whitney U test were used to compare continuous variables, and the χ2 test and Fisher’s exact test were used to compare discrete variables. Correlations were analyzed by Spearman’s rank correlation. Variables that had a P value < 0.05 in the univariate analysis were entered into the multivariate logistic regression analysis. Receiver operating characteristic (ROC) curve analysis was performed to identify the threshold of the LPC ratio in terms of POC. P < 0.05 was considered significant. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University), which is a graphical user interface for R, version 3.1.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patients’ characteristics
Table 1 summarizes the clinical characteristics of the two study groups (the No-POC group vs. the POC group) and the results of univariate analyses of intergroup differences. The two groups did not differ significantly in sex, age, BMI, comorbidities, ASA score, tumor location, pathological stage, surgical approach, resection of other organs, or intraoperative blood loss. The operative time was significantly longer (P = 0.048) and intraoperative blood loss was significantly greater (P = 0.049) in the POC group than in the No-POC group. Among preoperative blood inflammation and nutritional variables, WBC, CRP, albumin concentrations did not differ significantly between the groups. The preoperative LPC was also not significantly different between the groups.
The prevalence of POCs (Clavien–Dindo grading ≥ I) was 10/43 (23.3%). Table 2 details the complications in the two groups. Four patients with grade IIIb POCs required further surgery. None of the patients died within 30 days. The median timing of POC diagnosis was POD 5 (range: PODs 3–16).
Postoperative inflammatory responses
Compared with the preoperative values, the CRP and IL-6 levels in both groups increased significantly after surgery and peaked on POD 3 and immediately post-surgery, respectively (Fig. 1a, b). The postoperative increases in CRP on PODs 1, 3, 5, and 7 for both groups and the IL-6 levels immediately post-surgery, and on PODs 1, and 3 for the No-POC group, and immediately post-surgery, and on POD 1 for the POC group were all significant. The preoperative CRP levels of the two groups did not differ significantly, but the POC group had significantly higher CRP levels on PODs 5, and 7. In contrast, no significant differences were observed for IL-6 during the entire perioperative period because of the large individual variations.
Postoperative changes in blood C-reactive protein (CRP) (a), IL-6 (b), and lysophosphatidylcholine (LPC) levels (c) in the patients without (No-POC group; open circles) and those with (POC group; closed circles) postoperative complications (POCs). LPC is expressed as ratio of preoperative value. Data are expressed as means ± SE. *P < 0.05 vs. preoperative values in the same group; †P < 0.05 vs. No-POC group at the same time. POC postoperative complication, pre preoperative, post immediately after surgery, POD postoperative day
Postoperative changes in LPC
Figure 1c shows the postoperative changes in the blood LPC ratios (to the preoperative values) in the two groups. Both groups showed decreased LPC ratios until POD 1 and then recovered gradually thereafter. Although the No-POC group recovered and reached preoperative levels on POD 7, the LPC ratios in the POC group remained significantly decreased during the entire postoperative period. The POC group had significantly lower LPC ratios than the No-POC group during the entire postoperative period.
Correlation between LPC and IL-6 levels
Figure 2 shows the correlations between blood LPC ratios and IL-6 levels immediately post-surgery and on POD 1. At both time points, the LPC ratios were significantly inversely correlated with the IL-6 levels (P = 0.033 immediately post-surgery and P = 0.041 on POD 1, respectively; Fig. 2a, b).
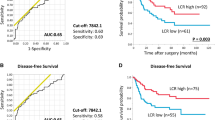
Predictive value of LPC on postoperative complications
The ROC curve analysis of LPC ratios (post to pre) with respect to POCs identified 51.2% as the optimal cut-off point [area under the ROC curve (AUC) 0.798, 95% confidence interval (CI) 0.629–0.952; Fig. 3], with 80.0% sensitivity and 81.2% specificity.
Multivariate logistic regression analysis of POCs vs. variables selected by univariate analyses and classified into dichotomous variables using cut-off values determined by ROC analyses showed only the LPC ratio (post to pre) as an independent risk factor for POCs (odds ratio 15.1, 95% CI 1.83–125, P = 0.011; Table 3).
Mechanism of decreased LPC after surgical stress
The postoperative to preoperative ratios of blood PC and LPC were significantly correlated (P = 0.040; Fig. 4a). Both groups showed decreased postoperative blood PC ratios until POD 1 (Fig. 4b), but the POC group had significantly lower postoperative PC ratios than the No-POC group. Blood ATX levels were investigated in the same manner as for PC, but preoperative levels were maintained after surgical stress in both groups (data not shown).
Correlation between blood phosphatidylcholine (PC) and LPC immediately after surgery (a). Changes in the blood PC levels in the No-POC (open circles) and POC (closed circles) groups (b). PC and LPC are expressed as ratios from the preoperative values. Data are expressed as means ± SE. *P < 0.05 vs. preoperative values in the same group; †P < 0.05 vs. No-POC group at the same time. POC postoperative complication, pre preoperative, post immediately after surgery, POD postoperative day
Predictive value of PC and LPC combined scoring for POCs
The results shown in Fig. 4a, b suggest the predictive potential not only of LPC, but also of PC for POCs. The ROC curve analysis of PC ratios (post to pre) with respect to POCs identified 88.7% as the optimal cut-off point [area under the ROC curve (AUC) 0.764, 95% confidence interval (CI) 0.572–0.955), with 63.6% sensitivity and 90.0% specificity (Supplementary Fig. 1). To increase the predictive potential for POCs, we established an LPC and PC combined scoring system. As shown in Supplementary Table 1, 70% of patients with a score of 2 had POCs, with a diagnostic likelihood ratio of 7.7. In contrast, none of patients with a score of 0 had POCs.
Discussion
The main and novel finding of this study is that a decrease in blood LPC levels immediately after surgery is an independent risk factor for the development of POCs in patients undergoing CRC surgery. The decreased LPC levels contribute to exaggerated pro-inflammatory host responses after surgery, which might result in POCs.
LPC is a highly abundant bioactive lysoglycerophospholipid, present at high concentrations (of about 190 µM) in the circulation. The early observation that LPC is upregulated at sites of inflammation was followed by numerous publications on LPC-elicited responses in various cell types [11,12,13]. Notably, most reported studies on LPC regulation of inflammatory responses have been performed in vitro, in the absence of co-stimulatory and/or inhibitory signals. Moreover, extreme caution should be exercised when evaluating reported LPC actions, to ensure that used concentrations are within the physiological range and to exclude experiments that were conducted in the presence of serum (containing phospholipids and albumin, which quench LPC activity) and/or LPC-hydrolyzing enzymes. For instance, the activation of nuclear factor-κB (NF-κB; a major transcriptional regulator of pro-inflammatory cytokine expression) by LPC appears to depend on the LPC concentration: lower LPC concentrations increase endothelial NF-κB activity, whereas higher LPC concentrations inhibit it [29]. Thus, positive and negative biphasic regulatory actions of LPC on NF-κB activity in endothelial cells suggest different functions for LPC in mediating endothelial barrier functions and the extravasation of immune mediators, depending on its concentration in the inflamed site. A recent in vitro study demonstrated that LPC alone triggers a classical pro-inflammatory phenotype by activating TLR4- and TLR2-1-mediated signaling; however, in the presence of classical TLR ligands, LPC counteracted some TLR-mediated intracellular responses, ultimately inducing an anti-inflammatory phenotype in macrophages [30].
Amid the controversy between the pro-inflammatory and anti-inflammatory properties of LPC, Yan et al. [19] demonstrated the protective effects of LPC in animal models of lethal sepsis, attributed to the anti-inflammatory effect of protection from stimulating neutrophils to destroy ingested bacteria via an H2O2-dependent mechanism. LPC also helps protect against lethal endotoxemia, which implies that it may exert protective effects through an additional, bactericidal-independent mechanism [19, 31]. Chen et al. [32] reported that stearoyl LPC dramatically inhibited the release of endotoxin-induced high-mobility group box 1 (HMGB1), a late lethal mediator of sepsis, from monocytic cells by inhibiting the active release pathway. These protective effects of LPC against sepsis are mediated through the LPC receptor G2A, which is expressed in neutrophils and macrophages [33]. In studies of sepsis in humans, decreased LPC blood levels were observed and found to be correlated with sepsis-related mortality [16,17,18]. Blood LPC levels in sepsis were inversely correlated with CRP and procalcitonin levels [16], which imply the function of LPC in controlling inflammatory responses in vivo. In line with these in vivo observations, we found that patients with more decreased postoperative LPC levels had greater postoperative inflammatory responses. These results suggest that LPC has a major function in attenuating systemic inflammation, thus decreasing the likelihood of POCs after CRC surgery.
CRC surgery is common and involves major abdominal procedures with a complication rate of about 30% [4, 5]. Previous clinical studies suggest that the hyper-inflammatory host response following major surgical trauma, based on excessive release of the pro-inflammatory cytokines, TNF-α and IL-1β, is the cause of the increased mortality and risk of POCs and multiple organ failure [34, 35]. Early recognition of POCs optimizes the chance of better outcomes. One way to enhance early detection of complications is by using pro-inflammatory markers as predictors of outcome [36]. For instance, CRP, which is generally used to monitor the patient’s condition over time after surgery, is a widely accepted predictor of POCs after CRC surgery [37,38,39]. However, the diagnostic window of 3–4 days after surgery is relatively late for early recognition [37,38,39]. The median time from surgery to a complication was 5 days in our cohort, which suggests that a substantial number of POCs are diagnosed before CRP and can even be used to identify which patients are at higher risk. A recent study found that high IL-6 levels on POD1were associated with an increased risk of complications after major abdominal surgery, but its predictive value is not high (AUC 0.67) [22]. In our study, CRP and IL-6 levels did not predict POCs.
A focus of the present study was to ascertain how surgical stress reduces circulating LPC levels. We measured the blood levels of PC, a phospholipid and precursor of LPC, as well as ATX, a major enzyme synthesizing lysophospatidic acid (LPA) from LPC. We found that preoperative blood ATX levels were maintained after surgery, which implies that LPC metabolism is not activated by surgical stress. However, the blood PC levels decreased after surgery and the POC group showed more profound decreases than the No-POC group. Moreover, the postoperative changes in PC were significantly correlated with the changes in LPC levels. Taken together, these results indicate that decreased blood PC levels induced by surgical stress were responsible for the decreased LPC levels. A plausible mechanism for the surgical stress-induced lower PC levels is decreased release of PC from cell membranes to the circulation.
To be useful, biomarkers should be measured quickly, easily, and effectively in the clinical setting. Although several methods of measuring LPC concentrations have been reported, these methods (especially liquid-chromatography-mass spectrometry) are too complicated and/or time-consuming for measuring LPC in human blood samples. The enzymatic LPC assay utilized in this study is simple, specific for LPC, and can be applied with an automatic analyzer, thus facilitating its clinical application [40].
This study has several potential clinical benefits. For patients with higher levels of blood LPC than the cut-off, it may provide their clinicians with reassurances about POC development and allow for early discharge. In contrast, for those with lower levels, it may provide an early warning to provide prompt reassessment and careful management.
This observational study had several limitations. First, it was a single-institutional study limited by its relatively small sample size, which influenced the predictive power of the marker to differentiate POCs from no POCs. Second, we analyzed total blood LPC levels, rather than specific molecular LPC species, using commercial enzymatic LPC assay kits. Third, the influence of blood LPC levels on long-term outcomes was not evaluated, so this needs further investigation. Fourth, the magnitude of surgical stress of different procedures varied; for example, colonic and rectal surgery, and open vs. laparoscopic surgery.
In conclusion, our data indicate that decreased blood LPC levels immediately after surgery may predict whether CRC patients will produce exaggerated inflammatory host responses and thus be more susceptible to POCs. We postulate that this biomarker could enhance the ability to predict operative risk for patients undergoing CRC surgery, which in turn could improve their postoperative management.
References
Projected cancer statistics, 2017 https://ganjoho.jp/en/public/statistics/short_pred.html.
Oliphant R, Nicholson GA, Horgan PG, McMillan DC, Morrison DS, West of Scotland Colorectal Cancer Managed Clinical N. The impact of surgical specialisation on survival following elective colon cancer surgery. Int J Colorectal Dis. 2014;29:1143–50.
Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Med Care. 2011;49:1076–81.
Alves A, Panis Y, Mathieu P, Mantion G, Kwiatkowski F, Slim K, et al. Postoperative mortality and morbidity in French patients undergoing colorectal surgery: results of a prospective multicenter study. Arch Surg. 2005;140:278–83 (discussion 284).
Sjo OH, Larsen S, Lunde OC, Nesbakken A. Short term outcome after emergency and elective surgery for colon cancer. Colorectal Dis. 2009;11:733–9.
Artinyan A, Orcutt ST, Anaya DA, Richardson P, Chen GJ, Berger DH. Infectious postoperative complications decrease long-term survival in patients undergoing curative surgery for colorectal cancer: a study of 12,075 patients. Ann Surg. 2015;261:497–505.
Brown SR, Mathew R, Keding A, Marshall HC, Brown JM, Jayne DG. The impact of postoperative complications on long-term quality of life after curative colorectal cancer surgery. Ann Surg. 2014;259:916–23.
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P. Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg. 2011;253:890–9.
Richards CH, Platt JJ, Anderson JH, McKee RF, Horgan PG, McMillan DC. The impact of perioperative risk, tumor pathology and surgical complications on disease recurrence following potentially curative resection of colorectal cancer. Ann Surg. 2011;254:83–9.
Bulger EM, Maier RV. Lipid mediators in the pathophysiology of critical illness. Crit Care Med. 2000;28:N27–36.
Kabarowski JH, Xu Y, Witte ON. Lysophosphatidylcholine as a ligand for immunoregulation. Biochem Pharmacol. 2002;64:161–7.
Kume N, Gimbrone MA Jr.. Lysophosphatidylcholine transcriptionally induces growth factor gene expression in cultured human endothelial cells. J Clin Investig. 1994;93:907–11.
Sevastou I, Kaffe E, Mouratis MA, Aidinis V. Lysoglycerophospholipids in chronic inflammatory disorders: the PLA(2)/LPC and ATX/LPA axes. Biochim Biophys Acta. 2013;1831:42–60.
Kabarowski JH, Zhu K, Le LQ, Witte ON, Xu Y. Lysophosphatidylcholine as a ligand for the immunoregulatory receptor G2A. Science. 2001;293:702–5.
Le LQ, Kabarowski JH, Weng Z, Satterthwaite AB, Harvill ET, Jensen ER, et al. Mice lacking the orphan G protein-coupled receptor G2A develop a late-onset autoimmune syndrome. Immunity. 2001;14:561–71.
Park DW, Kwak DS, Park YY, Chang Y, Huh JW, Lim CM, et al. Impact of serial measurements of lysophosphatidylcholine on 28-day mortality prediction in patients admitted to the intensive care unit with severe sepsis or septic shock. J Crit Care. 2014;29:882 e885-811.
Cho WH, Park T, Park YY, Huh JW, Lim CM, Koh Y, et al. Clinical significance of enzymatic lysophosphatidylcholine (LPC) assay data in patients with sepsis. Eur J Clin Microbiol Infect Dis. 2012;31:1805–10.
Drobnik W, Liebisch G, Audebert FX, Frohlich D, Gluck T, Vogel P, et al. Plasma ceramide and lysophosphatidylcholine inversely correlate with mortality in sepsis patients. J Lipid Res. 2003;44:754–61.
Yan JJ, Jung JS, Lee JE, Lee J, Huh SO, Kim HS, et al. Therapeutic effects of lysophosphatidylcholine in experimental sepsis. Nat Med. 2004;10:161–7.
McSorley ST, Khor BY, MacKay GJ, Horgan PG, McMillan DC. Examination of a CRP first approach for the detection of postoperative complications in patients undergoing surgery for colorectal cancer: a pragmatic study. Medicine (Baltimore). 2017;96:e6133.
McSorley ST, Ramanathan ML, Horgan PG, McMillan DC. Postoperative C-reactive protein measurement predicts the severity of complications following surgery for colorectal cancer. Int J Colorectal Dis. 2015;30:913–7.
Rettig TC, Verwijmeren L, Dijkstra IM, Boerma D, van de Garde EM, Noordzij PG. Postoperative interleukin-6 level and early detection of complications after elective major abdominal surgery. Ann Surg. 2016;263:1207–12.
Watt DG, McSorley ST, Park JH, Horgan PG, McMillan DC. A postoperative systemic inflammation score predicts short- and long-term outcomes in patients undergoing surgery for colorectal cancer. Ann Surg Oncol. 2017;24:1100–9.
Blajchman MA. Immunomodulation and blood transfusion. Am J Ther. 2002;9:389–95.
Chimienti G, Aquilino F, Rotelli MT, Russo F, Lupo L, Pepe G. Lipoprotein(a), lipids and proinflammatory cytokines in patients undergoing major abdominal surgery. Br J Surg. 2006;93:347–53.
Gilliland HE, Armstrong MA, Carabine U, McMurray TJ. The choice of anesthetic maintenance technique influences the antiinflammatory cytokine response to abdominal surgery. Anesth Analg. 1997;85:1394–8.
Veenhof AA, Sietses C, von Blomberg BM, van Hoogstraten IM, vd Pas MH, Meijerink WJ, et al. The surgical stress response and postoperative immune function after laparoscopic or conventional total mesorectal excision in rectal cancer: a randomized trial. Int J Colorectal Dis. 2011;26:53–9.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Sugiyama S, Kugiyama K, Ogata N, Doi H, Ota Y, Ohgushi M, et al. Biphasic regulation of transcription factor nuclear factor-kappaB activity in human endothelial cells by lysophosphatidylcholine through protein kinase C-mediated pathway. Arterioscler Thromb Vasc Biol. 1998;18:568–76.
Carneiro AB, Iaciura BM, Nohara LL, Lopes CD, Veas EM, Mariano VS, et al. Lysophosphatidylcholine triggers TLR2- and TLR4-mediated signaling pathways but counteracts LPS-induced NO synthesis in peritoneal macrophages by inhibiting NF-kappaB translocation and MAPK/ERK phosphorylation. PLoS One. 2013;8:e76233.
Wang H, Czura CJ, Tracey KJ. Lipid unites disparate syndromes of sepsis. Nat Med. 2004;10:124–5.
Chen G, Li J, Qiang X, Czura CJ, Ochani M, Ochani K, Ulloa L, et al. Suppression of HMGB1 release by stearoyl lysophosphatidylcholine:an additional mechanism for its therapeutic effects in experimental sepsis. J Lipid Res. 2005;46:623–7.
Kabarowski JH. G2A and LPC: regulatory functions in immunity. Prostaglandins Other Lipid Mediat. 2009;89:73–81.
Menger MD, Vollmar B. Surgical trauma: hyperinflammation versus immunosuppression? Langenbecks Arch Surg. 2004;389:475–84.
Roumen RM, Hendriks T, van der Ven-Jongekrijg J, Nieuwenhuijzen GA, Sauerwein RW, van der Meer JW, et al. Cytokine patterns in patients after major vascular surgery, hemorrhagic shock, and severe blunt trauma. Relation with subsequent adult respiratory distress syndrome and multiple organ failure. Ann Surg. 1993;218:769–76.
Mokart D, Merlin M, Sannini A, Brun JP, Delpero JR, Houvenaeghel G, et al. Procalcitonin, interleukin 6 and systemic inflammatory response syndrome (SIRS): early markers of postoperative sepsis after major surgery. Br J Anaesth. 2005;94:767–73.
Korner H, Nielsen HJ, Soreide JA, Nedrebo BS, Soreide K, Knapp JC. Diagnostic accuracy of C-reactive protein for intraabdominal infections after colorectal resections. J Gastrointest Surg. 2009;13:1599–606.
Platt JJ, Ramanathan ML, Crosbie RA, Anderson JH, McKee RF, Horgan PG, et al. C-reactive protein as a predictor of postoperative infective complications after curative resection in patients with colorectal cancer. Ann Surg Oncol. 2012;19:4168–77.
Warschkow R, Steffen T, Beutner U, Muller SA, Schmied BM, Tarantino I. Diagnostic accuracy of C-reactive protein and white blood cell counts in the early detection of inflammatory complications after open resection of colorectal cancer: a retrospective study of 1187 patients. Int J Colorectal Dis. 2012;27:1377.
Kishimoto T, Soda Y, Matsuyama Y, Mizuno K. An enzymatic assay for lysophosphatidylcholine concentration in human serum and plasma. Clin Biochem. 2002;35:411–6.
Acknowledgements
This study was supported financially by a Grant-in-Aid for Scientific Research from The Ministry of Education, Culture, Sports, Science and Technology of Japan (15K10037: Matsuda A).
Author information
Authors and Affiliations
Contributions
All authors are in agreement with the content of the manuscript. Authors’ contributions are as follows: study concept and design, AM and MY; acquisition of data, AM and NS; analysis and interpretation of data, AM, MY, SM, TY and TM; drafting of the manuscript, AM; study supervision, MM and EU.
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Matsuda, A., Yamada, M., Matsumoto, S. et al. Lysophosphatidylcholine as a predictor of postoperative complications after colorectal cancer surgery. Surg Today 48, 936–943 (2018). https://doi.org/10.1007/s00595-018-1675-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-018-1675-2